Abstract
To characterize the overall use, cost, and outcomes of extracorporeal membrane oxygenation (ECMO) as an adjunct to cardiopulmonary resuscitation (CPR) among hospitalized infants and children in the United States, retrospective analysis of the 2000, 2003, and 2006 Kids’ Inpatient Database (KID) was performed. All CPR episodes were identified; E-CPR was defined as ECMO used on the same day as CPR. Channeling bias was decreased by developing propensity scores representing the likelihood of requiring E-CPR. Univariable, multivariable, and propensity-matched analyses were performed to characterize the influence of E-CPR on survival. There were 8.6 million pediatric hospitalizations and 9,000 CPR events identified in the database. ECMO was used in 82 (0.9 %) of the CPR events. Median hospital charges for E-CPR survivors were $310,824 [interquartile range (IQR) 263,344–477,239] compared with $147,817 (IQR 62,943–317,553) for propensity-matched conventional CPR (C-CPR) survivors. Median LOS for E-CPR survivors (31 days) was considerably greater than that of propensity-matched C-CPR survivors (18 days). Unadjusted E-CPR mortality was higher relative to C-CPR (65.9 vs. 50.9 %; OR 1.9, 95 % confidence interval 1.2–2.9). Neither multivariable analysis nor propensity-matched analysis identified a significant difference in survival between groups. E-CPR is infrequently used for pediatric in-hospital cardiac arrest. Median LOS and charges are considerably greater for E-CPR survivors with C-CPR survivors. In this retrospective administrative database analysis, E-CPR did not significantly influence survival. Further study is needed to improve outcomes and to identify patients most likely to benefit from this resource-intensive therapy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Survival after pediatric in-hospital cardiac arrest remains poor. Contemporary studies of survival to discharge are variable [29] and have reported rates between 13 and 42 % after conventional cardiopulmonary resuscitation (C-CPR) [11, 13, 25–28, 31, 33, 34, 43–45]. Improved survival has been described for infants, cardiac surgery patients, patients in a critical care setting, and patients with ventricular fibrillation/tachycardia as the initial pulseless rhythm [27, 33, 34, 43]; most recently, an analysis of >3 million hospitalizations estimated survival to discharge at 48 % for hospitalized children who receive CPR [23].
Extracorporeal membrane oxygenation (ECMO) has been employed as a resuscitative support strategy during or shortly after cardiac arrest to improve survival. The use of ECMO in this capacity was first reported in 1992 for a cohort of pediatric cardiac surgery patients [12]; in 1993, Dalton et al. [10] reported 65 % survival to hospital discharge in a cohort of children with severe myocardial dysfunction who arrested and received E-CPR. Subsequently, the use of ECMO during or shortly after cardiac arrest as a resuscitative support measure (E-CPR) has been advocated as a potential strategy to improve outcomes. Reported rates of survival to hospital discharge after pediatric E-CPR are institution-specific and range from 33 to 73 % [2, 3, 10, 12, 18, 19, 30, 38, 41, 44, 49, 50]. This therapy is supported by many centers and is recommended by the American Heart Association (AHA) for consideration during in-hospital pediatric cardiac arrest due to a potentially reversible cause for which standard resuscitation attempts have failed [21].
Although there are several single-center studies [2, 4–6, 17–19, 30, 37, 39, 44] on the use of E-CPR, it is unknown how common the practice is across the United States. In addition, the outcomes reported from single-center, retrospective studies may or may not reflect the outcomes achieved at hospitals that have not reported their outcomes. Knowledge of these data are of critical importance because ECMO is a resource-intensive therapy and, to date, no prospective controlled data exist that show a survival advantage of E-CPR (during or after initial resuscitative efforts) compared with C-CPR in children. Rigorous evaluation of E-CPR is complicated by lack of a treatment control group that received C-CPR; therefore, any potential survival advantage is difficult to ascertain. Thus, we sought (1) to describe the overall frequency of ECMO as a rescue strategy for pediatric patients with in-hospital cardiac arrest in the United States and (2) to test the hypotheses that the use of ECMO after cardiac arrest would result in similar survival with a greater cost and length of stay (LOS) compared with C-CPR.
Methods
Data
With approval from the Baylor College of Medicine Institutional Review Board, we performed a retrospective analysis of the Health Care Cost and Use Project (HCUP) Kids’ Inpatient Database (KID) inclusive of years 2000 2003, and 2006 [16]. The KID, an administrative database released every 3 years since 1997, is a voluntary nationwide sampling of patients ≤ 20 years old discharged from hospitals in participating states. The KID is one of a number of HCUP databases, which are collectively coordinated by the Center for Organization and Delivery Studies within the federal Agency for Health care Research and Quality (AHRQ). State data agencies (private and public) partner with AHRQ to provide the uniform data included in these databases. The resulting databases can provide population-level estimates for use in health services research, including efforts aimed at improving health care delivery.
