Abstract
The objective of this analysis was to update trends in LOS and costs by survivorship and ECMO use among neonates with hypoplastic left heart syndrome (HLHS) undergoing stage 1 palliation surgery using 2016 data from the Healthcare Cost and Utilization Project Kids’ Inpatient Database. We identified neonates ≤ 28 days old with HLHS undergoing Stage 1 surgery, defined as a Norwood procedure with modified Blalock–Taussig (BT) shunt, Sano modification, or both. Multivariable regression with year random effects was used to compare LOS and costs by hospital region, case volume, survivorship, and ECMO vs. no ECMO. An E-value analysis, an approach for conducting sensitivity analysis for unmeasured confounding, was performed to determine if unmeasured confounding contributed to the observed effects. Significant differences in total costs, LOS, and mortality were noted by hospital region, ECMO use, and sub-analyses of case volume. However, other than ECMO use and mortality, the maximum E-value confidence interval bound was 1.71, suggesting that these differences would disappear with an unmeasured confounder 1.71 times more associated with both the outcome and exposure (e.g., socioeconomic factors, environment, etc.) Our findings confirm previous literature demonstrating significant resource utilization among Norwood patients, particularly those undergoing ECMO use. Based on our E-value analysis, differences by hospital region and case volume can be explained by moderate unobserved confounding, rather than a reflection of the quality of care provided. Future analyses on surgical quality must account for unobserved factors to provide meaningful information for quality improvement.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
According to the Centers for Disease Control and Prevention (CDC), hypoplastic left heart syndrome (HLHS) affects one of every 4344 infants born each year, or approximately 2–3 cases per 10,000 live births in the USA (960 births per year) [1]. While there is no corrective treatment for HLHS, patients undergo a three-stage surgical approach to provide a unique circulatory blood flow to the heart and lungs [2]. Stage 1 palliation surgery (Norwood procedure) establishes systemic blood flow from the single right ventricle and pulmonary blood flow from the right ventricle or through an arterial shunt. The subsequent surgical stages result in a unique circulation of direct passive venous return to the lungs and a single right heart chamber pumping systemic blood flow to the body. Despite improved survival with surgery, these patients experience significant morbidity and mortality associated with their condition [3,4,5,6,7]. Studies of resource utilization among Norwood patients in nationally representative samples have shown that these patients incur significant cost and length-of-stay (LOS) burdens with mixed survival outcomes dependent on factors such as hospital volume, teaching vs. nonteaching hospitals, surgeon volume, and geographic region [8,9,10,11,12,13,14,15,16]. In addition, studies do not consistently report extracorporeal membrane oxygenation (ECMO) use in the Norwood population, an important driving factor of cost and LOS, or had a small sample size [17,18,19]. Unsurprisingly, ECMO use is associated with an increased risk for death [20] with a survival rate of just 36% in Stage 1 Norwood patients utilizing ECMO support [21]. Additional factors may also affect cost, LOS, and mortality outcomes. In this paper, we update previous analyses on HLHS neonates undergoing Stage 1 palliation surgery and focus on differences in healthcare resource utilization and the role of ECMO between in-hospital survivors and non-survivors, as well as validate previous findings on predictors of LOS and cost. We further quantify the extent to which unmeasured factors may explain these differences and predictors using a novel statistic called the E-value.
Methods
We analyzed the Health Care Cost and Utilization Project (HCUP) Kids’ Inpatient Database (KID) data from 2003, 2006, 2009, 2012, and 2016. Every 3 years, the KID collects a national cross-sectional sample of inpatient discharges for patients ≤ 20 years of age from more than 4100 hospitals in the USA, including community-based, non-rehabilitation, and stand-alone pediatric hospitals from 44 states. Discharge weights are provided by HCUP to convert sample values into national estimates of inpatient visits. HCUP collects data on total charges billed to CMS for a hospital encounter, and these are converted to costs using the HCUP Cost-to-Charge Ratio Files, which are specific to year, database, and adjusted for area wage index and hospital characteristics, including state, urban/rural, investor-owned/other, and number of beds [22]. We chose to focus on the time period starting in 2003 due to the significant improvements in surgical technique and outcomes resulting from palliative surgery starting in the early 2000s, and because the charge-to-cost multiplier for KID is only available from 2003 onwards [5, 17, 22, 23].
We identified neonates ≤ 28 days diagnosed with HLHS using ICD9 code 746.7 or ICD10 code Q234. Surgical admissions were identified as Stage 1 Norwood with Blalock-Taussig (BT) shunt (ICD-9-CM code 39.0 and all corresponding ICD-10-PCS codes), Sano modification (SANO) (ICD9 code 35.92 and all corresponding ICD10 codes), or with both BT shunt and Sano modification. Because of concerns about inaccurate ICD10 coding of shunt type, we did not include this as a separate covariate in our primary analyses, but we performed a subsequent sensitivity analysis to test the effect of shunt type on cost and LOS. We did not include other types of Stage 1 palliative surgery besides Norwood because these were not reliably identifiable using ICD codes. We also focused only on the first stage because the KID does not report patient data longitudinally, and thus limits the ability to track patients’ subsequent surgeries to model their long-term outcomes.
