Abstract
We report a case of primary multifocal osseous lymphoma in a 6-year-old girl presenting with multifocal osteolytic lesions without systemic symptoms or identifiable non-osseous primary tumor. The differential diagnoses for such a presentation include histiocytosis X, chronic recurrent multifocal osteomyelitis, acute lymphoblastic leukemia, metastatic disease, and primary bone lymphoma. Although non-Hodgkin lymphoma is common in the pediatric population, its presentation as a primary bone tumor, especially with multifocal disease, is extremely rare and is frequently misdiagnosed. We hope that awareness of this entity will help radiologists achieve timely diagnosis and intervention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary osseous lymphoma in children is a rare entity, accounting for 2.8–4.2% of all pediatric non-Hodgkin lymphoma (NHL) cases [1, 2]. Primary multifocal osseous lymphoma is a subset of primary osseous lymphoma, in which multiple bones are involved in the absence of lymph node or visceral disease for at least 6 months following initial presentation [3]. Although lymphoma is a common neoplasm of the pediatric population, its initial presentation as lytic bone lesions is unusual [4]. In addition, the majority of osseous lymphomas are NHL of diffuse large B-cell type. It is extremely rare for a precursor B-cell neoplasm to present as a primary bone tumor [5]. To our knowledge, the imaging findings of primary multifocal osseous lymphoma in children have not been described in the radiology literature. We report a case of multifocal primary osseous lymphoma secondary to precursor B-cell lymphoblastic lymphoma (PBLL) in a 6-year-old girl.
Case report
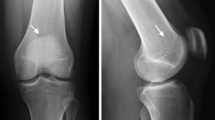
A 6-year-old girl presented with a 6-month history of polyarthralgia, initially involving the right hip, with subsequent involvement of the right knee, right ankle, left clavicle, and left elbow. Her symptoms were not accompanied by fever, night sweats or weight loss. Laboratory studies at presentation revealed a normal white blood cell count and a normal hemoglobin level. Her platelet count and C-reactive protein were minimally elevated. Initial radiographs revealed no bone abnormality. Five months after onset of symptoms an MRI scan of the right femur revealed a focal marrow lesion in the proximal shaft (Fig. 1). Biopsy of the femoral lesion and an iliac bone marrow biopsy were both normal. Given the history of multifocal bone pain and a negative bone biopsy, the clinical picture was thought to be most consistent with chronic recurrent multifocal osteomyelitis (CRMO), and the girl was referred to the rheumatology service at our institution. By this time she had to use a wheelchair because of bone pain, though her laboratory studies remained essentially unchanged. Radiographs revealed generalized osteopenia and a focal lytic area with cortical destruction on the medial aspect of the distal femoral metaphysis and an osteolytic area in the proximal tibial metaphysis (Fig. 1). The cortical destruction and lack of typical sclerotic borders led to our concern that this was malignancy rather than CRMO. A repeat MRI scan revealed multicentric areas of marrow infiltration involving the metaphyses, epiphyses and diaphyses of the femur, tibia and fibula (Fig. 1). CT-guided biopsy of the tibial lesion showed precursor B-cell lymphoblasts. a CT scan of the neck, chest, abdomen and pelvis and a whole-body FDG-PET scan performed 6 months after initial presentation showed no evidence of extraosseous disease (Fig. 1), leading to a diagnosis of primary multifocal osseous lymphoma.
A 6-year-old girl with multifocal bone pain for 6 months. a Coronal T1-W MRI shows a focal area of marrow replacement in the proximal femur (asterisk). b Radiograph of right knee obtained 1 month later shows generalized osteopenia and a focal lytic area with cortical destruction on the medial aspect of the distal femoral metaphysis and an osteolytic area in the proximal tibial metaphysis (arrows). c, d Coronal T1- and T2-W MR images of the femurs show marrow replacement in the left femoral neck and in the metaphyses and epiphyses of both distal femurs (arrows). e Coronal T1-W image shows extensive areas of marrow infiltration in both tibia, as well (arrows). f 18F-FDG-PET scan performed for staging shows hypermetabolic foci in the right femoral neck and both distal femurs, and multiple lesions in the tibia corresponding to the areas of marrow infiltration seen on the MR images, without evidence of extraosseous disease
Discussion
Primary lymphoma of bone in children is rare compared with other bone tumors [1]. It can affect children of all ages but is most commonly diagnosed in early adolescence, with a slight male predilection. The most common presenting complaint is localized or migratory pain, as in our patient [2]. Other symptoms include swelling or palpable mass, fever, weight loss, or limp. Common sites of bony involvement include femur, tibia, pelvis, and spine. The disease can be unifocal or multifocal. In one series of 15 pediatric cases of primary bone lymphoma, seven children had multifocal disease, with an average number of 3.1 lesions per child [2].
