Abstract
Background
Various strategies to mitigate children’s distress during voiding cystourethrography (VCUG) have been described. Sedation with nitrous oxide is comparable to that with oral midazolam for VCUG, but a side-by-side comparison of nitrous oxide sedation and routine care is lacking.
Objective
The effects of sedation/analgesia using 70% nitrous oxide and routine care for VCUG and radionuclide cystography (RNC) were compared.
Materials and methods
A sample of 204 children 4–18 years of age scheduled for VCUG or RNC with sedation or routine care were enrolled in this prospective study. Nitrous oxide/oxygen (70%/30%) was administered during urethral catheterization to children in the sedated group. The outcomes recorded included observed distress using the Brief Behavioral Distress Score, self-reported pain, and time in department.
Results
The study included 204 patients (99 nonsedated, 105 sedated) with a median age of 6.3 years (range 4.0–15.2 years). Distress and pain scores were greater in nonsedated than in sedated patients (P < 0.001). Time in department was longer in the sedated group (90 min vs. 30 min); however, time from entry to catheterization in a non-imaging area accounted for most of the difference. There was no difference in radiologic imaging time.
Conclusion
Sedation with nitrous oxide is effective in reducing distress and pain during catheterization for VCUG or RNC in children.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Distress experienced by children during voiding cystourethrography (VCUG) and radionuclide cystography (RNC) is well documented despite the short-lived nature of the procedures [1–4]. Various strategies have been investigated to mitigate the distress caused by VCUG and RNC. Midazolam, for example, limits distress without compromising the imaging quality of the study [5–7]. However, in one investigation, midazolam resulted in significant behavioral side effects including anger, physical aggression, and inconsolability in 12% of children undergoing VCUG [7]. In addition, the variable time of onset (between 10 and 30 min for oral or nasal administration) and duration of action (60–90 min) match poorly with the limited duration of a typical VCUG study [8, 9]. Deeper sedatives such as propofol can affect the test results, as children are less likely to void to completion [10]. Other reported methods of reducing distress during VCUG include introduction of the procedure with a story booklet [11], formatted play preparation [12], complete procedural review coupled with distraction [13], and hypnosis [14]. These interventions are of variable success in limiting distress, and in the case of hypnosis require an additional pretest visit.
Nitrous oxide as an inhalational agent has attractive properties for limiting distress in children by providing analgesia, anxiolysis, and amnesia. It has a predictable rapid onset of action within 5 min of initiation of inhalation with return to baseline function within 5 min of discontinuation [8, 15]. Nitrous oxide has an excellent safety record in alleviating childhood pain and anxiety during dental procedures as well as a variety of medical interventions [16–21]. Two preliminary studies suggest that nitrous oxide as a 50% mixture with oxygen is efficacious in partially limiting the distress of VCUG in children [22, 23]. Additional studies have demonstrated that nitrous oxide can be delivered safely in concentrations up to 70% by appropriately trained nursing personnel [24, 25].
The purpose of this prospective study was to evaluate the effect of sedation/analgesia on observed and perceived distress and pain, using 70% nitrous oxide compared to routine care for VCUG and RNC procedures. If nitrous oxide administered by appropriately trained nursing personnel can effectively and predictably minimize distress in children and not compromise image quality, the agent might become more widely accepted for use during VCUG and RNC.
Materials and methods
The study was conducted in the radiology department of a children’s hospital. Children 4–18 years of age who were scheduled for VCUG or RNC between November 2004 and May 2005 were eligible for the study. Children younger than 4 years were excluded to enhance the accuracy of the subjective measures (see below). At our facility, VCUG and RNC are routinely performed without sedation unless otherwise specified by the ordering physician. Thus, patients were stratified into two groups prior to presentation in the department, group 1 scheduled for sedation (sedated group), and group 2 scheduled for routine care (nonsedated group). A single investigator recruited a sample of eligible patients from each group. Patients were enrolled after the consent of the caregiver and assent of the patient, when deemed appropriate, had been obtained. Written consent was obtained prior to entry into sedation or imaging area. The Institutional Review Board of Children’s Hospitals and Clinics of Minnesota approved this study.