Patient demographics including gender, race/ethnicity, insurance type, income quartile based on family median income, complex chronic conditions, and comorbidities were examined as predictors of LOS and total hospital cost per encounter (Table 1). Per HCUP, the variable for median income provides a quartile classification derived from annual ZIP code-demographic data [24]. Additional clinical variables such as gestational age and birthweight were not included due to the high proportion (> 90%) of missing data for each variable in the KID. Insurance type was stratified as either government (Medicare/Medicaid), private (including HMO), or other (self-pay, no charge, worker’s compensation, CHAMPUS, CHAMPVA, and other government programs). Hospital LOS was analyzed as a continuous variable. Total hospital costs were adjusted to 2016 US dollars based on the Medical Consumer Price Index from the US Bureau of Labor Statistics. Patient comorbidities included heterotaxy, chromosomal abnormalities, and congenital syndromes consistent with the comorbid conditions reported in the Society for Thoracic Surgeons (STS) database, and considered via expert and literature review to be the most relevant to or associated with HLHS (Supplemental Table 1) [25]. Complex chronic conditions (CCCs) were included based on previously published guidelines, with individuals stratified as having 1, 2, or 3 + conditions. Pre-operative conditions were not identified as such as the HCUP does not timestamp diagnoses. We also identified any patients undergoing ECMO during their hospitalization with the ICD code for ECMO use. We did not explicitly look at outcomes by shunt type (BT vs. Sano) due to inconsistencies in ICD9 coding prior to 2016, and inconsistent mapping to ICD10 codes in the 2016 data.
Hospital characteristics examined included case volume, hospital region, and hospital location (Table 2). Case volume cutoffs were modeled after those used by the STS database. Geographic regions were classified as Northeast, Midwest, West and South. Per HCUP, rural hospitals are not split according to teaching status, because rural teaching hospitals are rare.
All analyses were completed using SAS 9.4 (SAS Institute, Cary, NC). All analyses were completed on hospital discharges, as HCUP only identifies unique hospitalization encounters, not patients. Pearson’s χ2 and Fisher’s Exact Test were used to compare characteristics between survivors and non-survivors and ECMO vs. non-ECMO users. Wilcoxon’s Rank Sum Test was used to compare continuous variables such as LOS and total hospital cost.
Finally, because we were limited to a narrow set of observable variables available in the data, we calculated E-values for predictors of mortality and ECMO use to determine the impact of treatment selection bias and potential unmeasured confounding variables on our results [26]. The E-value addresses how strong unmeasured confounding would have to be to negate the observed results by calculating a value based on: (1) the strength of the association between an unmeasured confounder and the exposure group, and (2) the strength and association of the unmeasured confounder with the outcome. This is interpreted as a relative risk ratio [26]. For example, an E-value = 2 means that an unmeasured confounder that (1) doubles the risk of the outcome, and (2) is twice as prevalent in the exposed vs. unexposed group, can explain away the observed association conditional on the observables included in the model, regardless of a p-value indicating statistical significance [27]. Conversely, a very high E-value relative to the point estimate may imply that the observed effect is in fact plausible, because the strength and association of the unmeasured confounder with the exposure group and outcome must be very high to negate the observed effect. E-values were calculated using the R package “E-Value” provided by the E-value creators [27].
Results
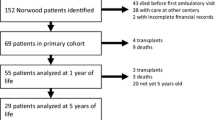
We identified 2,872 Norwood admissions among HLHS patients over five years (2003, 2006, 2009, 2012, 2016). Nearly two-thirds of patients were male, and > 50% White Non-Hispanic. The number of Norwood procedures increased throughout our study period, with most patients receiving their Norwood at a center performing ≥ 11 procedures per year. The mortality rate consistently decreased since 2003, from 28.3% to 14.1% in 2016 (p < 0.001), while the complexity of patients, as measured by number of CCCs, increased over time. There was an overall increase in LOS from a median of 26 days to 37 days in 2012, but this dropped to 22 days in 2016. Despite the drop in LOS in 2016, total encounter cost increased nearly threefold, from a median (IQR) of $81,281 ($47,764–114,661) in 2003, to $231,351 ($151,136–391,282) in 2016. ECMO use also increased over time, from 10.2% of encounters in 2003 to 17.3% in 2016 (p = 0.004). Patients with comorbid conditions made up a quarter of all encounters, with the most common comorbid condition being heterotaxy (Supplemental Table 1). Because our analysis was on a cohort of individuals with HLHS, by default all had one CCC (cardiovascular), but nearly half had additional CCCs. Although we did not explicitly include shunt type in our analysis due to the limitations described in the “Methods”, we verified that there were no differences in survival between Sano and BT shunt in all years prior to 2016. All trends in demographics, hospital characteristics, LOS, and costs per year of analysis are described in Table 1. Further demographic characteristics by case volume are shown in Supplemental Table 2.
Predictors of LOS and Costs
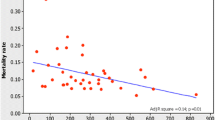
In multivariable analyses to evaluate predictors of LOS, we found that compared to the Northeast, the Midwest and South had significantly longer LOS of 7.69 (p = 0.03) and 11.66 days (p = 0.001) respectively, while LOS in the West was not significantly different (Table 2, Fig. 1). Unsurprisingly, ECMO use was also associated with a longer LOS of 20.23 days (p < 0.0001) and was the most significant predictor of increased LOS along with having 3 + CCCs, which extended LOS by 25.57 days (p < 0.0001) (Fig. 1, Table 3). In contrast, the only predictors of a shorter LOS were having private vs. government insurance, although this did not reach statistical significance (− 4.48 days, p = 0.06), and mortality, which was associated with a shorter LOS by 13.12 days (p < 0.001). We further stratified the analysis to compare ECMO vs. non-ECMO users. Among ECMO users, mortality was highly associated with a shorter LOS (− 35.15 days, p < 0.0001), but this was not seen in non-ECMO users. In fact, the only statistically significant results found for non-ECMO users were hospital region, with the Midwest and South being associated with longer LOS (8.75 and 13.72 days, p = 0.01 and p = 0.0001 respectively), and having 2 + CCCs (10.46 days for 2 CCCs; 25.97 days for 3 + CCCs, p < 0.0001). Case volume significantly impacted only ECMO users, with increased LOS of 17.09 days (p = 0.04) for centers performing 11–25 procedures per year.
