Abstract
Psoriasis is a skin disorder which mostly affects adults, beginning in childhood in almost one-third of patients. In adults it is associated with increased risk for cardiovascular diseases (CVD), while this association is still debated at younger age. Our aim was to evaluate the association between psoriasis and metabolic markers and cardiovascular findings in this age group. Twenty consecutive patients previously diagnosed with psoriasis (group A) were enrolled and compared with healthy non- psoriatic age- and sex-matched subjects (group B). The severity of the disease, CV risk factors, including anthropometric data with adiposity and its distribution, blood pressure (BP), laboratory metabolic tests, echocardiography and vascular ultrasound (transcranial echo-Doppler and carotid artery echo-Doppler with carotid intima-media thickness, cIMT) were performed for each subject. Personal history for CV risk, BP, anthropometric data were similar between the two groups, while familiar history for psoriasis was more frequent in group A (p < 0.02). C-IMT was significantly higher in group A compared to B (right, p = 0.001; left, p = 0.002). In addition, c-IMT was positively correlated with disease duration, triglycerides and triglycerides/glucose. Cerebral flow velocities, cardiac measurements, systo-diastolic function, ventricle geometry and mass were normal and comparable between the two groups, and did not correlate with CV risk factors. In childhood psoriasis c-IMT could represent a marker of pre-clinical cardiovascular involvement and contribute to start a personalized management, while cardiac findings seem to be normal in the early stage of disease. Longitudinal studies can clarify the progression of CV involvement in paediatric-onset psoriasis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
What is Known
Increase of cardiovascular risk is a well-documented issue in psoriatic adults. Its increase in childhood is nowadays matter of discussion. Some correlations between psoriasis and metabolic disease in children have already been discovered.
What is New
This study investigated cardiovascular risk using ultrasound. We evidenced a significant increase of carotid Intima-Media Thickness (cIMT) in psoriatic children compared to control group, identifying a possible early marker of disease and assuming a cut-off for early management.
Introduction
Psoriasis is a chronic, immune–mediated skin disorder mostly affecting adult population, with a prevalence of 0.1–2.1% [1]. In adults a link between psoriasis and cardiovascular disease (CVD) has been found [2, 3]: despite the precise mechanism has not been clarified yet, the systemic inflammation is hypothesized to predispose to pro-atherogenic profile and large vessel inflammation [4,5,6], sustaining an ongoing generalized inflammatory autoimmune diathesis.
The mechanism leading to increase CVD seems to be due to systemic inflammation and insulin resistance, with subsequent endothelial dysfunction that would predispose to atherosclerosis and finally to major cardiac events, such as myocardial infarction and stroke [7,8,9,10].
In children, metabolic conditions linked with increased CVD, such as obesity, systemic hypertension, hyperlipidaemia, diabetes mellitus, metabolic syndrome, have been associated with psoriasis [11,12,13,14,15,16,17,18,19].
In adults, carotid intima media thickness (cIMT) represents a well-established early marker of atherosclerosis in the pre-clinical stages and CVD: in moderate to severe cutaneous psoriasis it is significantly increased compared to controls [20,21,22,23,24,25] and it positively correlates with lipid profile [26]. Compared to controls, in psoriatic patients flow-mediated dilation, a marker of endothelial status, is not significantly impaired possibly suggesting a pathogenic mechanism of endothelial injury other than nitric oxide-mediated dysfunction [27,28,29], In addition, coronary artery calcification, another marker of CVD, is increased in adults with plaque type psoriasis [30].
All this considering, adults with psoriasis should be monitored for CVD risk especially when the disease is severe and long-lasting [31].
In children, psoriasis is associated with metabolic conditions linked with increased CVD, such as obesity, central adiposity [32], systemic hypertension, hyperlipidaemia, diabetes mellitus, metabolic syndrome, non-alcoholic fatty liver disease [7,8,9,10,11,12,13,14,15,16,17, 33].
Despite these findings, few studies have precisely focused on cardiovascular involvement and increased risk for CVD in children with psoriasis. The published works found left ventricular dysfunction, heart failure [33, 34].
