Abstract
Screening with portable echocardiography has uncovered a large burden of latent rheumatic heart disease (RHD) among asymptomatic children in endemic regions, the significance of which remains unclear. This study aimed to determine the 2-year outcomes for children with latent RHD diagnosed by echocardiographic screening. Children identified with latent RHD enrolled in a biannual follow-up program. Risk factors for disease persistence and progression were examined. Of 62 children, 51 (82 %) with latent RHD had a median follow-up period of 25 months. Of these 51 children, 17 (33.3 %) reported an interval sore throat or symptoms consistent with acute rheumatic fever (ARF). Of 43 children initially classified as having borderline RHD, 21 (49 %) remained stable, 18 (42 %) improved (to no RHD) and 4 (10 %) worsened to definite RHD. Of the 8 children initially classified as having definite RHD, 6 (75 %) remained stable, and 2 (25 %) improved to borderline RHD. Two children had confirmed episodes of recurrent ARF, one of which represented the sole case of clinical worsening. The risk factors for disease persistence or progression included younger age (p = 0.05), higher antistreptolysin O titers at diagnosis (p = 0.05), and more morphologic valve abnormalities (p = 0.01). After 2 years, most of the children had a benign course, with 91 % remaining stable or showing improvement. Education may improve recognition of streptococcal sore throat. Longer-term follow-up evaluation, however, is warranted to confirm disease progression and risk factor profile. This could help tailor screening protocols for those at highest risk.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Echocardiographic screening for rheumatic heart disease (RHD) indicates that previous estimates of the global RHD burden may be too low. Studies from RHD-endemic regions worldwide have found evidence of latent RHD in 1–5 % of asymptomatic schoolchildren [1, 2, 5, 8, 11, 15, 16, 18].
Latent RHD refers to children with echocardiographic evidence of RHD who have no known history of acute rheumatic fever (ARF) and no clinical symptoms [14]. A majority of these children (75–98 %) have subclinical RHD [1, 2, 5, 8, 11, 16, 18], latent RHD with no pathologic cardiac murmur [15]. Without echocardiographic screening, these children can be detected only after their valvular disease progresses.
Early detection of RHD through echocardiographic screening may provide a way to identify children at the earliest stages of disease, when secondary prophylaxis has the greatest chance of stopping disease progression. Important questions remain, however, before universal screening in RHD-endemic areas can be recommended. The high sensitivity of echocardiography is well accepted, but its specificity and rate of false-positive results remain questionable. Without a history of acute rheumatic fever (ARF) and without a confirmatory diagnostic test, no “proof” exists that early valvular lesions are, in fact, early RHD. The natural history of latent RHD also is not known. It remains to be determined whether these children are at risk for recurrence of ARF and whether they will progress to clinically significant RHD.
We recently reported a cross-sectional population-based RHD prevalence study of 4,869 Ugandan primary schoolchildren [1]. This report presents the 2-year follow-up evaluation of those with latent RHD.
Methods
Children identified during screening as having latent RHD or mitral regurgitation of unclear significance (MRUS) were eligible for enrollment in this study. We considered children to have latent RHD if they had echocardiographic evidence of RHD during school-based screening but no known history of ARF and no cardiovascular symptoms. At the initial follow-up visit, benzathine penicillin prophylaxis every 4 weeks was started for patients classified as having definite or probable RHD (according to the 2006 guidelines) and at a later follow-up visit for those with advancing lesions. Additionally, benzathine penicillin was prescribed to children classified as having possible RHD (according to the 2006 guidelines [5] ) if they had both functional and morphologic valve changes. Approval for this follow-up program was obtained from the institutional review boards of Children’s National Medical Center (Washington, DC) and Makerere University (Kampala, Uganda).
Each visit used standard forms that included clinical history (sore throat, fever, joint pain, rash, subcutaneous nodules) and information on secondary prophylaxis (prescription, adherence, and reasons for any nonadherence). Educational content on streptococcal sore throat, ARF, and RHD was provided through direct teaching and take-home materials. Families were instructed to seek evaluation of any sore throat with fever. If no alternative cause of symptoms could be confirmed, the children were instructed to receive a single intramuscular benzathine penicillin injection for presumed streptococcal sore throat.
