Abstract
Background
This study aimed to clarify whether children with neurocardiogenic syncope (NCS) differ from healthy control subjects in baseline heart rate variability (HRV) and in their response to orthostatic stress induced by active standing and tilt table.
Methods
This study analyzed the difference between 55 children with a history of NCS or presyncopal symptoms (PS) and healthy control subjects. Measurements included short-term HRV during resting position, tilt table testing, and active standing. Time and frequency domain HRV parameters were computed.
Results
Both the NCS and PS children differed significantly from healthy control subjects during resting position. During tilt table testing, nearly all NCS and PS subjects differed significantly from the control group in calculated HRV parameters. Moreover, for the low-frequency power and total power, the confidence intervals did not overlap.
Conclusions
The findings suggest that chronic autonomic differences exist between healthy children and patients with NCS and PS. These changes could be detected even by short-term HRV recordings. The tilt table maneuver provoked the most prominent differences between the groups. Low-frequency power and total power during tilt table testing helps to detect children with NCS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Syncope is a widespread clinical problem in childhood and adolescence. Approximately 15% of all children experience syncope before reaching adolescence. The most frequent cause of fainting in this age group is neurocardiogenic syncope (NCS) [17, 19, 25].
The European Society of Cardiology defines syncope as a transient, self-limited loss of consciousness, which usual leads to falling. The onset of syncope is relatively rapid, and the subsequent recovery is spontaneous, complete, and relatively prompt. The underlying mechanism is a transient global cerebral dysfunction [3]. Triggers causing global cerebral dysfunction are not fully understood. Previous studies suggest that imbalance in the autonomic control leads to the pathologic reaction during orthostatic stress due to increasing sympathetic tone [1, 11, 12, 15, 21, 23]. Other triggers also considered to be responsible for NCS include hormonal influences or a reduction in cerebral blood flow before the onset of syncope [7].
Heart rate variability (HRV) is caused by intrinsic autonomic oscillators. These oscillators arise from respiratory sinus arrhythmia with a usual frequency of 0.25 Hz from the baroreceptor reflex (Mayer waves) at 0.1 Hz (10-s rhythm of blood pressure), and from thermoregulatory modulations, usually at 0.05 Hz [5, 8, 13, 24]. These oscillators reflect feedback control systems created by the interaction of sympathetic and parasympathetic input and are necessary for the adaptability of the healthy organism.
Heart rate variability can be measured in both long-term recordings lasting 24 h and short-term recordings lasting 5–20 min [24]. The current study did not aim to provoke syncope in children, but sought to detect potential differences in the autonomic nervous system (ANS) function of children with a history of NCS. We investigated a standard test procedure with short standing/head-up tilt duration.
The parameters of HRV were estimated by standardized algorithms via statistical-mathematical methods (time domain parameters) and by fast Fourier transformation (frequency domain parameters) [2, 9, 18, 20, 22].
Only a few studies have investigated HRV in children, with conflicting results. Some investigators have reported that children with NCS had alterations in baseline autonomic balance [23, 26], whereas others did not [15, 21]. Moreover, it has been discussed that children with NCS exhibit abnormalities during orthostatic stress.
This study aimed to measure short-term HRV in children with a history of NCS or presyncopal symptoms (PS) and to compare it with short-term HRV in a healthy control group. We wanted to determine whether the NCS/PS group differed in baseline HRV and in their response to orthostatic stress induced by active standing and tilt table testing.
Materials and Methods
Patients
The study examined 55 children and adolescents 5–15 years of age. These patients had experienced syncope or PS symptoms (dizziness, sweating, weakness, headache, impaired vision, paleness, and nausea) and were therefore admitted to the University Children’s Hospital Mannheim. The NCS diagnosis for these children and adolescents was based on history, symptoms, and exclusion of organic (electrocardiography [ECG], echocardiography, electroencephalography, and blood analysis) and orthostatic (Schellong test) diseases.
All the patients, including 31 with NCS (22 girls and 9 boys) and 24 with PS (15 girls and 9 boys) were free of any medication and healthy, with normal clinical-neurologic examination results. The exclusion criteria for this study specified chronic diseases involving the ANS such as bronchial asthma, epilepsy, and diabetes mellitus.
The control group (gC) consisted of 77 healthy volunteers 5–15 years of age without any medication or history of NCS or PS.
