Abstract
Despite their anatomical differences, congenitally corrected (ccTGA) and complete transposition of the great arteries (d-TGA) post-atrial switch are frequently studied together and managed similarly from a medical standpoint due to the shared systemic right ventricle (sRV). The aim was to assess differences in their underlying hemodynamics. The study is a retrospective review of 138 adults with ccTGA or d-TGA post-atrial switch undergoing cardiac catheterization at Mayo Clinic, MN between 2000 and 2021. ccTGA was categorized into isolated or complex ccTGA depending on concomitant ventricular septal defect and/or left ventricular outflow obstruction. There were 53 patients with d-TGA (91% post-Mustard procedure), 51 with complex and 34 with isolated ccTGA. Isolated ccTGA patients were older (51.8 ± 13.1 years) than those with d-TGA (37.5 ± 8.3 years) or complex ccTGA (40.8 ± 13.4 years). There were no differences in sRV or left ventricular size and function across groups. The ccTGA group more commonly had ≥ moderate tricuspid regurgitation than those with d-TGA; ≥ moderate mitral and ≥ moderate pulmonary regurgitation were most prevalent in complex ccTGA. There were no differences in sRV end-diastolic pressure (sRVEDP) or PAWP between groups. However, the ratio of PAWP:sRVEDP was higher in those with d-TGA compared to those with ccTGA. Cardiac index was higher in the d-TGA group than both groups of ccTGA patients with the latter showing higher indices of ventricular afterload. In conclusion, despite sharing a sRV, adults with d-TGA and ccTGA have substantial differences in hemodynamics and structural/valvular abnormalities. Further investigation regarding disease-specific responses to heart failure therapy in those with d-TGA and ccTGA is warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The presence of a systemic right ventricle (sRV) is a shared anatomical feature of patients born with complete and congenitally corrected (ccTGA) transposition of the great arteries (TGA). Individuals with a sRV are at risk for progressive sRV enlargement and dysfunction, worsening tricuspid (systemic atrioventricular valve) regurgitation (TR), and atrial and ventricular arrhythmias [1]. Given these long-term sequelae and the inherent complications associated with surgically created atrial baffles, the arterial switch procedure is now the operation of choice in patients born with complete TGA. However, a substantial population of patients post-atrial switch operation are still followed and, as they approach the fourth and fifth decades of life, the number of individuals with complete TGA and a sRV presenting with heart failure is expected to rise [2].
Overwhelming data are now available demonstrating the efficacy of medical therapy in improving ventricular function, rates of hospitalization and death in individuals with systemic left ventricular systolic dysfunction [3, 4]. In contrast, these medications have not been proven to be beneficial in those with a sRV [5]. Given the obvious structural differences, it is possible that failing systemic right and left ventricles behave differently from a hemodynamic standpoint. Moreover, it would be intuitive to expect that not all patients with a sRV (given their heterogeneity) would have similar hemodynamic phenotypes, possibly responding differently to medical and interventional/surgical therapy. Accordingly, the aim of this study is to assess differences in underlying hemodynamics between adults with TGA post-atrial switch and ccTGA undergoing catheterization at our institution.
Methods
This retrospective cohort included 138 consecutive patients with ccTGA or complete TGA post-atrial switch procedure undergoing invasive hemodynamic evaluation at Mayo Clinic, Rochester, MN between January of 2000 and February 2021. Individuals undergoing palliative atrial switch procedure or Fontan operation were excluded. Patients with ccTGA were further categorized into complex ccTGA if repaired or unrepaired ventricular septal defect, left ventricular outflow obstruction, or pulmonary atresia was present; individuals were otherwise categorized as isolated ccTGA. Acknowledging that complete TGA and dextroposition of the aorta are not synonyms, complete TGA will henceforth be referred to as d-TGA to improve readership and avoid confusion. The Institutional Review Board approved the study and only patients previously providing research authorization for the use of medical records were selected.