Focused echocardiograms were performed with a standard portable echocardiography machine (GE VIVID I or VIVID Q; Milwaukee WI, USA). Treatment decisions were made during follow-up visits. Echocardiographic studies and clinical history forms were de-identified and stored for later review.
All echocardiographic studies were retrospectively reviewed by a single physician (A.B.) in a blinded fashion using the 2012 World Heart Federation (WHF) guidelines. Initial-intake diagnostic categories (2006 guidelines [5]) were compared with those resulting from application of the 2012 guidelines [13]. A second blinded reviewer (C.S.) reviewed all the studies from the most recent follow-up visit for calculation of inter-reviewer reliability.
The diagnosis at the initial echocardiogram was compared with that at the final echocardiogram. Patients were classified as “improved” if their disease category became less severe (e.g., definite to borderline) and “worsened” if their category became more severe (e.g., normal to borderline). Patients who did not change diagnostic category were classified as “stable.”
Statistical Methods
Contingency table analyses were used to estimate the prevalence of RHD by certainty and by evidence of persistence and progression over time. Likewise, contingency table analyses followed by multiple logistic regression analysis were used to identify risk factors for persistence/progression of RHD. We estimated kappa to evaluate chance-adjusted agreement between reviewers. The statistical significance of reported differences was based on two-tailed tests with the type 1 error set to 5 %.
Results
Study Population
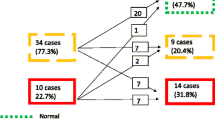
As previously reported [1], we identified 130 asymptomatic Ugandan schoolchildren with an abnormal screening echocardiogram. Figure 1 displays the flow of patients from screening to their status 2 years later. A small group of children (n = 9) classified as having no disease also participated in the follow-up evaluation. These children uniformly had isolated mitral regurgitation 1–1.9 cm in length, with normal mitral valve morphology.
A total of 71 children (62 with latent RHD, 9 with MRUS) were enrolled in biannual follow-up evaluation. Despite multiple attempts to contact patients before each follow-up visit, 11 patients did not return. The reasons for their absence included migration to other towns (n = 4), refusal by parents (n = 1), and nonworking phone contacts (n = 6).
Consequently, 51 children with latent RHD and 9 children with MRUS were restudied at a median follow-up time of 25 months (mean, 20.8 months; range, 7–25 months). The demographic characteristics and echocardiographic findings of these children are presented in Table 1.
Reclassification
The initial 2010 echocardiograms for all 72 children with latent RHD and the 9 children with MRUS were retrospectively reviewed in a blinded fashion. Diagnostic categories were compared between the 2006 [5] and 2012 [13] guidelines (Table 2). Three children initially classified as having possible disease were reclassified as having definite RHD because the 2006 guidelines required a pathologic murmur for probable or definite RHD, whereas the 2012 guidelines did not. Two children initially classified as having definite disease were reclassified as borderline because the 2012 guidelines provide a quantitative cutoff for anterior mitral valve thickness (3 mm), which was previously qualitative [5].
Clinical Follow-up Evaluation
Initially, benzathine penicillin was prescribed at 4-week intervals to 14 children (23 %) (11 with definite RHD and 3 with borderline RHD). For an additional 5 children classified as having borderline RHD, prophylaxis was started during the study period secondary to disease progression (n = 4) or occurrence of ARF (n = 1).
To determine the adherence rate, the number of scheduled injections was divided by the number of received injections. The overall adherence rate was 85.3 %. One child reported rash and was changed to receiving oral erythromycin. The most common reported reasons for nonadherence were misunderstanding regarding completion of the regimen (n = 6) and pain (n = 5).
At the initial intake, no child reported sore throat or ARF in the preceding 6 months. Of 17 children (33.3 %) who reported interval sore throat, 8 had concurrent fever. Seven of these eight patients underwent evaluation that identified two with malaria, one with measles, and four with a single benzathine penicillin injection received for presumed streptococcal sore throat. None of these children experienced the development of ARF.
Two children had clinical and laboratory evidence of ARF during the study period. Neither could remember a sore throat. The first, a 10-year-old girl, had initially received a diagnosis of borderline RHD and was not receiving prophylaxis. She experienced ARF between her 12- and 18-month follow-up appointments. Benzathine penicillin prophylaxis was initiated. No echocardiographic progression was seen.
