Abstract
Little research attention has been paid to the occurrence of heart failure (HF) in children with complex congenital heart diseases (CHDs). Herein, we describe the prevalence, risk factors, and costs associated with HF in complex CHD. Patients aged ≤17 years and diagnosed with a complex CHD on multiple service visits over a 15-year period in the SC Medicaid dataset (1996–2010) were tracked and analyzed. The cohort included 2999 unduplicated patients; 51.0% were male; 34.4% were African American. HF was diagnosed in 7.6%. Single ventricle lesions, genetic syndromes, and ventricular arrhythmia were significantly associated with an increased likelihood of being diagnosed with HF, controlling for development of comorbid pulmonary hypertension. Patients with HF received significantly more subspecialty care, more surgeries, more hospitalizations, more total days of inpatient care, and more emergency department care than those without HF. Patients with significantly higher total care costs paid by Medicaid had HF, more cardiac surgeries, and more specialized mechanical or other support procedures, controlling for diagnosed single ventricle CHD, a genetic syndrome, and number of non-cardiac surgeries. Complex CHD patients with HF incur significantly higher care costs but require multifaceted, intensive supports for management of incident complications and comorbid conditions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Survival rates for children with complex congenital heart disease (CHD) have increased in the past 15 years and services to these children have expanded dramatically [1,2,3,4]. At the same time, there has been an increasing recognition of heart failure (HF) in the pediatric population over the last 2 decades. Regardless of its underlying etiology, HF is commonly defined as a clinical and pathophysiological syndrome characterized by impairment of ventricular dysfunction (volume and pressure overload alone or in combination), the underlying structural malformation, age, and other precipitating factors, leading to inadequate end-organ perfusion [5, 6]. In children, HF can present as respiratory distress, easy fatigability, poor tolerance to exercise, or arrested growth and development, and is ultimately associated with substantial morbidity [7,8,9,10,11]. Some CHDs are also directly associated with ventricular dysfunction, so HF might be more frequent among pediatric patients with these structural abnormalities [5]. However, the prevalence and burden of pediatric HF are largely unknown, especially in the United States and in relation to specific underlying etiologies, such as complex CHD (i.e., hypoplastic left heart syndrome, Tetralogy of Fallot, etc.) [12]. In one extant study of HF in a pediatric CHD cohort treated in a tertiary care hospital, the rate of HF was 6.2% [13]. Cases of simple and complex CHD lesions are often combined in clinical epidemiologic and outcome studies, so that differences in their occurrence, natural history, and prognosis leading to HF are often obscured.
Furthermore, limited data exist regarding the costs of pediatric HF and are predominantly based on inpatient care, with no data available on non-hospital service costs. Previous studies examined separate episodes of care rather than the costs of care over multiple episodes for individual patients. Complications and prolonged lengths of stay (LOS) after congenital heart surgery are associated with significant costs [14]. The greatest charges are typically incurred in patients requiring specialized procedures such as extracorporeal membrane oxygenation (ECMO) or ventricular assist devices (VAD) [9, 15, 16]. Graft survival after pediatric heart transplantation is generally <20 years, but the costs of transplantation and subsequent care are also substantial [7]. Complications, including tracheostomy, mechanical circulatory support, sepsis, stroke and respiratory failure, renal failure, and unplanned reoperation or re-intervention, have also been associated with higher costs [9, 14]. Moreover, patients with single ventricle CHD not only incur high hospital costs during staged surgical palliation, but also those with comorbid non-cardiac diagnoses have higher health care resource utilization [17]. Further study is needed to understand potential factors driving these higher costs over time [14].
Based on prior investigations, then, it is important to further describe the costs associated with HF in patients with complex CHDs as well as to expand the scope of investigation beyond hospital-based tertiary care facilities for population-based estimates of pediatric HF. Herein, we identify the prevalence of HF in a large, community-based service system cohort of children diagnosed with complex CHDs and investigate the clinical factors most significantly associated with an increased likelihood of a HF diagnosis and its higher total costs of care compared to those without HF.
