Abstract
Deterioration of the right ventricular (RV) functions and the increase in the pulmonary arterial pressure (PAP) of children with moderate to severe adenotonsillar hypertrophy (ATH) have been well described. In addition to these complications, this study aimed to investigate the influence of ATH on the conduction system. The study investigated 46 patients with a diagnosis of ATH and 46 healthy control subjects. Conventional echocardiography, P-wave dispersion (Pd), tissue Doppler imaging (TDI) findings, and atrial electromechanical delay (AED) were compared between the patients and the control subjects before and after adenotonsillectomy. The maximum P-wave duration and Pd were significantly higher in the patients than in the control subjects (p < 0.001). The patient group showed significantly greater RV end-diastolic dimension (p = 0.01), right atrial area (p < 0.001), and mean PAP (p = 0.03) but lower E/A ratios for the mitral (p = 0.04) and tricuspid (p = 0.01) valves and a shorter pulmonary flow trace acceleration time (p = 0.03). The tricuspid annular-plane systolic excursion was similar between these groups (p = 0.21). In the patient group, TDI studies showed significantly lower E′/A′ ratios for the tricuspid lateral (p = 0.006) and mitral septal (p = 0.003) segments than in the control group. The myocardial performance index was lower for the mitral lateral, mitral septal, and tricuspid lateral segments in patient group (p < 0.001). Similarly, AED was prolonged in the patient group at all three segments (p < 0.001). Also, the patient group showed a significantly longer interatrial (p = 0.03) and intraatrial (p = 0.04) electromechanical delay. However, all the electro- and echocardiographic parameters were similar between the patients and the control subjects after adenotonsillectomy (p > 0.05). The prolongations in P-wave duration, Pd, and inter- and intraatrial electromechanical delays were first shown in this population. The cardiac changes induced by ATH-associated hypoxia may facilitate arrhythmias during the long term.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Adenotonsillar hypertrophy (ATH) is the leading cause of upper respiratory tract obstruction, obstructive sleep apnea (OSA), and hypoxia in children [2, 23, 35]. It can deleteriously affect the quality of life, somatic growth, and school performance of children [26]. Furthermore, a relationship of ATH with cardiovascular and pulmonary disorders is well described in previous studies [1, 2, 7, 13, 15, 17, 23, 25, 38].
Severe upper respiratory tract obstruction causes apnea or obstructive hypoventilation. Hypoxemia and hypercarbia, by inducing respiratory acidosis, are potent mediators of pulmonary vasoconstriction. Also, neurohumoral factors produced in response to hypoxemia may promote the changes in pulmonary vasculature. Consequently, the pathway may result in cor pulmonale and right ventricular (RV) dysfunction.
Echocardiography currently is most preferred noninvasive method for assessing the right and left ventricular (LV) functions in children. Tissue Doppler imaging (TDI) has been introduced as a relatively new echocardiographic technique that can detect both systolic and diastolic regional myocardial dysfunction earlier than conventional echocardiographic methods [13, 20, 24].
The development of pulmonary hypertension and RV dysfunction have been demonstrated by both conventional Doppler echocardiography and TDI in children with moderate to severe ATH [1, 2, 6, 15, 23, 26, 38]. On the other hand, enlarged atria may increase the conduction time of the impulse originating in the sinus node and also may cause deterioration in spread of the electrical impulse [3, 10]. An increase in P-wave dispersion (Pd) and atrial electromechanical delay (AED) reflects the inhomogeneous propagation of sinus impulses [14]. Thus, they are accepted as electrophysiologic characteristics of atria prone to fibrillation [11, 12]. Measurement of AED can be performed by both electrophysiologic and echocardiographic methods, and clinicians show interest in assessing atrial function using AED in patients with different disease states [3, 8, 28, 30, 37].
Prolongation of AED and Pd has been shown previously in adult patients with chronic obstructive pulmonary disease and OSA [37]. However, to the best of our knowledge, these parameters have not been assessed in children with ATH. This study aimed to evaluate cardiac functions and electrophysiologic characteristics of the atria in children with ATH.
