Abstract
Dobutamine stress cardiac magnetic resonance (dsCMR) has demonstrated value in identifying patients at risk for adverse cardiovascular events in adults with coronary artery disease, but its prognostic value in younger patients is unknown. This study sought to evaluate the relationship between dsCMR results and the risk of subsequent cardiovascular events in children. Patients age < 23 years who underwent dsCMR at Boston Children’s Hospital were eligible for inclusion. Patients were excluded if no follow-up data were available after dsCMR or the dsCMR protocol was not completed. Data regarding the presence of inducible regional wall motion abnormalities and subsequent cardiovascular events during follow-up were analyzed. Cardiovascular events included myocardial infarction, surgical or catheter-based coronary artery intervention, and ischemic symptoms. Among 80 dsCMR studies in 64 patients with median age 5.3 years (range 0.5–22.4 years), 3 patients had a positive dsCMR with inducible regional wall motion abnormalities. Over a median follow-up of 7.4 years (IQR 4.0–11.2), 2 of these patients underwent surgical intervention (coronary artery bypass grafting and unroofing of a myocardial bridge) and the third remained asymptomatic with no interventions. Among 61 patients with a negative dsCMR, none experienced myocardial infarction, death, or aborted sudden death. Four underwent cardiac interventions (cardiac transplantation, coronary artery bypass grafting, and unroofing) due to symptoms or catheterization findings. In pediatric patients undergoing dsCMR, wall motion abnormalities indicating inducible ischemia were uncommon. Those with a negative dsCMR were unlikely to experience an adverse cardiac event or undergo a cardiac intervention on medium-term follow-up.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Ischemic cardiac events are rare in the pediatric population but are associated with significant morbidity and mortality. Conditions associated with an increased risk of myocardial ischemia include coronary artery stenosis following Kawasaki disease, a history of surgical coronary artery transfer as part of congenital heart disease repair, and some variants of anomalous origin of the coronary arteries. In at-risk patients, there are several imaging testing options for surveillance and assessment, and the optimal approach has not been established. This limitation is in part because establishing the utility of a test for inducible ischemia is challenging. One approach is to compare the results of a given modality with those from another modality performed at approximately the same time. In this endeavor, it is important to recognize that tests which demonstrate coronary artery anatomy may not be an appropriate reference for those that evaluate for the physiology of reduced myocardial perfusion. An additional approach to evaluating test utility is to examine the relationship of test results to subsequent clinical outcomes over the longer term. This method is particularly valuable for establishing the negative predictive value of a test.
In adults with atherosclerotic coronary heart disease, dobutamine stress cardiac magnetic resonance (dsCMR) has been demonstrated to have a high sensitivity and specificity for identifying inducible ischemia [1, 2] as well as forecasting future cardiovascular adverse events [3,4,5]. For patients with suspected coronary artery disease, performing dsCMR for risk stratification prior to coronary angiography has been shown to improve cost-effectiveness [6]. A previous study from our institution demonstrated that dsCMR is feasible and safe in the pediatric population, and has low interobserver variability [7]. In the intervening years, the number of patients who have undergone dsCMR at our center has increased as has their follow-up duration. Thus, we sought to evaluate the utility of dsCMR by studying the relationship between test results and subsequent coronary events.
Methods
A retrospective database search identified all patients at our center who underwent dsCMR from January 2002 to January 2020. This cohort included the 28 patients described in our prior dsCMR report [7]. As a main study aim was to relate dsCMR results to subsequent outcomes, patients were excluded from this study if they had no clinical follow-up data available after the dsCMR or if the dsCMR imaging protocol was not completed. To limit our analysis to a primarily pediatric population, patients older than 22 years of age were excluded. Medical records and imaging reports were reviewed, and relevant data were abstracted pertaining to demographics and clinical outcome. This study was approved by the Institutional Review Board at Boston Children’s Hospital which waived the requirement for informed consent.