Imaging plays an important role in the diagnosis and staging of primary bone lymphoma. Though the imaging findings of primary lymphoma of bone have been reported in the radiology literature, these are predominantly adult series with solitary bone lesions [6]. We did not find a description of the imaging of primary bone lymphoma in children in the radiology literature, though case reports and small series have been described in the oncology and orthopedic literature [1, 2]. Primary multifocal osseous lymphoma is an even more rare entity and to our knowledge there is only one case series of eight patients (six adults, two children) describing the imaging findings of this entity in the radiology literature [3]. Radiographs demonstrate a predominantly osteolytic process (Fig. 1), though associated sclerosis can also be seen [2]. The radiographic appearance can mimic an aggressive lesion such as Ewing sarcoma or a benign process such as CRMO or histiocytosis X. Radiographic findings of bone lymphoma that can have a negative prognostic implication include associated cortical destruction, pathological fracture or a soft-tissue mass [6].
Advanced imaging techniques are essential, as radiographs can be normal or underestimate the extent of disease. In one series, plain films were noted to detect only 25% of lesions evident on scintigraphy [3]. Evaluation with MRI or FDG-PET can help determine the multifocality of disease (Fig. 1). MRI is especially helpful in local staging and can help evaluate extension across the physeal plate. The signal characteristics of osseous lymphoma on MRI have been described as being predominantly isointense to muscle on T1-weighted images and isointense to hematopoietic marrow on T2-weighted images [3]. The presence of fibrosis within the tumor might account for the relatively low signal on T2-weighted images. Some authors have found short tau inversion recovery (STIR) images to demonstrate the abnormality with maximum conspicuity [3]. In our patient the disease was hyperintense to marrow and most conspicuous on fat-suppressed T2-weighted images. Another imaging pattern that has been described in lymphoma and other small round cell tumors such as Ewing sarcoma is the presence of a large soft-tissue mass and marrow involvement with minimal associated cortical destruction. On CT images most lesions are permeative or destructive with or without sclerosis.
Because of the relative rarity of primary osseous lymphoma in children, it is often misdiagnosed or the diagnosis is delayed [5]. In one pediatric series of bone lymphoma the mean delay from onset of symptoms to diagnosis was 6.2 months [2]. In this series, 5 of 15 children were initially misdiagnosed as having metastatic disease, eosinophilic granuloma, osteosarcoma, or chronic sterile osteomyelitis. In another pediatric series, 10 of 11 children with osseous lymphoma had an incorrect referral diagnosis [1]. Our patient had been symptomatic for 6 months, with a negative bone biopsy that led to a misdiagnosis of CRMO at the referring institution. The radiographic finding atypical for CRMO in our patient was a predominant osteolytic process without associated sclerosis. MRI clearly demonstrated extensive areas of marrow replacement in the metaphysis with extension into the epiphysis. This led us to question the diagnosis of CRMO and suspect a malignancy. Our case and the series of Glotzbecker et al. [2] remind one of the need for an adequate biopsy specimen to avoid missing the diagnosis of bone lymphoma.
Primary bone lymphoma should be included in the differential diagnoses of lytic bone lesions, with the other more common diagnoses in the pediatric age group being the other small round blue cell tumors such as Ewing sarcoma, metastatic disease from neuroblastoma or rhabdomyosarcoma, and multifocal pyogenic osteomyelitis. The correct diagnosis of osseous small round blue cell tumors in children might be extremely difficult because of overlapping clinical, radiographic, histologic, and immunophenotypic features. Immunohistochemical studies are essential to clarify the histogenesis of small round blue cell tumors.