Methods and Materials
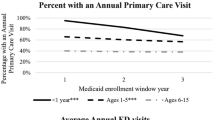
Data for this clinical epidemiologic study were obtained retrospectively from the South Carolina (SC) Medicaid database during a 15-year period from January 1, 1996 through December 31, 2010. Annually, about 375,000 children are covered by Medicaid; over the 15-year period examined in this study, about 500,000 were included in the Medicaid dataset. Access to healthcare in SC is funded predominantly by public (for low-income families) or private insurance payers, which cover about 90 and 10%, respectively, of the children and adolescents residing in the state. In SC, private insurance or self-pay patients initially diagnosed with a disabling CHD may apply for Medicaid coverage of his/her special medical needs regardless of income level, as long as Medicaid eligibility is maintained. There are three subspecialty clinics in each major region of SC and these pediatric cardiologists work closely with primary care centers throughout the state. When intensive, medical intervention is warranted, the patient is referred to tertiary care hospitals such as the Medical University of South Carolina or to Duke University Medical Center for care.
Medical claims were used to identify each patient’s service visits, date of service, and the International Classification of Diseases, 9th Clinical Modification diagnosis codes (ICD-9) related to each visit. Pharmacy claims were also coded for the outpatient medications prescribed to these patients. Inclusion criteria for the unduplicated patients were age ≤ 17 years, continuous enrollment in Medicaid for a minimum of nine months in each calendar year, and one or more service encounters with a complex CHD diagnosis (see Table 1 for the diagnoses and ICD-9 codes used). Simple CHDs, including isolated septal defects, patent ductus arteriosus, isolated coarctation, or partial anomalous pulmonary veins, were excluded.
Diagnostic codes were assigned by the licensed treating physician when the service contact/visit was billed to Medicaid. Once the unduplicated patients met the inclusion criteria, his/her service records were included in this longitudinal analysis for all the years he/she remained Medicaid-eligible within the 15-year period. These Medicaid data files are routinely cleaned to eliminate duplicate visit records and frequently updated before being made available for this research analysis. The methods involved in this study were approved by the University of South Carolina Institutional Review Board as exempt from human subject research guidelines (45 Code of Federal Regulations part 46) because existing medical database records for each patient meeting the criteria were de-identified and used for secondary analysis.
The primary outcome variable of interest was HF (see Table 1 for ICD-9 coding). Since previous research has demonstrated an association between HF and single ventricle lesions, these lesions were separated into one category. Other conotruncal/non-single ventricle complex lesions were grouped to include truncus arteriosus, any form of transposition of the great arteries, double outlet right ventricle, Tetralogy of Fallot, pulmonary atresia or stenosis, Ebstein’s anomaly, total anomalous pulmonary venous connections, and endocardial cushion defects. The remaining lesions were grouped as “other lesions.” Other conditions/exposures (comorbidities or complications) which might be associated with HF severity in this cohort were also coded as follows: prematurity, genetic syndrome, ECMO, VAD, transplant surgery, sepsis, renal failure, pulmonary hypertension, ventricular arrhythmia, stroke/cerebrovascular event/hemorrhage, respiratory failure, gastrostomy tube placement, and tracheostomy.
A common econometric approach to investigating the effect of a clinical practice or policy on a health care system is to model its effect on the average cost per patient over time [18, 19]. Applying this approach herein, the cost of each patient’s outpatient visits, emergency department visits, inpatient days, pharmacy claims for cardiac care medications, and total costs of care in Medicaid were calculated. Since the Medicaid reimbursement rate changed only once for a subset of outpatient psychiatric services during the study period and we are primarily interested in the relative per-patient service costs over time between the HF and non-HF groups over the same time period, the calculated costs were not adjusted for inflation using medical care components of the consumer price index. For this cost analysis, the amount paid for each outpatient service visit, emergency department visit, or inpatient hospitalization day billed to Medicaid was tallied, as were the length of stay for each episode of hospitalization and total number of hospitalizations and days of hospitalization.
