Abstract
Myocarditis is an inflammatory disease of the myocardium with numerous different etiologies, the vast majority of which are infectious in origin. Patients afflicted with myocarditis can have variable presentations from flu-like symptoms to cardiogenic shock and sudden death, thus making the diagnosis difficult. The purpose of this study is the development of an algorithm for early identification and management of myocarditis based on a review of the published data and available literature. To validate the efficacy of this algorithm, a retrospective chart review of all the patient’s presenting symptoms and diagnostic workup, treatment, and clinical progression was performed and applied to the algorithm to investigate whether they could be diagnosed at the time of presentation. Retrospective chart review was performed and all the patient’s diagnosed with myocarditis between the years 2009 and 2017 were included in the study. 12 patients were identified on chart review and the algorithm was found to be 100% accurate at identifying all myocarditis patients at presentation by using the symptom identification.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The presentation of acute myocarditis is variable, degeneration into florid right heart failure or life threating arrhythmia can occur within hours of presentation. The purpose of this paper is a review of the published data and development of a treatment algorithm based on an available literature. To test the algorithm, we have performed a retrospective case review of our patients to assess presentation/treatment/clinical progression against the proposed algorithm.
Methods
DCH electronic medical records were searched by decision support for diagnosis code of myocarditis from 2009 to 2017 and returned 599 records. Records were reviewed and 12 cases were found to be consistent with clinical diagnosis of myocarditis. Epidemiologic, demographic, clinical course, laboratories, treatments, and outcomes were recorded by retrospective chart review. The DCH institutional review board approved this retrospective chart review. Review of the literature was conducted via Pubmed, Clinical Key, and Ovid MEDLINE for articles on myocarditis symptoms, presentation, laboratories, imaging, diagnosis, treatment, and management. Articles were included if they included pediatric patients or discussed pediatric management. Articles exclusively with adult patients were excluded unless there was a lack of pediatric information on the topic. These articles were reviewed and a myocarditis protocol was derived. The 12 identified patients from DCH were then used to retrospectively validate the protocol.
Presentation of Patient with Suspected Myocarditis
Acute myocarditis is a serious pediatric problem, with high mortality rates, debilitating sequelae such as chronic dilated cardiomyopathy, no globally accepted treatment or protocol, and under recognition. It presents a clinical management problem [1, 2] Freedman et al. in 2007, and Soonsswang cite a mortality rate of 25% in children and up to 75% in infants when secondary to Coxsackie B virus [3,4,5]. Durani et al. reported in their pediatric patients with myocarditis that 83% were not diagnosed at the first visit to a clinician and required two or more clinician examinations before myocarditis was suspected [6]. Importantly, evidence of myocarditis has been found on 16–20% of sudden infant death syndrome (SIDS) autopsies and a cause of sudden cardiac death in 17% of adolescents [2]. In the Freedman et al. retrospective study of 31 pediatric patients, the most commonly presenting symptoms were respiratory (32%), cardiac (29%), hypoperfusion (22%), and gastrointestinal (6%) [3]. All children who presented with chest pain were > 10 years of age with statistical difference reported in presenting symptoms for age (p = 0.003). Rady and Zekri also report that the most common presenting symptom was respiratory (62.5%) in their prospective cohort of 63 children in the PICU [7]. Durani et al. had 60% of their cohort of 62 children present with tachypnea, hepatomegaly (50%), respiratory distress (47%), fever (36%), and abnormal lung exam (34%) [6]. In addition, in Banka et al. multi-institutional analysis of pediatric myocarditis, 74% presented with chest pain, 42% viral symptoms, and 32% shortness of breath [8]. Infants more commonly than older patients can present in fulminant myocarditis, a distinct myocarditis presentation characterized by onset of cardiogenic shock in less than 3 days [9, 10].
When Chong et al. conducted a case control study with children who were correctly diagnosed with myocarditis compared with those who were later found to be initially misdiagnosed, they reported five potentially discriminating factors: respiratory distress on examination (OR 21.3; 95% CI 2.63–172.41), poor perfusion (OR 11.0; 95% CI 3.67–32.89), hypotension (OR 12.6; 95% CI 3.32–48.08) any ECG abnormality (OR 43.8; 95% CI 2.49–770.31), or cardiomegaly, pulmonary congestion, or pleural effusion on chest radiograph (OR 5.5; 95% CI 1.93–15.3) [11]. If ≥ 3 of the five factors were present, there was a positive likelihood ratio of 13 (95% CI 3.31–51.06) and negative likelihood ratio of 0.35 (95% CI 0.22–0.55) for diagnosis of myocarditis [11]. While these have not been validated, these symptoms should raise the suspicion for further myocarditis evaluation in patients who present with them.
Dallas Criteria
The gold standard histological criteria, the Dallas Criteria, was published in 1987, defining myocarditis as a process characterized by an inflammatory infiltrate of the myocardium with necrosis and/or degeneration of adjacent myocytes not typical of the ischemic damage associated with coronary artery disease.
In his 2006 critique, Baughman details sampling error, variation in expert interpretation among pathologists, variance with other markers of viral infection and immune activation in the myocardium, in addition to variance with treatment outcomes as evidence that the Dallas Criteria are lacking in diagnostic value and are outdated for myocarditis diagnosis [12]. Despite this, EMB in pediatric patients is still commonly performed in conjunction with viral PCR on myocardial tissue in many cases of unexplained dilated cardiomyopathy [13].
