Abstract
Background: Nasal continuous positive airway pressure (CPAP) has been used since 1975 as the initial treatment for respiratory distress syndrome (RDS) in very premature infants. Gaseous distention of the abdomen (CPAP belly) is a common secondary effect of CPAP. Gaseous distention of the hypopharynx is also common. Objective: To determine the incidence of hypopharyngeal distention in infants on CPAP. Materials and methods: We performed a retrospective review of the chest radiographs of 57 premature infants treated with CPAP during a 4-week period to find the presence and degree of hypopharyngeal distention. Results: Of the 57 radiographs, 14 (25%) revealed gaseous distention of the hypopharynx and/or cervical esophagus. On occasion, this raised concern for pharyngeal perforation or esophageal atresia. Conclusion: Awareness that CPAP-related hypopharyngeal distention is common should help radiologists avoid erroneous consideration of esophageal atresia or hypopharyngeal perforation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Continuous positive airway pressure (CPAP) given at delivery to premature infants can prevent progression of respiratory distress syndrome (RDS) to respiratory failure. Given through nasal prongs, CPAP is thought to improve the survival of premature infants requiring respiratory support while decreasing the incidence of lung damage (chronic lung disease of prematurity) associated with endotracheal intubation. The use of CPAP helps to lessen the subsequent need for intubation and surfactant therapy. CPAP has been used as the first mode of treatment in spontaneously breathing infants at our institution since 1975 [1, 2].
Abdominal distention secondary to aerophagia in infants on CPAP (CPAP belly) has been reported from our institution [3]. In our experience, gaseous distention of the hypopharynx and the cervical esophagus is an equally common radiologic finding in the population of premature infants treated with CPAP. On occasion, it is confused with hypopharyngeal perforation or is a missed diagnosis of esophageal atresia with fistula. We attempted to assess the incidence and various patterns of hypopharyngeal and esophageal distention seen with the use of CPAP in a population of very premature infants treated in our NICU during a 4-week period. The majority of these infants weighed between 500 and 1000 g at birth.
Materials and methods
We retrospectively studied a nonrandomized group of newborn infants who required nasal CPAP in our neonatal intensive care unit during a 4-week period. Of these infants, 57 were imaged with supine chest radiographs while on CPAP. No infants requiring CPAP in the NICU during the 4-week period were excluded from the study. Nasal CPAP was administered via a two-pronged nasal cannula to all infants. A continuous mixture of oxygen and mixed air was provided. Flow rates ranging from 5 to 7 l/min were controlled by a flow meter.
All of the supine chest radiographs obtained during the 4 weeks that the infants were on CPAP were evaluated by one of two experienced pediatric radiologists (P.H., W.B.), a neonatologist (N.A.), and a medical student (M.F.) as either positive or negative for gaseous distention of the hypopharynx and esophagus. If there was confusion about esophageal perforation or esophageal atresia or clinical correlation, i.e., problems with swallowing or nasogastric tube passage, it was noted. Frontal and lateral dedicated radiographs of the neck were rarely needed to differentiate CPAP neck from these other two entities.
IRB approval was not necessary at our institution at the time of the study.
Results
Of the infants treated with nasal CPAP, gaseous distention of the pharynx and cervical esophagus developed in 25% (14/57). Of these14 infants, 10 had been born at less than 28 weeks gestation. Birth weight in this group ranged from 436 to 990 g. The other four infants with positive radiographic findings were between 31 and 32 weeks (1,100–1,800 g).
Of the infants treated with nasal CPAP who did not develop gaseous distention of the neck, 8 of 43 had been born at less than 28 weeks’ gestation. Birth weights in these infants ranged from 560 to 961 g.
Discussion
For three decades, our NICU has used nasal CPAP instead of intubation and surfactant therapy as the initial management of respiratory distress in a population of very low birth weight premature infants or so-called “micropremies” [1, 2].
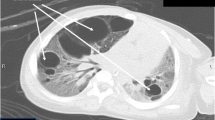
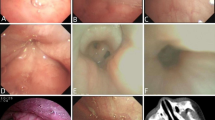
Gaseous distention of the pharynx and esophagus (CPAP neck), though not as common as gaseous distention of the small bowel and colon in infants on CPAP, is a relatively frequent occurrence. Findings range from the usually moderate dilatation (Fig. 1) of the pharynx to dramatic, marked dilatation (Fig. 2). The importance of this finding is the possible confusion with hypopharyngeal perforation, which is a possible complication in this population of sick infants who often have orogastric and nasogastric tubes placed. Gaseous dilatation of the pharynx can also potentially be radiologically confused with a missed diagnosis of esophageal atresia with distal fistula, though clinical confusion rarely occurs.
The distention of the hypopharynx and cervical esophagus can be explained by the closing of the upper esophageal sphincter during image acquisition. The amount of dilatation ranged from minimal to marked. If both esophageal sphincters are open, the gas can dilate the esophagus as it passes into the stomach and distal bowel, where it can lead to CPAP belly. Less commonly, the upper sphincter might be open while the lower sphincter remains closed, leading to distention of the cervical and thoracic esophagus.
Most infants were very premature (birth weights of 400–1,000 g), and one can speculate that these infants have less tone in their pharyngeal musculature because of prematurity. No gaseous distention was seen in a small number of term infants with cardiac disease who were treated with CPAP for a short time after extubation performed during cardiac surgery.
In conclusion, as the use of CPAP increases, radiologists should be aware that gaseous distention of the pharynx and esophagus is a relatively common occurrence in very premature infants on nasal CPAP and should not cause alarm.
References
Wung JT, Driscoll JM Jr, Epstein RA, et al (1975) A new device for CPAP by nasal route. Crit Care Med 3:76–78
Polin RA, Sahni R (2002) Newer experience with CPAP (review). Semin Neonatol 7:379–389
Jaile JC, Levin T, Wung JT, et al (1992) Benign gaseous distention of the bowel in premature infants treated with nasal continuous airway pressure: a study of contributing factors. AJR 158:125–127
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Walor, D., Berdon, W., Anderson, N. et al. Gaseous distention of the hypopharynx and cervical esophagus with nasal CPAP: a mimicker of pharyngeal perforation and esophageal atresia. Pediatr Radiol 35, 1196–1198 (2005). https://doi.org/10.1007/s00247-005-1576-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-005-1576-6