Because psoriasis begins in childhood in almost one-third of patients, early identification of CV risk may be crucial: an early intervention could modify the progression of CVD from the very beginning of the disease in a pre-clinical stage.
Consequently recommendations have proposed for routine screening in paediatric patients with psoriasis to early identify and monitor CV risk factors in order to minimize health effects over a lifetime [18].
The early identification of cardiovascular involvement could help the clinicians to monitor the disease and treat it to stop its progression.
The primary aim of this study was to assess cardiac and vascular involvement in affected children compared to healthy controls in order to early detect a marker of CV impairment. Secondary aim was to investigate the potential association of psoriasis with serological and anthropometric markers of metabolic syndrome, known risk factors for CVD, since metabolic syndrome is strictly linked to CVD.
Materials and Methods
Selection of Groups
We performed a monocentric, prospective, case–control study from August 2018 to September 2019.
Considering a mean prevalence of 1.1% [1] of psoriasis, an error margin of 5% with a confidence interval (CI) of 95%, we obtained a representative sample of population as follows:
We enrolled patients affected by psoriasis (group A) followed as outpatients by Pediatric Dermatology Department. Inclusion criteria included: age between 1 month and 18 years, paediatric onset of disease, acquisition of consent by patient’s parents/guardians[32]. Patients with chronic diseases or syndromes, secondary arterial hypertension, diabetes, or lipidic metabolism disorders were excluded.
For each of the selected patients, PASI (Psoriasis Area Severity Index) and BSA (Body Surface Area) affected by psoriasis were assessed by dermatologist, in order to define severity of disease, i.e. PASI > 10 or BSA > 10% [34].
We recruited age and sex-matched case controls without dermatological diseases including psoriasis, chronic diseases or syndromes (group B). These subjects were selected among hospitalized patients in Emergency Pediatric Department for acute illness or scheduled minor surgery.
Clinical and Laboratory Evaluation
Group A and B were screened for personal and familiar risk factors for CVD, included adiposity and its distribution, blood pressure and metabolic profile. They performed blood exams screening for metabolic syndrome, specifically cholesterol (total, HDL), triglycerides (TGR), fasting glucose (FG), glycated haemoglobin (HbA1c). LDL cholesterol was calculated according to Friedewald equation. A complete clinical evaluation was performed by paediatric cardiologist.
Demographic and anthropometric parameters (age, sex, ethnicity, height, weight, waist circumference (WC), body mass index (BMI), body shape index (ABSI) and waist/height ratio), patients’ disease duration (i.e. time from the time of diagnosis to the time of enrolment), personal (birth gestational age and weight, history of intra-uterine growth restriction (IUGR), perinatal morbidity, or cardiovascular and urologic diseases, smoke or alcohol habits, current pharmacotherapy) and familiar (psoriasis, metabolic, renal or cardiovascular diseases) risk for CVD were recorded.
Based on BMI, overweight was defined when > 85th percentile for age and sex, obesity when > 95th percentile for age and sex [35, 36]. Waist/height ratio is associated with risk for CVD when the ratio > 0.5 [37].
For each patients systolic (SBP) and diastolic arterial blood pressure (DBP) were measured with auscultatory method and expressed as absolute value and percentiles according to 2016 European Society of Hypertension [38]. Hypertension (HTN) was defined when SBP and/or DBP were at least 95th percentile for sex, age and height measured on at least three separate occasions, high-normal BP when the average SBP and/or DBP was at least 90th and less than 95th for children younger than 16 years-old. For boys and girls who were 16 year-old or older, BP was defined HTN was defined if 140/90 mmHg and high-normal if 130–139/85–89 mmHg but less than 140/90 mmHg.
Echocardiography and Vascular Echography
All subjects underwent echocardiography, transcranial echo-Doppler (TCD) and carotid artery echo-Doppler and intima-media thickness measurement (cIMT).