Cardiac MRI
CMR should be used in patients with current or persisting symptoms, evidence for significant myocardial injury, and suspected viral etiology. Evidence for significant myocardial injury includes new ECG findings, elevated troponin, or ventricular dysfunction. ECG, blood pressure, breathing, and oxygen saturation should be monitored during the imaging study. A cardiac resuscitation-trained physician should be available with ECHO machine, defibrillator, resuscitation drugs, and equipment ready [14].
Banka et al. published the largest pediatric CMR study analyzing 143 children up to 16 years of age, retrospectively, from 13 institutions [8]. Among the centers, there was variability in CMR tissue characterization, but CMR abnormalities were identified most commonly with late gadolinium enhancement 81%, T2-weighted imaging 74%, early gadolinium enhancement 55%, and first-pass contrast perfusion 8%. Of the 143 children in the study who underwent CMR, 117, or 82%, were interpreted as positive for myocarditis, 13% as negative, and 5% as equivocal, with the authors reporting a sensitivity of 82%. The study showed that CMR has high sensitivity for diagnosing myocarditis in pediatric patients when compared to EMB and is a much less invasive procedure [8].
Diagnostic criteria based on CMR in conjunction with clinical suspicion has been proposed and primarily relies on the presence 2 out of 3 of “regional or global myocardial SI increase I T2-weighted images, increased global myocardial early gadolinium enhancement ration between myocardium and skeletal muscle in gadolinium-enhanced T1-weighted images and the presence of at least one focal lesion with non-ischemic regional distribution in late IR-prepared gadolinium-enhanced T1-weighted images” in addition to clinical symptoms concerning for acute myocarditis [14].
Endomyocardial Biopsy
Unpublished data on a large number of pediatric patients presented by Dr. Franziska Degener from the German Multi-center Registry (MYKKE) at the ESC Working group for Myocardial and Pericardial Diseases (A Coruna 2019) suggest that endomyocardial biopsy (EMBX) may still play a role in early viral identification and thus effect treatment. Their data suggest a high number of positive viral PCR and culture positive biopsy specimens, many with limited cell edema and poor correlation of viral positivity and early cardiac MRI findings. This high viral positivity favored early use of IVIG empirically by many senior European cardiologists attending this meeting. No double-blinded study is underway regarding the MRI/EMBX or IVIG correlation, but their data collection is prospective and descriptive. The German data will deserve much scrutiny when it comes to publication to see how it affects the clinical management and whether EMBX in children should be return to common practice. The current best strategy for noninvasive evaluation is cardiac MRI with serial echocardiography.
Laboratory and Imaging Investigations/Clinical Suspicion
CXR and EKG
Freedman et al. concluded from their retrospective study that CXR alone was an insufficient screening test and all pediatric patients suspected of having myocarditis should undergo ECG [3]. ECG in this study was 93% sensitive, while CXR was 55% sensitive. The most common finding on CXR was cardiomegaly. The most common findings on ECG were ST or T wave abnormalities and axis deviations. Durani et al. reported cardiomegaly on CXR in 63% of their patients, while 100% had ECG changes [6]. Rady and Zekri reported a prospective cohort study of 63 critically ill children in the PICU [7]. They showed a statistically significant difference of cardiomegaly on CXR and elevated cardiac enzymes when compared to PICU patients without myocarditis. Vigneswaran et al. in their initial EKG results for 10 of their 17 patients showed results as follows: T-wave inversion as the most common finding, followed by ST segment elevation, prolonged PR interval, ST segment depression, Q waves, and low-voltage QRS complexes [15]. All 4 patients with ST segment elevation died.
ECHO
Echocardiogram is the initial imaging technique besides CXR that should be done in patients who raise clinical suspicion of myocarditis. Overall, global left ventricular or biventricular dysfunction can be seen, a dilated cardiomyopathy, or reduced LVEF [2, 9]. Additional abnormalities such as significant regurgitation of the mitral and tricuspid valves and atrial enlargement can be observed [2]. However, the diagnostic value of echocardiography is limited by the fact that many patients with less severe myocarditis have a normal echocardiogram and the highly variable echocardiographic findings lack specificity [14].
Fulminant myocarditis has a distinct onset of illness with severe hemodynamic compromise compared to acute myocarditis as well as a greater chance of progressing towards dilated cardiomyopathy.
Felker et al. suggested based on their study to determine the use of echocardiography as a means of differentiating acute and fulminant myocarditis that patients with fulminant myocarditis presented with near normal LV diastolic dimensions but increased septal thickness at presentation, while those with acute myocarditis had increased diastolic dimensions but normal septal thickness. They proposed that based on this study fulminant and acute myocarditis had distinct echocardiographic features [16]. This lends credibility toward utilizing echocardiography not only for diagnostic purposes, but also as a prognostic tool to predict acute hemodynamic compromise.
Troponin I Versus Troponin T
The diagnostic workup in any patient with a suspected diagnosis of myocarditis involves obtaining serum cardiac biomarkers including troponin testing. On literature review there have been no standardized large-scale reviews or studies looking at the superior sensitivity of troponin I over troponin T or vice versa with regards to sensitivity or specificity for the diagnosis of myocarditis.
Smith et al. in their study as part of the multicenter myocarditis treatment trial (mean age, 42.0 years ± 13.8 standard deviation) found that although the sensitivity of troponin I elevation for the entire group was low (34%), it did have a high specificity (89%) [17].
Conversely with regards to Troponin T and its diagnostic capabilities for myocarditis, Lauer et al. in their study of 80 patients (mean age group of 49 ± 14 years, ranging from 12 to 85 years old) with suspected myocarditis, found that 35% of patients had elevated troponin levels, the researchers concluded that the use of troponin T for the detection of myocarditis had a specificity of 94%, a sensitivity of 53%, a positive predictive value of 93%, and a negative predictive value of 56% [18].
