Abstract
Background
Malrotation is a congenital disorder of abnormal intestinal rotation and fixation that predisposes infants to potentially life-threatening midgut volvulus. Upper gastrointestinal tract (UGI) examination is sometimes equivocal and can lead to inaccurate diagnosis.
Objective
To determine the diagnostic performance of UGI examinations in children who subsequently underwent a Ladd procedure for suspected malrotation or volvulus.
Materials and methods
We reviewed all children up to 21 years old who had undergone both a UGI examination and a Ladd procedure for possible malrotation across 9 years. Children were excluded if they had not undergone either a UGI examination or a Ladd procedure and if congenital abdominal wall defects were present.
Results
Of 229 patients identified, 166 (59% male, median age 67 days) were included. Excluded were 47 without a UGI series, 12 with omphalocele or gastroschisis, 1 without verifiable operative data, 1 who had not undergone a Ladd procedure, and 2 older than 21 years. Of the 166 patients, 40% were neonates and 73% were <12 months old, and 31% presented with bilious vomiting and 15% with abdominal distention. Of 163 patients with surgically verified malrotation, 156 had a positive UGI examination, a sensitivity of 96%. There were two patients with a false-positive UGI examination and seven with false-negative examination. Jejunal position was normal in six of the seven with a false-negative examination and abnormal in the two with a false-positive examination. Of 38 patients with surgically verified volvulus, 30 showed volvulus on the UGI series. Five required bowel resection and three died.
Conclusion
Jejunal position can lead to inaccurate UGI series interpretation. Meticulous technique and periodic assessment of performance will help more accurately diagnose difficult or equivocal cases.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Intestinal malrotation, a congenital disorder of abnormal intestinal rotation and fixation within the peritoneal cavity, is present in approximately 1 in 500 neonates at birth [1]. Malrotation predisposes afflicted individuals to the potentially life-threatening condition of midgut volvulus, a surgical emergency. The upper gastrointestinal tract (UGI) examination is the gold standard for radiographic diagnosis of malrotation and volvulus [2–4]. Although this diagnosis is often straightforward, approximately 15% of UGI examinations are equivocal and lead to false-positive or false-negative interpretations [3].
The diagnosis of malrotation is usually made in the neonate or young infant, with up to 75% of symptomatic patients being neonates, and up to 90% being less than 1 year old [1–3, 5, 6]. Bilious vomiting with or without abdominal distention are the classic clinical manifestations of malrotation in newborns [2, 3, 7, 8]. Small-bowel necrosis, short-gut syndrome, dependence on total parenteral nutrition and death are possible sequelae if diagnosis and treatment are delayed. The literature and local practice patterns differ as to what is considered normal variation and what is considered abnormal malrotated small bowel. In addition, the surgical description of malrotation can vary. This confusion makes interpretation of the UGI series more challenging, leading to uncertainty in its accuracy.
We undertook a retrospective analysis of children with surgically proven malrotation to better understand our performance and the difficulties of accurate diagnosis or exclusion in children with clinically suspected malrotation. We also report presenting symptoms, surgical management and outcomes.
Materials and methods
Patient population
The Institutional Review Board approved this retrospective study with a waiver of informed consent. We identified all patients treated at one large Midwestern children’s hospital between September 1996 and November 2005 by searching the hospital admissions database for all patients with the principle diagnosis code for malrotation and volvulus, and for all patients with a current procedural terminology code for Ladd procedure. These cases were cross-referenced with a preexisting billing database maintained by the Pediatric Surgery Department.
Patients were eligible for inclusion in the study if they had received a UGI series prior to undergoing a Ladd procedure. Exclusion criteria were (1) no UGI performed, (2) no Ladd procedure performed, (3) data missing on items 1 or 2, (4) age greater than 21 years, and (5) presence of congenital diaphragmatic hernia, omphalocele or gastroschisis. Patients with a UGI series performed at an outside hospital/institution were included in the study when the interpretations of the UGI examinations were documented in the patient’s medical record. All patient-identifying information was replaced with new unique patient numbers to ensure protection of patient records.