Considering the physiologic maturation of the ANS unique to children [15] (E. Longin and colleagues, unpublished work), we subdivided the groups into children (age, 5–11 years) and adolescents (age, 12–15 years).
Informed written consent was obtained from the parents and/or the participants. Approval of the local ethics commission was obtained.
Study Protocol
The study was conducted in a quiet room with the temperature at 23–25°C in the morning. The subjects did not eat or drink for 2 h before testing.
The analog one-channel ECG signal, derived from surface chest electrodes, was continually recorded on a commercially available bedside monitor (VAGUS 2100; Sigma-Medical-Engineering, Aue, Germany). Upper arm cuff blood pressure was recorded noninvasively every 2 min during the test protocol. Tilt table testing was performed on an electrically driven tilt table. The subjects were not allowed to speak or move during the testing phase. All subjects were asked to indicate any clinical symptoms of orthostatic stress immediately so the testing could be stopped. The testing protocol for both the patient groups and healthy control subjects proceeded as follows:
-
Phase 0: Before the protocol began, the patients were allowed to rest for 10 min in supine position.
-
Phase 1 (baseline): Baseline ECG and blood pressure recordings (every other minute) were performed over a 5-min period. The subjects were kept in supine position.
-
Phase 2 (tilt table): The subjects were tilted to a 60° angle within 3–4 s for 5 min with continuous ECG and blood pressure measurement.
-
Phase 3 (active): After 2 min of recovery in supine position, the subjects stood actively for 5 min. They were instructed to stand up quickly without assistance within 3–4 s.
HRV Data Acquisition
The analog one-channel ECG signal and respiration data were recorded with a combined sensor on a commercially available bedside monitor (VAGUS 2100, Suess-Medical-Engineering, Aue, Germany). This monitor was used to analyze time and frequency domain indices. After signal amplifying and analog-to-digital conversion (sampling rate, 256 Hz) of the ECG signal, QRS complexes were identified stepwise. First, digital nonrecursive low-pass filtering (lowest rate, 5 Hz; highest rate, 25 Hz) of the ECG signal was performed using a fourth order Butterworth filter and subsequent elimination of amplitude artifacts. Second, R-wave detection was performed by a frequency-specific window algorithm. Third, the resulting arrhythmia and ectopic beats were eliminated by estimation of the adaptive mean and standard deviation. Finally, all ECG recordings were reviewed by a physician.
Time Domain
From lists of adjacent R-wave (RR) intervals, we computed the following time domain indices: mean heart rate (BpM) and standard deviation (SD in ms), coefficient of variation (VC) in percentage, expiration/inspiration ratio (E/I), root mean square of successive differences (RMSSD in ms), and the 30/15 ratio (30/15).
Frequency Domain
The time series of adjacent R-wave intervals were transformed to a continuous instantaneous heart rate function by taking reciprocals (heart rate [t i] = 1/length) (RRI) and subsequently linear interpolation with a sampling rate at 4 Hz.
Power spectra were computed with a fast Fourier transformation algorithm from segments of 256 sampling values in the following frequency bands: high frequency (HF, 0.15–0.5 Hz), low frequency (LF, 0.05–0.15 Hz), and very low frequency (VLF, 0.01–0.05 Hz). In each frequency band and within the total spectrum (Total < 0.5 Hz), power (*10e-4 Hz2) and peaks (peak very low frequency (PVLF), peak low frequency (PLF), peak high frequency (PHF)) (Hz) were computed as well as the ratio of medium- to high-frequency power (LF/HF) attributed to sympathetic–parasympathetic balance [6]. Data were compared with 77 normal-range children (Longin et al. unpublished work).
Statistical Analysis
The statistical analysis was performed in cooperation with the Institute of Statistics of the University of Mannheim. Data were analyzed using SAS software (version 8.02). Because we assumed nonnormality of distribution for the HRV parameters, nonparametric tests were used. Comparison of the HRV data within both groups (NCS versus control, PS versus control, and PS versus NCS) was computed for both age groups using the Wilcoxon test for unpaired samples. All p values less than 0.05 were considered significant. To achieve “cutoff” values for our data, we computed the confidence intervals using an alpha of 5%. Sensitivity and specificity were estimated.
Results
All recordings had good technical quality for analysis. None of the study participants fainted or became symptomatic during testing. Physiologic differences in blood pressure and heart rate between the different test intervals were detected (baseline versus tilting versus active standing), but no significant differences in blood pressure measurements between the groups (NCS versus PS versus control subjects) were found.