Materials and Methods
Study Population
This prospective study enrolled 46 consecutive ATH patients (29 boys and 17 girls) and 46 healthy control subjects (25 boys and 19 girls). A written informed consent was obtained from all parents of the children, which was approved by the Hospital Ethics Committee. We evaluated all the patients admitted to the ear, nose, and throat (ENT) clinic with reports of snoring, mouth-breathing, noisy breathing, or pauses in breathing during sleep or chronic adenotonsillar infection.
All the patients underwent a complete ENT examination including flexible nasopharyngoscopy. We used the Brodsky scale to grade hypertrophy of the tonsils [4] as follows: grade 1 (tonsils in the tonsillar fossa, barely visible behind the anterior pillars), grade 2 (tonsils easily visible behind the anterior pillars), grade 3 (tonsils extended three-fourths of the way to the midline), and grade 4 (tonsils completely obstructing the airway). Also, adenoid hypertrophy was graded according to the severity of airway obstruction as follows: grade 1 (<25 %), grade 2 (25–50 %), grade 3 (50–75 %), and grade 4 (>75 %) airway obstruction [36].
Adenoid hypertrophy was defined as obstruction blocking more than 50 % of the nasopharyngeal airway. Cases with grade 3 or 4 adenoid or tonsillar hypertrophy were included the study. The exclusion criteria ruled out patients with congenital cardiac anomalies, dysrhythmia, other causes of upper airway obstruction, grade 1 or 2 tonsillar hypertrophy, and incompatibility with echocardiographic examinations. The control group included sex- and age-matched healthy children with no cardiovascular or adenotonsillar disease, respiratory tract infection, or airway obstruction.
P-Wave Dispersion Measurements
All standard 12-lead electrocardiograms were obtained simultaneously at a paper speed of 50 mm/s and standardized at 1 mV/cm (0.08–35 Hz, 500 sps) using the same recorder (MAC 400; GE Medical Systems, Milwaukee, WI, USA). Electrocardiogram tracings of all the children were blindly analyzed by one investigator. Measurements of P-wave duration were obtained manually, performed with calipers to improve accuracy.
The onset of the P-wave was defined as the junction between the isoelectric line and the beginning of the P-wave deflection, and the offset of the P-wave was defined as the junction between the end of the P-wave deflection and the isoelectric line. The maximum P-wave duration (Pmax) and the minimum P-wave duration (Pmin) were measured in the 12 leads, and the Pd was calculated as the difference between the two P-wave durations. The Pd was not measured if fewer than nine leads were available for analysis.
Echocardiographic Examinations
Conventional echocardiographic and TDI studies (Vivid 7 pro, 3-MHz transducer; GE, Horten, Norway) of all the patients and control subjects were performed by a cardiologist blinded to the clinical details. A one-lead electrocardiogram (ECG) was recorded continuously during the echocardiography examinations. All the echocardiographic measurements were averaged over three consecutive beats.
First, two-dimensional, M-mode, pulsed-wave (PW) and continuous-wave Doppler echocardiographic images were acquired. The LV ejection fraction (EF) was calculated from M-mode measurements of LV dimensions at the level of mitral valve leaflets in the parasternal long-axis view. An apical four-chamber view was used for better visualization and measurement of the RV end-diastolic diameter (RVEDd) and the right atrial area (RAA).
The RV base-to-apex shortening during systole was measured as the systolic displacement of the lateral portion of the tricuspid annular-plane systolic excursion (TAPSE) [21]. A sample volume of the PW Doppler was placed between the tips of the mitral and tricuspid leaflets in the apical four-chamber view. The diastolic functions of the left and right ventricles were measured (peak early [E] and late [A] wave velocities of the mitral and tricuspid valves and the E/A ratio). The pulmonary artery flow in the RV outflow tract near the pulmonary valve was recorded by PW Doppler echocardiography in the parasternal short-axis view to measure the acceleration time of the pulmonary flow trace (AT), the RV ejection time (RVET), and the AT/RVET ratio. The AT is the interval between the beginning of the flow and its peak velocity, and RVET is defined as the interval from the onset of RV ejection to the point of systolic pulmonary arterial flow cessation. The mean pulmonary arterial pressure (mPAP) was calculated by the Mahan formula [9]:
Using the same echocardiography device, TDI studies were performed by switching to pulse-wave TDI mode. For TDI, transducer frequencies of 3 MHz were used, with adjustment of the spectral pulsed Doppler signal filters until a Nyquist limit of 15–20 cm/s was reached and the use of minimal optimal gain. The monitor sweep speed was set at 50–100 mm/s to optimize the spectral display of myocardial velocities. The sampling window was positioned as parallel as possible with the myocardial segment of interest to ensure the optimal angle of imaging.