It is also important to note that the test sensitivity of troponin T is also largely dependent on the cut off value being used.
Eisenberg et al. reported in a retrospective cohort study of 221 patients, a cardiac troponin T level of less than 0.01 ng/mL could exclude myocarditis in children without pre-existing heart disease [19].
Overall, Troponin T or I is an essential laboratory test to obtain in the work-up for myocarditis in the pediatric patient. Elevated values support the diagnosis of myocarditis, while a value of < 0.01 ng/mL does not support the diagnosis in previously healthy patients.
Additional Labs
Freedman et al. also found that aspartate aminotransferase (AST) measurement may be a useful laboratory adjunct, reporting sensitivity of 85% of their myocarditis patients with median AST value of 66 U/L in their definitive group and 116 U/L in their probable group [3]. Interestingly, there was no associated increase in alanine aminotransferase (ALT) level. This finding has not been reported in other studies, prior to their data. The elevation in liver enzymes could be attributed to right heart failure and/or known liver enzyme elevation in certain viral and bacterial illness, such as EBV or rickettsia infection. However, what cannot be accounted for is the elevation in only AST.
Other testing that adds supportive evidence for myocarditis, if elevated, includes: complete blood count, erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), and brain natriuretic peptide (BNP) [19].
Infectious Diseases and Virology
Viral myocarditis is the most common etiology in children, dominated by enteroviral species, such as Coxsackie virus in addition to other viruses such as Adenovirus. While myocarditis usually occurs sporadically, epidemics caused by coxsackie virus have been reported. During a 1965 European coxsackie B virus epidemic, 5% to 12% of patients had cardiac manifestations [2].
There are many other causes of myocarditis including infectious, allergen related, autoantigens such as associated with Kawasaki’s disease or Wegener’s granulomatosis, and toxic such as poisoning with heavy metals and medications such as cyclophosphamide and radiation therapy [19].
EMB PCR on myocardial samples has increased viral identification in those pediatric patients who were determined to be stable enough to undergo EMB. In the Freedman et al.'s study, five patients in the study underwent EMB where Parvovirus B19 was identified in two biopsies and Enterovirus and Coxsackie B identified in one biopsy each [3]. The utility of EMB with positive viral PCR on myocardium is limited by the invasive procedure of EMB, leading many to use less invasive ways to peripherally detected viruses. However, EMB can help delineate non-infectious causes leading to myocarditis.
Treatment
Initial measures of myocarditis treatment include bed rest to decrease oxygen consumption, salt and fluid restriction, supplemental oxygen, and correction of any identified anemia [4, 20].
IVIG
Reviewing the literature, several studies are available that do not support administration of IVIG. Drucker et al. reported a prospective trial of 21 pediatric patients receiving 2 mg/kg IVIG. They report the IVIG group achieving normal left ventricular function during the first year after presentation with a (p-value = 0.03) [21]. They reported a higher survival in IVIG-treated patients of 84% versus 60% in those not receiving IVIG, but there was no statistical significance found (p = 0.69). Though Drucker et al. reported promising improvement, these results have not been reproduced. Klugman et al. identified a retrospective cohort of 216 myocarditis patients, 0.05% of the discharged patient’s over a year from 35 academic children’s hospitals [22]. 82% were diagnosed as idiopathic and 3% bacterial or viral. Those given IVIG were overall 45.4%. 46.2% in the survival group and 35.3% in the group that died. However, IVIG was shown to not impact survival (p = 0.67). When analyzing patients with extreme severity scores, in cases where IVIG was more likely to be used, IVIG still did not impact mortality (p = 0.22). Similarly, Kim et al. after conducting a retrospective analysis of 33 children treated with IVIG or IVIG in addition to steroids, for clinical myocarditis, found no difference in 1-year survival or recovery of left ventricular function [23].
A 2015 Cochrane Review compared transplant-free survival of adults and children with presumed viral myocarditis treated with IVIG versus control without IVIG treatment [24]. The study also observed if a group of patients with presumed viral myocarditis could be identified as most likely to benefit from IVIG. The pediatric study that Cochrane Review included was conducted in India and had enrolled 83 children from 2 months to 12 years old with suspected viral encephalitis and associated myocarditis; note this is commonly associated with Enterovirus 71 infection. They received 400 mg/kg of IVIG for 5 consecutive days. Virus isolation was limited to a rise in Coxsackie B1 titers in 7 children and Enterovirus detection in 8 stool cultures. Those treated with IVIG had 7.39 (95% CI 0.91to 59.86) increase in odds ratio of event-free survival than those who were not treated. The LVEF at discharge was 49.5% in the treated group and 35.9% in the placebo group with a p value = 0.001. There was high bias identified in this study, in addition to extrapolation of data to those with isolated myocarditis not associated with encephalitis. It was concluded that IVIG for presumed viral myocarditis should not be included as part of routine practice until higher-quality studies demonstrate benefit. Other adult studies also do not support IVIG administration [25]. In summary, there are no prospective randomized controlled trials that support IVIG administration in the pediatric population.