PS Group Versus NCS Group
The comparison between children with PS (n = 31) and those with NCS (n = 24) showed no significant differences during tilt table testing. During active standing, only the following HRV parameters differed significantly from those for the control subjects: VC and E/I ratio (p = 0.01) in the children, and VLF power (p = 0.01), total power (p = 0.02), and E/I-ratio (p = 0.02) in the adolescents. During baseline measurement, only the children showed significant differences for VLF and total power (p = 0.02). The results are presented separately for the NCS and PS groups and for the two age groups (i.e., children versus adolescents).
NCS Group Versus Control Group of Children
Table 1 shows the significant (p < 0.05) differences in HRV parameters for the children with NCS (n = 12) and the control group (n = 36) for all study phases. All phases, even the baseline testing, showed significant differences, especially in the frequency domain parameters and most prominently during tilt testing. In particular, the NCS group demonstrated significant differences, with higher VLF, LF, and total power as well as a higher LF/HF ratio for nearly all testing phases compared with healthy children. Regarding the peaks in the frequency band, the VLF peak was significantly higher for the NCS children in all test phases. The time domain parameters differed significantly only during tilt testing, with the NCS group showing higher mean heart rates, E/I ratios, and VCs.
NCS Group Versus Control Group of Adolescents
Table 2 shows significant (p < 0.05) differences in HRV parameters for the adolescents with NCS (n = 17) and the control group (n = 36) for all study phases. As mentioned earlier, all testing phases showed significant differences, especially in the frequency domain parameters even for the adolescents. The results are identical to those for the children. The most significant differences were discerned during tilt table testing, with greater VLF, LF, and total power in the NCS group. Regarding the time domain parameter, the adolescents showed a lower 30/15 ratio, higher mean heart rates, and greater VCs during tilt testing. Again, the peak in the VLF spectrum appeared to be at 0.02 Hz (healthy children at 0.01 Hz).
PS Group Versus Control Group of Children
Table 3 shows the significant (p < 0.05) differences in HRV parameters for the children with PS (n = 10) and the control group (n = 36) for all study phases. Compared with the results for the NCS group, the PS group showed less significant differences. The differing parameters were the same as for the NCS group. With regard to the time domain parameters in the PS group, only the 30/50 ratio differed significantly.
PS Group Versus Control Group of Adolescents
Finally, Table 4 includes the significant data obtained from the adolescent PS group. The adolescents with PS showed more significant differences than the children with PS. The differences in relation to the healthy control subjects were most notable during tilt testing and were associated with higher values for VLF and total power as well as a higher LF/HF ratio. The VLF peak was higher in all test phases, and during tilt testing, the frequency domain parameters were greater in the PS group for SD, VC, and E/I ratios.
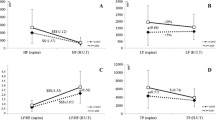
Confidence Intervals
For both age groups, significant differences between the NCS/PS group and the healthy control group were computed during tilt table testing for the following HRV parameters: mean heart rate, VLF, LF, total power, LF/HF ratio, and PVLF (Tables 5 and 6). The children with NCS/PS showed higher values than the healthy control subjects. For these indices, 95% confidence intervals were measured (Tables 5 and 6). In both groups, the specific confidence intervals did not overlap for VLF and total power.
Discussion
Methodologic Aspects
Short-Term Versus Long-Term Recordings
The noninvasive measurement of HRV showed important information for the children with syncope. The current study distinguished children with NCS/PS from healthy children by short-term HRV parameters. A significant finding showed that the NCS/PS group differed from the control subjects in the resting phase. In pediatric practice, a long orthostatic test is stressful for most children because many children will not keep quiet without moving or talking during tilting or active standing. Therefore, short-term HRV is a more realistic option for testing children.
Active Standing Test Versus Tilting
With 51 children, Matsushima et al. [16] examined active standing and head-up tilt test for diagnosis of syncope by frequency domain HRV parameters. These authors concluded that the active standing test was as powerful as tilt table testing for diagnosing syncope in children. Our data confirm this observation, although fewer HRV parameters showed significant difference from tilt table testing parameters. Moreover, our study presents the first standardized time and frequency domain HRV parameters for an active standing test involving children.