Patients in the nitrous oxide sedated group were assessed for specific contraindications to nitrous oxide (e.g., recent craniotomy, pneumothorax, bowel obstruction). Nitrous oxide was administered by nurses experienced in deep sedation monitoring who received additional training (including didactic and participatory sessions) in nitrous oxide administration. This training met educational requirements prescribed for state licensure of dentists and dental hygienists for nitrous oxide administration. Nitrous oxide/oxygen was administered as a 70%/30% mixture using a continuous flow nitrous oxide/oxygen flowmeter (Porter Instruments, Hatfield, Pa.) until urethral catheterization was complete. Catheterization was performed by a radiology technician. Following catheterization, 100% oxygen was administered for 2–3 min. As per institutional guidelines, patients were monitored with pulse oximetry and direct nursing observation throughout nitrous oxide administration and afterward until the presedation level of alertness had been achieved and discharge criteria met according to the American Academy of Pediatrics guidelines (i.e. cardiovascular and airway patency were satisfactory and stable and protective reflexes intact, patient was easily arousable and could talk and sit up unaided, hydration was adequate) [26]. VCUG or RNC was then performed according to the department protocol. All sedated patients had fasted for at least 4 h before the procedure.
Patients in the nonsedated group underwent VCUG or RNC according to the department protocol.
The Brief Behavioral Distress Score (BBDS) was used to quantify procedure-related distress. The reliability and validity of the BBDS, a total distress score, compared to other behavioral distress scores (Observational Scale of Behavioral Distress), provider estimate of distress, and parent and child self-report of pain were previously established [27]. Prior to the study, potential procedural steps were outlined for both VCUG and RNC (Table 1). All cases were observed by the same investigator to ensure consistency in applying the BBDS. This investigator had direct visualization of each patient throughout the procedure and noted the steps that actually occurred as well as the presence or absence of noninterfering (e.g., crying, verbally seeking physical comfort from another person or object), potentially interfering (e.g., screaming, tightly clenched fists), and/or interfering (e.g., kicking, getting up from the table) distress behaviors at each step. Because of the potential for variability in the number of steps within each group (e.g., a child who required bladder refilling to complete imaging for RNC would have additional steps compared to a child who did not require refilling), the total number of steps that actually occurred during the procedure were summed and used for distress score calculation. As described by Tucker et al. [27], the use of percentage scores supports the comparison of procedures with different numbers of steps. The number of steps in which behaviors from any of the three distress categories occurred were summed and divided by the total number of steps multiplied by three (number of distress categories), then multiplied by 100 to obtain a BBDS score for the procedure [27]. Because sedation was only administered during catheterization, steps were also grouped into those encompassing urethral catheterization (steps 4–6) and the postcatheterization procedure (steps 9–19). BBDS scores were similarly calculated for these portions of the procedure. To ensure that scoring remained consistent during the entire study, a second investigator scored a random selection of ten study patients, resulting in greater than 94% agreement on 540 BBDS scores.
Patients rated pain using the Wong-Baker FACES pain rating scale, a series of six facial expressions assigned a number from 0 (no hurt) to 10 (hurts worst) in even-numbered increments [28]. Previous reports have established the ability of children as young as 4 years to report subjective symptoms while undergoing nitrous oxide sedation [29]. The FACES scale has been used to measure pain before, during, and after nitrous oxide administration for minor pediatric surgical procedures [19]. The pain assessment for this study was done (1) immediately following consent (baseline pain assessment), (2) immediately following the urethral catheterization, and (3) at time of discharge.
Four distinct times were recorded by the investigator: (1) entry into the sedation area for VCUG-sedated and RNC-sedated groups, the nuclear medicine area for the RNC nonsedated group, or the fluoroscopy suite for the VCUG nonsedated group, (2) urethral catheterization, (3) the start of bladder emptying in the imaging area prior to initial instillation of contrast agent or radionuclide for each procedure, and (4) the time of discharge. The investigator also noted adverse events associated with the sedation or the procedure.