Echocardiography and TCD were performed by an expert paediatric cardiologist using a Philips IE33 ultrasound machine with S5-1 Phased Array Ultrasound Probe. All measurements were performed on 3 consecutive cardiac cycles. The paediatric cardiologist reviewed all the images acquired. Left chambers dimensions (interventricular septal width in end diastole, IVSD; left ventricle end-diastole diameter, LVEDD; posterior wall thickness at end diastole, PWD; left atrium volume, LA), biventricular systolic function (fractional shortening, FS%; tricuspid annular plane systolic excursion, TAPSE), left ventricle diastolic function (early diastolic filling wave, E; late diastolic filling wave, A and E/A ratios) and aortic dimensions (aortic root, root Ao; LA/Ao Root), left ventricular mass (left ventricular mass indexed to height, LVMI/h2.7) and geometry (relative wall thickness, RWT) were collected.
Transcranial Doppler (TCD) ultrasonography was obtained using transtemporal window, using a low frequency ultrasound probe (2 MHz in average) placed over the insonation windows to study bilateral middle cerebral artery (MCA) mean flow velocities.
cIMT, peak velocity of blood flow, resistivity index (RI) measurement were performed using ultrasound technique while the subject was in a supine position with the neck rotated (45°) to the side opposite to the undergoing examination. Mean cIMT measured from carotid ultrasound was obtained d in a standard manner according to the Mannheim cIMT [39] consensus. In brief, using a high-definition linear probe (High Linear Probe 7.5 MhZ, DC-T6 Diagnostic Ultrasound System Maindray), the intima-media thicknesses of the carotid arteries on both sides were evaluated through longitudinal projection. The measurement was carried out 1 cm before the bifurcation of the common carotid artery, at the level of the posterior wall of the vessel. cIMT was defined as the distance between the leading edge of the lumen-intima interface and the media-adventitia interface of the posterior wall measured during diastole. Three measurements were made on each side in order to obtain the average value. All measurements were performed by a single operator.
Informed Consent and Study Approval
All legal representatives of the children provided written informed consent before examination. The study was approved by the Ethics Committee of the Sant’Orsola-Malpighi Hospital (Approval Number 232/2018/Sper/AOUBo).
Statistical Analysis
Data were plotted in electronic database (©Excel) and analysed through Statistical Package for Social Sciences 17 (©SPSS). Quantitative variables were described by mean and standard deviation. Qualitative variables were described as frequencies and percentages. Since our groups were composed of less than 30 subjects, Kolmogorov–Smirnov test was used to test the normality of the distribution for each quantitative variable, to decide using parametrical or non-parametrical tests. We compared the two groups by t test for independent samples for quantitative variables with normal distribution, by Mann–Whitney test for quantitative variables without normal distribution, and by Chi-square test for qualitative variables. Pearson correlation coefficient was used to evaluate association between quantitative variables; Ro-Spearman correlation coefficient used to evaluate association between qualitative variables and quantitative variables with or without normal distribution. We, then, performed linear regression models.
A p value < 0.05 was considered statistically significant.
Results
We enrolled 20 subjects for group A (7 boys, mean age, 10.72 ± 4.63 years), and 20 age- and sex-matched controls for group B (8 boys, mean age, 10.66 ± 3.51 years). Demographic and anthropometric data, family and personal risk factors for CVD, blood pressure and laboratory exams are displayed in Table 1.
Anthropometric data and personal history, particularly risk factors for CVD, were comparable between the two groups. Family history was significantly different for the presence of psoriasis (p < 0.02) in group A.
Group A had a mean age at diagnosis of 8.82 ± 4.68 years, mean duration of disease of 22.1 ± 14.24 months. Fifteen out of 20 (65%) cases presented plaque psoriasis, 2/20 (10%) persistent guttate psoriasis, 4/20 (20%) inverse psoriasis and 4/20 (20%) nail psoriasis. Most involved skin sites were scalp in 12/20 (60%), both trunk and extremities in 10/20 (50%), face in 8/20 (40%), nail and genital mucosae in 4/20 (20%), respectively. The mean value of PASI was 2.64 ± 2.6 SD and BSA affected by psoriasis was 5.46 ± 7.5 SD, corresponding to a mild degree of severity. Three of 20 (15%) received systemic therapy with cyclosporine, switched to guselkumab in 2; 18 (90%) received topical therapy (corticosteroids, calcipotriol, urea, pimecrolimus, salicylic acid individually or in combination).