Primary osseous lymphoma is predominantly of non-Hodgkin type and accounts for 2.8–4.2% of all NHL cases in children [1, 2]. The WHO classifies NHL into four main types: precursor B-cell and precursor T-cell neoplasms, which include lymphoblastic lymphoma/leukemia, and mature B-cell and mature T-cell neoplasms. Although the majority of intraosseous lymphomas are mature B-cell tumors, PBLL can present with bony involvement in children and young adults [2]. In a review of 98 patients reported in the literature, 64% were found to be younger than 18 years of age [7]. While lymphoblastic lymphoma secondary to precursor T-cells typically presents with mediastinal disease, the three most common sites of disease in PBLL are skin, lymph nodes, and bone [7]. Multifocal bone involvement by PBLL has been previously described, but to our knowledge this has not been described in the radiology literature [4].
Precursor B-cell neoplasms usually originate in bone marrow as acute lymphoblastic leukemia (ALL), though rarely they present as a primary bone tumor [5]. The etiology for multifocal bone involvement from PBLL remains unclear and it suggests a close relationship of PBLL with leukemia [8]. However, progression of PBLL to leukemia is unusual even in patients with multiple and multifocal relapses. In patients who have a relapse, recurrent tumor tends to involve other extranodal sites, and leukemic involvement is uncommon [8]. The pattern of multifocal osseous involvement in our patient reminds one of advanced leukemia; however, our patient had no evidence of marrow involvement, with a normal white cell count and differential and normal hemoglobin. The criteria used to differentiate PBLL from ALL include: (1) manifestation as bulky masses in solid organs; (2) absent or less than 25% bone marrow involvement; and (3) absence of peripheral blood involvement [7]. Because PBLL and ALL are histologically and immunophenotypically similar, these tumors are considered by many researchers to represent different clinical presentations of the same neoplasm and are grouped in the category of B-cell lymphoblastic leukemia/lymphoma in the WHO classification of lymphoid neoplasms [7].
In conclusion, primary multifocal osseous lymphoma can manifest with lytic bone lesions without evidence of disease in the bone marrow or in the peripheral blood. It should be included in the differential diagnoses of multifocal lytic lesions or multifocal areas of marrow replacement with small round blue cells. Suggestion of this diagnosis by the pediatric radiologist can prompt the pathologist to perform immunophenotyping to establish the correct diagnosis. Imaging with whole-body MRI or PET scans can help to determine the extent of disease.
References
Furman WL, Fitch S, Hustu HO et al (1989) Primary lymphoma of bone in children. J Clin Oncol 7:1275–1280
Glotzbecker MP, Kersun LS, Choi JK et al (2006) Primary non-Hodgkin’s lymphoma of bone in children. J Bone Joint Surg Am 88:583–594
Melamed JW, Martinez S, Hoffman CJ (1997) Imaging of primary multifocal osseous lymphoma. Skeletal Radiol 26:35–41
Iravani S, Singleton TP, Ross CW et al (1999) Precursor B lymphoblastic lymphoma presenting as lytic bone lesions. Am J Clin Pathol 112:836–843
Ozdemirli M, Fanburg-Smith JC, Hartmann DP et al (1998) Precursor B-lymphoblastic lymphoma presenting as a solitary bone tumor and mimicking Ewing’s sarcoma: a report of four cases and review of the literature. Am J Surg Pathol 22:795–804
Krishnan A, Shirkhoda A, Tehranzadeh J et al (2003) Primary bone lymphoma: radiographic-MR imaging correlation. Radiographics 23:1371–1383
Maitra A, McKenna RW, Weinberg AG et al (2001) Precursor B-cell lymphoblastic lymphoma. A study of nine cases lacking blood and bone marrow involvement and review of the literature. Am J Clin Pathol 115:868–875
Lin P, Jones D, Dorfman DM et al (2000) Precursor B-cell lymphoblastic lymphoma: a predominantly extranodal tumor with low propensity for leukemic involvement. Am J Surg Pathol 24:1480–1490
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sato, T.S.P., Ferguson, P.J. & Khanna, G. Primary multifocal osseous lymphoma in a child. Pediatr Radiol 38, 1338–1341 (2008). https://doi.org/10.1007/s00247-008-0964-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-008-0964-0