UGI examinations
UGI examinations were performed with barium, which was administered either orally or via a preexisting nasogastric tube for some inpatients. A scout film of the abdomen was obtained as part of the UGI studies prior to 2002, but it was not a part of the standard protocol in the more recent studies. Following left lateral and anteroposterior (AP) pulsed fluoroscopic drinking films of the esophagus, drinking was stopped and the patient was placed in the right lateral position to empty the barium into the duodenum. True lateral views of the entire duodenum were obtained by most of the pediatric radiologists, and they were acquired as pulsed fluoroscopic films or serial spot images. The patients were then turned quickly onto their back for true AP imaging of the duodenum, to document the duodenal-jejunal junction (DJJ). For the UGI via nasogastric tube studies, the infant or child was initially in the right lateral position. The duodenum was imaged when barium filled the entire duodenum, and then an AP image was taken of the abdomen to document the position of the DJJ. A 5-min delayed AP view was subsequently obtained to assess gastric emptying, to look for gastroesophageal reflux, and to demonstrate jejunal position and appearance. Hard-copy films were filed in the patient’s film jackets. After 2001, soft-copy images were sent to the PACS.
UGI examinations were interpreted by all pediatric radiologists within our group, based on routine work schedule assignments. The interpretation of the UGI examinations and assessment for malrotation reflected individual radiologists’ preferences, and the majority of reports documented position, orientation and conformation of the stomach, duodenum, DJJ, jejunum, and cecum (if small-bowel follow-through had been performed). UGI examinations in this study performed at an outside hospital were reviewed by our pediatric radiologists. Patients with a UGI examination at an outside hospital were included in this study when the radiographic impression was documented in their medical record. The prospective interpretations of both in-house and outside-hospital UGI studies were documented in the patients’ medical records.
Clinical and UGI series data collection and analysis
Two of the authors retrospectively reviewed the medical records for pertinent data from clinical, radiographic and surgical history including age, sex, presenting symptoms, prior abdominal surgery, presence of congenital anomalies or syndromes, radiographic findings, surgical management and patient outcomes. Based on the prospective UGI examination report, these coauthors tabulated diagnoses as true-positive, true-negative, false-positive or false-negative for malrotation and for volvulus. The gold standard for these diagnoses was the prospective surgical findings. A UGI study was considered positive for malrotation if the UGI examination report included malrotation in the differential diagnosis. One author remained blinded to the UGI examination report and reviewed all false-negative and false-positive UGI images to describe findings that might have explained the misinterpretations.
The UGI examination reports were reviewed for the presence of individual signs that suggested malrotation or volvulus, including low position of the DJJ; DJJ not located to the left of the left vertebral body pedicle; the suggestive but nondiagnostic sign of jejunum on the right or of heterotaxy syndrome with dextrogastria and jejunum on the left; duodenal redundancy; duodenal distention; DJJ corkscrew appearance; when available on delayed films, an abnormal position of the cecum; and nonspecific findings on the UGI examination such as gastric distention and gastroesophageal reflux.
Sensitivity was calculated to assess performance of the UGI series in diagnosing malrotation. Tabulations and calculations for volvulus were performed in the same manner as for malrotation. All data were entered into Microsoft Excel 2002, version 10, and calculations were manually verified.
Results
Patient population
Based on the results of our admissions database query, we identified 229 patients who were scheduled for or who underwent a Ladd procedure. Of these, 63 were excluded from the study: 47 had no UGI series performed, 3 had omphalocele, 9 with gastroschisis had obligate malrotation, 1 had no Ladd procedure performed (a syndromic girl who had too many other medical problems to risk abdominal surgery), 2 were 21 years or older, and 1 had no data available. The remaining cohort consisted of 166 patients (Table 1), of whom 59% were male and 41% were female, 40% were neonates (the peak age for malrotation with volvulus), and 74% were infants younger than 1 year. Their median age at the time of the UGI examination was 67 days (mean age 2.4 years, range newborn to 19 years).
Prior abdominal surgery and associated anomalies
Five patients had prior abdominal surgery (one Nissen fundoplication, one umbilical hernia repair, two appendectomies, and two gastrostomy tube placements). All five had true-positive UGI examinations for malrotation and were true-negative for volvulus (Table 2).
A number of patients had congenital anomalies or syndromes: seven had Down syndrome (one had both Down syndrome and duodenal atresia); six had heterotaxy syndrome (three dextrocardia, three dextrogastria); four had situs inversus; five had duodenal atresia; duodenal web or annular pancreas (one had both duodenal atresia and annular pancreas); and one each with Cornelia de Lange syndrome, Meckel diverticulum, cystic fibrosis, and prune belly syndrome. In the patient with Meckel diverticulum the UGI study result was false-negative for malrotation. All other patients with these congenital syndromes were accurately diagnosed for malrotation and/or volvulus (Table 3).