BP values were not significantly different between the two groups. Systolic HTN was found in 1 patient (5%) and high-normal SBP in 1 (5%) in group A, diastolic HTN in 3/20 (15%) of group A and 2/20 (10%) of group B, high-normal DBP in 1 patient for each group (5%).
Among the metabolic markers, HDL-cholesterol and triglycerides, despite within normal values, were significantly different between the two groups (p = 0.021 and p = 0.046, respectively).
Cardiac and vascular echographic data are shown in Table 2. Cardiac dimensions and systo-diastolic function were normal and similar between the two groups, such as LV mass and geometry, LA dimensions, and global RV function. Blood flow velocities in carotid arteries and mean cerebral arteries were comparable. In addition peak and mean flow velocities in carotid arteries did not correlate with SBP nor DBP.
On the opposite, right and left cIMT were normal but significantly thinner in Group B (respectively p = 0.001 and p = 0.002).
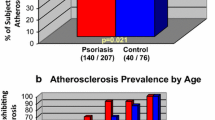
Through a linear regression model, we found a positive correlation between the disease duration (expressed as years of active disease) and cIMT (dependent variable) (Fig. 1), but none with anthropometric data (weight and abdominal circumference, WC/height, BMI), BSA affected by psoriasis, PASI, SPB and DBP. c-IMT was positively correlated with TRG and TRG/glucose ratio in Group A (Fig. 2).
We documented an inverse correlation between BMI and BSA affected by psoriasis (Fig. 3).
Furthermore, since the significant difference of c-IMT bilaterally between the groups, we tried to find a cut-off to distinguish healthy from affected subjects that could help to start a personalized program to limit the progression to CVD. We considered the worse value between left and right c-IMT and calculated for this new variable the quartile distribution for both cohorts. The quartile distributions of the two groups are characterized by opposite trends, which cross each other at the second quartile, corresponding to c-IMT = 0.53 mm (Fig. 4).
Discussion
Our findings showed a significant increase of c-IMT bilaterally in psoriatic children compared with controls, despite the absolute values of the c-IMT were normal in both.
In addition, c-IMT increases over time after diagnosis and it is positively related with markers of metabolic syndrome, particularly triglycerides and triglycerides/glucose.
Our findings are important because in adult patients cIMT is a recognized early marker of atherosclerosis and cardiovascular risk [25, 26, 31], and several studies have demonstrated the association between psoriasis and higher cIMT. Furthermore, c-IMT measurements are easy to do, safe and non-invasive technique, so easy to perform in paediatric age group. Thus, c-IMT could represent the first tool to monitor psoriatic young patients over time.
Moreover, despite c-IMT was normal in all patients, it seems that in our population, a measure of c-IMT of 0.53 mm could represent a value to distinguish subjects with psoriasis from controls, and that, despite normal, could contribute to drive the personalized management and monitoring of patients. Further larger studies are mandatory to support our findings.
Surprisingly, the lipidic profile, within normal range in all subjects of both cohorts, was however more “protective” with higher HDL-cholesterol and lower triglycerides in psoriatic children than in controls. These results could be explained, by one side, by the short duration and mild severity of the disease in our cohort, and, by the other, by the increased awareness of CVD in this population and consequent a tendency to healthy lifestyle. Since we would have expected a “worse” lipid profile in psoriatic patients as the basis of early atherogenesis in this condition, we hypothesize that the psoriasis itself might increase cIMT [28].