Predictors for LOS, cost, mortality, and ECMO use. a Predictors of length of stay. b Predictors of cost. c and d depict odds-ratios for predictors of mortality and ECMO use, respectively. In all figures, the reference group is male, White Non-Hispanic race, government insurance, Northeast, household income 1st quartile, no comorbidities, < 11 cases per year, and 1 CCC. Precise values for each figure are given in Tables 2, 3 and 4
Finally, we stratified the LOS analysis by survivorship, and interestingly found that ECMO use among survivors increased LOS by 35.32 days (p < 0.0001), with no LOS effect on non-survivors. Hispanic survivors also had significantly longer LOS than White Non-Hispanic (7.19 days, p < 0.01), but race did not have any impact on LOS in non-survivors. Only South region and case volume significantly impacted LOS in non-survivors; 26.38 days for the South vs. Northeast (p = 0.04), and 20.64 days for case volume 11–25 (p = 0.01). No impact of case volume was found for survivors. All LOS results are shown in Table 2.
We performed similar analyses on encounter costs. Findings were similar to those for LOS, although not identical. While there were significant increases in hospital costs for the Midwest and South compared to the Northeast ($56,054, p = 0.01 and $49,132, p = 0.02 respectively), having 3 + CCCs ($82,614, p < 0.0001), and ECMO use ($161,929, p < 0.0001) as in the LOS analysis, “Other” insurance and case volume of 11–25 were also significantly associated with increases in encounter costs ($43,468, p = 0.05 and $34,609, p = 0.02 respectively). Further stratification by ECMO use and survivorship yielded interesting results. “Other” insurance played a significant role among ECMO users and non-survivors, with increases in costs of $234,862 (p = 0.002) and $160,336 (p = 0.02) respectively; no effects of insurance type were seen for non-ECMO users and survivors. ECMO users with 2 CCCs or who died also experienced lower costs, with lower costs of $110,216 (p = 0.02) and $96,449 (p = 0.02 respectively. However, non-ECMO users who died experienced an increase in costs ($54,632, p = 0.004), as did those with 3 + CCCs ($78,583, p < 0.0001), in contrast to the cost decreases seen for ECMO users. All hospital regions compared to the Northeast and case volume 11–25 were also associated with increases in cost for non-ECMO users only.
As in the LOS analysis, Hispanic survivors also had higher costs by $39.085 (p = 0.01). Survivors in the Midwest and West, but not South, also had higher costs compared to the Northeast ($57,623, p = 0.01 and $43,727, p = 0.03) respectively. While having 3 + CCCs and using ECMO increased costs for survivors ($93,058, p < 0.0001 and $231,961, p < 0.0001 respectively), these did not impact non-survivors; in fact, having 2 CCCs lowered costs for non-survivors by -$101,977 (p = 0.02). Finally, as with LOS, case volume of 11–25 increased costs among non-survivors only by $105,609 (p = 0.02).
ECMO Use and Mortality
Demographics for ECMO use showed that race, hospital region, case volume, and number of CCCs were significantly different between ECMO and non-ECMO users (Table 4). Mortality was much higher in ECMO users (55.1% vs. 11.9% p < 0.001), as was median LOS and cost (47 vs. 32 days and $256,082 vs. $136,428, p < 0.001 for both). As the KID data are not granular enough to determine when a given comorbid condition was noted during the hospital encounter, we were only able to analyze general associations between various demographic characteristics and ECMO use. We found only that having 3 + CCCs increased the likelihood for ECMO use (OR 1.81, p = 0.004). Comorbidities as defined by STS did not have any effect on ECMO. Hospital region also significantly predicted ECMO use; compared to the Northeast, the Midwest and South were associated with OR 1.88 (p = 0.02) and OR 1.91 (p = 0.02) for ECMO use respectively. Only Hispanic race and being in the 3rd income quartile were associated with less ECMO use, OR 0.66 (p = 0.01) and OR 0.82 (p = 0.04) respectively.
In the mortality model, demographics were overall similar between survivors and non-survivors except gender, race/ethnicity, and ECMO use. ECMO use was most strongly associated with an increased odds of death, OR 12.84 (p < 0.0001). Although weaker, associations were also found with female gender (OR 1.34, p = 0.03), “Other” race/ethnicity (OR 1.82, p = 0.05), and having 3 + CCCs (OR 1.41, p = 0.02). Interestingly, having just 2 CCCs was associated with a lower odds for mortality, OR 0.89 (p = 0.05). Finally, high case volumes > 25 procedures/year were associated with significantly lower mortality, OR = 0.56 (p = 0.01). All demographics and results of the ECMO and mortality analyses are shown in Table 4.