dsCMR was performed on a 1.5 T scanner (Philips Achieva, Philips Medical Systems, Best, the Netherlands) and images were obtained awake or under general anesthesia, depending on patient age and ability to cooperate. The electrocardiogram tracing and pulse oximetry were monitored continuously, and cuff blood pressure measurements were obtained every 2 min during dobutamine stress. The protocol utilized for dsCMR by our institution has been previously described [7]. For the stress portion of the protocol, dobutamine was given at progressively increasing doses (10, 20, 30, and 40 µg/kg/min) with the addition of atropine if needed to achieve the target heart rate (0.85*(220-age)). Wall motion was evaluated according to an established 17-segment model for the left ventricle and 9-segment model for the right ventricle [8].
dsCMR studies were classified as positive if there were inducible regional wall motion abnormalities with dobutamine stress. The subjects’ course following dsCMR was determined through a careful review of their medical records. A coronary event was defined as a myocardial infarction, surgical- or catheter-based coronary artery intervention, or chest pain concerning for ischemia (as determined by the clinician based on further evaluation, such as troponin elevation). Follow-up was censored if heart transplantation occurred.
Results
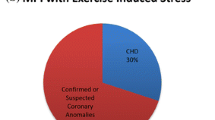
During the study period, 87 dsCMR examinations were performed in 71 patients (Fig. 1). Five patients were excluded from the study because of no available follow-up data (n = 2) or because the imaging protocol was not completed (n = 3). Two patients older than 22 years were excluded from this pediatric cohort; these patients had negative studies and no coronary events during follow-up. Thus, 64 patients (43 male) were included in this study and underwent a total of 80 dsCMR examinations (Table 1). Ten patients underwent 2 dsCMR examinations and 3 patients underwent 3 examinations. General anesthesia was used in 58 of the 80 examinations (73%). Median age at dsCMR was 5.4 years (range 0.5–22.4 years), and the most common clinical indications were Kawasaki disease with aneurysms, transposition of the great arteries status post-arterial switch operation, heart transplantation, and congenital coronary artery anomalies. None of the patients who underwent dsCMR examinations had previously had a catheterization or surgical procedure intended to treat coronary artery obstruction.
Subjects with a Positive dsCMR
Among the 80 dsCMR examinations included, 3 (3.8%) were positive for an inducible regional wall motion abnormality with dobutamine stress.
Case 1
The first patient was an 18-year-old male with previously diagnosed left main coronary artery atresia and a bicuspid aortic valve, who presented with exertional chest pain. His cardiac magnetic resonance (CMR) coronary angiogram demonstrated a normal origin of the right coronary artery (RCA) and no left coronary artery ostium or left main coronary artery. The left anterior descending (LAD) and circumflex (Cx) coronary arteries were visualized with no direct connection to the aorta. At rest, the left ventricle had apical cap dyskinesis and mid-anterolateral hypokinesis. At peak stress (heart rate 156 bpm and blood pressure 156/70 mm Hg), hypokinesis also developed in the basal anterolateral, mid inferolateral, apical anterior, and apical lateral segments. Catheterization performed 3 days after the dsCMR also showed that the LAD and Cx had no direct flow from the aorta and were supplied by collaterals from a large RCA. Two weeks after the dsCMR, the patient underwent a coronary artery bypass grafting (CABG) of the left internal mammary artery to the LAD.
Case 2
The second patient was a 4-year-old female with truncus arteriosus status post-repair with a right ventricle-to-pulmonary artery conduit, followed by 2 subsequent truncal valve repairs, 2 conduit replacements, and an unroofing of the LAD and Cx arteries. At rest, her CMR showed hypokinesis of the left ventricular basal and mid-inferoseptal segments and the apical cap. At peak stress (heart rate 149 bpm, blood pressure 136/87 mm Hg), all left ventricular segments showed new or worsening hypokinesis, more prominent in the septum compared to the free wall. A catheterization 1 month later demonstrated that all coronary artery branches were unobstructed. Over 4.7 years of follow-up, the patient did not have any coronary events.