Systematic random sampling is used to generate the data set, which is weighted to allow population-level prevalence estimates, when desired. Specifically, 80 % of all pediatric and adolescent hospital admissions, 80 % of complicated in-hospital births, and 10 % of uncomplicated in-hospital births are included from each participating state. The hospitals included in the database are specialty hospitals, public hospitals, and academic medical centers.
There were 27 states that contributed data to the 2000 database, 36 states that contributed data to the 2003 database, and 38 states that contributed data to the 2006 database. Data for two to three million pediatric hospitalizations are included in each release of the database; for our analysis, the three most current databases were merged into a single data set containing 8,632,286 discharges. The KID is composed of > 100 clinical and nonclinical variables for each hospital stay, including ≤ 15 diagnoses and 15 procedures for each hospitalization. Ultimately, the large sample size of the KID enables analysis of rare diagnoses and procedures, such as CPR and ECMO, in infants and children.
CPR, ECMO, and other diagnoses and comorbidities were identified by the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9) diagnosis and procedure codes (Data Supplement). Procedure codes (e.g., CPR, ECMO) are identified by the hospital day on which the event occurred, whereas diagnosis codes are summarily applied to the entire hospitalization (precluding temporal association between comorbidities and procedures). Because procedures are identified by hospital day and ICD-9 code in the database, the most specific definition possible consists of identifying CPR and ECMO events that occurred on the same hospital day. Additional database elements include admission and discharge status, patient demographics (e.g., sex, age, race), hospital LOS, hospital characteristics (e.g., location, size, teaching status), and total hospital charges.
The hospital’s location, teaching status, and size were determined by the AHA’s Annual Survey of Hospitals. Bed-size categories are based on hospital beds and are specific to the hospital’s location and teaching status. A hospital is considered to be a teaching hospital if it has an American Medical Association–approved residency program, is a member of the Council of Teaching Hospitals, or has a ratio of full-time equivalent interns and residents to beds ≥0.25. Children’s hospital designations were assigned in the KID based on information provided by the National Association of Children’s Hospitals and Related Institutions (NACHRI). Additional details regarding KID database design, sampling, and quality control have been previously published [46] and are available directly from the HCUP KID Web site [16].
Statistical Analysis
Data were not normally distributed. Categorical variables were reported as proportions, and scale variables were reported as median and interquartile range (IQR). Weighting was not used in this analysis (i.e., all reported values in this study are absolute values encountered in the data set, not calculated prevalence estimates). One-way analysis of variance was used to compare median hospital charges and LOS values between groups, and Dunn’s method was subsequently used for multiple comparison between individual pairs. Univariable analysis of categorical variables was performed by Pearson Chi square or Fisher’s exact test as appropriate, and results were reported using an odds ratio (OR) with 95 % confidence interval (CI). Continuous variables were analyzed using Mann–Whitney U test.
To control for channeling bias related to the likelihood of receiving E-CPR, we developed a propensity score reflecting the likelihood of E-CPR with arrest. Of the risk factors associated with E-CPR, i.e., those that were reliably present on admission (and not present as a potential comorbidity manifested during the hospitalization), were identified and applied to create this propensity score. In nonrandomized studies, propensity scores have been used to control for systematic differences between treatment groups [9]. Given that institutional and systematic differences likely exist regarding the use of E-CPR during resuscitation, propensity scores were generated for each subject using logistic regression with the following variables: age > 1 year, diagnosis of congenital (structural) heart disease, diagnosis of myocarditis, and hospital type (NACHRI children’s hospital designation). Because diagnosis codes in the KID are applied summarily to the entire hospitalization with no temporal information, only factors reliably present on admission (not as a potential complication of resuscitation) were used to generate propensity scores. One-to-two greedy propensity-score matching was then undertaken, effectively pairing one unique E-CPR case with two unique C-CPR cases with similar propensity scores. This model showed good discrimination with a c-statistic of 0.84. No case was used more than once in the propensity-matched group. Similar to previous studies, propensity score matching was used to simulate, to a degree, randomized groups and decrease selection bias between the two study groups [1, 38]. Two-tailed Student t test was used to compare the mean propensity values for use of ECMO between the two propensity-matched resuscitation cohorts (E-CPR vs. C-CPR).