E-Value Analysis
Due to HCUP data being limited to a small number of observable covariates that are consistently reported, we calculated E-values using the odds-ratios from our multivariable models for ECMO and mortality to determine how much unmeasured and unobservable confounders may have impacted our results (Table 4). Specifically, we found low E-values for covariates that had significant p-values for mortality, including number of CCCs and gender, with E-values of 1.66 (CI 1) for 3 + CCCs, and 1.58 (CI 1.16) for female gender. This suggests that the number of CCCs and gender do not necessarily explain mortality, despite an OR 1.41 (p = 0.02). Similarly, the E-value for case volume on mortality was just 2.01 (CI 1.48) despite regression analyses indicating a significant p-value = 0.001, suggesting that only a moderate confounder would explain the difference in mortality by case volume. In contrast, the E-value for the impact of ECMO use on mortality was relatively high at 6.63 (CI 5.67), implying that an unmeasured covariate must have a relative risk ratio of at least 6.34 to attenuate the effect of ECMO on mortality. This result confirms the significant relationship of ECMO to mortality as clinically expected. All E-values with associated confidence interval estimates for mortality and ECMO use predictors are shown in Table 4.
Discussion
Over the last two decades, there has been an increase in the number of HLHS patients undergoing Norwood Surgery, as well as improved survival to 80.8%. This directly correlates with an increase in costs despite a drop in median LOS from 37 days in 2012 to 22 days in 2016. Data from 2000 to 2009 show a survival rate of 78%, while the most recent STS data (2015–2018) show a survival rate of 86.2% for neonates undergoing a Norwood procedure, confirming that surgical outcomes continue to improve over time [28, 29]. The significant drop in LOS in 2016 we can only attribute to potential coding problems with ICD10; reasons for short LOS include early death or transfer, but given the significant IQR of 2–49 days, we believe there may be miscoding errors in some of the ICD10 encounters. Nonetheless, the trend of increased cost and survival rates may reflect findings that higher cost hospitals are associated with a 13.6% reduction in risk-adjusted mortality among children undergoing surgery for congenital heart disease in the USA [30]. Also noted in this study are significant racial and regional differences in survival and ECMO use, which might reflect socioeconomic disparities and/or practice variation that are not captured in administrative data. These confounders limit our ability to draw causal inferences between these outcomes and the covariates included in the analysis.
There were significant differences found in LOS and costs based on hospital region, case volume, survivors vs. non-survivors, and ECMO vs. non-ECMO users. Shorter LOS was associated with those who died prior to discharge, particularly among ECMO users [31]. Compared to all other hospital regions (Midwest, South, West), the Northeast had lower costs and mortality rates among non-ECMO users. This is in contrast to previous analyses with the HCUP KID that showed lower cost hospitals typically have increased mortality rates for children undergoing congenital heart disease surgery. It is unclear whether this is due to differences in patient care or if this reflects regional population differences, such as greater socioeconomic disparities in regions beyond the Northeast. It may also represent a different patient mix with more complex and/or severe congenital comorbidities, although we found no significant findings for income quartile except for ECMO use, and mixed findings for number of CCCs. Because we used administrative CCR data, costs are highly subject to internal accounting, thus the results of the cost analysis may not be completely accurate. We are the first to implement the E-value in our evaluation of the data, and as evidenced by our analysis, statistical significance associated with this finding is likely undermined by unobservable covariates. The plausible explanation is that unmeasured socioeconomic, environmental, and cultural factors likely play a significant role in regional outcome differences. Nonetheless, our findings point to inconsistencies in the delivery of care across the country that may not reflect the quality of the care itself.
In addition, our results showed that high-volume centers have lower mortality rates. Previous work using the HCUP KID to analyze HLHS patients undergoing Norwood surgery has also shown an inverse relationship between case volume and mortality. Regardless, the magnitude of the volume effect is difficult to assess and is likely skewed by unknown confounders as suggested by the E-value analysis [32]. For example, variations in population, case complexity, and regional hospital density may affect how cases are distributed between low, medium, and high-volume centers. Norwood procedures in the Northeast and the West were mostly performed in high-volume centers (> 25 per year), whereas Norwood procedures in the Midwest and South were more evenly distributed across low, medium, and high-volume centers. Government insurance was also highly associated with low case volume, perhaps indicating more restricted access to large, regional centers in more rural parts of the country. Finally, ECMO use was highest in low-volume centers, although this was not statistically significant, possibly due to less experience managing these complex patients or taking on high-risk cases with additional social complexity in more rural regional programs.
ECMO use was significantly higher among non-survivors compared to survivors, suggesting that despite non-survivors having a shorter LOS, significant hospital resources are used for this population. Interestingly, ECMO use was a significant predictor of costs, but only in survivors ($231,961, p < 0.0001). In children and neonates, the costs for patients receiving ECMO are much higher than other cost-intensive procedures such as bone marrow transplantation, liver transplantation, and kidney transplantation [33]. This is further corroborated by the fact that comorbid conditions have been found to have a minimal effect on LOS and cost, as well as on mortality [28]. In recent years, ECMO has been increasingly used as a post-operative bridge for Norwood patients that cannot come off bypass intraoperatively, [34] or to provide hemodynamic stability and prevent cardiac arrest during interventional catheter-based treatment [35,36,37]. In fact, we noted an increase in ECMO use from 2003 to 2016, perhaps reflecting this shift in practice and potentially contributing to the shorter LOS, but increased costs over time. Although ECMO is costly and appears to be associated with worse mortality, it may nevertheless be cost-effective for a small subset of patients who require intensive cardiopulmonary support as a bridge post-operatively to survive [38]. ECMO has been shown to improve mortality outcomes in Norwood patients and the 11.9% of ECMO use we found among our survivors could reflect these findings [39, 40].