Analysis
The two-sided Pearson chi-squared or the Fisher exact test was used to test the significance of differences in the percentage of male patients between the sedated and nonsedated groups. The latter test was used when cell entries did not meet the requirements of the chi-squared test. The two-sided Mann-Whitney U test was used to test for significant differences in median values between the sedated and nonsedated groups including age, BBDS and pain scores, and procedure times. The nonparametric method was selected because of the non-normal distribution of the data determined with the Shapiro-Wilk test. P=values < 0.05 were considered significant. All statistical analyses were done using SPSS version 11.5 (SPSS, Chicago, Ill.).
Results
Demographics
During the 6-month study period, 1,011 patients were scheduled for either VCUG (562 patients) or RNC (449 patients) in the radiology department. Of those scheduled, 389 met study criteria based on age (191 VCUG, 198 RNC). Written consent was obtained for 214 patients (107 nonsedated, 107 sedated). Eight patients in the routine-care (nonsedated) group were excluded from analysis because of failure to complete the procedure (two RNC, six VCUG). Two patients enrolled in the VCUG sedated group were found to have failed testing without sedation in the 2 weeks prior to the study because of extreme distress and were excluded from analysis. Data from the remaining 204 patients (99 nonsedated, 105 sedated) were analyzed. There were no significant differences in age or gender between the sedated and nonsedated groups within the VCUG, RNC, or all-patient categories (Table 2).
Observed distress
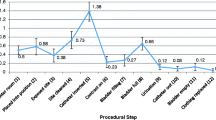
Overall, children in the sedated group undergoing urethral catheterization exhibited significantly less distress behavior (P<0.001) according to the BBDS score than children in the nonsedated group (Fig. 1 and Table 3). The difference in BBDS score between the sedated and nonsedated groups was significant for children undergoing VCUG, but not for children undergoing RNC. During the procedure steps associated with catheter placement (steps 4–6), the sedated group experienced significantly less distress (P<0.001) regardless of the test being performed. There were no differences in distress between the sedated and nonsedated groups for procedure steps 9–19 (postcatheterization). Comparison of distress scores between nonsedated VCUG patients and nonsedated RNC patients and between sedated VCUG patients and sedated RNC patients yielded no statistically significant difference.
Pain scores
All children in the sedated group remained at a level of minimal sedation, able to appropriately respond to verbal conversation. Self-reported pain scores were significantly higher (P < 0.001) immediately after catheterization in all nonsedated children than in sedated children (Table 4 and Fig. 2). There were no significant differences between the groups in pain scores at baseline or at time of discharge from the radiology department (Table 4).
Time in department
Median times for segments of the procedure are shown in Table 5. The overall procedure time was significantly longer for the sedated group regardless of procedure (median 90 min for sedated vs. 30 min for nonsedated patients). Time from entry to catheter placement (median 47 min for sedated vs. 9 min for nonsedated patients) accounted for most of this time difference. The 12-min difference between the median time from catheterization to discharge for sedated patients (32 min) vs. nonsedated patients (20 min) included sedation recovery time plus time required to move patients from the sedation area to the imaging suite. There was no difference in radiologic imaging time (bladder emptying to discharge) between groups.
Adverse events
One patient (1%) in the sedated group experienced nausea. No patients were noted to have vomiting, oxygen desaturation below 92%, airway obstruction or apnea.
Discussion
This study demonstrates that the pain and distress caused by catheterization during VCUG and RNC can in large part be extinguished by sedation with a 70%/30% mixture of nitrous oxide and oxygen which can be administered by specifically trained nurses. Our findings are consistent with those of prior investigators who demonstrated that discomfort in children during VCUG is suppressed by sedation with a 50% nitrous oxide mixture. One study in children older than 5 years undergoing VCUG demonstrated that sedation with 50% nitrous oxide provides pain relief in girls but not in boys [22]. In a recent study comparing oral midazolam with 50% nitrous oxide among children older than 3 years undergoing VCUG, pain and anxiety scores measured by observers were comparable with the two agents [23]. This study, however, was limited by the lack of a nonsedated control group. Our study builds upon these prior investigations by demonstrating that sedation with a 70% nitrous oxide mixture not only decreases observational distress scores but also decreases self-reported pain in children undergoing VCUG and RNC studies compared to those receiving no sedation for the procedures.