To assess the influence of E-CPR on survival relative to C-CPR, multivariable analysis was performed using logistic regression on the entire unmatched cohort of C-CPR and E-CPR patients. The multivariable model included sex, age > 1 year, NACHRI children’s hospital designation, and the presence of acute renal failure, acute cerebrovascular disease, hepatic disease, sepsis/systemic inflammatory response syndrome (SIRS), arrhythmias, pulmonary hypertension, congenital heart disease, myocarditis, recent invasive cardiovascular procedure (performed before the arrest event), and E-CPR. All variables had < 5 % missing values. A univariate regression was also performed on the propensity-matched cohort. The propensity score matched cohort had 80 % power to detect a 20 % difference in survival with a two-tailed alpha of 0.05.
Propensity score matching was performed using SAS statistical software version 9.1 (SAS, Cary, NC). All other analyses were performed with SPSS, version 18.0 (SPSS, Chicago, IL). Statistical significance was defined as p < 0.05.
Results
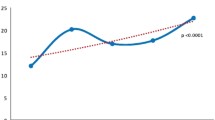
Of 8.6 million pediatric hospitalizations, 9,000 CPR events were identified, which included 82 (0.9 %) E-CPR events. In 2000, E-CPR was used in 16 of 2,427 arrests (0.66 %) compared with 25 of 3,002 arrests in 2003 (0.83 %), and 41 of 3,571 arrests in 2006 (1.15 %). Although E-CPR use increased over time, this trend was not statistically significant (p = 0.102).
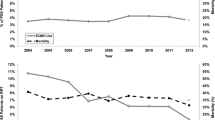
The rates of congenital heart disease, myocarditis, and recent cardiovascular procedures were significantly greater in the E-CPR group (Table 1). Hospitalization in a children’s hospital, myocarditis, and acute CNS disease carried the strongest association with E-CPR. E-CPR was associated with greater hospital charges and greater LOS (Table 2). Excluding patients who were transferred to another acute care hospital after the CPR event, median total hospital charges for the E-CPR group were $205,833 (IQR 114,330–$313,495) compared with a median of $28,259 (8,812–$100,983) for the entire C-CPR group (p < 0.05). E-CPR survivors incurred median charges of $310,824 (263,344–477,239), whereas median charges for C-CPR survivors were $50,392 (9,396–168,268) (p < 0.001). This trend also persisted when comparing the E-CPR cohort to the propensity-matched C-CPR cohort. E-CPR survivors had more than twice the charges relative to propensity-matched C-CPR survivors (median $310,824 vs. $147,817, respectively) (p < 0.05).
Consistent with the discrepant hospital charges between groups, the LOS was considerably longer for the E-CPR group as well. The median hospital LOS (excluding patients who were transferred to another acute care hospital after the CPR event) among survivors was 10 days (IQR 3–34) for the entire C-CPR group, 18 days (IQR 7–48) for the propensity-matched C-CPR group, and 31 days (IQR 19–48) for the E-CPR group (p < 0.001) (Table 2).
Mortality was greater for those undergoing CPR with ECMO support. Unadjusted mortality in the E-CPR group was 65.9 % compared with 50.9 % in the entire (unmatched) C-CPR group (OR 1.9, 95 % CI 1.2–2.9). Other factors associated with increased mortality after C-CPR were age > 1 year, sepsis/SIRS, congenital heart disease, and acute renal failure (p < 0.001 for all) (Table 3). In a multivariable analysis of patients undergoing CPR, age > 1 year, acute kidney injury, and sepsis were all independently associated with death; however, there was no identified survival benefit between the E-CPR and unmatched C-CPR groups (OR death 1.0, 95 % CI 0.6–1.7) (Table 3).
Propensity-matched groups were similar with respect to age, sex, presence/type of cardiac disease, and history of invasive cardiac procedure or congenital heart surgery before resuscitation. Acute CNS disease and acute kidney injury were disproportionately represented in the E-CPR group; this is consistent with analysis of the groups before propensity matching (Table 1), which showed that acute CNS disease and acute kidney injury were among the factors most strongly associated with E-CPR. Furthermore, there was no significant difference between the E-CPR and C-CPR groups with respect to mean propensity score values (e.g., both groups were equally likely to receive ECMO as part of their resuscitation based on the factors we included in the propensity model, whereas only those in the E-CPR group actually received ECMO support during resuscitation). Ultimately, there was no difference in survival identified between the propensity-matched E-CPR and C-CPR groups (34.1 % survival to hospital discharge after E-CPR vs. 43.3 % for C-CPR; OR 0.7 [95 % CI 0.4–1.3]) (Table 4).