Anti-Viral Treatments
Pleconaril is an anti-viral drug that prevents Enterovirus, such as Coxsackie virus, from infecting target cells [20]. A randomized, double blind, placebo-controlled trial of Pleconaril by Abzug et al. enrolled 61 neonates at 15 days of life or less from June 1999 to December 2010 [26]. Survival probability over 2 months was higher in the treatment group with p = 0.02 and after adjustment for duration of symptoms prior to enrollment p = 0.057. Cumulative survival probability in the treatment group continued to exceed placebo group over 18 months with p = 0.07 and p = 0.23 between the Enteroviral group, but the result was not statistically significant. The study did show time to negativity of oropharynx, rectal, urine, and serum cultures for Enterovirus occurred faster, 4 days versus 7 days with p = 0.08. Overall, Pleconaril has not been shown to significantly improve survival when administered in Enteroviral myocarditis cases.
HIV, CMV, and HSV should be treated with already established antiviral therapies.
Immunosuppressant Therapy
Focusing on immunomodulation, the second phase in the proposed triphasic understanding of myocarditis, the myocarditis treatment trial randomized 111 adult patients with the histopathological diagnosis of myocarditis and LVEF < 45% to receive conventional therapy alone or combined with 24-week regimen of prednisone with cyclosporine or prednisone with azathioprine [27]. Overall, LVEF improved in all groups from 25 to 34% at 28 weeks with p = < 0.001, but without statistical difference between the groups of patients. There was also no significant difference in survival between the two groups, p = 0.96. The study concluded the results did not support routine treatment of myocarditis with immunosuppressive drugs. Additionally, ventricular function improved regardless of whether patients received immunosuppressive therapy. Immune response was also considered in the trial by measuring cardiac IgG antibodies, anti-skeletal-muscle IgG antibodies, general IgG antibody titer, Helper T cell count < 30%, increased white cell count, and increased levels of natural killer cells and macrophages. These all were associated with differing positive factors, such as higher LVEF, and when adjusted for clinical characteristics still remained significant, p = < 0.05. However, none of the immunologic variables on outcome were evaluated and were not significantly associated with measures of cardiac performance for the whole group.
Hia et al. conducted a systematic review from 1984 to 2003, where nine pediatric population studies were reviewed: one randomized controlled trial, one case control trial, one prospective non-controlled trial, and four retrospective studies [28]. These studies included the immunosuppressive agents: Prednisone, IVIG, cyclosporine, azathioprine, interferon-alpha, and Orthoclone OKT®3. Though an increased odds ratio with immunosuppression was reported as 2.7 (95%, CI 0.59–14.21) in the case–control trial and randomized control trial, there was no statistical significance. Hia et al. cite that several of the studies showed improvement in outcome when an adjunctive immunosuppressant was added to prednisolone, but only one study showed an increased odds ratio of 0.09 (95% CI 0.01–0.52) when prednisolone plus another adjunctive immunosuppressant was used.
Gagliardi, Bevilacqua et al. published in 2004 a study that followed 114 pediatric patients who underwent EMB and were consistent with acute myocarditis or borderline myocarditis [29]. They were then treated with cyclosporine and prednisone in addition to conventional treatment. 13-year transplant-free survival and assessment of left ventricular function were then assessed. Event-free survival for both groups was 96% at one year and 83% at 13 years. Complete cardiac recovery in both groups combined was 70%. There was additional non-inflammatory group that was only treated with conventional therapy. Researchers included this third group in their overall survival rate of 65%. They compared this to a known survival rate of 44% and found a statistically significant comparison with p = 0.004. There was no control group for this study. Overall, studies by Hia et al. and Gagliardi et al. show mixed results [28, 29]. Gagliardi et al. improvements in survival rate have not been reproduced. There are consistent results showing improvement in LVEF after corticosteroid treatment [29].
A 2015 Cochrane review assessed the efficacy of corticosteroids in 2 pediatric and 6 adult randomized controlled trials of 719 patients, of which 200 were pediatric patients [30]. The study concluded that corticosteroid treatment did not significantly reduce the death rate or death rate combined with heart transplant. However, at 1–3 months follow-up there was significant differences in left ventricular systolic function with a 7% increase in LVEF. Additionally, reduced serum levels of creatine kinase, CK-MB, and alpha-hydroxybutyrate dehydrogenase were significantly associated with corticosteroid treatment.
There are consistent results showing improvement in LVEF after corticosteroid treatment, however, not in survival rate when looking at the current literature for immunomodulation therapy.
Management
ICU Admission
Due to myocarditis’s variable presentation with the ability to worsen quickly, intensive care unit verses general inpatient floor admission can be a difficult decision. Vigneswaran et al. concluded from their study of Parvovirus B19 positive myocarditis cases, that children presenting in fulminant myocarditis, EKG with ST segment changes (especially ST elevation), history of a short prodromal illness (< 48 h), or those in severe heart failure have worse outcomes [15]. Bergmann et al.’s ER algorithm for the management of myocarditis and pericarditis have all myocarditis patient’s going to PICU and does not consider floor admission for these patients [9]. However, not all myocarditis patients require PICU admission. Klugman et al. stratified patients based on a severity score as minor, moderate, major, and extreme [21]. Myocarditis patients with a severity score of major or extreme were 53.2% and those admitted to the ICU were 53.7% of the studies participants overall. The study found the only statistically significant variable between those who survived or died was the severity of the presentation (p = < 0.0001), and supports more severe patients being admitted to the PICU. Of those who died, 41.2% had a severity score of major and 58.8% were extreme. Length of stay was 14.4 days and mortality rate was 7.8%.
Arrhythmias
Arrhythmias are a common sequela and/or manifestation of myocarditis. They may sometimes be the only manifestation of myocarditis and both tachyarrhythmias and bradyarrhythmias are a significant cause for concern as contributors to sudden cardiac death in these patients.