Cardiac catheterization data were abstracted from the procedural reports. The procedure was carried out in a fasting state, without discontinuation of chronic medications, and under mild sedation except for 8 patients (5.7%) whose procedures were performed under general anesthesia. Reported pressure measurements represent a mean of ≥ 5 consecutive beats under spontaneous breathing. Cardiac output was calculated by the Fick principle. In patients with bilateral pulmonary artery and/or pulmonary artery wedge (PAWP) pressure measurements, the right one was arbitrarily chosen since it was more commonly recorded. Pulmonary vascular resistance (PVR) was calculated as the difference between ipsilateral pulmonary artery mean pressure and PAWP divided by pulmonary flow (Qp). Systemic vascular resistance (SVR) was calculated as the difference between the arterial mean pressure and right atrial/systemic venous atrial pressure divided by systemic flow (Qs); effective arterial elastance (Ea) was calculated as (systolic arterial pressure × 0.9)/stroke volume [6]. For patients with d-TGA, the presence of baffle obstruction at cardiac catheterization was based on the operator’s interpretation of hemodynamic, angiographic and/or intraprocedural echocardiographic data.
Clinical, echocardiography, and surgical data were obtained from the medical records. The model for end-stage liver disease score excluding international normalized ratio (INR) (MELD-XI), a marker of hepatic disease that has been used in other cohorts of cardiac patients [7], was calculated using creatinine and bilirubin. Given its clinical relevance, if sRV ejection fraction, sRV size, or degree of atrioventricular valve regurgitation were not reported at the time of clinical study, images were reviewed offline by an experienced congenital echocardiographer (H.M.C.). Reflecting the practice of our laboratory, the assessment of RV size and systolic function was performed qualitatively; sRV ejection fraction data reported herein represent visually estimated values.
Statistical Analysis
Nominal data are presented as counts (%) and continuous data as mean (± standard deviation) or median (25–75th percentile), whichever appropriate. Comparisons between all 3 groups were performed using one-way ANOVA or the Kruskal–Wallis test for continuous variables and the chi-square test for nominal variables. Individual comparisons were performed using the chi-square for nominal and unpaired t-test or rank sum for continuous variables. Due to sample size, comparisons between nominal and continuous variables within the ccTGA group were done using the rank sum or Fisher’s exact test, respectively. Regression analyses were used to assess the association between hemodynamics and transposition type while adjusting for age, with respective results presented as β coefficients ± standard error. Statistical analysis was performed using JMP 14.1 for SAS (Cary, NC); a p-value < 0.05 was considered statistically significant.
Results
The d-TGA group included 53 individuals. Venous catheterization was performed in all patients and systemic ventricular catheterization in 46. Median age at the time of atrial switch operation was 17 months (9; 32.3 months). Most patients underwent the Mustard procedure (48 individuals, 90.5%) with 3 patients undergoing the Shumacker modification [8] and 2 undergoing the Senning procedure. A history of systemic or pulmonary venous baffle obstruction was present in 21 (39.6%) and 13 (24.5%) patients, respectively; at the time of catheterization, evidence of residual or de novo systemic and pulmonary venous obstruction was diagnosed in 29 (54.7%) and 9 individuals (16.9%), respectively.
There were 85 patients with ccTGA (51 complex and 34 isolated); cardiac catheterization was ordered as part of pre-operative evaluation in 33 of them (38.6%). Venous catheterization was performed in 74 patients and systemic ventricular catheterization in 75. Among those with complex ccTGA, a history of ventricular septal defect was present in 45 (88.2%) and left ventricular outflow tract obstruction/pulmonary atresia in 38 (74.5%). Forty patients (75.5%) had undergone cardiac operations, including ventricular septal defect closure in 31 (60.8%), implantation of pulmonary valve prosthesis/conduit in 21 (40.1%), tricuspid valve intervention in 12 (23.5%, including 2 prior tricuspid repairs), and relief of subpulmonary/pulmonary stenosis in 11 (22.0%). In contrast, among those with isolated ccTGA, only 5 patients (14.7%) had undergone cardiac surgery (concomitant tricuspid valve surgery/atrial septal defect closure in 2; isolated tricuspid valve replacement, patent ductus arteriosus and coarctation of the aorta repair in one each).