Apical four-chamber views were obtained. The longitudinal peak annular velocities during systole (S′) as well as early (E′) and late (A′) diastole, the E′/A′ ratio, the ejection time (ET), the isovolumic contraction time (ICT), and the isovolumic relaxation time (IRT) were measured at lateral and septal annuli of the mitral valve and the lateral annulus of the tricuspid valve. The myocardial performance index (MPI) at these three segments then was calculated as follows [33]:
For this study, AED was defined as the interval from the onset of the atrial electrical activity (P-wave on surface electrocardiography) to the beginning of the mechanical atrial contraction (A′ wave) (Fig. 1). It was measured from the same cardiac segments mentioned earlier. The difference between the lateral mitral annulus and the tricuspid lateral annulus AEDs was defined as the interatrial conduction delay, and the difference between the mitral septal annulus and the tricuspid lateral annulus AEDs was defined as the intraatrial conduction delay [28].
Statistical Analysis
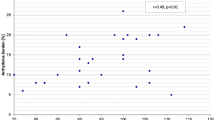
The results were analyzed with a commercially available statistical package (SPSS for Windows, version 17.0; SPSS Inc., Chicago, IL, USA). Continuous variables are presented as means ± standard deviations and categorical variables as ratios. The Chi square test was used for categorical changes. Continuous variables were compared between the groups using Student’s t test or the Mann–Whitney U test depending on whether they were distributed normally or not, as tested by the Shapiro–Wilk test. A p < 0.05 was considered statistically significant.
Results
The baseline demographic and clinical characteristics of the study subjects are presented in Table 1. The mean age was 6.1 ± 2.8 years (range, 2.0–14.5 years) in the patient group and 6.1 ± 1.9 years (range, 3.1–10.5 years) in the control group (p = 0.5). While 43 patients (93 %) had grade 4 and 3 patients (7 %) had grade 3 adenoid hypertrophy, 25 subjects (54 %) had grade 3 or 4 tonsillar hypertrophy.
We performed adenotonsillectomy for 25 patients (54 %) and adenoidectomy for the remaining 21 patients (46 %). All the patients were reevaluated after the 3rd month (mean, 3.7 ± 0.8 months) of the operation. We then compared both the pre- and postoperative data with the findings of the control group.
None of the patients with the diagnosis of ATH had clinically significant arrhythmia. The comparison of ECG parameters among the preoperative, postoperative, and control groups showed no significant differences in terms of heart rate or Pmin among the three groups. However, Pmax and Pd were significantly higher in the ATH patients than the control subjects (95.6 ± 10.5 vs 82.5 ± 8.5 ms; p < 0.001 ms and 54 ± 12.1 vs 40.6 ± 8.4 ms; p < 0.001, respectively). After the surgical treatment, Pmax, Pmin, and Pd did not differ significantly between the patients and the control subjects (Table 2).
All the patients underwent pre- and postoperative echocardiographic evaluation (at the beginning, the study excluded the children with ATH who were incompatible with the examinations). Left ventricular EF and end-diastolic diameter did not differ significantly between the patients and the control subjects (p > 0.05). Similarly, TAPSE showed no difference between in the two groups. However, the patient group had higher mean mPAP values than the control group (p = 0.03).
The increase in RVEDd (p = 0.01) and RAA (p < 0.001) values in the patient group were statistically significant. Also, the E/A ratios at the tricuspid and mitral valves were significantly lower in the patient group than in the control group. Postoperative echocardiographic evaluation of the patient group showed findings similar to those of the control group (Table 3).
Assessment of cardiac functions by TDI demonstrated that the patients with ATH had significantly higher MPI values at all three segments we analyzed. Also, the E′/A′ ratio values were lower on the tricuspid lateral (p = 0.006) and mitral septal (p = 0.003) annuli in the ATH group than in the control group. But it was found to be similar on the mitral lateral annulus between these groups (p = 0.1). However, no significant differences were observed between the patients and the control subjects in terms of TDI parameters in the postoperative evaluation (Table 4).