Cardiac involvement was not detected in our cohorts, where all echocardiographic measurements were normal. In addition, systo-diastolic function, dimensions, mass and geometry of left ventricle were comparable with healthy controls, and they were not related with metabolic pattern nor BP. Our results differ from those published by Cevik et al. [40] that found bigger LV diameters in psoriatic children compared to healthy, comparable systolic, but impaired diastolic function. The discrepancy can partially be due to the differences between the recruited populations: our patients had a shorter duration of the disease and are younger compared to Turkish Cohort (respectively mean age 10.72 ± 4.63 versus 14.2 ± 0.89 years [40]). Abnormalities of left ventricle could occur at a later stage of disease, while cIMT could be the first and earliest marker of CVD.
Transcranial Doppler (TCD) ultrasonography provides a non-invasive real-time measurement of blood flow characteristics and cerebrovascular hemodynamics within the basal arteries of the brain, and it represents an easily, non-irradiant way to monitor vascular changes. In children it is a well-recognized tool to identify those subject at risk for cerebrovascular accidents in sickle cell disease [41]. We applied this modality to study cerebral vessels in the psoriatic population to see if it could detect vascular involvement and correlate with blood pressure. In our cohort, TCD did not evidence any significant differences in blood flow characteristics in middle cerebral artery in affected and healthy children and did not correlate with pressure nor metabolic panel.
Differently from psoriatic adults, our patients had familiar and personal risks for CV diseases, including anthropometric data, distribution of adiposity and systolic and diastolic blood pressures, comparable with healthy subjects, and the metabolic panel was normal. We found a positive familiar history for psoriasis in 35% of affected children, according with literature reporting it in 32.71–48.8% of cases [1, 17].
Conflictual data have, indeed, been published [14, 17, 18, 33] about the association of adiposity and metabolic syndrome. In our psoriatic patients’ anthropometric data, fat distribution and blood values were not correlated with metabolic syndrome. Furthermore, they had normal weight and mean blood pressure, despite 7/20 (35%) had altered blood pressure absolute values, in line with findings by Fortina et al. [12].
Surprisingly, the area of the body affected by psoriasis, expressed by the BSA, was inversely correlated with the body mass index (BMI), and not with the parameters of central obesity, such as body shape index (ABSI), waist/height ratio and waist circumference, in contrast with previous studies that report an increase of central obesity increases for each year of psoriasis duration [18, 32]. These findings could be partially due to the relative homogeneity of disease severity in our patients and awareness of lifestyle and dietary habits, in addition to the younger age and shorted disease the duration of our patients.
Since early identification of subjects at risk for CVD could modify the natural history of atherogenesis progression and prolong the life expectancy, further studies are needed to support the role of c-IMT in psoriatic young patients and a longitudinal cardiovascular follow-up. The screening should include cardiac US and cIMT beside the lipid profile.
There are some limitations in our study: firstly, the small sample size mainly due to the extreme rarity of the disease in paediatric age, and secondly the relative homogeneity of the disease, generally characterized by mild severity and short duration.
Conclusions
This is the first report identifying c-IMT as a marker of vascular involvement in children with psoriasis from the very early stage of the disease, when serological metabolic panel and cardiac measurements and left ventricular geometry and mass are still normal.
C-IMT could contribute to drive a personalized pharmacological and non-pharmacological management, together with echocardiography and metabolic panel.
Longitudinal studies are needed to study the progression of cardiovascular involvement when psoriasis begins in early ages.
Data Availability
Individual participant data will not be available due to confidentiality. Database with anonymous data will be available if requested.
Code Availability
Not applicable.