Clinical and echocardiography data are presented in Table 1. Patients with isolated ccTGA were older than those with complex ccTGA and d-TGA. As expected, the number of prior cardiac operations was higher in those with d-TGA and complex ccTGA than in individuals with isolated ccTGA. Similarly, prior pulmonary valve replacement/conduit implantation was most commonly seen in those with complex ccTGA. Prior tricuspid valve surgery was more prevalent in complex ccTGA but no differences were present between d-TGA and isolated ccTGA. Otherwise, there were no differences in comorbidities, functional capacity, medications, or symptoms. Regarding laboratory values, those with complex ccTGA demonstrated higher MELD-XI scores than both d-TGA and isolated ccTGA groups.
There were no differences in sRV ejection fraction, left ventricular size, and function across groups. Complex ccTGA patients less commonly had ≥ moderate RV enlargement when compared to d-TGA patients. The presence of ≥ moderate pulmonary regurgitation was much more common in complex ccTGA than in the other two groups. Similarly, ≥ moderate mitral (subpulmonary) regurgitation was more commonly seen in patients with complex ccTGA (p = 0.007 and p = 0.03 when compared to d-TGA and isolated ccTGA, respectively).
Patients with ccTGA more frequently had ≥ moderate tricuspid regurgitation than those with d-TGA, but the prevalence was similar between isolated and complex ccTGA. The median tricuspid valve/prosthesis gradient was 5 mmHg (3; 6.2) for patients with complex ccTGA; all 3 patients in isolated ccTGA who had tricuspid valve intervention had gradients ≤ 6 mmHg, whereas the transtricuspid gradient was 9 mmHg for the single d-TGA patient with a tricuspid prosthesis.
Cardiac Catheterization
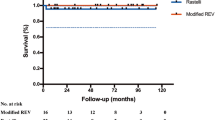
Cardiac catheterization findings are presented in Table 2 and summarized in Figs. 1 and 2. There were no differences in sRV end-diastolic pressure (sRVEDP) or PAWP between all groups. However, the ratio of PAWP:sRVEDP was significantly higher in those with d-TGA compared to patients with complex or isolated ccTGA. When adjusting for age, the association between higher PAWP:sRVEDP and d-TGA remained (β = 0.18 ± 0.04, p < 0.0001), while no association between d-TGA and sRVEDP (β = − 1.0 ± 0.6, p = 0.09) or PAWP (β = 1.2 ± 0.7, p = 0.09) was seen.
Filling pressures and mean pulmonary artery pressures in patients with d-TGA and ccTGA. Higher systemic venous pressure/right atrial pressure was seen among patients with complex ccTGA compared to other groups. No differences were seen across groups with regard to mean pulmonary artery (PA) pressures, pulmonary artery wedge pressure (PAWP), or sRV end-diastolic pressures (sRVEDP). However, PAWP:sRVEDP was highest in the d-TGA group, suggesting a larger role played by the pulmonary venous atrium/baffle in pulmonary venous hypertension among these patients.
Systemic venous atrium/right atrial pressures were lower in individuals with isolated ccTGA compared to those with d-TGA or complex ccTGA. As anticipated given the anatomic substrate, left ventricle systolic pressure was highest among patients with complex ccTGA. No differences were seen with regards to mean pulmonary artery pressure or PVR. A mean pulmonary artery pressure > 25 mmHg was seen in 45.1% of patients in the d-TGA group, 45.6% in the complex ccTGA group, and 50% in the isolated ccTGA group.