No significant adverse effects were observed during this study. One child experienced nausea (1%) but none contended with vomiting. A similar safety profile emerges from a review of the published literature on the use of nitrous oxide in pediatric dentistry as well as during an array of medical procedures including laceration repair, dressing changes, venous cannulation, lumbar puncture, bone marrow biopsy, bronchoscopy, otomicroscopic examination, and gastrointestinal endoscopy [16–25]. The largest published series of pediatric procedures performed with 50% nitrous oxide (7,511 sedations) noted an incidence of major adverse events (e.g., oxygen desaturation, over-sedation) of 0–0.8% and minor adverse events (e.g., nausea, vomiting) in 1.8–6.4%, depending upon procedure and concomitant use of psychotropic medications [30]. Although our study had fewer patients, the low incidence of adverse effects demonstrated is likely a result of the use of nitrous oxide as a single sedative agent as well as the short administration time required for urethral catheterization compared with other procedures such as wound suturing or incision and drainage.
Although much of the medical literature describes experience with the use of 50% nitrous oxide for pediatric sedation, we chose to use 70% nitrous oxide and 30% oxygen for this study. The premixed 50% nitrous oxide/50% oxygen system that is commercially available for medical sedation incorporates a demand valve that must be overcome to initiate gas flow. This system requires a degree of cooperation that limits its recommended use to children older than 4 years [8]. Although this study was limited to children older than 4 years, our department serves a significant number of younger children. The nitrous oxide system used for this study delivers a continuous flow of gas with the ability to titrate nitrous oxide from 0% to 70% with the remainder of the gas as oxygen. A scavenging system that eliminates nitrous oxide to minimize environmental exposure is an integral part of this nitrous oxide delivery system. Based on literature review and conversations with pediatric dental colleagues who use this system on a regular basis, it was originally anticipated that 70% nitrous oxide would be most useful for the younger, more uncooperative toddler-age patients [31]. However, this study and others [24, 25] substantiate the notion that 70% nitrous oxide is effective for older children with few side effects. Despite sedation with 70% nitrous oxide, all of the children remained able to appropriately respond to verbal conversation, corresponding to a level of minimal sedation.
This study also demonstrates that nitrous oxide can be utilized within a radiology department without disrupting patient flow. Although the total time required to perform VCUG and RNC was longer in the sedated group, the difference in time cost was primarily during the preprocedure period. On average for all procedures, the nitrous group required 47 min for entry to catheter placement versus 9 min for the nonsedated group. This time difference is somewhat artificial, however, as our scheduling template for sedated procedures, which allows for 1 h of presedation time, was originally developed based on nursing time requirements for patients receiving oral sedatives. Before the availability of nitrous oxide sedation, urologic imaging scheduled with sedation at our institution was performed with oral midazolam, which requires 10–30 min for onset of action. For this study, patient/family communication, patient presedation assessment, and catheterization all took place during this interval in an area within the radiology department but not in the actual fluoroscopy or nuclear medicine suites, freeing these areas for other patients. The rapid recovery from nitrous oxide sedation allowed patients to achieve discharge criteria and transfer to the imaging suite expeditiously. Because oral midazolam has a half-life that exceeds the time required for imaging, nursing time previously required for monitoring of midazolam-sedated patients during and after imaging is now freed for other sedation duties, improving efficiency in the department. Since equipment costs are nominal (the cost of one nitrous oxide flowmeter with scavenging system is less than half that of our standard hospital monitor or intravenous infusion pump), this increased efficiency translates to reduced cost compared to midazolam sedation. Additionally, 70% nitrous oxide facilitates scheduling because of its predictable rapid onset of action and by virtually eliminating procedure failures caused by patient distress. Although not formally studied, our impression in speaking with our radiology colleagues is that the overall impact of nitrous oxide on the radiology department is positive.