Clinical presentations
The most frequent presenting symptom was emesis of any type, at 59%. Bilious emesis was present in 31% of the patients and was seen most frequently in neonates (37 of 66 neonates, 56%). Feeding intolerance and abdominal pain were the second and third most frequent presenting symptoms, at 27% and 15%, respectively (Table 4).
UGI series
Of the 166 patients, 115 had UGI examinations performed at our institution and 51 had UGI studies at outside hospitals that were reviewed and recorded in the medical records. All UGI results were combined to provide a pooled analysis of the 166 children included in this study. Based on surgical reports, 163/166 (98%) patients were found to have malrotation and 38/166 (23%) had volvulus at the time of surgery.
At our institution, there were 7/115 (6%) false-negative and 1/115 (1%) false-positive UGI study interpretations. Among the 51 examinations performed at outside hospitals, there were no false-negative interpretations and one (2%) false-positive interpretation. Overall, there were 156/163 (96%) true-positive, 7/163 (4%) false-negative, and 2/163 (1%) false-positive UGI study interpretations for malrotation (Table 5). Of the seven false-negative studies, five (71%) were in children after the neonatal age (Table 6). Of the false-positive studies, one was in a neonate and one in an older infant. The sensitivity of the UGI series to correctly diagnose malrotation both overall and at our institution was 96%.
The UGI series reports were reviewed for the presence of individual signs that suggested malrotation (Table 7). The UGI series showed the DJJ not left of the left pedicle in 54 of the 166 patients (33%; all true-positive for malrotation), a low position of the DJJ in 23 patients (14%; 1 false-positive for malrotation), a displaceable DJJ position in 4 patients (2%; all true-positive for malrotation), a corkscrew/spiraling duodenum in 19 patients (11%; all true-positive for malrotation), duodenal distention in 13 patients (8%; all true-positive for malrotation), duodenal redundancy in 14 patients (8%; 11 true-positive, 1 false-positive and 2 false-negative for malrotation), and gastroesophageal reflux in 40 patients (24%). In 30 patients (18%) the cecal position on delayed films after the UGI series was reported, and was considered abnormal in 26 of the 30 (87%). In 62 patients (37%) an abnormal location of the jejunum was reported. The jejunum was on the right in 56 of the 62 patients (2 false-positive for malrotation), and was abnormally positioned on the left in 6 with heterotaxy syndrome (all 6 true-positive for malrotation).
False-negative results
There were seven patients with a false-negative UGI study result. These patients had anatomy that overlapped with normal anatomy or variants: 2 (29%) had duodenal redundancy and 3 (43%) had a normal position of the jejunum in the left abdomen, and yet 6 (86%) had the jejunum in the left abdomen on review of the images (Table 8). Two studies showed an abnormality with distal small-bowel distention but no malrotation. Cecal position was not reported in these examinations. No other abnormalities were reported for these seven UGI examinations. On review of the UGI images in these seven patients false-negative for malrotation, three had normal lateral views, although these images were both oblique lateral rather than true lateral position. Four had no lateral view on the UGI study.
The following three case reports demonstrate some of the difficulties in differentiating normal anatomic variants from malrotation.
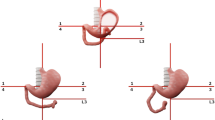
Images from the UGI series in an 11-month-old boy showed a subtle redundant course of the duodenum to the right of the spine prior to its course toward the left upper quadrant (Fig. 1). The appearance of the duodenum was similar to that seen in duodenum inversum. A subsequent lateral image in this study showed a normal ascending duodenum and DJJ at the level of the duodenal bulb (Fig. 1). This study was interpreted as normal, although malrotation and volvulus were found at surgery.
False-negative UGI series in an 11-month-old boy with abdominal distention and bilious emesis. a Frontal image demonstrates barium passing through the duodenum and a subtle redundant course of the duodenum to the right of the spine prior to its expected course toward the left upper quadrant. Barium was injected through a nasogastric tube with its tip located in the duodenal bulb. There are dilated small bowel loops in the left upper quadrant. b Lateral image shows barium ascending in a mildly anteriorly positioned posterior fourth duodenal segment, as expected. Malrotation and volvulus were found at surgery
Images from the UGI series in a 14-year-old boy with Down syndrome showed a redundant duodenum (Fig. 2). The duodenum appeared to be in the right upper quadrant; however, the DJJ was interpreted to be in the normal position and the study was read as negative. Surgical findings revealed a right paraduodenal internal hernia and malrotation.