Case 3
The third patient was a 6-year-old male with an anomalous aortic origin of the RCA from the left sinus of Valsalva and an interarterial course who had undergone surgical unroofing of the RCA at age 1 year. At age 6 years, he began having episodes of pallor, chest pain, shortness of breath, dizziness, and palpitations with exertion which persisted despite initiation of a beta-blocker and calcium channel blocker. CMR demonstrated the presence of a myocardial bridge in the mid-left anterior descending coronary artery. At rest, there was no regional dysfunction. At peak stress (heart rate 163 bpm, blood pressure 159/67 mm Hg), there was hypokinesis of the left ventricular free wall segments and akinesis of the septum. Right ventricular wall motion was normal. At catheterization 6 weeks later, intravascular ultrasound of the left coronary was aborted due to significant ST-segment elevation with placement of the guidewire. Coronary angiography did not demonstrate significant LAD compression. Due to persistent symptoms despite medical therapy, he underwent surgical division of the myocardial bridge and unroofing of the LAD at age 8 years. His exertional symptoms subsequently resolved, and he had no further coronary events during 12.3 years of follow-up.
Subjects with a Negative dsCMR and a Subsequent Coronary Event
The median duration of follow-up after dsCMR was 7.4 years (IQR 4.0–11.2 years). During follow-up, 4 of the 61 patients (6.6%) with negative dsCMR examinations experienced coronary events. None of the patients who experienced a coronary event had undergone more than one dsCMR examination.
Case 4
A 20-year-old patient with pulmonary atresia, intact ventricular septum, and coronary artery fistulae status post-Fontan underwent dsCMR to evaluate symptoms of chest pain and dyspnea with mild exertion. At rest, CMR demonstrated mild global left ventricular systolic dysfunction, with akinesis of the basal septum and severe hypokinesis of the apex. At peak stress (heart rate 155 bpm, peak systolic blood pressure 185 mmHg), there were no new regional wall motion abnormalities detected. She underwent heart transplantation 10 months after dsCMR due to ongoing symptoms and a catheterization that showed no perfusion of the distal LAD territory.
Case 5
A 3-year-old male status post heart transplantation at age 1 year for dilated cardiomyopathy and with a history of acute humoral rejection underwent dsCMR. At rest, there was normal biventricular systolic function with no regional wall motion abnormalities. At peak stress (heart rate 160 bpm, blood pressure 115/52 mmHg), there were no regional wall motion abnormalities detected. The patient underwent catheterization 3 months after the dsCMR, which demonstrated post-transplant coronary artery vasculopathy. Cardiac re-transplantation was performed 1 year after the dsCMR.
Case 6
A 7-year-old patient underwent dsCMR due to a history of Kawasaki disease with giant coronary artery aneurysms (right, left main, and LAD coronary artery involvement) and severe coronary artery stenosis (> 90% occlusion) between 2 aneurysms in the RCA demonstrated at catheterization. At rest, there was normal global biventricular systolic function with mild hypokinesis noted at the basal inferior and inferoseptal segments. At peak stress (heart rate 169 bpm, blood pressure 122/62 mmHg), no inducible wall motion abnormalities were seen. Based on the catheterization angiography, the patient underwent a CABG of the right internal mammary artery to the RCA 2 days after dsCMR.
Case 7
An asymptomatic 7-year-old male with a history of Kawasaki disease, giant coronary artery aneurysms (LAD and RCA), and an occluded RCA diagnosed at his last catheterization at age 2 years underwent dsCMR as part of planned surveillance. At rest, there was normal biventricular systolic function and no regional wall motion abnormalities. At peak stress (heart rate 160 bpm, blood pressure 178/99), no inducible wall motion abnormalities were detected. Four years after the dsCMR, the patient experienced multiple episodes of syncope and nonspecific chest pain and underwent catheterization (the first since age 2 years). Angiography demonstrated a large, calcified aneurysm in the LAD with severe stenosis proximally and distally, as well as previously diagnosed occlusion of the RCA. The patient underwent CABG of the left internal mammary artery to the mid-LAD and right internal mammary artery to the posterior descending artery.