Abbreviations
- ABSI:
-
A body shape index
- BMI:
-
Body mass index
- BSA:
-
Body Surface Area
- CI:
-
Confidence interval
- cIMT:
-
Carotid intima media thickness
- CV:
-
Cardiovascular
- CVD:
-
Cardiovascular diseases
- DBP:
-
Diastolic blood pressure
- FG:
-
Fasting glucose
- FS%:
-
Fractional shortening
- HbA1c:
-
Glycated haemoglobin
- HDL:
-
High density lipoprotein
- HTN:
-
Hypertension
- IUGR:
-
Intra uterine growth restriction
- IVSD:
-
Interventricular septal width in end-diastole
- LA:
-
Left atrium volume
- LDL:
-
Low density lipoprotein
- LV:
-
Left ventricular
- LVEDD:
-
Left ventricle end-diastole diameter
- LVMI/h2.7:
-
Left ventricular mass indexed to height
- MCA:
-
Middle cerebral artery
- PASI:
-
Psoriasis Area Severity Index
- PWD:
-
Posterior wall thickness at end-diastole
- RI:
-
Resistivity index
- RWT:
-
Relative wall thickness
- SBP:
-
Systolic blood pressure
- TAPSE:
-
Tricuspid annular plane systolic excursion
- TCD:
-
Transcranial echo-Doppler
- TGR:
-
Triglycerides
- US:
-
Ultrasound
- WC:
-
Waist circumference
References
Burden-Teh E, Thomas KS, Ratib S, Grindlay D, Adaji E, Murphy R (2016) The epidemiology of childhood psoriasis: a scoping review. Br J Dermatol 174(6):1242–1257. https://doi.org/10.1111/bjd.14507
Armstrong EJ, Harskamp CT, Armstrong AW (2013) Psoriasis and major adverse cardiovascular events: a systematic review and meta-analysis of observational studies. J Am Heart Assoc. https://doi.org/10.1161/JAHA.113.000062
Samarasekera EJ, Neilson JM, Warren RB, Parnham J, Smith CH (2013) Incidence of cardiovascular disease in individuals with psoriasis: a systematic review and meta-analysis. J Invest Dermatol 133(10):2340–2346. https://doi.org/10.1038/jid.2013.149
Li W, Han J, Hu FB, Curhan GC, Qureshi AA (2012) Psoriasis and risk of type 2 diabetes among women and men in the United States: a population-based cohort study. J Invest Dermatol 132(2):291–298. https://doi.org/10.1038/jid.2011.319
Mehta NN et al (2012) Abnormal lipoprotein particles and cholesterol efflux capacity in patients with psoriasis. Atherosclerosis 224(1):218–221. https://doi.org/10.1016/j.atherosclerosis.2012.06.068
Sunitha S et al (2015) Comprehensive lipid tetrad index, atherogenic index and lipid peroxidation: surrogate markers for increased cardiovascular risk in psoriasis. Indian J Dermatol Venereol Leprol 81(5):464–471. https://doi.org/10.4103/0378-6323.163734
Osier E et al (2017) Pediatric psoriasis comorbidity screening guidelines. JAMA Dermatol 153(7):698–704. https://doi.org/10.1001/jamadermatol.2017.0499
Torres T, Machado S, Mendonça D, Selores M (2014) Cardiovascular comorbidities in childhood psoriasis. Eur J Dermatol 24(2):229–235. https://doi.org/10.1684/ejd.2014.2291
Boehncke WH, Boehncke S, Tobin AM, Kirby B (2011) The ‘psoriatic march’: a concept of how severe psoriasis may drive cardiovascular comorbidity. Exp Dermatol 20(4):303–307. https://doi.org/10.1111/j.1600-0625.2011.01261.x
Kwa L, Kwa MC, Silverberg JI (2017) Cardiovascular comorbidities of pediatric psoriasis among hospitalized children in the United States. J Am Acad Dermatol 77(6):1023–1029. https://doi.org/10.1016/j.jaad.2017.08.034
Miller IM, Skaaby T, Ellervik C, Jemec GBE (2013) Quantifying cardiovascular disease risk factors in patients with psoriasis: a meta-analysis. Br J Dermatol 169(6):1180–1187. https://doi.org/10.1111/bjd.12490
Caroppo F, Ventura L, Belloni Fortina A (2019) High blood pressure in normal-weight children with psoriasis. Acta Derm Venereol 99(3):329–330. https://doi.org/10.2340/00015555-3076
Augustin M, Glaeske G, Radtke MA, Christophers E, Reich K, Schäfer I (2010) Epidemiology and comorbidity of psoriasis in children. Br J Dermatol 162(3):633–636. https://doi.org/10.1111/j.1365-2133.2009.09593.x