False-negative UGI series in a 14-year-old boy with Down syndrome, air swallowing and nonbilious emesis. a, b Oblique lateral images demonstrate a redundant duodenum with a subtly abnormal course. Neither the duodenal descent nor the ascent (a) is parallel to the spine. c Subsequent frontal image demonstrates the majority of the duodenum and proximal small bowel in the right upper quadrant prior to crossing over to the left upper abdomen. Malrotation with a right paraduodenal internal hernia was found at surgery
UGI images from the UGI series in a 2-week-old girl showed a normal course of the duodenum and DJJ on the first few views (Fig. 3), mimicking normal anatomy. However, the duodenum was distended with barium and the more distal bowel was air-distended. Malrotation with volvulus, a partially formed ligament of Treitz and a malpositioned cecum in the left upper quadrant were found at surgery.
False-negative UGI series in a 2-week-old girl with nonbilious emesis. The study was performed by injecting barium through a nasogastric tube. The initial lateral view (a) and subsequent AP and lateral views (b, c) show an apparently normal position of the duodenum and DJJ. However, the duodenum is dilated and the adjacent bowel is markedly air-distended. At surgery, the baby had malrotation with volvulus, with a partially formed ligament of Treitz, and the cecum was located in the left upper quadrant
False-positive results
There were two patients with a false-positive UGI study result. Both patients had a redundant duodenum, which in one patient was also noted on the surgical report. Both patients had the jejunum on the right, which is an associated but nondiagnostic sign in malrotation. One of the patients had stomach distention creating a low DJJ, demonstrating how adjacent bowel distention can displace the DJJ because of lax peritoneal ligaments in children younger than 4 years (Fig. 4). Reviewing the UGI images in these two patients false-positive for malrotation, one had no lateral view and one had a normal lateral view.
False-positive UGI series in a 5-month-old boy with feeding intolerance demonstrates how the distended stomach displaces the DJJ in children younger than 4 years. The frontal view (a) appears to be positive, with a low and somewhat rightward position of the DJJ, whereas the lateral view (b) demonstrates a normal posterior descent and then more anterior ascent of the distal duodenum. Surgical exploration revealed a normal bowel position
Volvulus
There were overall eight false-negative and two false-positive UGI studies for volvulus. Of 51 UGI series performed at outside hospitals, 4 (8%) were false-negative and none was false-positive. Of 115 UGI series performed at our institution, 4 (3%) were false-negative and 2 (2%) were false-positive. Overall, of 38 patients with volvulus, 30 (79%) had a true-positive UGI study result and 8 (21%) had a false-negative UGI study result, and of 128 patients without volvulus, 2 (2%) had a false-positive UGI study result. The overall sensitivity for detecting volvulus on the UGI series at this institution was 79%.
Surgical management and outcomes
Of the 166 patients, 5 (3%), all neonates, required bowel resection, and 4 of these 5 had a true-positive UGI study result and 1 a false-negative result. Two neonates and one older infant died (3/166, 2%); all had a true-positive UGI study result. No bowel perforations were reported.
Discussion
The sensitivities of the UGI series during a recent 9-year period were 96% for detecting malrotation and 79% for detecting volvulus. These results are consistent with the sensitivities of the UGI series reported in the literature: 93% [3, 9], 95% [1, 3], and 100% [3, 10] for the diagnosis of malrotation, and 54% for the diagnosis of midgut volvulus [3, 10]. In patients with an equivocal diagnosis or in whom diagnosis is challenging there is often difficulty in distinguishing anatomic normal variants from malrotation [2, 3, 11], and the necessity for meticulous technique in acquiring and interpreting the UGI series to accurately differentiate normal anatomic variants from disease has been recently emphasized [2, 3]. Improvements in technique have helped reduce the mortality of affected newborns, which has improved from 30% in the 1950s and 1960s to 3–5% more recently [3, 8, 12–15].