The second patient, an 11-year-old boy, had initially received a diagnosis of definite RHD and was prescribed monthly benzathine penicillin. He was stable at 6 months but did not report for his 12- or 18-month follow-up visit. He returned at 24 months with worsening of his mitral regurgitation plus new mild aortic regurgitation and reported a hospitalization secondary to recurrent ARF and severe congestive heart failure. He reported 100 % adherence to every-4-week prophylaxis, so he was changed to every-3-week injections. We could confirm his source of benzathine penicillin, but in 2012 Uganda banned drugs from one company that supplied benzathine penicillin due to their “substandard” quality. A chance therefore exists that this boy received poor-quality benzathine penicillin. He was the only child to report worsening of clinical symptoms.
Echocardiographic Follow-up Evaluation
Figures 2 and 3 display the 2-year outcomes. Echocardiography showed nonprogressive valve disease in eight children with MRUS. In one MRUS patient, who initially met all the criteria for significant mitral regurgitation except length of the regurgitant jet, the length of the mitral valve regurgitant jet increased from 1.8 to 2 mm. This changed his diagnosis to borderline disease.
Of the 43 children who initially had borderline RHD, 21 (49 %) were stable, and 4 (10 %) showed worsening with development of morphologic valve changes to accompany their significant mitral regurgitation. These children were reclassified as having definite RHD.
A total of 18 patients (42 %) showed improvement in their mitral regurgitation and no longer met the criteria for significant regurgitation. These were reclassified as having no disease. Two of the eight children initially classified as having definite RHD showed improvement in their mitral regurgitation (jet<2 cm) and were reclassified as having borderline disease. Neither of these children had improvement in valve morphology.
Interreviewer Reliability
The agreement between reviewers on both diagnostic category and presence of mitral regurgitation in two views was perfect (kappa = 1). Measurements of mitral regurgitation length showed almost perfect agreement (ICC = 0.90). The reviewers exhibited less agreement on the following mitral valve morphologic features: mitral valve thickness (ICC = 0.57), restricted leaflet motion (kappa = 0.69), and chordal thickening (kappa = 0.41). The prevalence of excessive anterior mitral valve leaflet mobility and of all aortic valve criteria met were too low for agreement to be assessed.
Predictors of Outcome
Multiple factors present at initial screening were evaluated as potential risk factors for change in disease status. Those who improved were compared with those whose disease persisted or progressed (Table 3). Children with MRUS (because they did not meet the criteria for RHD) were excluded from these analyses. Older children were more likely to improve (p = 0.05). Those with a greater number of mitral valve morphologic changes were less likely to improve (p = 0.013). The mean difference in antistreptolysin O (ASO) titer at the initial evaluation was not found to be predictive. However, to account for outliers, the ASO data also were evaluated in ordinal groups, showing that those with higher ASO levels were less likely to improve (p = 0.05).
Discussion
Echocardiographic survey of asymptomatic school children has proved to be a powerful tool for detecting clinically silent minor valvular pathology [1, 8, 16]. In populations at high risk for rheumatic heart disease, these subclinical changes are reasonably interpreted as signs of latent RHD. If all children with echocardiographically suspected RHD truly have clinically significant disease, previous estimates of the global burden of RHD have grossly underestimated the problem, placing 64 to 72 million children with disease worldwide [11]. Screening to detect these latent RHD cases thus may provide the best hope for reducing global RHD morbidity and mortality in our lifetime.
However, caution must be exercised in our depiction of this latent RHD population. The natural history of RHD detected through echocardiography is only beginning to be understood. We contribute to this nascent body of knowledge in this first study to examine outcomes in latent RHD using the 2012 WHF criteria. Importantly, we show that these cohorts of patients can be followed successfully, with 83 % of our children returning for regular follow-up visits. We also present data showing that family education can increase recognition and health-seeking behavior for streptococcal sore throat and ARF.
In our cohort, stability dominated the short-term clinical picture, with only one child (who experienced ARF recurrence) presenting with symptoms. Likewise, echocardiographic disease categorization remained stable or improved for 90 % of our cohort.
However, not all latent RHD appears benign. Notably, two children had documented ARF recurrences, and one of these children showed marked deterioration in clinical status. Definite RHD tended not to improve, and almost 10 % of our borderline cases progressed to definite RHD. Younger children, those with multiple morphologic abnormalities, and those with elevated ASO titers at the time of initial screening were less likely to improve.