Anderson et al. investigated the usefulness of arrhythmias as predictors of death and resource utilization in children with myocarditis. In their review of 2041 pediatric patients with myocarditis, the incidence of tachyarrhythmias was reported in 11.5% and bradyarrhythmias in 1.1% of the subjects, with an overall mortality of 8.7%.
The investigators also performed a multivariable analysis taking into account the gender, age of admission, and presence of underlying anatomic defects among other variables and found that tachyarrhythmias were associated with a 2.3 times increase in odds of mortality [31].
On review of literature a paucity of data to be found regarding the length of monitoring for patients with arrhythmias after myocarditis, instead the various studies focus on the incidence and timeline of arrhythmias after myocarditis that may be used to provide guidance regarding the follow-up management for such patients. While Gao et al. demonstrated the ANF dysfunction that led to arrhythmogenic potential decreased over time it is crucial to note that given that multiple factors lead to electrical membrane potential alteration as demonstrated by Klein et al. [32, 33]. The timeline of monitoring would depend on the degree of the various triggering factors for arrhythmia that have developed in the case of the individual patient afflicted with myocarditis. Higher alterations in ventricular dynamic parameters, ANF dysfunction, and/or structural/vascular changes would require closer spaced and longer follow up to monitor for the development of arrhythmias.
Miyake et al. performed a 14-year retrospective review of patients < 21 years of age that were hospitalized with myocarditis. The study reported that arrhythmias occurred in 45% of the patients. The study also demonstrated that arrhythmias in the subacute stage were associated with proceeding ST wave changes [34].
Based on current literature review there is evidence that ECG changes may be used in identification of the onset of subacute arrhythmia as well as follow-up post-discharge to monitor for the recurrence. Given the documented association of arrhythmias in particular tachyarrhythmia on literature review with increased mortality, consideration should be given to closer monitoring in the PICU for patients who develop these ECG changes with underlying suspicion of myocarditis [31].
Maron et al. in their task force recommendations, looked at various cardiac conditions in relation to considerations for athletes. With regards to myocarditis, the recommendations emphasized that athletes with “probable or definite evidence of myocarditis should be withdrawn from all competitive sports and undergo a prudent convalescent period of about 6 months following the onset of clinical manifestations.” Athletes were able to return to training after this time period had elapsed provided that there was echocardiograph and/or radionuclide studies proven return of cardiac dimensions, LV function and wall motion to baseline, holter, and exercise testing proven absence of clinically relevant arrhythmias as well as normalization of serum inflammatory/heart failure markers and 12 lead EKG [35].
Ionotropes, Beta Blockers, and Diuretics
Ionotropes and diuretics comprise a mainstay for the treatment of myocarditis as indicated per heart failure protocols.
The current recommendations for patients with pediatric myocarditis continue to place emphasis on supportive management. The treatment for heart failure should proceed as per the guidelines endorsed by the American Heart Association the American College of cardiology and the heart failure Society of America [36,37,38].
While no randomized controlled trials could be found on literature review to assess the efficacy of one particular inotropic agent over another with regards to the management and treatment of pediatric myocarditis, Klugman et al. in their multi-institutional analysis to look at pediatric patients hospitalized with myocarditis found that of the 216 children in the review were given milrinone or epinephrine in 45% and 35% of the patients respectively [22].
Follow Up
It should be noted that on the literature review there is no consensus found regarding what the frequency or standardized duration of follow-up for pediatric patients admitted with myocarditis should be. This is likely resultant from the fact that there are various etiologies that can cause myocarditis and the spectrum of the illness is wide in terms of the degree of heart failure to the arrhythmogenic potential for each particular patient. What is clear however is that these patients should be followed closely outpatient especially if there are any signs of significant residual congestive heart failure present. Based on the general pathophysiology of the disease on literature review, it can be argued that patient should at the very least be reevaluated within 5 days by their primary care pediatrician to monitor the volume status, symptoms, medication regimen and side effects. Follow up with the cardiologist should be within the first 2 weeks of this discharge to monitor for any arising side effects of newly started medications, as well as continued response to these medications clinically. Follow up after 2 weeks with a cardiologist should be decided on the spectrum of the disease and would be dependent on the residual presence of congestive heart failure, concerned for the development of arrhythmias, hospital course, and monitoring of medications. Recovery of cardiac function after myocarditis tends to be gradual and although most children will ultimately have complete or partial recovery of LV function a subset of patients develop chronic dilated myocarditis. We recommend long-term follow-up with the cardiologist to monitor hemodynamics until full recovery.
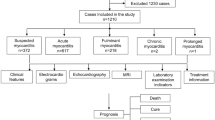
Retrospective Validation of Pediatric Myocarditis Algorithm (Fig. 1)
Twelve patients aged 16 days–17 years old were identified at Driscoll Children’s Hospital between 2009 and 2017. Seven children were males and five were females. Patients were ill for a mean of 4 days ± 5.2 days prior to admission. 41.7% saw a medical professional at least one time prior to seeking emergency department (ED) care. Two patients saw a medical professional three separate times prior to presenting to the ED. 33.3% were on one or more antibiotic/antiviral prior to seeking tertiary care where the diagnosis of myocarditis was made. 91.7% of patients had at least one respiratory or cardiovascular-related complaint. The only one who did not was < 1 month old. She instead presented with diarrhea and fever. The youngest patient presenting with chest pain was 7.5 years old. The most common presenting symptom was any cardiovascular symptom: tachycardia, chest pain, orthopnea, or hypoperfusion. All patients retrospectively would have been identified as at risk for myocarditis if using the protocol (Table 1).