Discussion
This large retrospective database analysis of ECMO-supported resuscitation of infants and children is notable for several findings. One of the most striking findings is the overall infrequent use of E-CPR. Of 9,000 episodes of CPR, < 1 in 100 resuscitations included the use of ECMO. Although many centers and the AHA recommend consideration of E-CPR for cardiac arrest not responding to conventional strategies [19, 21, 30, 41], widespread adoption of this therapy has not occurred. There has been a reemphasis in recent years on delivering high-quality CPR [14, 15, 51]. High-quality CPR is associated with improved outcomes among adult cardiac arrest victims. Improvements in attention to depth of compressions, compression frequency, full chest wall recoil, and avoidance of hyperventilation may result in improved survival with C-CPR, which may attenuate the theoretical advantages of E-CPR (e.g., faster clearance of acidosis, improved coronary perfusion pressure) compared with C-CPR. It was not possible to evaluate CPR quality in our study; thus, any contribution of increased C-CPR quality to survival is purely speculative.
Comparison of hospital charges and LOS between the two groups highlights the resource-intensive nature of ECMO. Survivors who received ECMO as a component of resuscitation incurred hospital charges and a LOS approximately twice that of their propensity-matched non-ECMO (C-CPR) counterparts. The contrast in hospital charges between the two groups is even greater when including deaths in the analysis of respective groups as listed in Table 2.
This study is based on a large administrative database containing limited clinical data, thus precluding any ability to draw firm conclusions about differences in morbidity or mortality between the two strategies. The specificity with which patient populations are identified is limited as is the ability to control for demographics, risk factors, and other clinically significant variables in evaluating risk factors and outcome measures. Nonetheless, large databases and registries remain useful in characterizing rare conditions and events. Direct clinical extrapolation may be limited, but these characterizations remain clinically useful approximations of overall use, morbidity, and mortality.
Only 34 % of patients who received ECMO as part of the resuscitation strategy survived to hospital discharge. This is not dissimilar from reported rates of survival to discharge after E-CPR for pediatric patients (38–39 % survival) and pediatric patients with heart disease (42 % survival) in the Extracorporeal Life Support Organization Registry [7, 49]. Nonetheless, whereas no survival advantage was shown compared with C-CPR in this analysis, it remains likely that certain well-defined groups may benefit from E-CPR. There clearly are patients who will not survive an arrest even with the use of ECMO (nearly 70 % in this study). It has been speculated that all patients who have received ECMO during or after CPR would have died without ECMO [20]; however, this hypothesis should be tested further. Survivors of E-CPR generally have shorter duration of CPR before the use of ECMO [4, 5, 18, 44], and because some centers aim to employ ECMO early into resuscitative efforts [18, 44], it should be considered that some of these E-CPR survivors would have survived without the addition of ECMO.
We were able to identify a group of patients for whom E-CPR was more likely. Not surprisingly, children with congenital heart disease and myocarditis, as well as those hospitalized in a children’s hospital, were more likely to undergo CPR with ECMO support. However, no statistically significant difference in survival was noted between the two groups. Our study was powered to detect a 20 % survival difference between the E-CPR and C-CPR groups, and we identified a statistically insignificant 9 % difference in mortality. A larger E-CPR population may provide the statistical power necessary to identify a mathematically significant survival benefit; however, the clinical significance of any potential small/modest survival benefit must be weighed against the known potential for morbidity associated with this costly and resource-intensive resuscitation strategy.
In a 2005 cost analysis of pediatric ECMO, Van Litsenburg et al. [52] argue that identification of subgroups most likely to benefit from ECMO is crucial to improving the cost-effectiveness of this expensive therapy. Similarly, a 2011 editorial by Thiagarajan [48] concludes that insufficient evidence exists to support widespread adoption of pediatric E-CPR and that research is needed to “better defin[e] a population that may be best suited for its use.” Unfortunately, a randomized controlled trial comparing E-CPR and C-CPR will likely never be performed for many reasons, including limited sample size, variations in regional and institutional practice, or institutional unwillingness to randomize. As such, data attempting to directly compare these strategies is limited. A propensity-matched analysis by Lin et al. comparing E-CPR with C-CPR in an adult Taiwanese population [24] found a 30-day survival of 33 % with no difference between E-CPR and C-CPR groups. A recent analysis of infants with hypoplastic left heart syndrome who required resuscitation after Norwood surgery found no difference in 12-month transplant-free survival between E-CPR and C-CPR groups [40].