Use of varied echocardiographic criteria for echocardiographic diagnosis of RHD has historically made direct comparison between screening studies challenging. Currently, the WHF has provided the first evidence-based and internationally endorsed set of guidelines, which should allow for standardized reporting. Thus, we reclassified all our patients, originally categorized based on the joint World Health Organization (WHO)–National Institutes of Health (NIH) criteria, according to these new recommendations. This reclassification, specifically its elimination of physical examination, appropriately moved three children from “possible” to “definite” RHD. These children had both functional and morphologic mitral valve abnormalities but lacked an audible murmur.
In addition, the 2012 criteria provide a quantitative cutoff for thickness of the anterior mitral valve leaflet (>3 mm), which downgraded two patients, previously thought to have subjectively thickened valves, from “definite” to “borderline” RHD. Importantly, the new criteria proved to be consistent for implementation between reviewers, with perfect agreement on disease categorization, suggesting the high potential for accurate comparison between future studies.
One of the most puzzling features of latent RHD is that affected children, by definition, have no history of ARF. Clearly, RHD without a history of ARF is not unprecedented because 30–40 % of young adults with rheumatic mitral stenosis are unable to recall ARF [4]. None of the 72 children in our cohort could recall an episode of ARF, and no child had sought treatment for sore throat in the 6 months before screening. This left it unclear whether this lack of preceding symptoms was the result of the children’s lack of clinical disease or simply their lack of diagnosis. Thus, we provided targeted teaching on pharyngitis and ARF at each of our follow-up appointments. The increase in the reporting and evaluation of pharyngitis during the study period suggested that these children in fact had previously unevaluated episodes of pharyngitis and that education about these symptoms could increase health-seeking behavior.
Of more concern are the two children in our follow-up cohort (3.3 %) who experienced ARF. This rate is higher than the only reported recurrence rate from an echocardiographic prevalence study, in which none of the 54 children, all prescribed secondary prophylaxis, experienced ARF during 5–24 months of follow-up evaluation [3]. This is considerably lower than the 2-year recurrence rate of 16.5 % reported for children with a prior episode of confirmed ARF [12]. Nevertheless, we believe it indicates that this population of children with minor valve pathology may be at risk.
Most of the patients in this cohort also showed echocardiographic stability or improvement. Overwhelmingly, the children with MRUS showed no disease progression. It can be argued, even for the one child who showed “progression,” that a change in mitral regurgitation from 1.8 to 2.1 cm is unlikely to represent a clinically meaningful change, even though it tips over the boundary into borderline disease.
Borderline RHD remained stable in 49 % of our cohort and resolved to no disease in 42 % of our population. These outcomes are similar to the report of a 4–12-month follow-up study in Nicaragua showing that 58 % of the children with subclinical RHD remained stable and 32.5 % improved [11]. Slightly higher numbers of disease stability (67.7–68 %) and lower numbers of disease improvement (28–33 %) have been reported from two Indian studies, although patients with 1 cm of mitral regurgitation (MRUS in our study) were included [4, 16].
More robust data exist regarding the outcome of subclinical carditis in patients after an episode of ARF. A systematic review of 1,817 ARF cases found 322 cases of subclinical RHD, giving a weighted pooled prevalence of 16.8 %. Nine of these series followed these patients for at least 3 months (99 patients), with 49 % experiencing complete resolution of subclinical carditis. No distinction was made between stable and progressive disease in the remaining 51 % [17].
Borderline RHD, however, is not necessarily benign. It progressed to definite RHD in 10 % of our cohort and in 0–9.5 % of similarly reported cohorts [3, 11, 16]. Although progression was mild in our group, and no clinical worsening was reported, the development of new morphologic mitral valve pathology suggested the presence of an ongoing inflammatory process.
The frequency whereby borderline RHD was able to persist and progress also has support from those who have subclinical carditis after an episode of ARF. In that context, it is reported that up to 60 % of silent carditis persisted after 5 years of follow-up evaluation.
The importance of finding latent but definite RHD by echocardiographic screening also should be emphasized. Although it is difficult to determine with exact precision based on the variety of historic guidelines, the rates of definite RHD through echocardiographic screening have ranged from 5 to 33.2 per 1,000 children [1, 2, 5, 10, 11, 16, 18]. Although the follow-up data on these children do not reach the huge numbers associated with borderline disease, the findings have shown that they are much less likely to have disease improvement, with only two of our patients (25 %) improving to borderline RHD and none our patients experiencing complete resolution of disease.