In all three segments we evaluated, the AED was significantly higher (p < 0.001) in the ATH patients than in the control group. Moreover, the inter- and intraatrial electromechanical delays were longer in the ATH patients than the control group (23.1 ± 6.5 vs 20.1 ± 6.5 ms; p = 0.03 and 14.4 ± 6.3 vs 11.3 ± 6.4 ms; p = 0.04 ms, respectively). Postoperative echocardiographic evaluation showed similar findings in terms of AED as well as inter- and intraatrial electromechanical delay between the patients and the control subjects (Table 4).
Discussion
The current study showed that ATH has a significant effect on mPAP, RV diastolic function, and AED. While RVEDd, RAA, and mPAP were found to be significantly higher in the ATH patients than in the control group, the AT and AT/RVET ratios were lower. Similarly, the decrease in E/A and E′/A′ ratios at the tricuspid valve was statistically significant in the patient group. Moreover, both the inter- and intraatrial electromechanical delays were significantly increased.
All these findings improved after the adenotonsillectomy operation. Recently, the increase in PAP and the deterioration in the cardiac functions of these patients had been demonstrated clearly by some authors. However, the AED change in the children with ATH had not been evaluated previously.
Recent studies have demonstrated that ATH causes higher mPAP and increased RVEDd, which may improve postoperatively [15, 17, 38]. When we assessed the RV and LV diastolic function indices by conventional echocardiography and TDI, we found that the E/A ratio at both the mitral and tricuspid valves of the patients was significantly decreased. Also, the E′/A′ ratios were significantly decreased at the tricuspid lateral and mitral septal segments in the ATH patients, suggesting diastolic dysfunction.
Uğur et al. [35] investigated the effect of the adenotonsillectomy operation on cardiac functions. They observed a significant relief in systolic PAP and diastolic function parameters in both ventricles. However, they showed a statistically significant increase in the E′ value and the E′/A′ ratio at the lateral segment of the mitral valve, in contrast to our study.
El-Moneim et al. [1] demonstrated a significant improvement in the E/A ratio at the tricuspid valve and RVEDd and in the velocity time integral of the tricuspid and pulmonary valve flows after adenoidectomy. They claimed that relieving upper airway obstruction might result in improved RV filling and right ventricle output, associated with the reduction in PAP.
The results of similar studies regarding the effects of ATH on diastolic function and PAP are in accordance with our findings [2, 17, 25, 35, 38]. Additionally, increased RAA in the patient group and the disappearance of these findings after surgery confirm the effects of ATH on PAP in our study, and these had not been evaluated in this group previously. Also, TAPSE did not decrease significantly in the ATH patients, excluding RV systolic dysfunction in our study.
The MPI is a sensitive noninvasive Doppler parameter that can be used to assess global systolic and diastolic myocardial functions at the same time [32]. It is claimed that abnormal systolic function often is accompanied by abnormal diastolic function in patients. Findings have shown that the results achieved by MPI are well correlated with the results observed during cardiac catheterization [33]. Although MPI is traditionally calculated using conventional PW Doppler echocardiography, it is accepted that MPI values achieved by TDI are more reliable than those derived by conventional Doppler echocardiography [2, 18].
Children with ATH had significantly increased preoperative MPI values at the mitral lateral and septal segments and the tricuspid lateral segment in this study. Furthermore, adenotonsillectomy provided a notable relief at all segments we evaluated, with no significant difference relative to the control group.
A few researches have investigated the effects of ATH and OSA on MPI in children and adults. Duman et al. [15] found that RV MPI values were significantly higher in the patient group than in the control group (p < 0.001) and strongly correlated with the mPAP and OSA scores in children. Similarly, Koç et al. [23] showed a significant decrease in MPI and mPAP values 3 months after adenotonsillectomy in children with ATH. While most researchers have focused on the RV functions of patients with ATH, biventricular echocardiographic evaluation has been performed only in a limited number of studies.
Attia et al. [2] investigated the impact of OSA and adenotonsillectomy on global myocardial performance in children with ATH. They demonstrated that patients with OSA had higher systolic and mean PAP, RVEDd, pulmonary vascular resistance, and indexed LV mass (LVMi). Additionally, TDI-derived RV and LV MPI measurements of the patients with OSA were higher than in the control group. Moreover, a repeat of the echocardiographic evaluation showed no significant differences between the patients and the control subjects. Similarly, Chan et al. [7] demonstrated that children with moderate to severe OSA had a significantly higher RV MPI and LVMi than the reference group in a community-based study.