Discussion
This study evaluated the relationship of dsCMR and subsequent coronary events in pediatric patients. The rate of a positive dsCMR test was low with inducible regional wall motion abnormalities in only 3 of 80 examinations. Two of these patients underwent surgical revascularization (CABG or myocardial bridge unroofing), and the third had no subsequent coronary events. Over a median follow-up period of 7.4 years, 4 patients with a negative dsCMR had coronary events including transplantation and surgical revascularization due to findings at catheterization or ongoing symptoms. To our knowledge, this is the first study to relate dsCMR results with medium-term outcomes in a pediatric cohort.
The safety and feasibility of dsCMR in adult patients has been demonstrated in multiple large multicenter studies [9, 10]. Data regarding the utility of dsCMR for risk stratification is primarily focused on adult patients with atherosclerotic coronary heart disease. Gargiulo et al. demonstrated a negative predictive value of 98% for adverse cardiac events, including cardiac death or nonfatal myocardial infarction after dsCMR over a mean follow-up period of 2 years [11]. Jahnke et al. found that a positive result on stress CMR was an independent predictor of death or MI and had incremental benefit over resting wall motion abnormalities or clinical risk factors, such as diabetes or coronary artery disease [12]. In a meta-analysis including over 11,000 patients, Lipinski et al. demonstrated excellent prognostic value of dsCMR in patients with known or suspected coronary artery disease, with a combined annualized event rate for death or myocardial infarction of 4.9% with a positive dsCMR versus 0.8% for those with a negative result [13].
There are only a few reports regarding the utility of dsCMR to detect inducible ischemia in pediatric patients. We previously published data demonstrating that dsCMR was safe and feasible and had excellent interobserver agreement [7]. Among 28 patients ≤ 22 years of age with congenital or acquired coronary artery abnormalities, or history of coronary artery translocation, there were no serious adverse events and image quality scores were high. Additional studies have confirmed the safety of dsCMR in pediatric patients as well as explored its accuracy. A prospective study of 13 pediatric patients with a history of or risk factors for coronary artery disease demonstrated that dsCMR was well tolerated and had good agreement with coronary angiography performed at a similar timepoint [14]. In a cohort of 182 pediatric patients ≤ 20 years old with anomalous aortic origin of a coronary artery, there were no major adverse events during dsCMR [15]. In a study of 19 patients < 18 years old with diagnoses of anomalous aortic origin of a coronary artery or myocardial bridge who underwent both stress CMR (with dobutamine or regadenoson) and invasive fractional flow reserve (FFR), there were no adverse events related to CMR (or FFR) [16]. Abnormal stress CMR results correlated well with FFR, with a positive percent agreement of 78% and negative percent agreement of 80%.
In the current study, only 3 of 80 dsCMR examinations showed inducible wall motion abnormalities. Two of these patients underwent subsequent surgical intervention for coronary artery ischemia and the other remained asymptomatic for over 4 years of follow-up. These data demonstrate an overall low positivity rate in dsCMR studies performed in a pediatric population, as well as the clinical utility and need to interpret the results within the full clinical context. In a patient with concern for coronary insufficiency, a positive dsCMR result confirms the clinical suspicion and supports revascularization. In the absence of symptoms, a positive result alone may not warrant such an intervention. Although the low positivity rate in our study could suggest an error in interpretation and potential false-negative results; the clinical event rate during follow-up was low and we have previously demonstrated good inter-reader agreement. Alternatively, the low positivity rate may truly reflect the rarity of ischemia in a pediatric population. This may be related to a greater propensity for developing coronary artery collaterals that can bypass anatomic obstructions to supply the myocardial capillary bed. In support of this, Schmitt et al. showed that among patients with repaired anomalous left coronary artery arising from the pulmonary artery, those with more collaterals were less likely to have inducible wall motion abnormalities on dsCMR [17].