Thus the challenge lies in knowing how to differentiate the children with latent RHD who are at risk of disease persistence and progression from those who are not at risk. Historical data on children with subclinical RHD after ARF identify the lack of cardiac murmur at diagnosis [20], milder valvular regurgitation [9], isolated mitral valve disease [19], and avoidance of additional episodes of ARF [6, 7] as good prognostic signs.
Almost all the children in our cohort had both mild and isolated mitral valve involvement at the time of screening, and only two children reported symptoms consistent with ARF. Younger children were less likely to improve. This finding also is supported by data showing that younger children are more likely to experience a recurrence of ARF [12]. In our study, those with more morphologic mitral valve changes were less likely to improve. This is similar to other follow-up studies of screened schoolchildren, which reported that mitral valve regurgitation coexisting with valve deformities was more likely to persist [3].
Finally, higher ASO levels at the time of initial evaluation also predicted persistence or progression of disease. Although more data are needed to verify this finding, it may indicate that proof of recent streptococcal infection may be useful in identifying children at highest risk.
Our study had several inherent limitations. An ideal study would include prospective clinical and echocardiographic follow-up findings for all 4,869 children who participated in the initial school screening. Without these data, we cannot know the baseline rates of sore throat or ARF in this larger population and cannot account for false-negative studies from our initial screening. Additionally, we relied solely on retrospective reporting to identify episodes of pharyngitis. Prospective confirmatory testing would provide better data.
Finally, only children with more advanced or advancing RHD were administered secondary prophylaxis. Thus, although we report rates of secondary prophylaxis and adherence to this prophylaxis, its exact role in determining disease outcome cannot be drawn from these data. A logistically challenging large-scale prospective randomized control trial is needed to answer this question fully.
Finally, 2 years is short in the lifecycle of RHD, which can take decades to manifest clinically. We exercise caution in presuming that short-term outcomes data predict long-term clinical outcomes. However, the stability or improvement of borderline RHD in 91 % of our cohort and similar percentages across other latent RHD cohorts emphasize the benign course for a majority of these children, at least within 2 years after diagnosis. Importantly, children with borderline and definite RHD appear to be at some risk for recurrent ARF, although it is not precisely defined to date. The risk factors for disease persistence and progression include definite RHD, morphologic valve changes, younger age, and evidence of recent streptococcal infection. While we await longer-term follow-up results, we think it prudent both to push forward with research initiatives aimed at expanding our knowledge of latent RHD and to exercise restraint in advocating for these initiatives as a policy matter, especially in the context of severe resource constraints.
References
Beaton A, Okello E, Lwabi P, Mondo C, McCarter R, Sable C (2012) Echocardiography screening for rheumatic heart disease in Ugandan schoolchildren. Circulation 125:3127–3132
Bhaya M, Panwar S, Beniwal R, Panwar RB (2010) High prevalence of rheumatic heart disease detected by echocardiography in school children. Echocardiography 27:448–453
Bhaya M, Beniwal R, Panwar S, Panwar RB (2011) Two years of follow-up validates the echocardiographic criteria for the diagnosis and screening of rheumatic heart disease in asymptomatic populations. Echocardiography 28:929–933
Bland EF, Duckett Jones T (1951) Rheumatic fever and rheumatic heart disease; a twenty-year report on 1,000 patients followed since childhood. Circulation 4:836–843
Carapetis JR, Hardy M, Fakakovikaetau T, Taib R, Wilkinson L, Penny DJ, Steer AC (2008) Evaluation of a screening protocol using auscultation and portable echocardiography to detect asymptomatic rheumatic heart disease in Tongan schoolchildren. Nat Clin Pract Cardiovasc Med 5:411–417