Statistical Analysis
Descriptive statistical analyses were performed first; unadjusted likelihood ratio Chi-square statistics are reported to distinguish the HF and non-HF groups. To address research questions regarding clinical factors differentiating cases with and without HF, one multiple logistic regression equation was constructed. The measure of association reported is the adjusted odds ratio (aOR) with a corresponding 95% confidence interval. P values of less than 0.05 (two-sided tests) were considered statistically significant. Ordinary least squares regression was then used to model the clinical factors most highly associated with total costs paid for the care of these cases by Medicaid. Because the studentized residuals using the raw total cost variable were skewed/not normally distributed (i.e., varied widely from year to year so that annual aggregations were not reliable estimates), but those using the log of this variable were normally distributed, a log-transformation of the total cost aggregated across all years the patient was in the Medicaid dataset was used as the dependent variable. T-statistics are presented to demonstrate the significance level of each predictor. All statistical analyses were performed in SAS software, version 9.3 (SAS Institute, Cary, North Carolina).
Results
After applying the inclusion criteria, the final Medicaid cohort included 2999 unduplicated pediatric patients with complex CHD. HF was diagnosed in 229 (7.6%) of these children. Fifty-one percent of the cohort was male; African Americans constituted 34.4% of the cohort, 43.5% were White, and those remaining were small percentages of Hispanics, Asians, Native Americans, or 16.7% mixed/unknown descent. The modal age at complex CHD diagnosis was 0 months (i.e., at birth). These complex CHD patients were followed in the Medicaid dataset for a median of 66 months (IQR = 30–116 months), as long as Medicaid eligibility was maintained. Age at first hospitalization was a median of 0 months (at birth) (IQR = 0–12 months), but 673 children (22.4%) in the cohort were not hospitalized at all during the follow-up period.
Single ventricle lesions were present in 306 (10.2%) of the cohort, conotruncal/non-single ventricle complex lesions in 1410 (47.0%), and other complex lesions in 1283 (42.8%). Related morbidity factors were diagnosed in the CHD cohort as follows: prematurity (0.3%), genetic syndromes (9.5%), kidney failure (0.8%), pulmonary hypertension (2.8%), ventricular arrhythmia (12.7%), stroke/cerebrovascular attack/hemorrhage (1.1%), respiratory failure (1.6%), or sepsis (0.2%). Specialized surgical procedures possibly related to HF were documented as follows: ECMO or VAD (0.1%), heart transplant (0.6%), gastrostomy tube placement (2.8%), or tracheostomy (4.5%).
Demographics and related medical diagnoses are compared across those with and without HF in Table 2. African Americans with complex CHD were less likely to be diagnosed with HF, while children with single ventricle lesions, ventricular arrhythmia, and genetic syndromes were more likely to be diagnosed with HF. Moreover, receipt of transplant surgery, a catheter procedure, or an electrophysiology procedure, and complications such as pulmonary hypertension were more likely to occur in those diagnosed with HF. Few non-cardiac complications such as sepsis, renal failure, stroke/cerebrovascular events, or respiratory failure occurred, but there was greater incidence of renal failure and respiratory failure in those complex CHD patients with HF compared to those without HF.
Clinical factors representing significant differences were then used as independent predictors in the logistic regression analysis. Multivariable logistic regression results indicated that children with these clinical factors were significantly more likely to be diagnosed with HF, controlling for all other clinical factors present (Table 3): single ventricle lesions (adjusted Odds Ratio [aOR] = 2.14), genetic syndromes (aOR = 2.07), pulmonary hypertension (aOR = 3.62), and ventricular arrhythmia (aOR = 3.44).