During a median follow-up period of 7.4 years after dsCMR, 4 of the 61 patients with a negative dsCMR examination (77 negative examinations, as some patients had more than 1 dsCMR) experienced coronary events defined as a myocardial infarction, surgical- or catheter-based coronary artery intervention, or chest pain concerning for ischemia. This observation indicates that patients with a negative dsCMR generally have a good medium-term prognosis and that the test had a high negative predictive value for coronary events (95%). Nevertheless, a review of the 4 patients with coronary events who may represent failures of dsCMR from a prognostic standpoint is useful. Coronary events occurred at 2 days, 10 months, 1 year, and 4 years following dsCMR. All the coronary event endpoints were surgical interventions, 2 of which were in the setting of possible ischemic symptoms (cases 4 and 7). No patient had a myocardial infarction, death, or aborted sudden death. None had physiologic testing for inducible ischemia by another modality (e.g., single-photon emission computed tomography), but all 4 had coronary angiography at catheterization that showed significant anatomic obstruction. For case 7, the catheterization occurred 4 years after the dsCMR and it is plausible that there could have been significant disease progression in the interim. These cases highlight that the clinical management in patients with coronary obstruction is complex and requires the synthesis of all the available information.
The small number of positive dsCMR examinations and subsequent coronary events in this study make it challenging to make recommendations for the use of dsCMR. Moreover, there are insufficient data in pediatric patients to compare the performance of dsCMR to other tests for inducible ischemia. Considering these constraints, we believe it is reasonable to use dsCMR to assess patients at risk for coronary ischemia and without ischemic symptoms. Those with a negative dsCMR likely have a low risk of myocardial infarction, death, or aborted sudden death over the next few years. The interval between dsCMR examinations should be determined based on additional clinical information including patient symptoms and coronary anatomy from cardiac catheterization, cardiac magnetic resonance, or cardiac computed tomography. In patients at risk for coronary ischemia who have ischemic symptoms, assessment with dsCMR is also reasonable and, in most cases, should be accompanied by high-quality anatomic delineation of the coronary arteries. A positive dsCMR result confirms the clinical suspicion and supports revascularization.
Our study has several important limitations. As a single-center study, it may not be generalizable to other settings. Despite being the largest pediatric dsCMR series with medium-term follow-up to date, the small number of positive dsCMR studies and subsequent coronary events limited its analytic power and precluded a meaningful statistical analysis. The varied diagnoses and indications for dsCMR also confound the interpretation of the results. Lastly, the follow-up duration was variable.
Conclusion
In this series of pediatric patients undergoing dsCMR, wall motion abnormalities indicating inducible ischemia were uncommon. On medium-term follow-up, those with a negative dsCMR did not experience myocardial infarction, death, or aborted sudden death. However, several of these patients underwent revascularization procedures or heart transplantation driven by angiographic findings at catheterization and, in some cases, by symptoms as well. Larger multicenter studies with long-term follow-up are needed to further assess the prognostic value of dsCMR in pediatric patients.
Data Availability
No datasets were generated or analysed during the current study.
References
Nagel E, Lehmkuhl HB, Bocksch W et al (1999) Noninvasive diagnosis of ischemia-induced wall motion abnormalities with the use of high-dose dobutamine stress MRI: comparison with dobutamine stress echocardiography. Circulation 99(6):763–770. https://doi.org/10.1161/01.CIR.99.6.763
Nandalur KR, Dwamena BA, Choudhri AF, Nandalur MR, Carlos RC (2007) Diagnostic performance of stress cardiac magnetic resonance imaging in the detection of coronary artery disease: a meta-analysis. J Am Coll Cardiol 50(14):1343–1353. https://doi.org/10.1016/j.jacc.2007.06.030