Collectively, the disparities seen in mortality and LOS suggest possible regional or center-specific differences that may affect outcomes and resource utilization. Although we could not explicitly include center-level effects, this has been shown in previous papers to affect hospital costs and outcomes, particularly in relation to hospital leadership, organizational values, and institutional structure [41,42,43]. Differences may reflect variations in institutional practices, patient demographics, case severity index, and socioeconomic status despite observing no significant differences in survivorship or LOS by race or income quartile. Given the broad nature of the HCUP data, we were unfortunately unable to control for additional covariates that may have affected cost and mortality, such as pre-operative comorbid conditions and socioeconomic status. We were also unable to account for differences in surgical complexity or technical adequacy of the repair.
Lack of specific clinical information in the HCUP database were a concern. In particular, gestational age and low birthweight are not accurately coded in the HCUP KID, but are likely to have contributed to the outcomes we observed. Jolley et al. analyzed ECMO use among HLHS patients undergoing Stage 1 Norwood surgery using 1998–2013 data from the Extracorporeal Life Support Organization (ELSO), a registry that collects voluntarily reported data on ECMO use from 230 US international center. They found that lower gestational age, body weight, and renal failure were associated with non-survival, as well as longer duration and multiple runs of ECMO [21]. We could not capture these covariates in the HCUP KID, which may have contributed to the unmeasured confounding quantified by our E-values calculated for predictors of mortality and ECMO use. We did attempt to use codes for dialysis and renal replacement therapy as proxies for renal failure during model development but found < 10 cases with these codes. Further, identifying renal failure in pediatric cardiac patients is particularly complex due to difficulties in diagnosis, and rather than reflecting true renal failure, proxy codes may reflect therapeutic modalities for fluid overload or peritoneal drains, and such use is subject to variable clinical practice. Although we used CCCs as a proxy for severity of illness, the inability to ascertain severity of conditions within each CCC category limited our analysis to broader generalizations. We found that more CCCs were associated with a decrease in costs, although this is likely due to an increase in mortality (and subsequently shorter LOS). Previous work has also found that pre-operative ventilatory or circulatory support is associated with an increased odds of mortality of 1.3 (95% CI 1.03–1.6) and 4.0 (95% CI 1.6–10.2) respectively [28]. While we could not differentiate pre-operative vs. post-operative use of ECMO, our results can only indicate that any ECMO use is associated with increased mortality.
Finally, our E-value analysis suggests that overall, unmeasured confounders may have attenuated the results from our initial multivariable models, a common concern in secondary database analyses. Although we found a significant OR of 1.34 (p = 0.03) for mortality among females vs. males, the E-value indicates that this result could be explained by an unmeasured confounder that has a relative risk association with mortality and gender of at least 1.58. The confidence interval value of 1.16 means that the relative risk association of the unmeasured confounder need only be 1.16 times more likely for the confidence interval to include the null. Thus, despite a statistically significant odds-ratio for gender, unmeasured confounding probably attenuates this effect. Similarly, we found a statistically significant OR 0.56 (p = 0.01) for mortality in high-volume centers (> 25 cases) compared to low-volume centers, but the E-value for this association suggests the result could also be explained by an unmeasured confounder that has a minimum relative risk association with mortality and case volume of 2.01 (CI = 1.48).
Regional differences in outcomes may be due to population vs. hospital/provider characteristics, rural vs. urban hospitals, or even regional institutional practices. It is plausible that high-volume centers are twice as likely to be located in regions with easier access to specialized care, or that certain families self-select into high-volume centers due to better prenatal counseling or improved awareness of their child’s condition. Differences in prenatal counseling by education level or socioeconomic status may affect the decision to terminate a pregnancy or lead to more proactive perinatal management, affecting the ultimate outcomes of the Norwood surgery. Institutional practices may also reflect differences in case selection, particularly in an age when surgical mortality rates, irrespective of patient severity, are a significant part of institutional ratings for quality of care. Thus, even if case volume or race/ethnicity appear to be statistically significant for mortality, unmeasured factors could easily explain these findings.
The results of the E-value analyses suggest that quality improvement efforts may need to focus on factors beyond medical care within the hospital to achieve optimal outcomes. For example, previous studies have found that socioeconomic factors such as maternal education can affect 1 year mortality or unplanned readmission for post-surgical HLHS patients [44]. Socioeconomic status also independently predicts post-op mortality, even when other hospital or patient-level medical factors are included [45]. We could only include income quartile, which only accounts for a portion of socioeconomic status. Institutional variation may also lead to different practices in the management of the interstage period between Norwood and Glenn, [46,47,48] and different management strategies can impact institutional LOS and cost. In addition, this may be influenced by factors such as payer mix and reimbursement rates. Thus, while the results of our primary analysis may point to specific hospital characteristics as predictors of LOS / mortality, it is unlikely that these factors are causal given the corresponding E-values and evidence pointing to numerous other influences on these outcomes.
In conclusion, we find that survivorship among HLHS infants undergoing Norwood surgery has improved over time while costs have tripled. Despite statistical significance, causal factors behind outcomes differences by hospital region and case volume cannot be determined due to unmeasured covariates as evidenced by the E-value analysis. Future research should be cautious in interpreting traditional measures of significance as evidence of causality, and focus on the numerous non-medical factors that affect health outcomes in addition to traditional measures to improve quality of care.