There are limitations to this study. Although children in both groups received preprocedure education, the children in the sedated group were given additional attention by pediatric nurses in a sedation area that is perhaps less threatening than the fluoroscopy or nuclear medicine suites. This individualized attention, including encouragement to play with the nitrous oxide mask prior to sedation, may have made the entire experience, including the urethral catheterization, less distressing.
Another limitation to the study is the lack of randomization to sedated and non-sedated groups. At this institution, the decision to order VCUG or RNC with or without sedation rests with the patient’s primary physician and is scheduled accordingly. Based on prestudy discussions with parents, families arriving with the expectation that their child would be sedated for the test would be unlikely to participate in a randomized study with a non-sedation arm. Children scheduled for testing without sedation were unlikely to meet institutional fasting guidelines for sedation. With the anticipated difficulty of enrolling patients in a randomized study, a convenience sample of patients scheduled for either routine care or sedation was chosen. Although this study design invites selection bias at the level of the ordering physician, it is possible that bias would be skewed toward ordering sedation for the more anxious patients (or parents). If this is the case, distress scores might be expected to be higher rather than lower for the sedated patients. Conversely, the knowledge that their child will receive sedation may make parents less anxious, potentially lowering distress scores as a result. It should also be noted that the child, the parent(s), and the investigator observing the patient behaviors were not blinded to the treatment group.
Conclusions
Sedation with nitrous oxide delivered by nurses with specific training in deep sedation monitoring and nitrous oxide administration is safe and effective in reducing observed distress and self-reported pain during catheterization in children undergoing VCUG or RNC. Although the use of sedation increased the total procedure time, the time spent in either the fluoroscopy or nuclear medicine areas did not differ, and throughput of patients in radiology was not compromised. Areas fertile for investigation include the impact of nitrous oxide administration on the incidence of failed VCUG or RNC resulting from patient anxiety and the potential use of the agent for other diagnostic and/or therapeutic procedures in the radiology department.
References
Stashinko EE, Goldberger J (1998) Test or trauma? The voiding cystourethrogram experience of young children. Issues Compr Pediatr Nurs 21:85–96
Phillips D, Watson AR, Collier J (1996) Distress and radiological investigations of the urinary tract in children. Eur J Pediatr 155:684–687
Merritt KA, Ornstein PA, Spicker B (1994) Children’s memory for a salient medical procedure: implications for testimony. Pediatrics 94:17–23
Elder JS (2005) Imaging for vesicoureteral reflux – is there a better way? J Urol 174:7–8
Akil I, Ozkol M, Ikizoglu OY et al (2005) Premedication during micturating cystourethrogram to achieve sedation and anxiolysis. Pediatr Nephrol 20:1106–1110
Stokland E, Andréasson S, Jacobsson B et al (2003) Sedation with midazolam for voiding cystourethrography in children: a randomised double-blind study. Pediatr Radiol 33:247–249
Elder JS, Longenecker R (1995) Premedication with oral midazolam for voiding cystourethrography in children: safety and efficacy. AJR 164:1229–1232
Krauss B, Green SM (2000) Sedation and analgesia for procedures in children. N Engl J Med 342:938–945
Jones RD, Visram AR, Kornberg JP et al (1994) Premedication with oral midazolam in children: an assessment of psychomotor function, anxiolysis, sedation and pharmacokinetics. Anaesth Intensive Care 22:539–544