On CXR, 75% of DCH patients had cardiomegaly, the most common abnormality identified. Pleural effusions were identified on 41.7% and perihilar congestion 8.3%. This supports that cardiomegaly alone on CXR is not a sensitive screening test as the studies above suggest. 90.9% of patients had abnormal ECG on admission. 63.6% with non-specific T wave abnormalities, 54.5% with non-specific ST segment changes, and 18.2% with diffuse ST elevations which are similar to Vigneswaran and Freedman. This supports the need for obtaining both CXR and EKG in the evaluation of myocarditis. 91.7% of our patients had abnormal ECHO findings. Mean LVEF 32% ± 0.17, min 11.9%–max 64% (normal EF considered 56–78%). Two patients had normal ejection fractions. Mean fractional shortening 19% ± 0.10, min 5.2%–max 35.4% (normal fractional shortening considered 28–44%). Two patients had normal fractional shortening.
Cardiac biomarkers were all elevated on admission for the DCH myocarditis patient population. All patients had troponin I level > 0.01 ng/mL. The lowest reported troponin I was 0.04 ng/mL. Extrapolating Soonsgwang and Eisenberg’s studies using troponin T to troponin I, Soonsgwang et al. criteria of troponin T < 0.052 ng/mL, would have excluded one of our patients, but Eisenberg et al. lower cut-off of < 0.01 ng/mL would have included them [5, 19]. Based on this comparison of these two studies and our own patient results, it appears that using a lower troponin T cut-off value at 0.01 ng/mL would help achieve a greater sensitivity without a significant compromise on the specificity of troponin T testing and perhaps should be held as the standard in troponin testing for suspected myocarditis. Surprisingly, the findings of Freedman et al., mean AST elevation with normal mean ALT, were replicated in our patients (Table 2) [3]. No significant mean leukocytosis or cell differential abnormality was identified. Patients were relatively normocytic at presentation and without electrolyte aberrances.
Overall infectious disease investigation yielded poor results for isolation of an infectious agent. 50% (6/12), of patients had viral cultures taken from the nasopharnyx and rectum for Enterovirus and/or Adenovirus without any of them isolating a virus. 16.7% had titers drawn: one titer was positive for Cocksackie B1, B2, B3, B6 and the other for Cocksackie B2, B4, B6, and Echovirus 4, 7, 11, 30. No convalescent titers were drawn. Both had viral RNA by multiplex respiratory pathogen panel (BioFire®) rhinovirus/enterovirus nasopharyngeal swabs positive. Serology was done in three cases. One case was identified as Mycoplasma IgM+ . No other serology was identified in the other two cases. 75% had positive nasopharyngeal PCR swabs (BioFire®). Eight had nasopharyngeal swabs+ for Rhinovirus/Enterovirus. One had positive respiratory syncytial virus swab. One had history of recent influenza A infection in addition to Rhino/Enterovirus nasopharyngeal swab positive. 41.7% patients had PCR from the blood drawn and all were negative: CMV (2), Parvovirus B19 (2), EBV (2), HHV6 (1), West Nile CSF (1), HSV (1), Enterovirus (1). All patients were fully immunized. Only one patient was screened for TB by PPD which was 0 mm of induration. Findings in these patients support the inutility of obtaining viral cultures and titers. Viral serum PCR also did not identify any etiologies, though there are more promising in the reviewed studies, without carrying the risk of EMB. All patients were assessed for immunization status and were all fully immunized.
58.3% of DCH patients developed an arrhythmia with mean time to develop an arrhythmia from reported symptom onset was 6 days ± 7.1. Average time to develop an arrhythmia from admission was 1.7 days ± 1.7 days. Three patients developed ventricular tachycardia with one decompensating into ventricular fibrillation. One patient developed supraventricular tachycardia, two patients developed sinus bradycardia, and one with bradycardia and complete AV block. Two of the patients who were initially admitted to the floor and transferred to PICU for acute decompensation were due to development of ventricular tachycardia: One patient had acute onset of symptoms that day with tachycardia and mild cardiomegaly on CXR. One patient had > 48 h of illness, no ST elevation on ECG, but did have signs of heart failure with hepatomegaly, hypotension, tachycardia, and tachypnea with admission diagnosis of dehydration. The other patient who required floor to PICU transfer was due to hypernatremia of 160 mmol/L, but he had history of acute prodromal illness < 48 h. Overall the protocol would have placed three patients in the PICU when they were originally on the floor and placed patients at decreased risk of morbidity/mortality. The rest of the patients though sent to PICU at the discretion of the admitting physicians, would also be sent to PICU if following the protocol due to either unstable vitals or had history of < 48 h prodromal illness, arrhythmia, or supportive signs of fulminant myocarditis on admission.
In our patient group, 75% required one or more inotrope medication. 66.7% were intubated and mechanically ventilated; mean 3.7 days of ventilation ± 4.11. One patient required ECMO for 13 days after developing ventricular tachycardia. Patients spent a mean time in ICU 8 days ± 6.7 and mean days on the floor prior to discharge 4.3 ± 8.4. Total mean time hospitalized was 12 days ± 14.5. Mean EF at discharge 53% ± 17.2, min 20.1%–max 69%. 4 patients had EF < 55% at discharge, 6 had EF ≥ 55% at discharge, and 2 were transferred to different facility prior to convalescence. 83.3% of patients received IVIG and 25% received steroids at some time during their illness. Of the 6 patients that regained normal LVEF by discharge, two patients received IVIG and steroids. Three received IVIG and no steroids, and one did not receive either IVIG or steroids. Of the four patients who did not recover their LVEF by discharge, three received IVIG and one did not, and none of the four received steroids. No patients died.