It is also important to note that malrotation of the bowel is associated with a number of syndromes and anatomic anomalies [3, 7, 16]. It is always present in children with omphalocele, gastroschisis or congenital diaphragmatic hernia, in whom a disruption of the normal positioning of the developing gut occurs during fetal development. Malrotation occurs fairly often in association with other gastrointestinal abnormalities, especially jejunal and duodenal stenosis or atresia, annular pancreas and Hirschsprung disease (congenital megacolon). Malrotation is also very common in children with heterotaxy syndrome [17].
Strengths
This study represents a large descriptive series of children who underwent a Ladd procedure for malrotation after UGI series. Review of these patients allowed us to consider helpful findings and common errors in false-negative and false-positive findings to better understand why these misinterpretations arise. These difficult cases provide additional examples to assist in improving the performance and interpretation of the UGI series. It is reassuring to find that the sensitivity of the upper GI series in this study was consistent with that reported in the literature. The majority of patients in whom the diagnosis was missed had a subtle abnormality in the course of the duodenum that was often interpreted as a normal variation, which is also consistent with reports in the literature [2, 3, 11].
Meticulous evaluation of the first pass of barium through the duodenum is essential to document the DJJ position. The initial true lateral view of the entire duodenum is of particular importance in this regard. A normal duodenum on the lateral view demonstrates caudal descent of the second segment parallel to the spine, accompanied by ascent of the forth segment, slightly anterior to the descending duodenum. If the duodenum angles ventrally at its most caudal point on the lateral view, it is leaving the retroperitoneum and therefore is considered abnormal [18].
Of interest, the two patients with a false-positive UGI study had the jejunum on the right, which might be an important pitfall in overdiagnosing malrotation when this finding is not accompanied by duodenal abnormalities on the UGI series. Conversely, in six of the seven patients with a false-negative study the jejunum was demonstrated or reported to be located on the left side, which might have falsely reassured the radiologist that there was no malrotation. Katz et al. [19] noted that the jejunum was located in the right upper abdomen in 1 of 43 children (2%) with a normal UGI study versus 23 of 35 (66%) with a UGI study indicating malrotation. The rarity of right-side jejunum in normal individuals and its common appearance in patients with malrotation make the interpretation of the UGI study difficult in subtle or complex situations. If the findings of a UGI study are unclear, it might be helpful to perform a small-bowel follow-through or contrast enema to document the cecal position or, when possible, repeat the UGI study on a subsequent day.
Volvulus can be an intermittent phenomenon, as is suggested by our results. The UGI studies had both false-positive and false-negative results with a sensitivity of 79% for this diagnosis, and the literature reports a sensitivity of 54% [3]. These results therefore are not surprising and remind us of the limitations of comparing imaging with surgical findings.
Limitations and suggestions for further research
Our study had several limitations. Our evaluation of the nuances of the UGI series and operative reports was restricted because it was retrospective, which introduces selection bias. The number of UGI studies performed to exclude the diagnosis of malrotation was not known and was likely a large number. We limited the study to only those UGI series in children who underwent a Ladd procedure, our gold standard. This greatly diminished the number of studies with a true-negative result and likely artificially decreased the number with a false-positive result.
The UGI series in this study have not been prospectively interpreted using the criteria identified by Katz et al. [19]; however, this is planned. Katz and colleagues identified nine criteria on UGI examinations to aid in distinguishing normal from malrotation and abnormal positioning of the duodenum and proximal jejunum. A control group of 43 patients (neonate to 17 years old) were studied by UGI series to determine the position of key duodenal landmarks and the mobility of the duodenojejunal flexure with manual displacement. These results were compared with the duodenal positions of 35 children of similar ages with surgically confirmed malrotation. Nine criteria were identified as a useful means of detecting subtle abnormalities of duodenal position. The normal duodenojejunal flexure was found to be readily displaceable in neonates and could be pushed to the right of the spine in more than two-thirds of patients younger than 4 months. In those older than 4 years, mobility was very limited. In their study, the presence of three or more of the nine criteria indicated malrotation, the presence of two criteria was equivocal, and the presence of one criterion was likely normal, providing the cecum location was also normal. In our study, the two patients with a false-positive result had only one and two of the Katz criteria, respectively, and therefore would not have been considered positive by these criteria. On the prospective UGI reports, the seven patients with a false-negative result had only two criteria in the UGI reports; yet the images have not been reviewed to verify the value of these criteria. Applying the Katz criteria to the findings in these patients might provide additional insight as to why the cases were misinterpreted.