In the analyses describing services and costs of care as indicated by the amount paid by Medicaid presented in Table 4, complex CHD patients with HF received significantly more subspecialty care, more surgeries, more hospitalizations, more total days of inpatient care, and more emergency department care than those without HF. Mean total costs paid by Medicaid were 3.2-fold higher for complex CHD patients with HF ($105,141) compared to complex CHD patients without HF ($32,899). The mean amounts paid by Medicaid for medical services to these children also differed significantly for inpatient service (2.8-fold higher for the HF group), emergency care (3.0-fold higher for the HF group), outpatient services (2.4-fold higher for the HF group), and outpatient medication services (3.8-fold higher for the HF group) (Table 4). Furthermore, the pattern of service costs differed somewhat between the two groups, with inpatient service costs accounting for 73.7% of the total costs in the HF group versus 71.6% in the non-HF group, whereas outpatient service costs accounted for 18.6% of the total costs in the HF group versus 21.5% in the non-HF group.
The clinical factors most highly associated with log-transformed total costs paid for care of these cases were then modeled in a regression equation. Because the provision of specialized surgical procedures was a low-frequency event, we tallied the total number provided across ECMO, VAD, transplant surgery, gastrostomy tube placement, or tracheostomy to model this variable in the regression, consistent with extant studies. Non-cardiac complications were too infrequently diagnosed to use in the multivariate model. While all the clinical factors modeled represent statistically significant associations with higher total costs paid, three are especially compelling: diagnosed HF (t-statistic = 11.48; <0.0001), number of cardiac surgeries (t-statistic = 29.24; <0.0001), and number of specialized procedures needed (t-statistic = 30.19; <0.0001), controlling for diagnosed single ventricle CHD (t-statistic = 9.05; <0.0001), genetic abnormality/syndrome (t-statistic = 8.61; <0.0001), and number of non-cardiac surgeries (t-statistic = 6.30; <0.0001).
Discussion
Heart failure is a complex clinical syndrome resulting from multiple, diverse underlying structural causes such as type of CHD, increasing age, and other precipitating factors [5]. The prevalence of pediatric HF has been largely unreported, especially in relation to specific underlying etiologies, such as complex CHDs [5, 12]. Herein, we have shown HF to be diagnosed in 7.6% of children with complex CHDs in a population-based study, which generally comports with the rate of 6.2% previously identified in a tertiary care hospital [13]. Furthermore, 20.5% of those with HF had single ventricle anomalies, compared to the 10–14% reported previously [20]. Most types of complex CHD are diagnosed during infancy, accounting for the higher percentage of HF admissions among children <1 year of age, ~55–60% [21]. As would be expected, we also demonstrated that the median age of first hospitalization (representing 50% of the cohort) was at birth.
In the multivariate analysis, genetic abnormalities, single ventricle lesions, and ventricular arrhythmia were significantly associated with developing HF, along with the comorbid complication of pulmonary hypertension. Although genetic syndromes generally account for varying amounts of pediatric CHD cases [5, 22, 23], we found 9.5% in this complex CHD cohort. Moreover, genetic syndrome cases were 2-fold more likely to be diagnosed with HF. While there is a clear recognition that genetic syndromes are often associated with complex CHD and extracardiac complications, the clinical entity of HF in repaired complex CHD patients with genetic abnormalities may be widely under-recognized [22]. Furthermore, single ventricle lesions represent the greatest severity of ventricular dysfunction and association with HF [5]. The 2-fold increase in likelihood of the onset of HF for the single ventricle subgroup demonstrated herein would be an expected finding for many practitioners. Conversely, ventricular arrhythmia is a clinically well-documented precipitator of HF and was diagnosed in 12.5% of this cohort, while pulmonary hypertension is a widely acknowledged comorbid complication of HF and CHD [24, 25]. However, our results suggested that conotruncal/non-single ventricle lesions were not significantly associated with an increased risk of HF as would be expected based on previous studies [5]. Therefore, our results suggest that in a community-based care system, practitioners should exercise a heightened awareness for the development of heart failure in patients with single ventricle lesions and genetic syndromes who develop ventricular arrhythmia or have evidence of burgeoning elevations in pulmonary vascular resistance.