Autonomic Changes
A large number of studies have investigated the role of the ANS in the pathogenesis of NCS in adults. For children, only a limited number of studies deal with this issue, and the results of these studies are conflicting. The data presented here suggest that children with NCS or even PS differ from healthy subjects in autonomic pulses at baseline and during tilt testing. The deviating HRV parameters were related to sympathetic and baroreceptor reflex activity, suggesting a chronic elevation of sympathetic tone and baroreceptor sensitivity in children with NCS. These findings are supported by the results of Stewart et al. [23] and Zygmunt and Stanczyk [26]. Both authors also described alterations in basal autonomic balance in children with NCS. Consistent with our results, they demonstrated an increased sympathetic modulation. Whether these chronic alterations in sympathetic tone are the result of fainting or the reason for it cannot be elucidated from our data.
On the other hand, Massin et al. [15] and Alehan et al. [1] did not corroborate any changes in resting autonomic tone in children with NCS. Massin et al. [15] studied a small sample of children with NCS during a 24-h recording in comparison with healthy volunteers and described HRV indices within the normal range.
Mechanisms of Fainting
The cause of fainting in children and adolescents is subject to speculation. A few factors predispose to fainting, although the autonomic responses to orthostatic stress are similar between healthy subjects and frequent fainters. For young adults, triggers of syncope are warm environment, prolonged standing, and pain [4].
The peripheral arteriolar tone plays an important role in blood pressure control. The arteriolar tone is controlled largely by negative feedback through baroreceptor reflexes. During orthostatic stress, peripheral vascular resistance is increased by increasing baroreceptor sensitivity. Patients with NCS evidence a sudden inhibition of sympathetic activity associated with the abrupt reduction in arteriolar tone, which in turn causes an intense vasodilation [7]. The triggers for this “abnormal” physiologic reaction are speculative. The “ventricular theory” [14] considered a paradoxical stimulation of ventricular receptors to be responsible, but this theory is now regarded as obsolete [7].
The role of cerebral vessel reactivity and therefore the cerebral circulation in syncope still is being evaluated. Syncope is very often preceded by hyperventilation. The combination of hypocapnia and hypotension in turn causes a vasoconstrictor response of cerebral vessels and therefore cerebral hypoperfusion [10].
Hormonal changes are associated with syncope. A sudden increase in vasopressin has been shown before the onset of syncope in humans. Vasopressin causes vasoconstriction and increases baroreceptor reflex sensitivity. This might explain the sudden sympathetic inhibition by “overstimulation” [7].
In summary, a few mechanisms contribute to the pathophysiologic reactions that lead to NCS, but to date, no definite explanation elucidates why some humans faint and others do not. By a combination of typical stimuli for syncope, fainting can be induced in most people. Therefore, not only qualitative differences of ANS regulation but also quantitative deviations and threshold phenomena have to be sought.
Prediction
The question whether HRV data, measured at baseline or during tilt table testing, can discern children with NCS or PS from healthy subjects is of great clinical interest. Alehan et al. [1] demonstrated that an LF/HF ratio greater than 2.7 during tilt testing was a specific marker and could correctly predict a positive tilt test in 85% of older children. Lippman et al. [12] suggested that no RMSSD decrease in response to orthostatic stress had 100% specificity and 41% sensitivity for predicting a positive tilt table test result in adults with NCS.
The data obtained from the current study did not confirm the latter results. The LF/HF in the current study significantly distinguished the children with NCS from healthy children during tilt testing, but confidence intervals overlapped. On the other hand, RMSSD, as a time domain parameter, did not reach statistical significance in all recordings. Our data suggest that VLF and total power measured during a 5-min period of tilt testing may serve as a predictive tool to identify potential fainters among children and adolescents. This conclusion must be corroborated with further studies in the future.
Summary
In an effort to clarify the underlying mechanism of ANS changes in NCS, this study suggests that chronic autonomic differences exist between patients with NCS, even those with presyncopal symptoms, and healthy children. Patients with NCS and PS show a higher baseline sympathetic tone at rest and during orthostatic stress. Therefore, HRV analysis may be a useful clinical tool in qualifying patients for therapy and medication.
The novel finding of our study is that these changes were discerned by short-term HRV recordings, which can be performed easily and are less stressful to children.
Tilt table testing shows the most prominent differences between the groups, but even the active standing test seems to be a suitable tool for assessing NCS in childhood.
During tilt table testing, VLF and total power may identify children with NCS.
Age is reported to alter autonomic tone. This must be taken into consideration when pediatric populations are studied with HRV analysis.