Conclusion
Our 12-patient retrospective validation of the Driscoll Children’s Hospital Pediatric Myocarditis Algorithm was supported by 100% accuracy of identifying all myocarditis patients at presentation by using the symptom identification. All patients would have been admitted to PICU based on admitting criteria in the algorithm due to either: short < 48-h prodromal illness, arrhythmia, heart failure, or unstable vital signs including three patients who were originally placed on the general pediatric floor and later transferred to the PICU. All patients would be identified if minimum of CXR, EKG, Troponin with minimum cut-off value of < 0.01 ng/mL were completed in the ED. Though no definitive infectious etiology was found for any of the patients, utilizing the infectious disease tests on the protocol did away with unnecessary testing and suggests, based on literature review, higher yield tests, most of which were not done consistently on all patients undergoing work-up. Given that the majority of our patients received IVIG, a substantial comparison in the outcomes of LVEF recovery could not be made by comparing IVIG receiving and non-IVIG receiving patients. However, based on our literature review there is no strong evidence for administering IVIG. Based on the literature review, we recommend the use of cardiac MRI as a less invasive tool for diagnosis of myocarditis and reserving the use of endomyocardial biopsy for those cases where the lack of clinical improvement raises suspicion for an unusual non-infectious etiology. This protocol is a derivative of literature review and attempts to standardize myocarditis patient care on presentation and admission. Because the degree and progression of the myocarditis is difficult to predict, suspicion must remain high for a fulminant course until several clinical data points can be obtained. It would be prudent to assume a severe course and have the patient in a center where adjunct support with LVAD or ECMO can be given along with full support of a skilled pediatric intensive care unit. The authors of this paper hope that the algorithm presented is a useful and adaptable tool to assist the clinicians in initial management of this challenging disease.
A means to validate the protocol through a retrospective analysis at a singular institution has been made in this study however ideally it requires prospective validation. Aspects of further validation would include a larger group of patients in a multi-centered trial to not only assess the ability of the algorithm to identify and triage clinical cases suspicious for myocarditis but also to further delineate the differences in outcome between patients who received steroids at the time of diagnosis, patients who received IVIG, patients who received both therapies and patients who received neither.
References
Liu PP, Mason JW (2001) Advances in the understanding of myocarditis. Circulation. https://doi.org/10.1161/hc3401.095198
Durani Y, Giordano K, Goudie BW (2010) Myocarditis and pericarditis in children. Pediatr Clin North Am. https://doi.org/10.1016/j.pcl.2010.09.012
Freedman SB, Haladyn JK, Floh A, Kirsh JA, Taylor G, Thull-Freedman J (2007) Pediatric myocarditis: emergency department clinical findings and diagnostic evaluation. Pediatrics. https://doi.org/10.1542/peds.2007-1073
Dancea AB (2001) Myocarditis in infants and children: a review for the paediatrician. Paediatr Child Health (Oxford). https://doi.org/10.1093/pch/6.8.543
Soongswang J, Durongpisitkul K, Nana A et al (2005) Cardiac troponin T: a marker in the diagnosis of acute myocarditis in children. Pediatr Cardiol. https://doi.org/10.1007/s00246-004-0677-6
Durani Y, Egan M, Baffa J, Selbst SM, Nager AL (2009) Pediatric myocarditis: presenting clinical characteristics. Am J Emerg Med. https://doi.org/10.1016/j.ajem.2008.07.032
Rady HI, Zekri H (2015) Prevalence of myocarditis in pediatric intensive care unit cases presenting with other system involvement. J Pediatr (Rio J). https://doi.org/10.1016/j.jped.2014.05.011
Banka P, Robinson JD, Uppu SC et al (2015) Cardiovascular magnetic resonance techniques and findings in children with myocarditis: a multicenter retrospective study. J Cardiovasc Magn Reson. https://doi.org/10.1186/s12968-015-0201-6
Bergmann KR, Kharbanda A, Haveman L (2015) Myocarditis and pericarditis in the pediatric patient: validated management strategies. Pediatr Emerg Med Pract 12:1–22
Amabile N, Fraisse A, Bouvenot J, Chetaille P, Ovaert C (2006) Outcome of acute fulminant myocarditis in children. Heart. https://doi.org/10.1136/hrt.2005.078402
Chong SL, Bautista D, Ang ASY (2015) Diagnosing paediatric myocarditis: what really matters. Emerg Med J. https://doi.org/10.1136/emermed-2013-202926
Baughman KL (2006) Diagnosis of myocarditis death of Dallas criteria. Circulation. https://doi.org/10.1161/CIRCULATIONAHA.105.589663
Gagliardi MG, Fierabracci A, Pilati M et al (2016) The impact of specific viruses on clinical outcome in children presenting with acute heart failure. Int J Mol Sci. https://doi.org/10.3390/ijms17040486
Friedrich MG, Sechtem U, Schulz-Menger J et al (2009) Cardiovascular magnetic resonance in myocarditis: a JACC white paper. J Am Coll Cardiol. https://doi.org/10.1016/j.jacc.2009.02.007
Vigneswaran TV, Brown JR, Breuer J, Burch M (2016) Parvovirus B19 myocarditis in children: an observational study. Arch Dis Child. https://doi.org/10.1136/archdischild-2014-308080