Our results also add to the very limited existing knowledge base regarding the costs of pediatric HF-related hospitalizations and non-hospitalization service costs [12]. The mean amounts paid by Medicaid for medical services to these children over time were 2- to 3-fold higher in the HF group for inpatient service, emergency care, outpatient services, outpatient medication services, and total service costs. Furthermore, the patterns of service costs differed somewhat between the two groups, with inpatient service costs accounting for 73.7% of the total costs in the HF group versus 71.6% in the non-HF group, whereas outpatient service costs accounted for 18.6% of the total costs in the HF group versus 21.5% in the non-HF group.
All the clinical factors examined as predictors of higher total per-episode medical costs paid in complex CHD cases were significantly related to our “total per-patient costs over time”: diagnosed HF, number of cardiac surgeries, and number of specialized procedures needed, controlling for diagnosed single ventricle CHD, genetic syndrome, and number of non-cardiac surgeries. Our results from a population-based cohort generally comport with the findings of other investigators conducted predominantly in tertiary care, hospital facilities. Since (a) very few of our patients received high-cost, specialized surgical procedures such as ECMO, VAD, or transplantation, (b) very few were diagnosed with non-cardiac complications which would prolong hospital stays or require additional intensive treatment, and (c) only Medicaid-reimbursed costs for one state were used in this analysis, these “total per-patient costs” are likely to be considerably lower than those “per-episode costs” reported from tertiary care facilities.
Strengths and Limitations
There are several ways in which this research cohort differed from those of previous epidemiologic investigations. Longitudinal data were available on this cohort to examine the more complex defects and those which present later in childhood. Our cohort included a higher percentage of African Americans than previous studies, except those conducted in Atlanta, Georgia, USA [2, 26]. Also, while the percentage of African Americans served in this state’s Medicaid program is higher than their representation in the general population of South Carolina, African American patients were less likely to develop HF. Furthermore, we are unable to separate outcomes or costs for pediatric patients who were covered by private insurance prior to obtaining Medicaid coverage. The pediatric CHD cohort examined represents a large, heterogeneous group of children representative of pediatric patients in routine care settings in small urban/rural area states, especially the southeastern USA states, in terms of age, sex, racial demographics, and Medicaid eligibility [27,28,29], but the results might also be informative to pediatric cardiologists in small countries with predominantly small cities and rural populations. However, we encourage readers to exercise caution in generalizing these results to service settings which differ dramatically from the target group examined herein.
At the same time, some limitations of the study include the following: no gold standard for the clinical diagnosis of HF or ventricle dysfunction; no access to data on fetal diagnosis in terminated pregnancies or stillbirths; and no access to age calculated in days rather than months. Children and adolescents who dropped out of treatment were periodically ineligible for Medicaid, or those who died before they were registered in Medicaid coverage are not represented in this dataset; and a reliance on physician-assigned ICD-9 codes to categorize patients may have contributed some degree of ascertainment bias or coding invalidity. All diagnostic codes reported to Medicaid by a licensed physician for each patient service visit (up to 8 codes) were used in the analysis. While there was potential for misclassification based on individual service visits, over the 5–8 years on average each child/patient was followed in the dataset, the chance of miscoding these severe conditions decreased. The results may not be generalizable to patients with referral limitations or other constraints on access to care or no coverage. We report associations and, as a result, directions of causality cannot be inferred. Finally, although many significant covariates have been controlled for, other unmeasured differences in patients or their treatment, including non-pharmacological treatments, may explain the findings.
Conclusion
Complex CHD patients with HF represent about 7.6% of the total cohort of complex CHD patients and they require more intensive and specialized surgical supports over time, especially those with single ventricle lesions, genetic abnormalities, ventricular arrhythmia, and pulmonary hypertension. Additionally, patients with complex CHD and HF incur significantly higher costs compared to those without HF highlighting that further study on cost-effective treatment strategies is needed for this challenging and growing population.