References
Parker SE, Mai CT, Canfield MA, Rickard R, Wang Y, Meyer RE, Anderson P, Mason CA, Collins JS, Kirby RS, Correa A (2010) Updated National Birth Prevalence estimates for selected birth defects in the United States, 2004–2006. Birth Defects Res A 88(12):1008–1016. https://doi.org/10.1002/bdra.20735
Fontan F, Baudet E (1971) Surgical repair of tricuspid atresia. Thorax 26(3):240–248
Allan LD, Apfel HD, Printz BF (1998) Outcome after prenatal diagnosis of the hypoplastic left heart syndrome. Heart 79(4):371
Caneo LF, Neirotti RA, Turquetto AL, Jatene MB (2016) The fontan operation is not the end of the road. Arq Bras Cardiol 106(2):162–165. https://doi.org/10.5935/abc.20160017
Feinstein JA, Benson DW, Dubin AM, Cohen MS, Maxey DM, Mahle WT, Pahl E, Villafane J, Bhatt AB, Peng LF, Johnson BA, Marsden AL, Daniels CJ, Rudd NA, Caldarone CA, Mussatto KA, Morales DL, Ivy DD, Gaynor JW, Tweddell JS, Deal BJ, Furck AK, Rosenthal GL, Ohye RG, Ghanayem NS, Cheatham JP, Tworetzky W, Martin GR (2012) Hypoplastic left heart syndrome: current considerations and expectations. J Am Coll Cardiol 59(1 Suppl):S1–42. https://doi.org/10.1016/j.jacc.2011.09.022
Marshall AC, van der Velde ME, Tworetzky W, Gomez CA, Wilkins-Haug L, Benson CB, Jennings RW, Lock JE (2004) Creation of an atrial septal defect in utero for fetuses with hypoplastic left heart syndrome and intact or highly restrictive atrial septum. Circulation 110(3):253–258. https://doi.org/10.1161/01.cir.0000135471.17922.17
Shenoy RU, Parness IA (2014) Hypoplastic left heart syndrome: looking back, looking forward. J Am Coll Cardiol 64(19):2036–2038. https://doi.org/10.1016/j.jacc.2014.09.018
Williams DL, Gelijns AC, Moskowitz AJ, Weinberg AD, Ng JH, Crawford E, Hayes CJ, Quaegebeur JM (2000) Hypoplastic left heart syndrome: valuing the survival. J Thorac Cardiovasc Surg 119(4 Pt 1):720–731. https://doi.org/10.1016/s0022-5223(00)70007-9
Ohye RG, Sleeper LA, Mahony L, Newburger JW, Pearson GD, Lu M, Goldberg CS, Tabbutt S, Frommelt PC, Ghanayem NS, Laussen PC, Rhodes JF, Lewis AB, Mital S, Ravishankar C, Williams IA, Dunbar-Masterson C, Atz AM, Colan S, Minich LL, Pizarro C, Kanter KR, Jaggers J, Jacobs JP, Krawczeski CD, Pike N, McCrindle BW, Virzi L, Gaynor JW (2010) Comparison of shunt types in the Norwood procedure for single-ventricle lesions. N Engl J Med 362(21):1980–1992. https://doi.org/10.1056/NEJMoa0912461
Debrunner MG, Porayette P, Breinholt JP 3rd, Turrentine MW, Cordes TM (2013) Midterm survival of infants requiring postoperative extracorporeal membrane oxygenation after Norwood palliation. Pediatr Cardiol 34(3):570–575. https://doi.org/10.1007/s00246-012-0499-x
Anderson BR, Ciarleglio AJ, Cohen DJ, Lai WW, Neidell M, Hall M, Glied SA, Bacha EA (2016) The Norwood operation: relative effects of surgeon and institutional volumes on outcomes and resource utilization. Cardiol Young 26(4):683–692. https://doi.org/10.1017/S1047951115001031
Pinto NM, Waitzman N, Nelson R, Minich LL, Krikov S, Botto LD (2018) Early childhood inpatient costs of critical congenital heart disease. J Pediatr 203(371–379):e377. https://doi.org/10.1016/j.jpeds.2018.07.060
Essaid L, Strassle PD, Jernigan EG, Nelson JS (2018) Regional differences in cost and length of stay in neonates with hypoplastic left heart syndrome. Pediatr Cardiol 39(6):1229–1235. https://doi.org/10.1007/s00246-018-1887-7
McHugh KE, Pasquali SK, Hall MA, Scheurer MA (2016) Impact of postoperative complications on hospital costs following the Norwood operation. Cardiol Young 26(7):1303–1309. https://doi.org/10.1017/S1047951115002498
Danford DA, Karels Q, Kulkarni A, Hussain A, Xiao Y, Kutty S (2015) Mortality-related resource utilization in the inpatient care of hypoplastic left heart syndrome. Orphanet J Rare Dis 10:137. https://doi.org/10.1186/s13023-015-0355-1
Benavidez OJ, Connor JA, Gauvreau K, Jenkins KJ (2007) The contribution of complications to high resource utilization during congenital heart surgery admissions. Congenit Heart Dis 2(5):319–326. https://doi.org/10.1111/j.1747-0803.2007.00119.x
Czosek RJ, Anderson JB, Heaton PC, Cassedy A, Schnell B, Cnota JF (2013) Staged palliation of hypoplastic left heart syndrome: trends in mortality, cost, and length of stay using a national database from 2000 through 2009. Am J Cardiol 111(12):1792–1799. https://doi.org/10.1016/j.amjcard.2013.02.039
Hirsch JC, Gurney JG, Donohue JE, Gebremariam A, Bove EL, Ohye RG (2008) Hospital mortality for Norwood and arterial switch operations as a function of institutional volume. Pediatr Cardiol 29(4):713–717. https://doi.org/10.1007/s00246-007-9171-2