Feinstein AR, Spagnuolo M, Wood HF, Taranta A, Tursky E, Kleinberg E (1964) Rheumatic fever in children and adolescents: a long-term epidemiologic study of subsequent prophylaxis, streptococcal infections, and clinical sequelae: VI. Clinical features of streptococcal infections and rheumatic recurrences. Ann Intern Med 60(Suppl 5):68–86
Majeed HA, Yousof AM, Khuffash FA, Yusuf AR, Farwana S, Khan N (1986) The natural history of acute rheumatic fever in Kuwait: a prospective six year follow-up report. J Chron Dis 39(5):361–369
Marijon E, Ou P, Celermajer DS, Ferreira B, Mocumbi AO, Jani D, Paquet C, Jacob S, Sidi D, Jouven X (2007) Prevalence of rheumatic heart disease detected by echocardiographic screening. N Engl J Med 357:470–476
Meira ZM, Goulart EM, Colosimo EA, Mota CC (2005) Long-term follow-up of rheumatic fever and predictors of severe rheumatic valvar disease in Brazilian children and adolescents. Heart 91:1019–1022
Mirabel M, Celermajer DS, Ferreira B, Tafflet M, Perier MC, Karam N, Mocumbi AO, Jani DN, Sidi D, Jouven X, Marijon E (2012) Screening for rheumatic heart disease: evaluation of a simplified echocardiography-based approach. Eur Heart J Cardiovasc Imaging 13:1024–1029
Paar JA, Berrios NM, Rose JD, Caceres M, Pena R, Perez W, Chen-Mok M, Jolles E, Dale JB (2010) Prevalence of rheumatic heart disease in children and young adults in Nicaragua. Am J Cardiol 105:1809–1814
Pelajo CF, Lopez-Benitez JM, Torres JM, de Oliveira SK (2010) Adherence to secondary prophylaxis and disease recurrence in 536 Brazilian children with rheumatic fever. Pediatr Rheum Online J 8:22
Remenyi B, Wilson N, Steer A, Ferreira B, Kado J, Kumar K, Lawrenson J, Maguire G, Marijon E, Mirabel M, Mocumbi AO, Mota C, Paar J, Saxena A, Scheel J, Stirling J, Viali S, Balekundri VI, Wheaton G, Zuhlke L, Carapetis J (2012) World Heart Federation criteria for echocardiographic diagnosis of rheumatic heart disease-an evidence-based guideline. Nat Rev Cardiol 9:297–309
Remenyi B, Carapetis J, Wyber R, Taubert K, Mayosi BM (2013) Position statement of the World Heart Federation on the prevention and control of rheumatic heart disease. Nat Rev Cardiol 10:284–292
Roberts K, Colquhoun S, Steer A, Remenyi B, Carapetis J (2012) Screening for rheumatic heart disease: current approaches and controversies. Nat Rev Cardiol 10(1):49–58
Saxena A, Ramakrishnan S, Roy A, Seth S, Krishnan A, Misra P, Kalaivani M, Bhargava B, Flather MD, Poole-Wilson PP (2011) Prevalence and outcome of subclinical rheumatic heart disease in India: the RHEUMATIC [Rheumatic Heart Echo Utilisation and Monitoring Actuarial Trends in Indian Children] study. Heart 97:2018–2022
Tubridy-Clark M, Carapetis JR (2007) Subclinical carditis in rheumatic fever: a systematic review. Int J Cardiol 119:54–58
Webb RH, Wilson NJ, Lennon DR, Wilson EM, Nicholson RW, Gentles TL, O’Donnell CP, Stirling JW, Zeng I, Trenholme AA (2011) Optimising echocardiographic screening for rheumatic heart disease in New Zealand: not all valve disease is rheumatic. Cardiol Young 21:436–443
Yavuz T, Nisli K, Oner N, Dindar A, Aydogan U, Omeroglu RE, Ertugrul T (2008) Long-term follow-up results of 139 Turkish children and adolescents with rheumatic heart disease. Eur J Pediatr 167:1321–1326
Yilmazer MM, Oner T, Tavli V, Cilengiroglu OV, Guven B, Mese T, Vitrinel A, Devrim I (2012) Predictors of chronic valvular disease in patients with rheumatic carditis. Pediatr Cardiol 33:239–244
Acknowledgments
We thank the Uganda Heart Institute, its physicians, nurses, and support staff, which made this research possible. This project was supported by Award no. UL1TR000075 from the NIH National Center for Advancing Translational Sciences. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Center for Advancing Translational Sciences or the NIH.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Beaton, A., Okello, E., Aliku, T. et al. Latent Rheumatic Heart Disease: Outcomes 2 Years After Echocardiographic Detection. Pediatr Cardiol 35, 1259–1267 (2014). https://doi.org/10.1007/s00246-014-0925-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-014-0925-3