References
Alehan D, Ayabakan C, Ozer S (2002) Heart rate variability and autonomic nervous system changes in children with vasovagal syncope. Pacing Clin Electrophysiol 25:1331–1338
Berger RD, Akselrod S, Gordon D, Cohen RJ (1986) An efficient algorithm for spectral analysis of heart rate variability. IEEE Trans Biomed Eng 33:900–904
Brignole M, Alboni P, Benditt D et al (2001) Guidelines on management (diagnosis and treatment) of syncope. Eur Heart J 15:1256–1306
Ganzeboom KS, Colman N, Reitsma JB (2003) Prevalence and triggers of syncope in medical students. Am J Cardiol 91:1006–1008
Giddens DP, Kitney RI (1985) Neonatal heart rate variability and its relation to respiration. J Theor Biol 113:759–780
Goldberger JJ (1999) Sympathovagal balance how should we measure it? Am J Physiol 276:H1273–H1280
Hainsworth R (2004) Pathophysiology of syncope. Clin Auton Res 14(Suppl 1):18–24
Hyndman BW, Kitney RI, Sayers BM (1971) Spontaneous rhythms in physiological control systems. Nature 233:339–341
Kaplan DT (1994) The analysis of variability. J Cardiovasc Electrophysiol 5:16–19
Kaufmann H, Hainsworth R (2001) Why do we faint? Muscle Nerve 24:981–983
Lazzeri C, La villa G, Barletta G, Franchi F (2000) 24-Hour heart rate variability in patients with vasovagal syncope. Pacing Clin Electrophysiol 23:463–468
Lippman N, Stein KM, Lerman BB (1995) Failure to decrease parasympathetic tone during upright tilt predicts a positive tilt-table test. Am J Cardiol 75:591–595
Malik M, Camm AJ (1993) Components of heart rate variability: what they really mean and what we really measure. Am J Cardiol 72:821–822
Mark AL (1983) The Bezold-Jarisch reflex revisited: clinical implications of inhibitory reflexes originating in the heart. J Am Coll Cardiol 1:90–102
Massin MM, Henrard V, Gerard P (2000) Heart rate variability and the outcome of head-up tilt in syncopal children. Acta Cardiol 55:163–168
Matsushima R, Tanaka H, Tamai H (2004) Comparison of active standing test and head-up tilt test for diagnosis of syncope in childhood and adolescence. Clin Auton Res 14:376–384
McHarg ML, Shinnar S, Rascoff H, Walsh CA (1997) Syncope in childhood. Pediatr Cardiol 18:367–371
Merri M, Farden DC, Mottley JG, Titlebaum EL (1990) Sampling frequency of the electrocardiogram for the spectral analysis of heart rate variability. IEEE Trans Biomed Eng 37:99–106
Ruckman RN (1987) Cardiac causes of syncope. Pediatr Rev 9:101–108
Schechtmann VL, Kluge KA, Harper RM (1988) Time-domain system for assessing variation in heart rate. Med Biol Eng Comput 26:367–373
Sehra R, Hubbard JE, Straka SP et al (1999) Autonomic changes and heart rate variability in children with neurocardiac syncope. Pediatr Cardiol 20:242–247
Scherer P, Ohler JP Hirche H, Höpp HW (1993) Definition of a new beat-to-beat parameter of heart rate variability. PACE Pacing Clin Electrophysiol 16:939
Stewart JM, Erb M, Sorbera C (1996) Heart rate variability and the outcome of head-up tilt in syncopal children. Pediatr Res 40:702–709
Task Force of the European Society of Cardiology, the North American Society of Pacing and Electrophysiology (1996) Heart rate variability: standards of measurement, physiological interpretation, and clinical use. Circulation 93:1043–1065
Wieling W, Ganzeboom KS, Saul JP (2004) Reflex syncope in children and adolescents. Heart 90:1094–1100
Zygmunt A, Stanczyk J (2004) Heart rate variability in children with neurocardiogenic syncope. Clin Auton Res 14:99–106
Acknowledgment
This study was supported by the Junior Investigation Fund of the University of Mannheim and by the Dietmar-Hopp-Stiftung, Walldorf, Germany.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Longin, E., Reinhard, J., von Buch, C. et al. Autonomic Function in Children and Adolescents with Neurocardiogenic Syncope. Pediatr Cardiol 29, 763–770 (2008). https://doi.org/10.1007/s00246-008-9198-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-008-9198-z