Stacey RB, Vera T, Morgan TM et al (2018) Asymptomatic myocardial ischemia forecasts adverse events in cardiovascular magnetic resonance dobutamine stress testing of high-risk middle-aged and elderly individuals. J Cardiovasc Magn Reson 20(1):1–11. https://doi.org/10.1186/s12968-018-0492-5
Kelle S, Chiribiri A, Vierecke J et al (2011) Long-term prognostic value of dobutamine stress CMR. JACC Cardiovasc Imaging 4(2):161–172. https://doi.org/10.1016/j.jcmg.2010.11.012
Korosoglou G, Elhmidi Y, Steen H et al (2010) Prognostic value of high-dose dobutamine stress magnetic resonance imaging in 1,493 consecutive patients: assessment of myocardial wall motion and perfusion. J Am Coll Cardiol 56(15):1225–1234. https://doi.org/10.1016/j.jacc.2010.06.020
Petrov G, Kelle S, Fleck E, Wellnhofer E (2015) Incremental cost-effectiveness of dobutamine stress cardiac magnetic resonance imaging in patients at intermediate risk for coronary artery disease. Clin Res Cardiol 104(5):401–409. https://doi.org/10.1007/s00392-014-0793-0
Strigl S, Beroukhim R, Valente AM et al (2009) Feasibility of dobutamine stress cardiovascular magnetic resonance imaging in children. J Magn Reson Imaging 29(2):313–319. https://doi.org/10.1002/jmri.21639
Cerqueira MD, Weissman NJ, Dilsizian V et al (2002) Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. J Cardiovasc Magn Reson 4(2):203–210. https://doi.org/10.1081/JCMR-120003946
Menadas JVM, Lopez-Lereu MP, Erill JE, Gonzalez PG, Muñoz BI, Gonzalez AM (2016) Pharmacological stress cardiovascular magnetic resonance: feasibility and safety in a large multicentre prospective registry. Eur Heart J Cardiovasc Imaging 17(3):308–315. https://doi.org/10.1093/ehjci/jev153
Wahl A, Paetsch I, Gollesch A et al (2004) Safety and feasibility of high-dose dobutamine-atropine stress cardiovascular magnetic resonance for diagnosis of myocardial ischaemia: experience in 1000 consecutive cases. Eur Heart J 25(14):1230–1236. https://doi.org/10.1016/j.ehj.2003.11.018
Gargiulo P, Dellegrottaglie S, Bruzzese D et al (2013) The prognostic value of normal stress cardiac magnetic resonance in patients with known or suspected coronary artery disease: a meta-analysis. Circ Cardiovasc Imaging 6(4):574–582. https://doi.org/10.1161/CIRCIMAGING.113.000035
Jahnke C, Nagel E, Gebker R et al (2007) Prognostic value of cardiac magnetic resonance stress tests: adenosine stress perfusion and dobutamine stress wall motion imaging. Circulation 115(13):1769–1776. https://doi.org/10.1161/CIRCULATIONAHA.106.652016
Lipinski MJ, McVey CM, Berger JS, Kramer CM, Salerno M (2013) Prognostic value of stress cardiac magnetic resonance imaging in patients with known or suspected coronary artery disease: a systematic review and meta-analysis. J Am Coll Cardiol 62(9):826–838. https://doi.org/10.1016/j.jacc.2013.03.080
Stagnaro N, Moscatelli S, Cheli M, Bondanza S, Marasini M, Trocchio G (2023) Dobutamine stress cardiac MRI in pediatric patients with suspected coronary artery disease. Pediatr Cardiol 44(2):451–462. https://doi.org/10.1007/s00246-022-03007-7
Doan TT, Molossi S, Sachdeva S et al (2021) Dobutamine stress cardiac MRI is safe and feasible in pediatric patients with anomalous aortic origin of a coronary artery (AAOCA). Int J Cardiol 334:42–48. https://doi.org/10.1016/j.ijcard.2021.04.031
Agrawal H, Wilkinson JC, Noel CV (2021) Impaired myocardial perfusion on stress CMR correlates with invasive FFR in children with coronary anomalies. J Invasive Cardiol 33(1):45–51
Schmitt B, Bauer S, Kutty S et al (2014) Myocardial perfusion, scarring, and function in anomalous left coronary artery from the pulmonary artery syndrome : a long-term analysis using magnetic resonance imaging. Ann Thorac Surg 98:1425–1436
Author information
Authors and Affiliations
Contributions
M.B. designed the study, collected data, wrote the manuscript text, and revised the manuscript. A.P. designed the study, participated in data collection, and revised the manuscript. R.B., A.D., D.A., and A.B. reviewed the study design and revised the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Beattie, M., Beroukhim, R., Annese, D. et al. Coronary Events Following Dobutamine Stress Cardiac Magnetic Resonance Imaging in Pediatric Patients. Pediatr Cardiol (2024). https://doi.org/10.1007/s00246-024-03632-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00246-024-03632-4