References
Meberg A, Otterstad JE, Froland G, Lindberg H, Sarland SJ (2000) Outcome of congenital heart defects—a population based study. Acta Pediatr 89:1344–1351
Shuler CO, Black GB, Jerrell JM (2013) Population-based treated prevalence of congenital heart disease in a pediatric cohort. Pediat Cardiol 34(3):606–611
van der Bom T, Zomer AC, Zwinderman AH, Meijboom FJ, Bouma BJ, Mulder BJ (2011) The changing epidemiology of congenital heart disease. Nat Rev Cardiol 8(1):50–60
Wren C, O’Sullivan JJ (2001) Survival with congenital heart disease and need for follow up in adult life. Heart 85:438–443
Hinton RB, Ware SM (2017) Heart failure in pediatric patients with congenital heart disease. Circ Res 120(6):978–994
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, Casey DE Jr, Drazner MH, Fonarow GC, Geraci SA, Horwich T, Januzzi JL, Johnson MR, Kasper EK, Levy WC, Masoudi FA, McBride PE, McMurray JJ, Mitchell JE, Peterson PN, Riegel B, Sam F, Stevenson LW, Tang WH, Tsai EJ, Wilkoff BL, American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines (2013) ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation 128:e240–e327
Dayton JD, Kanter KR, Vincent RN, Mahle WT (2006) Cost effectiveness of pediatric heart transplantation. J Heart Lung Transplant 25:409–415
Law SP, Kim JJ, Decker JA, Price JF, Cabrera AG, Graves DE, Morales DL, Heinle JS, Denfield SW, Dreyer WJ, Rossano JW (2012) Hospital charges for pediatric heart transplant hospitalizations in the United States from 1997 to 2006. J Heart Lung Transplant 31:485–491
Nandi D, Lin KY, O’Connor MJ, Elci OU, Kim JJ, Decker JA, Price JF, Zafar F, Morales DL, Denfield SW, Dreyer WJ, Jefferies JL, Rossano JW (2016) Hospital charges for pediatric heart failure-related hospitalizations from 2000 to 2009. Pediatr Cardiol 37(3):512–518. doi:10.1007/s00246-015-1308-0
O’Connor MJ, Rossano JW (2014) Ventricular assist devices in children. Curr Opin Cardiol 29:113–12122
Rossano JW, Kim JJ, Decker JA, Price JF, Zafar F, Graves DE, Morales DL, Heinle JS, Bozkurt B, Towbin JA, Denfield SW, Dreyer WJ, Jefferies JL (2012) Prevalence, morbidity, and mortality of heart failure-related hospitalizations in children in the United States: a population-based study. J Card Fail 18:459–470
Nandi D, Rossano JW (2015) Epidemiology and cost of heart failure in children. Cardiol Young 25(8):1460–1468. doi:10.1017/S104795111500228021
Massin MM, Astadicko I, Dessy H (2008) Epidemiology of heart failure in a tertiary pediatric center. Clin Cardiol 31(8):388–391
Pasquali SK, He X, Jacobs ML, Shah SS, Peterson ED, Gaies MG, Hall M, Gaynor JW, Hill KD, Mayer JE, Li JS, Jacobs JP (2014) Excess costs associated with complications and prolonged length of stay after congenital heart surgery. Ann Thorac Surg 98(5):1660–1666. doi:10.1016/j.athoracsur.2014.06.032
Faraoni D, Nasr VG, DiNardo JA, Thiagarajan RR (2016) Hospital costs for neonates and children supported with extracorporeal membrane oxygenation. J Pediatr 169(69–75):e1. doi:10.1016/j.jpeds.2015.10.002
Mahle WT, Ianucci G, Vincent RN, Kanter KR (2008) Costs associated with ventricular assist device use in children. Ann Thorac Surg 86(5):1592–1597. doi:10.1016/j.athoracsur.2008.07.022
Thomas ID, Seckeler MD (2016) Resource utilization for noncardiac admissions in pediatric patients with single ventricle disease. Am J Cardiol 117(10):1661–1666
Bloom JR, Hu TW, Wallace N, Cuffel B, Hausman JW, Sheu ML, Scheffler R (2002) Mental health costs and access under alternative capitation systems in Colorado. Health Serv Res 37(2):315–340