Duodenal redundancy is cited in the literature as a subtle sign of malrotation that overlaps with normal variation [11]. It was documented in 14 of 166 patients in our study, in 11 of whom the result was true-positive, yet the incidence of duodenal redundancy in normal patients is not known. Excluding nonoperative cases from our study eliminated the possibility of studying the incidence of duodenal redundancy in normal patients. We recommend investigating the incidence of duodenal redundancy, including its course on the true lateral view as well as jejunal position, in future research.
Conclusion
The conclusions from our study are not new, but confirm what is taught to many radiologists and clinicians. In a small but troubling percentage of patients with malrotation the anatomy may overlap with normal variant anatomy. A normal UGI series should include a true lateral view to document the retroperitoneal position of the third and fourth portions of the duodenum. A jejunum located in the right abdomen might lead to a false-positive interpretation and when located in the left abdomen might lead to a false-negative result. Meticulous technique is essential to the successful interpretation of a UGI study. When the results are equivocal, consider either repeating the UGI series or performing a small-bowel follow-through or a contrast enema to document cecal position in order to avoid delay in diagnosis of malrotation or unnecessary laparotomy in children with normal anatomy.
References
Torres A, Ziegler M (1993) Malrotation of the intestine. World J Surg 17:326–331
Strouse P (2004) Disorders of intestinal rotation and fixation (“malrotation”). Pediatr Radiol 34:837–851
Applegate KE, Anderson JM, Klatte EC (2006) Intestinal malrotation in children: a problem-solving approach to the upper gastrointestinal series. Radiographics 26:1485–1500
Orzech N, Navarro O, Langer J (2006) Is ultrasonography a good screening test for intestinal malrotation? J Pediatr Surg 41:1005–1009
Millar A, Rode H, Brown R et al (1987) The deadly vomit: malrotation and midgut volvulus. Pediatr Surg Int 2:172–176
Spigland N, Brandt M, Yazbeck S (1990) Malrotation presenting beyond the neonatal period. J Pediatr Surg 25:1139–1142
Jamieson D, Stringer DA (2000) Small bowel. In: Babyn P (ed) Pediatric gastrointestinal imaging and intervention. Decker, Hamilton, Ontario, pp 311–332
Bonadio WA, Clarkson T, Naus J (1991) The clinical features of children with malrotation of the intestine. Pediatr Emerg Care 7:348–349
Lin J, Lou C, Wang K (1995) Intestinal malrotation and midgut volvulus: a 15-year review. J Formos Med Assoc 94:178–181
Seashore J, Touloukian R (1994) Midgut volvulus. An ever-present threat. Arch Pediatr Adolesc Med 148:43–46
Long F, Kramer S, Markowitz R et al (1996) Intestinal malrotation in children: tutorial on radiographic diagnosis in difficult cases. Radiology 198:775–780
Rescorla F, Shedd F, Grosfeld J et al (1990) Anomalies of intestinal rotation in childhood: analysis of 447 cases. Surgery 108:710–715
Berdon WE, Baker DH, Bull S et al (1970) Midgut malrotation and volvulus. Which films are most helpful? Radiology 96:375–384
Andrassy RJ, Mahour GH (1981) Malrotation of the midgut in infants and children: a 25-year review. Arch Surg 116:158–160
Ford EG, Senac MO Jr, Srikanth MS et al (1992) Malrotation of the intestine in children. Ann Surg 215:172–178
Taybi H, Lachman R (1990) Radiology of syndromes, metabolic disorders, and skeletal dysplasias. Yearbook Medical Publishers, Chicago, IL
Applegate KE, Goske MJ, Pierce G et al (1999) Situs revisited: imaging of the heterotaxy syndrome. Radiographics 19:837–852; discussion 853–834
Koplewitz B, Daneman A (1999) The lateral view: a useful adjunct in the diagnosis of malrotation. Pediatr Radiol 29:144–145
Katz ME, Siegel MJ, Shackelford GD et al (1987) The position and mobility of the duodenum in children. AJR 148:947–951
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sizemore, A.W., Rabbani, K.Z., Ladd, A. et al. Diagnostic performance of the upper gastrointestinal series in the evaluation of children with clinically suspected malrotation. Pediatr Radiol 38, 518–528 (2008). https://doi.org/10.1007/s00247-008-0762-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-008-0762-8