In the absence of a randomized controlled trial, multicenter or cooperative studies are needed to compare the safety and effectiveness of different resuscitation strategies, and further research to identify patients most likely to benefit from E-CPR is imperative. Without robust evidence to guide clinical application, the widespread adoption and use of E-CPR should be balanced against other less costly measures that may improve mortality in critically ill hospitalized patients. In a 2008 editorial regarding E-CPR in adults [53], Acosta and Varon posited that although this therapy makes physiologic sense and ECMO outcomes have continued to improve, logistic issues at many centers and the absence of randomized control trials precludes any recommendation for widespread or universal availability. The 2010 AHA Pediatric Basic and Advanced Life Support recommendations, which reflect consensus of the 2010 International Liaison Committee on Resuscitation Pediatric Task Force, conclude the following regarding pediatric E-CPR: “ECPR can only be employed if the cardiac arrest occurs in a monitored environment with protocols and personnel for rapid initiation… ECPR may be beneficial for infants and children with cardiac arrest if they have heart disease amenable to recovery or transplantation and the arrest occurs in a highly supervised environment such as an intensive care unit with existing clinical protocols and available expertise and equipment to rapidly initiate ECPR” [22]. Particularly in less specialized centers with fewer resuscitation resources, cost-effective systematic measures directed at preventing or improving CPR (e.g., in-hospital rapid response teams, resuscitation-simulation training, improved postresuscitation care, etc.) [14, 15, 42, 47] may have a much greater impact on patient outcomes than the adoption of costlier or more resource-intensive strategies.
It should be noted that recent advances have resulted in simpler and more efficient extracorporeal devices (oxygenators, circuits, pumps, etc.) which may be more suitable for rapid deployment. Use and outcomes of E-CPR and rapid-deployment ECMO are likely to be impacted by these advances, and more contemporary data will likely reflect this evolution as it becomes available. Notwithstanding, data comparing high-quality conventional CPR with E-CPR are greatly needed.
Limitations
Analysis of large databases may prove useful in overcoming some of the limitations of registries and single-center studies that aim to characterize rare conditions and/or small populations. Nonetheless, there are many shortcomings inherent to the use of an administrative database (such as the KID) to approach these types of clinical questions. First, it should be noted that this is a retrospective study, and results are likely to differ from those obtained from prospective randomized cohorts. Although there are quality-control measures in place to ensure accuracy of the data, there is no panel of cardiologists, intensivists, or resuscitation specialists to adjudicate cases. Clinical data are limited, and factors known to be associated with resuscitation outcomes (such as initial rhythm at onset of arrest, resuscitation duration, underlying cause, characteristics of the initial resuscitative effort, location within the hospital, duration of resuscitation before ECMO, etc.) [8, 13, 27, 32, 35, 36, 54] were not available. Furthermore, the chronological order of diagnoses is not provided. This complicates the distinction between pre-existing risk factors and sequelae of an event or procedures. A propensity-matched analysis is only as robust as the quality and number of variables accounted for in the model; because the chronological order of diagnoses was not provided, we were restricted to include only the risk factors that were reliably present on admission and not a potential complication of the intervention itself (e.g., congenital heart disease, myocarditis, age, children’s hospital status). In addition, the results of laboratory testing and diagnostic studies were not available, and data were not captured after discharge. Thus, quality-of-life measures, neurological sequelae, and other late comorbidities were not available for analysis.
Regarding procedures (e.g., CPR and ECMO), the hospital day of the event is provided, but time and duration are not captured in the database. Thus, our cohort of patients receiving ECMO and CPR on the same calendar day likely includes those meeting a strict definition of E-CPR as well as some with persistent hemodynamic compromise after ROSC. It is unlikely, but possible, that a very small number received CPR after initiation of ECMO. Results may have differed if only cases meeting a strict E-CPR definition had been included; as discussed previously, the degree of clinical detail available in the KID remains one of the greatest limitations to its use in outcome or quality research.
Conclusion
E-CPR is infrequently used for pediatric in-hospital cardiac arrest in the United States. Patients who survived to discharge after E-CPR incurred hospital charges more than twice that of propensity-matched C-CPR survivors and had a considerably longer hospital LOS. In this retrospective administrative database analysis, there was no identified difference in survival to hospital discharge between conventional CPR and CPR involving ECMO. Further study is needed to identify patients most likely to benefit from this costly, resource-intensive therapy.