Merguerian PA, Corbett ST, Cravero J (2006) Voiding ability using propofol sedation in children undergoing voiding cystourethrograms: a retrospective analysis. J Urol 176:299–302
Zelikovsky N, Rodrigue JR, Gidycz CA et al (2000) Cognitive behavioral and behavioral interventions help young children cope during a voiding cystourethrogram. J Pediatr Psychol 25:535–543
Phillips DA, Watson AR, MacKinlay D (1998) Distress and the micturating cystourethrogram: does preparation help? Acta Paediatr 87:175–179
Salmon K, McGuigan F, Pereira JK (2006) Brief report: optimizing children’s memory and management of an invasive medical procedure: the influence of procedural narration and distraction. J Pediatr Psychol 31:522–527
Butler LD, Symons BK, Henderson SL et al (2005) Hypnosis reduces distress and duration of an invasive medical procedure for children. Pediatrics 115:e77–e85
Webb MD, Moore PA (2002) Sedation for pediatric dental patients. Dent Clin North Am 46:803–814
Michaud L, Gottrand F, Ganga-Zandzou PS et al (1999) Nitrous oxide sedation in pediatric patients undergoing gastrointestinal endoscopy. J Pediatr Gastroenterol Nutr 28:310–314
Annequin D, Carbajal R, Chauvin P et al (2000) Fixed 50% nitrous oxide oxygen mixture for painful procedures: a French survey. Pediatrics 105:e47
Luhmann JD, Kennedy RM, Porter FL et al (2001) A randomized clinical trial of continuous-flow nitrous oxide and midazolam for sedation of young children during laceration repair. Ann Emerg Med 37:20–27
Burnweit C, Diana-Zerpa JA, Nahmad MH et al (2004) Nitrous oxide analgesia for minor pediatric surgical procedures: an effective alternative to conscious sedation? J Pediatr Surg 39:495–499
Fauroux B, Onody P, Gall O et al (2004) The efficacy of premixed nitrous oxide and oxygen for fiberoptic bronchoscopy in pediatric patients: a randomized, double-blind, controlled study. Chest 125:315–321
Fishman G, Botzer E, Marouani N et al (2005) Nitrous oxide-oxygen inhalation for outpatient otologic examination and minor procedures performed on the uncooperative child. Int J Pediatr Otorhinolaryngol 69:501–504
Schmit P, Sfez M (1997) Management of anxious and painful manifestations in pediatric uroradiology. J Radiol 78:367–372
Keidan I, Zaslansky R, Weinberg M et al (2005) Sedation during voiding cystourethrography: comparison of the efficacy and safety of using oral midazolam and continuous flow nitrous oxide. J Urol 174:1598–1600
Kanagasundaram SA, Lane LJ, Cavalletto BP et al (2001) Efficacy and safety of nitrous oxide in alleviating pain and anxiety during painful procedures. Arch Dis Child 84:492–495
Frampton A, Browne GJ, Lam LT et al (2003) Nurse administered relative analgesia using high concentration nitrous oxide to facilitate minor procedures in children in an emergency department. Emerg Med J 20:410–413
American Academy of Pediatrics Committee on Drugs (1992) Guidelines for monitoring and management of pediatric patients during and after sedation for diagnostic and therapeutic procedures. Pediatrics 89:1110–1115
Tucker CL, Slifer KJ, Dahlquist LM (2001) Reliability and validity of the brief behavioral distress scale: a measure of children’s distress during invasive medical procedures. J Pediatr Psychol 26:513–523
Wong DL, Baker CM (1988) Pain in children: comparison of assessment scales. Pediatr Nurs 14:9–17
Houpt MI, Limb R, Livingston RL (2004) Clinical effects of nitrous oxide conscious sedation in children. Pediatr Dent 26:29–36
Gall O, Annequin D, Benoit G et al (2001) Adverse events of premixed nitrous oxide and oxygen for procedural sedation in children. Lancet 358:1514–1515
Wilson S (2000) Pharmacologic behavior management for pediatric dental treatment. Pediatr Clin North Am 47:1159–1175
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zier, J.L., Kvam, K.A., Kurachek, S.C. et al. Sedation with nitrous oxide compared with no sedation during catheterization for urologic imaging in children. Pediatr Radiol 37, 678–684 (2007). https://doi.org/10.1007/s00247-007-0508-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-007-0508-z