Cardiac index was significantly higher in the d-TGA group compared to both groups of ccTGA patients. Noteworthy, there were no differences in heart rate or body mass index across the 3 groups. Both complex and isolated ccTGA had higher SVR than those with d-TGA; similarly, Ea was lower in the d-TGA group compared to complex ccTGA patients, but no differences were seen between the latter and patients with isolated ccTGA. The associations between d-TGA and higher cardiac index (β = 0.15 ± 0.06, p = 0.02), as well as higher SVR and ccTGA (β = 122.2 ± 46.3, p = 0.001) remained present after adjustment for age.
Due to the potential influences of TR on underlying hemodynamics, ccTGA patients with and without ≥ moderate TR were compared (Supplemental Table 1). Among those with complex ccTGA, ≥ moderate TR was associated with higher PAWP:RVEDP ratios and lower right atrial pressure:PAWP indices. The sample size did not allow for intragroup comparisons among those with isolated ccTGA.
Given the inherent impact on PAWP, hemodynamic findings across the 3 groups were also compared after excluding patients with pulmonary venous baffle obstruction (Supplemental Table 2). Even after excluding the 9 patients found to have pulmonary venous obstruction at catheterization, findings were similar to those presented in Table 2.
Discussion
We present herein clinical and cardiac catheterization findings in a large cohort of predominantly symptomatic adults with d-TGA and ccTGA. Our results demonstrate that despite sharing a sRV, these patients markedly differ both structurally and hemodynamically. The main findings of our study are as follows: (1) cardiac index was significantly lower and afterload higher in those with ccTGA when compared to d-TGA; (2) there were no differences in PAWP but the higher PAWP:sRVEDP suggests a lower contribution of sRV filling pressures and larger role played by the pulmonary venous atrium/baffle in pulmonary venous hypertension among those with d-TGA; (3) venous/right atrial hypertension was more common in d-TGA and complex ccTGA patients; (4) ≥ moderate pulmonary regurgitation and mitral regurgitation were prevalent among complex ccTGA patients.
In patients with a systemic left ventricle, systolic ventricular dysfunction culminates in a reduction in cardiac output. This low-flow state results in an increase in adrenergic tone and neurohormonal activation to maintain systemic perfusion [3, 4]. These physiologic changes are the pillar for the use of intensive medical therapy and provided the foundation for the initial studies assessing the role of beta blockers and angiotensin-converting enzyme inhibitors in heart failure. Systolic dysfunction of the sRV is highly prevalent in adults with d-TGA post-atrial switch and ccTGA [1]. Therefore, it would be intuitive to apply the medical armamentarium proven to be highly effective in dysfunctional left ventricles to individuals with sRV. However, investigations of standard heart failure medical therapy in patients with sRV have been disappointing [5]. The use of sacubitril/valsartan was recently noted to be associated with improvements in cardiac biomarkers and echocardiography parameters in patients with sRV [9,10,11] but our understanding of its benefits in this population is still incipient. It has been suggested that patients with sRV are unique anatomically but also biochemically, as most have normal catecholamine levels [12, 13]. It is important to note that most studies in patients with a sRV have included patients with d-TGA and ccTGA interchangeably, with d-TGA typically constituting the majority.
Data regarding invasive hemodynamics in patients with sRV are mostly limited to small studies, predominantly including pediatric patients [14,15,16,17,18,19,20,21,22]. Similar to individuals with a dysfunctional systemic left ventricle, in our cohort, patients with isolated ccTGA were found to have reduced cardiac indices and, notably, higher afterload indices when compared to those with d-TGA. Interestingly, we previously reported systemic hypertension to be a risk factor for progressive sRV dysfunction in ccTGA patients [23]. Given the intrinsic abnormalities of the tricuspid valve, it is not surprising that many patients with ccTGA had significant TR, contributing to the reduction in forward flow and increase in PAWP. Although the small number of individuals with < moderate TR limited our analysis, the hemodynamics in this subset of patients do not appear to markedly differ from those with significant TR, suggesting a significant role played by the sRV itself in these hemodynamic derangements. Importantly, right atrial pressure was lowest in the isolated ccTGA group, underscoring the predominantly systemic/“left-sided” pathology. Therefore, of all 3 groups, patients with isolated ccTGA might be the closest to individuals with myopathic left ventricles. It should also be highlighted that, in contrast to the latter, TR in ccTGA is typically related to a primary pathology of the valve [24] and should be sought and addressed proactively due to negative consequences to the sRV.