References
Ahmed A, Zannad F, Love TE, Tallaj J, Gheorghiade M, Ekundayo OJ et al (2007) A propensity-matched study of the association of low serum potassium levels and mortality in chronic heart failure. Eur Heart J 28(11):1334–1343
Alsoufi B, Al-Radi OO, Nazer RI, Gruenwald C, Foreman C, Williams WG et al (2007) Survival outcomes after rescue extracorporeal cardiopulmonary resuscitation in pediatric patients with refractory cardiac arrest. J Vasc Thorac Cadiovasc Surg 134(4):952–959 e952
Chan T, Thiagarajan RR, Frank D, Bratton SL (2008) Survival after extracorporeal cardiopulmonary resuscitation in infants and children with heart disease. J Vasc Thorac Cadiovasc Surg 136(4):984–992
Chen Y-S, Chao A, Yu H-Y, Ko W-J, Wu IH, Chen RJ-C et al (2003) Analysis and results of prolonged resuscitation in cardiac arrest patients rescued by extracorporeal membrane oxygenation. J Am Coll Cardiol 41(2):197–203
Chen Y-S, Lin J-W, Yu H-Y, Ko W-J, Jerng J-S, Chang W-T et al (2008) Cardiopulmonary resuscitation with assisted extracorporeal life-support versus conventional cardiopulmonary resuscitation in adults with in-hospital cardiac arrest: An observational study and propensity analysis. Lancet 372(9638):554–561
Chen Y-S, Yu H-Y, Huang S-C, Lin J-W, Chi N-H, Wang C-H et al (2008) Extracorporeal membrane oxygenation support can extend the duration of cardiopulmonary resuscitation. Crit Care Med 36(9):2529–2535
Conrad SA, Rycus PT (2004) Dalton H (2005) Extracorporeal Life Support Registry Report. ASAIO J 51(1):4–10
Cooper S, Janghorbani M, Cooper G (2006) A decade of in-hospital resuscitation: Outcomes and prediction of survival? Resuscitation 68(2):231–237
D’Agostino RB Jr (2007) Propensity scores in cardiovascular research. Circulation 115(17):2340–2343
Dalton HJ, Siewers RD, Fuhrman BP, del Nido PJ, Thompson AE, Shaver MG et al (1993) Extracorporeal membrane oxygenation for cardiac rescue in children with severe myocardial dysfunction. Crit Care Med 21(7):1020–1028
de Mos N, van Litsenburg RR, McCrindle B, Bohn DJ, Parshuram CS (2006) Pediatric in-intensive-care-unit cardiac arrest: Incidence, survival, and predictive factors. Crit Care Med 34(4):1209–1215
del Nido PJ, Dalton HJ, Thompson AE, Siewers RD (1992) Extracorporeal membrane oxygenator rescue in children during cardiac arrest after cardiac surgery. Circulation 86(Suppl 5):II300–II304
Donoghue A, Berg RA, Hazinski MF, Praestgaard AH, Roberts K, Nadkarni VM (2009) Cardiopulmonary resuscitation for bradycardia with poor perfusion versus pulseless cardiac arrest. Pediatrics 124(6):1541–1548
Edelson DP, Abella BS, Kramer-Johansen J, Wik L, Myklebust H, Barry AM et al (2006) Effects of compression depth and pre-shock pauses predict defibrillation failure during cardiac arrest. Resuscitation 71(2):137–145
Edelson DP, Litzinger B, Arora V, Walsh D, Kim S, Lauderdale DS et al (2008) Improving in-hospital cardiac arrest process and outcomes with performance debriefing. Arch Intern Med 168(10):1063–1069
Healthcare Cost and Utilization Project Kids’ Inpatient Database (KID) (200, 2003, 2006) Healthcare Cost and Utilization Project. Agency for Healthcare Research and Quality, Rockville, MD. www.hcup-us.ahrq.gov/kidoverview.jsp. Accessed 1 Oct 2011
Hei F, Lou S, Li J, Yu K, Liu J, Feng Z et al (2011) Five-year results of 121 consecutive patients treated with extracorporeal membrane oxygenation at Fu Wai Hospital. Artif Organs 35(6):572–578
Huang S-C, Wu E-T, Chen Y-S, Chang C-I, Chiu I-S, Wang S–S et al (2008) Extracorporeal membrane oxygenation rescue for cardiopulmonary resuscitation in pediatric patients. Crit Care Med 36(5):1607–1613
Kane DA, Thiagarajan RR, Wypij D, Scheurer MA, Fynn-Thompson F, Emani S et al (2010) Rapid-response extracorporeal membrane oxygenation to support cardiopulmonary resuscitation in children with cardiac disease. Circulation 122(Suppl 11):S241–S248