In a study investigating adult patients with OSA, Tavil et al. [31] reported that both RV systolic and diastolic functions were impaired. They also claimed that RV MPI was the parameter most closely related to OSA severity and RV subclinical dysfunction. Similar findings were reported by Tugcu et al. [34] for adult patients with newly diagnosed OSA and normal systemic blood pressure.
On the other hand, Kim et al. [22] noted the negative effects of OSA on the LV diastolic function, and Okuda et al. [27] demonstrated decreased myocardial contractile reserve with dobutamine stress echocardiography in an adult population with OSA.
The entire spectrum of arrhythmias appears to be increased upto 48–58 % during sleep in individuals with OSA [19, 29]. Findings have shown that patients with arrhythmias have more severe nocturnal hypoxemia [19]. Sustained ventricular tachycardia, sinus arrest, second-degree atrioventricular block, frequent premature ventricular contractions, and marked sinus arrhythmia are reported arrhythmias in this population. Furthermore, Gami et al. [16] showed that 49 % of 151 patients undergoing elective cardioversion for atrial fibrillation (AF) had significant OSA. Also, the prevalence of OSA in this group was higher than in high-risk patients with multiple other cardiovascular diseases.
The surface ECGs of the patients in our study did not show any significant arrhythmia. However, we did not perform 24-h rhythm Holter monitoring to assess the rhythm disturbances during sleep.
The P-wave duration on the surface ECG reflects the atrial depolarization time and is mostly affected by the atrial size, left atrial pressure, and interatrial conduction time. Dąbrowska-Kugacka et al. [10] clearly demonstrated that P-wave duration is highly correlated with the AED. An increase in the interatrial electromechanical delay is reported to be an important factor in the pathophysiology of AF.
The prolongation of intra- and interatrial conduction times and the inhomogeneous propagation of sinus impulses are well-known electrophysiologic characteristics of the atrium prone to fibrillate [14, 28, 37]. Yagmur et al. [37] reported that inter- and intraatrial electromechanical delay and Pd were significantly prolonged in adults with moderate to severe OSA. Also, Can et al. [5] showed the prolongation of Pd and P-wave duration in adult patients with OSA and the association with severity of the disease.
Similarly, we demonstrated that Pd, interatrial and intraatrial delays were longer for the children with ATH than for the control subjects. Furthermore, none of these parameters differed significantly among these groups postoperatively.
The current study had several limitations. First, a relatively small number of patients were studied, which may have affected the power of the study. Second, all the ECG and echocardiographic studies were performed by a single observer in blinded fashion, but intra-observer reliability was not assessed. Third, although the ECGs of the patients were normal and the patients had no history of palpitations or syncope, 24-h rhythm Holter monitoring was not performed to assess the rhythm during sleep. Finally, polysomnography was not performed in the patient group due to the lack of a sleep lab in our center. But it was not necessarily because the main purpose of this study was to assess the effects of moderate to severe ATH on the heart.
In conclusion, in accordance with previous reports, our findings showed that children with moderate to severe ATH demonstrate diastolic dysfunction and higher mPAP, right atrial and ventricular dimensions than control subjects. However, prolongations in P-wave duration, Pd, and inter- and intraatrial conduction times were first shown in this patient group. Thus, we state that the cardiac changes induced by ATH-associated hypoxia may facilitate arrhythmias in the long term because this is a known risk factor in adults.