Dean PN, Hillman DG, McHugh KE, Gutgesell HP (2011) Inpatient costs and charges for surgical treatment of hypoplastic left heart syndrome. Pediatrics 128(5):e1181–1186. https://doi.org/10.1542/peds.2010-3742
Menon SC, Keenan HT, Weng HY, Lambert LM, Burch PT, Edwards R, Spackman A, Korgenski KE, Tani LY (2012) Outcome and resource utilization of infants born with hypoplastic left heart syndrome in the Intermountain West. Am J Cardiol 110(5):720–727. https://doi.org/10.1016/j.amjcard.2012.04.050
Jolley M, Yarlagadda VV, Rajagopal SK, Almodovar MC, Rycus PT, Thiagarajan RR (2014) Extracorporeal membrane oxygenation-supported cardiopulmonary resuscitation following stage 1 palliation for hypoplastic left heart syndrome. Pediatr Crit Care Med 15(6):538–545. https://doi.org/10.1097/PCC.0000000000000159
Healthcare Cost and Utilization Project (2019) User Guide: Cost-to-Charge Ratio File for KID, 2003–2016. Healthcare Cost and Utilization Project. https://www.hcup-us.ahrq.gov/db/state/costtocharge.jsp. Accessed 18 April 2019
van der Ven JPG, van den Bosch E, Bogers A, Helbing WA (2018) State of the art of the Fontan strategy for treatment of univentricular heart disease. F1000Res. https://doi.org/10.12688/f1000research.13792.1
Healthcare Cost and Utilization Project (2019) ZIPINC_QRTL - Median household income for patient's ZIP Code (based on current year). Healthcare Cost and Utilization Project,. https://www.hcup-us.ahrq.gov/db/vars/zipinc_qrtl/nisnote.jsp. Accessed 12 March 2020
Society of Thoracic Surgeons (2019) Data Collection Form v3.41. https://www.sts.org/registries-research-center/sts-national-database/congenital-heart-surgery-database/data-collection. Accessed 18 April 2019
Haneuse S, VanderWeele TJ, Arterburn D (2019) Using the E-value to assess the potential effect of unmeasured confounding in observational studies. JAMA 321(6):602–603. https://doi.org/10.1001/jama.2018.21554
Mathur MB, Ding P, Riddell CA, VanderWeele TJ (2018) Web site and R package for computing E-values. Epidemiology 29(5):e45–e47. https://doi.org/10.1097/EDE.0000000000000864
Hornik CP, He X, Jacobs JP, Li JS, Jaquiss RD, Jacobs ML, O'Brien SM, Peterson ED, Pasquali SK (2011) Complications after the Norwood operation: an analysis of The Society of Thoracic Surgeons Congenital Heart Surgery Database. Ann Thorac Surg 92(5):1734–1740. https://doi.org/10.1016/j.athoracsur.2011.05.100
Society of Thoracic Surgeons (2019) Neonates - Spring 2019 Harvest. https://www.sts.org/registries-research-center/sts-national-database/sts-congenital-heart-surgery-database. Accessed November 12 2019
Romley JA, Chen AY, Goldman DP, Williams R (2014) Hospital costs and inpatient mortality among children undergoing surgery for congenital heart disease. Health Serv Res 49(2):588–608. https://doi.org/10.1111/1475-6773.12120
Tabbutt S, Ghanayem N, Ravishankar C, Sleeper LA, Cooper DS, Frank DU, Lu M, Pizarro C, Frommelt P, Goldberg CS, Graham EM, Krawczeski CD, Lai WW, Lewis A, Kirsh JA, Mahony L, Ohye RG, Simsic J, Lodge AJ, Spurrier E, Stylianou M, Laussen P, Pediatric Heart Network I (2012) Risk factors for hospital morbidity and mortality after the Norwood procedure: a report from the Pediatric Heart Network Single Ventricle Reconstruction trial. J Thorac Cardiovasc Surg 144(4):882–895. https://doi.org/10.1016/j.jtcvs.2012.05.019
Pieper D, Mathes T, Asfour B (2014) A systematic review of the impact of volume of surgery and specialization in Norwood procedure. BMC Pediatr 14:198. https://doi.org/10.1186/1471-2431-14-198
Faraoni D, Nasr VG, DiNardo JA, Thiagarajan RR (2016) Hospital costs for neonates and children supported with extracorporeal membrane oxygenation. J Pediatr 169(69–75):e61. https://doi.org/10.1016/j.jpeds.2015.10.002
Gulgun M, Slack M (2016) Stent placement in a neonate with sano modification of the norwood using semi-elective extracorporeal membrane oxygenation. Arq Bras Cardiol 107(6):600–604. https://doi.org/10.5935/abc.20160080
Brown KL, Shekerdemian LS, Penny DJ (2002) Transcatheter closure of a patent arterial duct in a patient on veno-arterial extracorporeal membrane oxygenation. Intensive Care Med 28(4):501–503. https://doi.org/10.1007/s00134-001-1202-5
Zahn EM, Dobrolet NC, Nykanen DG, Ojito J, Hannan RL, Burke RP (2004) Interventional catheterization performed in the early postoperative period after congenital heart surgery in children. J Am Coll Cardiol 43(7):1264–1269. https://doi.org/10.1016/j.jacc.2003.10.051
Booth KL, Roth SJ, Perry SB, del Nido PJ, Wessel DL, Laussen PC (2002) Cardiac catheterization of patients supported by extracorporeal membrane oxygenation. J Am Coll Cardiol 40(9):1681–1686