It would be natural to focus on the systemic ventricle in all individuals with ccTGA presenting with symptoms. Contrary to these expectations, our findings in the subgroup of patients with complex ccTGA actually share several similarities with observations in adults late after repair of tetralogy of Fallot. Firstly, the prevalence of ≥ pulmonary regurgitation was high, being present in more than 25% of patients. Secondly, one third of patients had significant subpulmonary mitral regurgitation. Subpulmonary atrioventricular valve regurgitation is a well-known late complication in adults with tetralogy of Fallot, particularly in those with dilated subpulmonary ventricles and pulmonary regurgitation. In our experience, the mechanisms of subpulmonary mitral regurgitation in complex ccTGA are due to a combination of annular dilatation, intrinsic mitral valve abnormalities and, in some, device lead-related regurgitation [25]. Although not the focus of the study, this is an important observation given the propensity of this group to develop conduction abnormalities and other arrhythmias which require pacemaker/device implantation. Thirdly, right atrial hypertension was common, perhaps explaining the MELD-XI score seen in this group. Therefore, it is mandatory that adults with complex ccTGA are seen as having biventricular pathology with equal attention paid to the subpulmonary and systemic ventricles and valves.
We have highlighted the role of the atrial baffles in pulmonary venous pressure and pathophysiology of pulmonary hypertension in patients with d-TGA [26]. This contribution went beyond the risk of pulmonary venous baffle obstruction with some patients having clear invasive hemodynamic findings of atrial noncompliance. In the present study, no differences in the degree of pulmonary venous hypertension (i.e., PAWP) were seen between patients with d-TGA and ccTGA. However, the ratio of PAWP:RVEDP was significantly higher in those with d-TGA, supporting a different mechanism in the pathogenesis of pulmonary congestion in the two groups. It is also interesting that despite the presence of atrial baffles, cardiac indices were higher and afterload lower in those with d-TGA than ccTGA. These findings reinforce the differences in underlying hemodynamics between the two transposition groups and might have explained the findings of previous studies focusing on neurohormonal activation and catecholamine release in patients with d-TGA.
Future Implications
Figure 3 summarizes the invasive hemodynamic and structural abnormalities according to subgroups of individuals with TGA. Neurohormonal activation and biomarker release may differ among those with ccTGA and d-TGA [10] not only due to the presence of atrial baffles, but also due to the differences in filling pressures and intrinsic ventricular/myopathic disease (including the subpulmonary left ventricle). As we investigate the role of additional heart failure therapies such as sodium-glucose cotransporter-2 inhibitors [9] and expand our experience with sacubitril/valsartan in this population, further analyses regarding the disease-specific therapeutic responses (i.e., ccTGA vs d-TGA) are warranted. Lastly, the impact of percutaneous or surgical valvular interventions in adults with sRV (particularly in those with significantly reduced systolic function) is still poorly delineated and requires additional investigation.
Limitations
We acknowledge the limitations of the study, including its retrospective nature. This represents a cohort of patients referred for cardiac catheterization at a quaternary care center, and some of the findings may not be fully applicable to asymptomatic individuals with preserved functional capacity seen in the outpatient practice. Despite the relatively large sample size compared to other studies including patients with a sRV, the number of individuals in some subgroups limited our analyses. Additionally, the sample size might have resulted in type II error. Specifically, the number of individuals with isolated ccTGA and < moderate TR was particularly small. Lastly, cross-sectional data were unavailable and, therefore, might have affected the prevalence of significant ventricular enlargement and dysfunction given the inherent limitations of transthoracic echocardiography in those with sRV.