References
Abd El-Moneim ES, Badawy BS, Atya M (2009) The effect of adenoidectomy on right ventricular performance in children. Int J Pediatr Otorhinolaryngol 73:1584–1588
Attia G, Ahmad MA, Saleh AB, Elsharkawy A (2010) Impact of obstructive sleep apnea on global myocardial performance in children assessed by tissue Doppler imaging. Pediatr Cardiol 31:1025–1036
Biliciler-Denktas G, Rao PS (2013) Atrial electromechanical delay measured by tissue Doppler imaging in patients with secundum atrial septal defects. Echocardiography 30:619–620
Brodsky L (1989) Modern assessment of tonsils and adenoids. Pediatr Clin North Am 36:1551–1569
Can I, Aytemir K, Demir AU, Deniz A, Ciftci O, Tokgozoglu L et al (2009) P-wave duration and dispersion in patients with obstructive sleep apnea. Int J Cardiol 133:e85–e89
Cayler GG, Johnson EE, Lewis BE, Kortzeborn JD, Jordan J, Fricker GA (1969) Heart failure due to enlarged tonsils and adenoids: the cardiorespiratory syndrome of increased airway resistance. Am J Dis Child 118:708–717
Chan JY, Li AM, Au CT, Lo AF, Ng SK, Abdullah VJ et al (2009) Cardiac remodelling and dysfunction in children with obstructive sleep apnoea: a community-based study. Thorax 64:233–239
Ciftel M, Turan O, Simşek A, Kardelen F, Akçurin G, Ertuğ H (2012) Assessment of atrial electromechanical delay in children with acute rheumatic fever. Cardiol Young. doi:10.1007/s00246-013-0732-2
Dabestani A, Mahan G, Gardin JM, Takenaka K, Burn C, Allfie A, Henry WL (1987) Evaluation of pulmonary artery pressure and resistance by pulsed Doppler echocardiography. Am J Cardiol 59:662–668
Dąbrowska-Kugacka A, Lewicka-Nowak E, Ruciński P, Zagożdżon P, Raczak G, Kutarski A (2011) Relationship between P-wave duration and atrial electromechanical delay assessed by tissue Doppler echocardiography. Pacing Clin Electrophysiol 34:23–31
Daubert JC, Pavin D, Jauvert G, Mabo P (2004) Intra- and interatrial conduction delay: implications for cardiac pacing. Pacing Clin Electrophysiol 27:507–525
den Uijl DW, Gawrysiak M, Tops LF, Trines SA, Zeppenfeld K, Schalij MJ et al (2011) Prognostic value of total atrial conduction time estimated with tissue Doppler imaging to predict the recurrence of atrial fibrillation after radiofrequency catheter ablation. Europace 13:1533–1540
Di Lisi D, Bonura F, Macaione F, Peritore A, Meschisi M, Cuttitta F et al (2011) Chemotherapy-induced cardiotoxicity: role of the tissue Doppler in the early diagnosis of left ventricular dysfunction. Anticancer Drugs 22:468–472
Dilaveris PE, Gialafos EJ, Sideris SK, Theopistou AM, Andrikopoulos GK, Kyriakidis M et al (1998) Simple electrocardiographic markers for the prediction of paroxysmal idiopathic atrial fibrillation. Am Heart J 135:733–738
Duman D, Naiboglu B, Esen HS, Toros SZ, Demirtunc R (2008) Impaired right ventricular function in adenotonsillar hypertrophy. Int J Cardiovasc Imaging 24:261–267
Gami AS, Pressman G, Caples SM, Kanagala R, Gard JJ, Davison DE et al (2004) Association of atrial fibrillation and obstructive sleep apnea. Circulation 110:364–367
Görür K, Döven O, Unal M, Akkuş N, Ozcan C (2001) Preoperative and postoperative cardiac and clinical findings of patients with adenotonsillar hypertrophy. Int J Pediatr Otorhinolaryngol 59:41–46
Harada K, Tamura M, Toyono M, Yasuoka K (2002) Comparison of the right ventricular Tei index by tissue Doppler imaging to that obtained by pulsed Doppler in children without heart disease. Am J Cardiol 90:566–569
Hoffstein V, Mateika S (1994) Cardiac arrhythmias, snoring, and sleep apnea. Chest 106:466–471
Isaaz K, Thompson A, Ethevenot G, Cloez JL, Brembilla B, Pernot C (1989) Doppler echocardiographic measurement of low-velocity motion of the left ventricular posterior wall. Am J Cardiol 64:66–75
Kaul S, Tei C, Hopkins JM, Shah PM (1984) Assessment of right ventricular function using two-dimensional echocardiography. Am Heart J 107:526–531