Petrou S, Bischof M, Bennett C, Elbourne D, Field D, McNally H (2006) Cost-effectiveness of neonatal extracorporeal membrane oxygenation based on 7-year results from the United Kingdom Collaborative ECMO Trial. Pediatrics 117(5):1640–1649. https://doi.org/10.1542/peds.2005-1150
Hoskote A, Bohn D, Gruenwald C, Edgell D, Cai S, Adatia I, Van Arsdell G (2006) Extracorporeal life support after staged palliation of a functional single ventricle: subsequent morbidity and survival. J Thorac Cardiovasc Surg 131(5):1114–1121. https://doi.org/10.1016/j.jtcvs.2005.11.035
Ungerleider RM, Shen I, Yeh T, Schultz J, Butler R, Silberbach M, Giacomuzzi C, Heller E, Studenberg L, Mejak B, You J, Farrel D, McClure S, Austin EH (2004) Routine mechanical ventricular assist following the Norwood procedure—improved neurologic outcome and excellent hospital survival. Ann Thorac Surg 77(1):18–22. https://doi.org/10.1016/s0003-4975(03)01365-1
Hearld LR, Alexander JA, Fraser I, Jiang HJ (2008) Review: how do hospital organizational structure and processes affect quality of care? A critical review of research methods. Med Care Res Rev 65(3):259–299. https://doi.org/10.1177/1077558707309613
Shipton H, Armstrong C, West M, Dawson J (2008) The impact of leadership and quality climate on hospital performance. Int J Qual Health Care 20(6):439–445. https://doi.org/10.1093/intqhc/mzn037
Skinner J (2011) Causes and Consequences of Regional Variations in Health Care11This chapter was written for the Handbook of Health Economics (Vol. 2). My greatest debt is to John E. Wennberg for introducing me to the study of regional variations. I am also grateful to Handbook authors Elliott Fisher, Joseph Newhouse, Douglas Staiger, Amitabh Chandra, and especially Mark Pauly for insightful comments, and to the National Institute on Aging (PO1 AG19783) for financial support. 2:45–93. doi:10.1016/b978-0-444-53592-4.00002-5
Peyvandi S, Baer RJ, Moon-Grady AJ, Oltman SP, Chambers CD, Norton ME, Rajagopal S, Ryckman KK, Jelliffe-Pawlowski LL, Steurer MA (2018) Socioeconomic mediators of racial and ethnic disparities in congenital heart disease outcomes: a population-based study in California. J Am Heart Assoc 7(20):e010342. https://doi.org/10.1161/JAHA.118.010342
Bennett KM, Scarborough JE, Pappas TN, Kepler TB (2010) Patient socioeconomic status is an independent predictor of operative mortality. Ann Surg 252(3):552–557; doi: 10.1097/SLA.0b013e3181f2ac64
Castellanos DA, Herrington C, Adler S, Haas K, Ram Kumar S, Kung GC (2016) Home Monitoring Program Reduces Mortality in High-Risk Sociodemographic Single-Ventricle Patients. Pediatr Cardiol 37(8):1575–1580. https://doi.org/10.1007/s00246-016-1472-x
Hanke SP, Joy B, Riddle E, Ravishankar C, Peterson LE, King E, Mangeot C, Brown DW, Schoettker P, Anderson JB, Bates KE (2016) Risk Factors for Unanticipated Readmissions During the Interstage: A Report From the National Pediatric Cardiology Quality Improvement Collaborative. Semin Thorac Cardiovasc Surg 28(4):803–814. https://doi.org/10.1053/j.semtcvs.2016.08.011
Rudd NA, Frommelt MA, Tweddell JS, Hehir DA, Mussatto KA, Frontier KD, Slicker JA, Bartz PJ, Ghanayem NS (2014) Improving interstage survival after Norwood operation: outcomes from 10 years of home monitoring. J Thorac Cardiovasc Surg 148(4):1540–1547. https://doi.org/10.1016/j.jtcvs.2014.02.038
Acknowledgements
CLG conceived the study design and analysis and wrote the manuscript. AYS performed all statistical analyses. RH, AL, PSF, LY, JDP, RKS, and RW each provided input on additional statistical analyses and critical editorial feedback on the manuscript.
Funding
This work is supported by the Teresa and Byron Pollitt Family Chair in Fetal & Neonatal Medicine at Children’s Hospital Los Angeles (Los Angeles/CA/USA). Dr. Lakshmanan is supported by grant KL2TR001854 from the National Center for Advancing Translational Science (NCATS) of the U.S. National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors report no other disclosures or conflicts of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (include name of committee + reference number) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Gong, C.L., Song, A.Y., Horak, R. et al. Impact of Confounding on Cost, Survival, and Length-of-Stay Outcomes for Neonates with Hypoplastic Left Heart Syndrome Undergoing Stage 1 Palliation Surgery. Pediatr Cardiol 41, 996–1011 (2020). https://doi.org/10.1007/s00246-020-02348-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-020-02348-5