Conclusion
Despite sharing a sRV, adults with d-TGA and ccTGA have substantial differences in hemodynamics and associated structural/valvular abnormalities (particularly those with complex ccTGA). As we expand our experience and investigate the role of newer heart failure therapeutic agents, further investigation regarding the disease-specific responses in those with d-TGA and ccTGA is warranted.
Abbreviations
- ccTGA:
-
Congenitally corrected transposition of the great arteries
- d-TGA:
-
Complete transposition of the great arteries
- PAWP:
-
Pulmonary artery wedge pressure
- PVR:
-
Pulmonary vascular resistance
- sRV:
-
Systemic right ventricle
- SVR:
-
Systemic vascular resistance
- TGA:
-
Transposition of the great arteries
- TR:
-
Tricuspid regurgitation
References
Brida M, Diller GP, Gatzoulis MA (2018) Systemic right ventricle in adults with congenital heart disease: anatomic and phenotypic spectrum and current approach to management. Circulation 137:508–518
Roos-Hesselink JW, Meijboom FJ, Spitaels SE, van Domburg R, van Rijen EH, Utens EM, McGhie J, Bos E, Bogers AJ, Simoons ML (2004) Decline in ventricular function and clinical condition after Mustard repair for transposition of the great arteries (a prospective study of 22–29 years). Eur Heart J 25:1264–1270
Joseph P, Swedberg K, Leong DP, Yusuf S (2019) The evolution of beta-blockers in coronary artery disease and heart failure (Part 1/5). J Am Coll Cardiol 74:672–682
Leong DP, McMurray JJV, Joseph PG, Yusuf S (2019) From ACE Inhibitors/ARBs to ARNIs in coronary artery disease and heart failure (Part 2/5). J Am Coll Cardiol 74:683–698
Zaragoza-Macias E, Zaidi AN, Dendukuri N, Marelli A (2019) Medical therapy for systemic right ventricles: a systematic review (Part 1) for the 2018 AHA/ACC guideline for the management of adults with congenital heart disease: a report of the American college of cardiology/American heart association task force on clinical practice guidelines. Circulation 139:e801–e813
Kelly RP, Ting CT, Yang TM, Liu CP, Maughan WL, Chang MS, Kass DA (1992) Effective arterial elastance as index of arterial vascular load in humans. Circulation 86:513–521
Heuman DM, Mihas AA, Habib A, Gilles HS, Stravitz RT, Sanyal AJ, Fisher RA (2007) MELD-XI: a rational approach to “sickest first” liver transplantation in cirrhotic patients requiring anticoagulant therapy. Liver Transpl 13:30–37
Hbs HB (1961) A new operation for transposition of the great vessels. Surgery 50:773–777
Egorova AD, Nederend M, Tops LF, Vliegen HW, Jongbloed MRM, Kies P (2022) The first experience with sodium-glucose cotransporter 2 inhibitor for the treatment of systemic right ventricular failure. ESC Heart Fail 9:2007–2012
Nederend M, Kies P, Regeer MV, Vliegen HW, Mertens BJ, Robbers-Visser D, Bouma BJ, Tops LF, Schalij MJ, Jongbloed MRM, Egorova AD (2023) Tolerability and beneficial effects of sacubitril/valsartan on systemic right ventricular failure. Heart. https://doi.org/10.1136/heartjnl-2022-322332
Zandstra TE, Nederend M, Jongbloed MRM, Kies P, Vliegen HW, Bouma BJ, Tops LF, Schalij MJ, Egorova AD (2021) Sacubitril/valsartan in the treatment of systemic right ventricular failure. Heart 107:1725–1730
Dore A, Houde C, Chan KL, Ducharme A, Khairy P, Juneau M, Marcotte F, Mercier LA (2005) Angiotensin receptor blockade and exercise capacity in adults with systemic right ventricles: a multicenter, randomized, placebo-controlled clinical trial. Circulation 112:2411–2416