Kelly RB, Harrison RE (2010) Outcome predictors of pediatric extracorporeal cardiopulmonary resuscitation. Pediatr Cardiol 31(5):626–633
Kleinman ME, Chameides L, Schexnayder SM, Samson RA, Hazinski MF, Atkins DL et al (2010) Part 14: Pediatric Advanced Life Support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 122(18 Suppl 3):S876–S908
Kleinman ME, de Caen AR, Chameides L, Atkins DL, Berg RA, Berg MD et al (2010) Part 10: Pediatric basic and advanced life support: 2010 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation 122(16 Suppl 2):S466–S515
Knudson JD, Neish SR, Cabrera AC, Lowry AW, Shamszad P, Morales DLS et al (2012) Estimated prevalence and outcomes of pediatric in-hospital cardiopulmonary resuscitation in the United States: An analysis of the Kids’ Inpatient Database. Crit Care Med 40(11):2940–2944
Lin J-W, Wang M-J, Yu H-Y, Wang C-H, Chang W-T, Jerng J-S et al (2010) Comparing the survival between extracorporeal rescue and conventional resuscitation in adult in-hospital cardiac arrests: Propensity analysis of three-year data. Resuscitation 81(7):796–803
Lopez-Herce J, Garcia C, Dominguez P, Carrillo A, Rodriguez-Nunez A, Calvo C et al (2004) Characteristics and outcome of cardiorespiratory arrest in children. Resuscitation 63(3):311–320
Lopez-Herce J, Garcia C, Rodriguez-Nunez A, Dominguez P, Carrillo A, Calvo C et al (2005) Long-term outcome of paediatric cardiorespiratory arrest in Spain. Resuscitation 64(1):79–85
Meaney PA, Nadkarni VM, Cook EF, Testa M, Helfaer M, Kaye W et al (2006) Higher survival rates among younger patients after pediatric intensive care unit cardiac arrests. Pediatrics 118(6):2424–2433
Meert KL, Donaldson A, Nadkarni V, Tieves KS, Schleien CL, Brilli RJ et al (2009) Multicenter cohort study of in-hospital pediatric cardiac arrest. Pediatr Crit Care Med 10(5):544–553
Moler FW, Meert K, Donaldson AE, Nadkarni V, Brilli RJ, Dalton HJ et al (2009) In-hospital versus out-of-hospital pediatric cardiac arrest: A multicenter cohort study. Crit Care Med 377:2259–2267
Morris MC, Wernovsky G, Nadkarni VM (2004) Survival outcomes after extracorporeal cardiopulmonary resuscitation instituted during active chest compressions following refractory in-hospital pediatric cardiac arrest. Pediatr Crit Care Med 5(5):440–446
Nadkarni VM, Larkin GL, Peberdy MA, Carey SM, Kaye W, Mancini ME et al (2006) First documented rhythm and clinical outcome from in-hospital cardiac arrest among children and adults. JAMA 295(1):50–57
Nadkarni VM, Larkin GL, Peberdy MA, Carey SM, Kaye W, Mancini ME et al (2006) First documented rhythm and clinical outcome from in-hospital cardiac arrest among children and adults. JAMA 295(1):50–57
Ortmann L, Prodhan P, Gossett J, Schexnayder S, Berg R, Nadkarni V et al (2011) Outcomes after in-hospital cardiac arrest in children with cardiac disease: A report from Get With the Guidelines—Resuscitation. Circulation 124(21):2329–2337
Parra DA, Totapally BR, Zahn E, Jacobs J, Aldousany A, Burke RP et al (2000) Outcome of cardiopulmonary resuscitation in a pediatric cardiac intensive care unit. Crit Care Med 28(9):3296–3300
Peberdy MA, Kaye W, Ornato JP, Larkin GL, Nadkarni V, Mancini ME et al (2003) Cardiopulmonary resuscitation of adults in the hospital: A report of 14720 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation 58(3):297–308
Peberdy MA, Ornato JP, Larkin GL, Braithwaite RS, Kashner TM, Carey SM et al (2008) Survival from in-hospital cardiac arrest during nights and weekends. JAMA 299(7):785–792
Posner JC, Osterhoudt KC, Mollen CJ, Jacobstein CR, Nicolson SC, Gaynor JW (2000) Extracorporeal membrane oxygenation as a resuscitative measure in the pediatric emergency department. Pediatr Emerg Care 16(6):413–415