Kim SH, Cho GY, Shin C, Lim HE, Kim YH, Song WH et al (2008) Impact of obstructive sleep apnea on left ventricular diastolic function. Am J Cardiol 101:1663–1668
Koç S, Aytekin M, Kalay N, Ozcetin M, Burucu T, Ozbek K et al (2012) The effect of adenotonsillectomy on right ventricle function and pulmonary artery pressure in children with adenotonsillar hypertrophy. Int J Pediatr Otorhinolaryngol 76:45–48
Kocabaş A, Kardelen F, Ertuğ H, Aldemir-Kocabaş B, Tosun O, Yeşilipek A et al (2013) Assessment of early-onset chronic progressive anthracycline cardiotoxicity in children: different response patterns of right and left ventricles. Pediatr Cardiol. doi:10.1007/s00246-013-0735-z
Miman MC, Kirazli T, Ozyurek R (2000) Doppler echocardiography in adenotonsillar hypertrophy. Int J Pediatr Otorhinolaryngol 54:21–26
Naiboglu B, Deveci S, Duman D, Kaya KS, Toros S, Kinis V et al (2008) Effect of upper airway obstruction on pulmonary arterial pressure in children. Int J Pediatr Otorhinolaryngol 72:1425–1429
Okuda N, Ito T, Emura N, Suwa M, Hayashi T, Yoneda H, Kitaura Y (2007) Depressed myocardial contractile reserve in patients with obstructive sleep apnea assessed by tissue Doppler imaging with dobutamine stress echocardiography. Chest 131:1082–1089
Ozer N, Yavuz B, Can I, Atalar E, Aksöyek S, Ovünç K et al (2005) Doppler tissue evaluation of intraatrial and interatrial electromechanical delay and comparison with P-wave dispersion in patients with mitral stenosis. J Am Soc Echocardiogr 18:945–948
Phillips B (2005) Sleep-disordered breathing and cardiovascular disease. Sleep Med Rev 9:131–140
Sengul C, Cevik C, Ozveren O, Sunbul A, Kilicarslan F, Oduncu V et al (2011) Assessment of atrial conduction time in patients with coronary artery ectasia. Pacing Clin Electrophysiol 34:1468–1474
Tavil Y, Kanbay A, Sen N, Ciftçi TU, Abaci A, Yalçin MR et al (2007) Comparison of right ventricular functions by tissue Doppler imaging in patients with obstructive sleep apnea syndrome with or without hypertension. Int J Cardiovasc Imaging 23:469–477
Tei C, Ling LH, Hodge DO, Bailey KR, Oh JK, Rodeheffer RJ et al (1995) New index of combined systolic and diastolic myocardial performance: a simple and reproducible measure of cardiac function—a study in normals and dilated cardiomyopathy. J Cardiol 26:357–366
Tei C, Nishimura RA, Seward JB, Tajik AJ (1997) Noninvasive Doppler-derived myocardial performance index: correlation with simultaneous measurements of cardiac catheterization measurements. J Am Soc Echocardiogr 10:169–178
Tugcu A, Guzel D, Yildirimturk O, Aytekin S (2009) Evaluation of right ventricular systolic and diastolic function in patients with newly diagnosed obstructive sleep apnea syndrome without hypertension. Cardiology 113:184–192
Uğur MB, Dogan SM, Sogut A, Uzun L, Cinar F, Altin R, Aydin M (2008) Effect of adenoidectomy and/or tonsillectomy on cardiac functions in children with obstructive sleep apnea. ORL J Otorhinolaryngol Relat Spec 70:202–208
Wormald PJ, Prescott CA (1992) Adenoids: comparison of radiological assessment methods with clinical and endoscopic findings. J Laryngol Otol 106:342–344
Yagmur J, Yetkin O, Cansel M, Acikgoz N, Ermis N, Karakus Y, Tasolar H (2012) Assessment of atrial electromechanical delay and influential factors in patients with obstructive sleep apnea. Sleep Breath 16:83–88
Yilmaz MD, Onrat E, Altuntaş A, Kaya D, Kahveci OK, Ozel O et al (2005) The effects of tonsillectomy and adenoidectomy on pulmonary arterial pressure in children. Am J Otolaryngol 26:18–21
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kocabaş, A., Salman, N., Ekici, F. et al. Evaluation of Cardiac Functions and Atrial Electromechanical Delay in Children With Adenotonsillar Hypertrophy. Pediatr Cardiol 35, 785–792 (2014). https://doi.org/10.1007/s00246-013-0853-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-013-0853-7