Szymanski P, Klisiewicz A, Lubiszewska B, Janas J, Baranska K, Lipczynska M, Kowalski M, Rozanski J, Hoffman P (2010) Endogenous catecholamine levels and function of the systemic right ventricle following atrial switch. Int J Cardiol 138:81–86
Schiebler GL, Edwards JE, Burchell HB, Dushane JW, Ongley PA, Wood EH (1961) Congenital corrected transposition of the great vessels: a study of 33 cases. Pediatrics 27(5):849–888
Cumming GR (1962) Congenital corrected transposition of the great vessels without associated intracardiac anomalies. A clinical, hemodynamic and angiographic study. Am J Cardiol 10:605–614
Friedberg DZ, Nadas AS (1970) Clinical profile of patients with congenital corrected transposition of the great arteries. A study of 60 cases. N Engl J Med 282:1053–1059
Mair DD, Danielson GK, Wallace RB, McGoon DC (1974) Long-term follow-up of Mustard operation survivors. Circulation 50:II46-53
Graham TP Jr, Atwood GF, Boucek RJ Jr, Boerth RC, Nelson JH (1975) Right heart volume characteristics in transposition of the great arteries. Circulation 51:881–889
Silove ED, Taylor JF (1976) Haemodynamics after Mustard’s operation for transposition of the great arteries. Br Heart J 38:1037–1046
Hagler DJ, Ritter DG, Mair DD, Davis GD, McGoon DC (1978) Clinical, angiographic, and hemodynamic assessment of late results after Mustard operation. Circulation 57:1214–1220
Hagler DJ, Ritter DG, Mair DD, Tajik AJ, Seward JB, Fulton RE, Ritman EL (1979) Right and left ventricular function after the Mustard procedure in transposition of the great arteries. Am J Cardiol 44:276–283
Graham TP Jr, Parrish MD, Boucek RJ Jr, Boerth RC, Breitweser JA, Thompson S, Robertson RM, Morgan JR, Friesinger GC (1983) Assessment of ventricular size and function in congenitally corrected transposition of the great arteries. Am J Cardiol 51:244–251
Egbe AC, Miranda WR, Jain CC, Connolly HM (2022) Prognostic implications of progressive systemic ventricular dysfunction in congenitally corrected transposition of great arteries. JACC Cardiovasc Imaging 15:566–574
Connolly HM, Miranda WR, Egbe AC, Warnes CA (2019) Management of the adult patient with congenitally corrected transposition: challenges and uncertainties. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu 22:61–65
Abdelrehim AA, Dearani JA, Miranda WR, Connolly HM, Stephens EH (2023) Surgical considerations for the mitral valve in congenitally corrected transposition. Ann Thorac Surg. https://doi.org/10.1016/j.athoracsur.2023.07.009
Miranda WR, Jain CC, Connolly HM, DuBrock HM, Cetta F, Egbe AC, Hagler DJ (2020) Prevalence of pulmonary hypertension in adults after atrial switch and role of ventricular filling pressures. Heart. https://doi.org/10.1136/heartjnl-2020-317111
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
WRM—study design, data abstraction/analysis, and drafting of the manuscript; CCJ, ACE, YND, JAD, DJH—critical review of the manuscript; HMC—data abstraction and critical review of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Miranda, W.R., Jain, C.C., Egbe, A.C. et al. Hemodynamics in Adults with Systemic Right Ventricles: Differences Between Congenitally Corrected and Complete Transposition of the Great Arteries. Pediatr Cardiol (2024). https://doi.org/10.1007/s00246-023-03381-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00246-023-03381-w