Iribarren C, Tolstykh I, Somkin CP, Ackerson LM, Brown TT, Scheffler R, Syme L, Kawachi I (2005) Sex and racial/ethnic disparities in outcomes after acute myocardial infarction: a cohort study among members of a large integrated health care delivery system in northern California. Arch Intern Med 165(18):2105–2113
Rossano JW, Goldberg DJ, Mott AR, Gaynor JW, Lin KY, Falkensammer CB, Shaddy RE, Kaufman BE, Rychik J (2012) The burden of heart failure related hospitalizations in children with single ventricle heart disease in the United States (abstract). Circulation 126(Suppl 21):A11975
Pradat P, Francannet C, Harris JA, Robert E (2003) The epidemiology of cardiovascular defects, Part I: a study based on data from three large registries of congenital malformations. Pediatr Cardiol 24(3):195–221
Formigari R, Michielon G, Digilio MC, Piacentini G, Carotti A, Giardini A, Di Donato RM, Marino B (2009) Genetic syndromes and congenital heart defects: how is surgical management affected? Eur J Cardio-Thoracic Surg 35(4):606–614
Gelb B, Brueckner M, Chung W, Goldmuntz E, Kaltman J, Kaski JP, Kim R, Kline J, Mercer-Rosa L, Porter G, Roberts A, Rosenberg E, Seiden H, Seidman C, Sleeper L, Tennstedt S, Kaltman J, Schramm C, Burns K, Pearson G, Rosenberg E (2013) The congenital heart disease genetic network study: rationale, design, and early results. Circ Res 112:698–706
Hoeper MM, Bogaard HM, Condliffe R, Frantz R, Khanna D, Kurzyna M, Langleben D, Manes A, Satoh T, Torres F, Wilkins MR, Badesch DB (2013) Definitions and diagnosis of pulmonary hypertension. J Am Coll Cardiol 62(25):D42–D50
Lo R, Hsia HH (2008) Ventricular arrhythmias in heart failure patients. Cardiol Clin 26(3):381–403
Botto LD, Correa A, Erickson JD (2001) Racial and temporal variations in the prevalence of heart defects. Pediatrics 107(3):E32
Census (2010a) Health insurance coverage for children under 19 years of age, at or below 200% of Poverty by State, 2006–2008 and 2009–2011. http://www.census.gov/hhes/www/hlthins/data/children/low-income.html. Accessed 30 Jan 2013
Census (2010b) Table D1: children under 18 and their designated parents, and table D2: children under 18 and their designated parents—characteristics of families (including Region). http://www.census.gov/hhes/socdemo/children/data/sipp/well2009/tables.html. Accessed 30 Jan 2013
Census (2010c) Summary file 2, demographic profile 1 by state. http://factfinder2.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=DEC_10_SF2_SF2DP1&prodType=table. Accessed 4 Feb 2013
Acknowledgements
The views expressed do not necessarily represent official findings of the South Carolina Department of Health and Human Services (Medicaid).
Funding
Funding for the analyses in this study was provided through a Clinical Incentive Research Grant from the University of South Carolina, Office of the Provost. No external funding was received.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no conflicts of interest to report.
Ethical Approval
All research procedures performed in this study were in accordance with the ethical standards of the University of South Carolina institutional research committee as noted in the Methods section.
Rights and permissions
About this article
Cite this article
Nandi, D., Rossano, J.W., Wang, Y. et al. Risk Factors for Heart Failure and Its Costs Among Children with Complex Congenital Heart Disease in a Medicaid Cohort. Pediatr Cardiol 38, 1672–1679 (2017). https://doi.org/10.1007/s00246-017-1712-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-017-1712-8