Prodhan P, Fiser RT, Dyamenahalli U, Gossett J, Imamura M, Jaquiss RD et al (2009) Outcomes after extracorporeal cardiopulmonary resuscitation (ECPR) following refractory pediatric cardiac arrest in the intensive care unit. Resuscitation 80(10):1124–1129
Prodhan P, Fiser RT, Dyamenahalli U, Gossett J, Imamura M, Jaquiss RDB et al (2009) Outcomes after extracorporeal cardiopulmonary resuscitation (ECPR) following refractory pediatric cardiac arrest in the intensive care unit. Resuscitation 80(10):1124–1129
Ravishankar C, Tabbutt S, Allen K, Cooper DS, Frank DU, Frommelt PC, for the Pediatric Heart Network Investigators, et al (2011) Abstract 9897: Impact of extracorporeal membrane oxygenation and cardiopulmonary resuscitation on Norwood procedure outcomes: Data from the Single Ventricle Reconstruction Trial. Circulation 124(Suppl 21):A9897
Raymond TT, Cunnyngham CB, Thompson MT, Thomas JA, Dalton HJ, Nadkarni VM (2010) Outcomes among neonates, infants, and children after extracorporeal cardiopulmonary resuscitation for refractory inhospital pediatric cardiac arrest: A report from the National Registry of Cardiopulmonary Resuscitation. Pediatric Critical Care Medicine: A Journal of the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies 11(3):362–371
Sahu S, Kishore K, Lata I (2010) Better outcome after pediatric resuscitation is still a dilemma. J Emerg Trauma Shock 3(3):243–250
Samson RA, Nadkarni VM, Meaney PA, Carey SM, Berg MD, Berg RA (2006) Outcomes of in-hospital ventricular fibrillation in children. N Engl J Med 354(22):2328–2339
Sivarajan VB, Best D, Brizard CP, Shekerdemian LS, D’Udekem Y, Butt W (2011) Duration of resuscitation previous to rescue extracorporeal membrane oxygenation impacts outcome in children with heart disease. Intensive Care Med 37(5):853–860
Slonim AD, Patel KM, Ruttimann UE, Pollack MM (1997) Cardiopulmonary resuscitation in pediatric intensive care units. Crit Care Med 25(12):1951–1955
Steiner C, Elixhauser A, Schnaier J (2002) The healthcare cost and utilization project: An overview. Eff Clin Pract 5(3):143–151
Sunde K, Pytte M, Jacobsen D, Mangschau A, Jensen LP, Smedsrud C et al (2007) Implementation of a standardised treatment protocol for post resuscitation care after out-of-hospital cardiac arrest. Resuscitation 73(1):29–39
Thiagarajan RR (2011) Extracorporeal membrane oxygenation to support cardiopulmonary resuscitation: Useful, but for whom? Crit Care Med 39(1):190–191
Thiagarajan RR, Laussen PC, Rycus PT, Bartlett RH, Bratton SL (2007) Extracorporeal membrane oxygenation to aid cardiopulmonary resuscitation in infants and children. Circulation 116(15):1693–1700
Thourani VH, Kirshbom PM, Kanter KR, Simsic J, Kogon BE, Wagoner S et al (2006) Venoarterial extracorporeal membrane oxygenation (VA-ECMO) in pediatric cardiac support. Ann Thorac Surg 82(1):138–144 discussion 144-135
Travers AH, Rea TD, Bobrow BJ, Edelson DP, Berg RA, Sayre MR et al (2010) Part 4: CPR overview: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 122(18 Suppl 3):S676–S684
Van Litsenburg R, de Mos N, Edgell D, Gruenwald C, Bohn DJ, Parshuram CS (2005) Resource use and health outcomes of paediatric extracorporeal membrane oxygenation. Arch Dis Child Fetal Neonatal Ed 90(2):F176–F177
Varon J, Acosta P (2008) Extracorporeal membrane oxygenation in cardiopulmonary resuscitation: Are we there yet? Crit Care Med 36(9):2685–2686
Weil MH, Fries M (2005) In-hospital cardiac arrest. Crit Care Med 33(12):2825–2830
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lowry, A.W., Morales, D.L.S., Graves, D.E. et al. Characterization of Extracorporeal Membrane Oxygenation for Pediatric Cardiac Arrest in the United States: Analysis of the Kids’ Inpatient Database. Pediatr Cardiol 34, 1422–1430 (2013). https://doi.org/10.1007/s00246-013-0666-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-013-0666-8