Jensen P, Zachariae C, Iversen L, Hansen PR, Skov L (2014) Cardiovascular risk factors in children and adolescents with psoriasis: a case-control study. Acta Derm Venereol 94(1):76–78. https://doi.org/10.2340/00015555-1607
Paller AS et al (2013) Association of pediatric psoriasis severity with excess and central adiposity: an international cross-sectional study. JAMA Dermatol 149(2):166–176. https://doi.org/10.1001/jamadermatol.2013.1078
Stefanaki C et al (2011) Psoriasis in children: a retrospective analysis. J Eur Acad Dermatol Venereol 25(4):417–421. https://doi.org/10.1111/j.1468-3083.2010.03801.x
Kelati A, Baybay H, Najdi A, Zinoune S, Mernissi FZ (2017) Pediatric psoriasis: should we be concerned with comorbidity? Cross-sectional study. Pediatr Int 59(8):923–928. https://doi.org/10.1111/ped.13309
Guidolin L, Borin M, Fontana E, Caroppo F, Piaserico S, Belloni Fortina A (2018) Central obesity in children with psoriasis. Acta Dermato Venereol 98(2):282–283. https://doi.org/10.2340/00015555-2816
Tollefson MM, Van Houten HK, Asante D, Yao X, Kremers HM (2018) Association of psoriasis with comorbidity development in children with psoriasis. JAMA Dermatol 154(3):286–292. https://doi.org/10.1001/jamadermatol.2017.5417
Yiu KH et al (2013) Prevalence and extent of subclinical atherosclerosis in patients with psoriasis. J Intern Med 273(3):273–282. https://doi.org/10.1111/joim.12002
Arias-Santiago S et al (2012) Atheroma plaque, metabolic syndrome and inflammation in patients with psoriasis. Eur J Dermatol 22(3):337–344. https://doi.org/10.1684/ejd.2012.1714
Balci DD et al (2009) Increased carotid artery intima-media thickness and impaired endothelial function in psoriasis. J Eur Acad Dermatol Venereol 23(1):1–6. https://doi.org/10.1111/j.1468-3083.2008.02936.x
El-Mongy S et al (2010) Subclinical atherosclerosis in patients with chronic psoriasis: a potential association. J Eur Acad Dermatol Venereol 24(6):661–666. https://doi.org/10.1111/j.1468-3083.2009.03481.x
Enany B, El Zohiery AK, Elhilaly R, Badr T (2012) Carotid intima-media thickness and serum leptin in psoriasis. Herz 37(5):527–533. https://doi.org/10.1007/s00059-011-3547-z
Troitzsch P et al (2012) Psoriasis is associated with increased intima-media thickness-The Study of Health in Pomerania (SHIP). Atherosclerosis 225(2):486–490. https://doi.org/10.1016/j.atherosclerosis.2012.09.026
Antonucci VA, Tengattini V, Balestri R, Patrizi A, Filippini M, Bardazzi F (2014) Intima-media thickness in an Italian psoriatic population: correlation with lipidic serum levels, PASI and BMI. J Eur Acad Dermatol Venereol 28(4):512–515. https://doi.org/10.1111/jdv.12075
Martyn-Simmons CL et al (2011) A prospective case-controlled cohort study of endothelial function in patients with moderate to severe psoriasis. Br J Dermatol 164(1):26–32. https://doi.org/10.1111/j.1365-2133.2010.10031.x
Ulusoy RE, Karabudak O, Yokusoglu M, Kilicaslan F, Kirilmaz A, Cebeci BS (2010) Noninvasive assessment of impaired endothelial function in psoriasis. Rheumatol Int 30(4):479–483. https://doi.org/10.1007/s00296-009-0995-3
Usta M et al (2011) Vascular endothelial function assessed by a noninvasive ultrasound method and serum asymmetric dimethylarginine concentrations in mild-to-moderate plaque-type psoriatic patients. Clin Biochem 44(13):1080–1084. https://doi.org/10.1016/j.clinbiochem.2011.06.007
Ludwig RJ et al (2007) Psoriasis: a possible risk factor for development of coronary artery calcification. Br J Dermatol 156(2):271–276. https://doi.org/10.1111/j.1365-2133.2006.07562.x
S. Shaharyar et al., “Subclinical cardiovascular disease in plaque psoriasis: Association or causal linkα,” Atherosclerosis, vol. 232, no. 1. Elsevier Ireland Ltd, pp. 72–78, 2014, doi: https://doi.org/10.1016/j.atherosclerosis.2013.10.023.