Felker GM, Boehmer JP, Hruban RH et al (2000) Echocardiographic findings in fulminant and acute myocarditis. J Am Coll Cardiol. https://doi.org/10.1016/S0735-1097(00)00690-2
Smith SC, Ladenson JH, Mason JW, Jaffe AS (1997) Elevations of cardiac troponin I associated with myocarditis: experimental and clinical correlates. Circulation. https://doi.org/10.1161/01.CIR.95.1.163
Lauer B, Niederau C, Kühl U et al (1997) Cardiac troponin T in patients with clinically suspected myocarditis. J Am Coll Cardiol. https://doi.org/10.1016/S0735-1097(97)00317-3
Caforio ALP, Pankuweit S, Arbustini E et al (2013) Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology Working Group on myocardial and pericardial diseases. Eur Heart J. https://doi.org/10.1093/eurheartj/eht210
Levi D, Alejos J (2002) An approach to the treatment of pediatric myocarditis. Pediatr Drugs. https://doi.org/10.2165/00128072-200204100-00002
Drucker NA, Colan SD, Lewis AB et al (1994) γ-Globulin treatment of acute myocarditis in the pediatric population. Circulation. https://doi.org/10.1161/01.CIR.89.1.252
Klugman D, Berger JT, Sable CA, He J, Khandelwal SG, Slonim AD (2010) Pediatric patients hospitalized with myocarditis: a multi-institutional analysis. Pediatr Cardiol. https://doi.org/10.1007/s00246-009-9589-9
Kim HJ, Yoo GH, Kil HR (2010) Clinical outcome of acute myocarditis in children according to treatment modalities. Korean J Pediatr. https://doi.org/10.3345/kjp.2010.53.7.745
Robinson J, Hartling L, Vandermeer B, Klassen TP (2015) Intravenous immunoglobulin for presumed viral myocarditis in children and adults. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD004370.pub3
Vashist S, Singh GK (2009) Acute myocarditis in children: current concepts and management. Curr Treat Options Cardiovasc Med. https://doi.org/10.1007/s11936-009-0039-z
Abzug MJ, Michaels MG, Wald E et al (2015) A randomized, double-blind, placebo-controlled trial of pleconaril for the treatment of neonates with enterovirus sepsis. J Pediatric Infect Dis Soc. https://doi.org/10.1093/jpids/piv015
Mason JW, O’Connell JB, Herskowitz A et al (1995) A clinical trial of immunosuppressive therapy for myocarditis. The myocarditis treatment trial investigators. N Engl J Med. https://doi.org/10.1056/NEJM199508033330501
Giulia Gagliardi M, Bevilacqua M, Bassano C et al (2004) Long term follow up of children with myocarditis treated by immunosuppression and of children with dilated cardiomyopathy. Heart. https://doi.org/10.1136/hrt.2003.026641
Caldeira D, Lopes LR, Vaz-Carneiro A, Costa J (2015) Cochrane corner: corticosteroids for viral myocarditis. Rev Port Cardiol (English Ed). https://doi.org/10.1016/j.repce.2014.08.007
Kühl U, Pauschinger M, Schwimmbeck PL et al (2003) Interferon-β treatment eliminates cardiotropic viruses and improves left ventricular function in patients with myocardial persistence of viral genomes and left ventricular dysfunction. Circulation. https://doi.org/10.1161/01.CIR.0000072766.67150.51
Klein RM, Vester EG, Brehm MU et al (2000) [Inflammation of the myocardium as an arrhythmia trigger]. Z Kardiol 89:24–35
Gao X, Peng L, Zeng Q, Wu ZK (2009) Autonomic nervous function and arrhythmias in patients with acute viral myocarditis during a 6-month follow-up period. Cardiology. https://doi.org/10.1159/000167794
Pieroni M, Dello Russo A, Marzo F et al (2009) High prevalence of myocarditis mimicking arrhythmogenic right ventricular cardiomyopathy. differential diagnosis by electroanatomic mapping-guided endomyocardial biopsy. J Am Coll Cardiol. https://doi.org/10.1016/j.jacc.2008.11.017
Blauwet LA, Cooper LT (2010) Myocarditis. [Review] [188 refs]. Prog Cardiovasc Dis. https://doi.org/10.1016/j.pcad.2009.11.006
Hunt SA, Abraham WT, Chin MH et al (2009) Focused update incorporated into the ACC/AHA 2005 guidelines for the diagnosis and management of heart failure in adults. A report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines developed. J Am Coll Cardiol. https://doi.org/10.1016/j.jacc.2008.11.013
Lindenfeld J, Albert NM, Boehmer JP et al (2010) HFSA 2010 comprehensive heart failure practice guideline. J Card Fail. https://doi.org/10.1016/j.cardfail.2010.04.004
Dickstein K, Cohen-Solal A, Filippatos G et al (2008) ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2008. Eur Heart J. https://doi.org/10.1093/eurheartj/ehn309
Latifi S, Lidsky K, Blumer JL (2000) Pharmacology of inotropic agents in infants and children. Prog Pediatr Cardiol. https://doi.org/10.1016/S1058-9813(00)00059-X
Funding
The authors have no funding source to disclose.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare that they have no conflict of interest.
Ethical Approval
This is a retrospective chart review with no identifiable individual data. No procedures were performed for the sole purpose of the study. The study was approved by the institutional research committee to be compliant with ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Howard, A., Hasan, A., Brownlee, J. et al. Pediatric Myocarditis Protocol: An Algorithm for Early Identification and Management with Retrospective Analysis for Validation. Pediatr Cardiol 41, 316–326 (2020). https://doi.org/10.1007/s00246-019-02258-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-019-02258-1