Badaoui A, Tounian P, Mahé E (2019) Psoriasis and metabolic and cardiovascular comorbidities in children: a systematic review. Arch Pediatr 26(2):86–94. https://doi.org/10.1016/j.arcped.2018.12.005
Flynn JT et al (2017) Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics. https://doi.org/10.1542/peds.2017-1904
Finlay AY (2005) Current severe psoriasis and the Rule of Tens. Br J Dermatol 152(5):861–867. https://doi.org/10.1111/j.1365-2133.2005.06502.x
Freedman DS, Mei Z, Srinivasan SR, Berenson GS, Dietz WH (2007) Cardiovascular risk factors and excess adiposity among overweight children and adolescents: The Bogalusa Heart Study. J Pediatr. https://doi.org/10.1016/j.jpeds.2006.08.042
Leone A et al (2020) Evaluation of different adiposity indices and association with metabolic syndrome risk in obese children: is there a winner? Int J Mol Sci. https://doi.org/10.3390/ijms21114083
Ashwell M, Hsieh SD (2005) Six reasons why the waist-to-height ratio is a rapid and effective global indicator for health risks of obesity and how its use could simplify the international public health message on obesity. Int J Food Sci Nutr 56(5):303–307. https://doi.org/10.1080/09637480500195066
Lurbe E et al (2016) 2016 European Society ofHypertension guidelines for themanagement of high blood pressure in children and adolescents. J Hypertens 34(10):1887–1920. https://doi.org/10.1097/HJH.0000000000001039
Touboul PJ et al (2012) Mannheim carotid intima-media thickness and plaque consensus (2004–2006-2011). An update on behalf of the advisory board of the 3rd, 4th and 5th watching the risk symposia, at the 13th, 15th and 20th European Stroke Conferences, Mannheim, Germany, 2004, Brussels, Belgium, 2006, and Hamburg, Germany, 2011. Cerebrovasc Dis 34(4):290–296. https://doi.org/10.1159/000343145
Çevik BS, Akalin F, Erolu E, Gençosmanoğlu S, Ergun T (2019) Assessment of cardiac and vessel functions in childhood psoriasis. Turk J Med Sci 49(2):617–623. https://doi.org/10.3906/sag-1812-139
Purkayastha S, Sorond F (2012) Transcranial doppler ultrasound: technique and application. Semin Neurol 32(4):411–420. https://doi.org/10.1055/s-0032-1331812
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
MF conceptualized and designed the study, coordinated and supervised data collection, drafted the initial manuscript, and reviewed and revised the manuscript. MAC and DP conceptualized and designed the study, collected data and carried out statistical analysis, drafted the initial manuscript, and reviewed and revised the manuscript. AD and AG collected data and carried out statistical analysis, and reviewed and revised the manuscript. AP and FB coordinated and supervised data collection, and reviewed and revised the manuscript. AR and EF designed the data collection instruments, and review and revised the manuscript. IN and ML conceptualized and designed the study, drafted the initial manuscript, and reviewed and revised the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest relevant to this article to disclosure.
Ethical Approval
The study was approved by the Ethics Committee of the Sant’Orsola-Malpighi Hospital (Approval Number 232/2018/Sper/AOUBo).
Consent to Participate
All legal representatives of the children provided written informed consent before examination.
Consent for Publication
All legal representatives of the children provided written informed consent to publication of data anonymously.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fabi, M., Chessa, M.A., Panizza, D. et al. Psoriasis and Cardiovascular Risk in Children: The Usefulness of Carotid Intima-Media Thickness. Pediatr Cardiol 43, 1462–1470 (2022). https://doi.org/10.1007/s00246-022-02869-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-022-02869-1