Abstract
We aimed to evaluate the impact of surgical treatment for urinary stones on perioperative health-related quality of life (HRQOL) using the Japanese Wisconsin Stone Quality of Life questionnaire (J-WISQOL), an HRQOL measure designed for patients with urinary stones. This study prospectively enrolled 123 patients with urinary stones who visited three academic hospitals for stone treatment. The participants completed the J-WISQOL within 4 weeks before and after the urinary stone treatment. Treatments included shock wave lithotripsy (SWL), ureteroscopy lithotripsy, and endoscopic combined intrarenal surgery. J-WISQOL was assessed for age, stone size and location, type of treatment, stone-free status, postoperative ureteral stent placement, hospital stay, and complications in all patients. Patients with stones in the ureter had significantly greater social impact D1 and disease impact D3 than those with stones in the kidney. In a comparison of pre- and postoperative J-WISQOL, patients without postoperative ureteral stent placement scored significantly higher on social impact D1 and disease impact D3. Patients with shorter hospital stays had significantly higher social impact D1 and disease impact D3 (p < 0.001) than those with longer hospital stays. SWL significantly improved the total score, social impact D1, and disease impact D3 compared with other treatments. Perioperative HRQOL in patients with urinary stones is particularly affected by the type of treatment, ureteral stent placement, and hospital stay, which should be considered in surgical selection and patient decision-making.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Health-related quality of life (HRQOL) assesses the impact of health conditions and symptoms on daily life [1]. There is growing interest in the effects of symptoms and treatment on HRQOL. The prevalence of urinary stones has increased owing to dietary changes and lifestyle-related diseases, and the treatment has evolved into a more minimally invasive endoscopic approach [2]. Although technological advances have led to the development of minimally invasive treatments for urinary stones, they still significantly reduce patients’ physical, social, and emotional quality of life. Therefore, the treatment of urinary stones should focus on the patient’s quality of life. In addition, treatment choices should be based on each patient’s HRQOL.
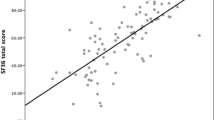
Previous studies have used the Short-Form 36-item survey version 2 (SF-36v2) questionnaire to assess patients with urinary stones and have reported an overall low HRQOL [3]. Although the SF-36v2 is useful for assessing HRQOL, it is not disease-specific. Therefore, the Wisconsin Stone Quality of Life questionnaire (WISQOL) was designed in 2016 to assess HRQOL in patients with urinary stones [4]. We developed and validated a Japanese version of the WISQOL (J-WISQOL) [5] and reported that HRQOL is reduced in the social, emotional, disease, and vitality aspects, owing to the onset and symptoms of urinary stones. However, no study has yet compared the HRQOL pre- and post-operation for urinary stones and the factors associated with these changes by WISQOL. Therefore, this study aimed to evaluate the impact of surgical treatment of urinary stones on perioperative HRQOL using the J-WISQOL.
Materials and methods
Patient selection and data collection
This study was a part of a prospective cohort study performed at Gyotoku General Hospital, Hara Genitourinary Hospital, and Nagoya City University Hospital, which were part of the Skilled Endoscopic Management of Renal & Ureteral Stones (SMART) study group. We retrospectively collected data from 123 patients from our prospective dataset and electronic medical records. This study was conducted in accordance with the Declaration of Helsinki. The study was approved by the Institutional Review Board of Nagoya City University (Approval No. 60-20-0047, June 19, 2020), and written informed consent for publication of their details was obtained from the study participants. Participants completed the J-WISQOL within 4 weeks before and after the urinary stone treatment. Treatments included shock wave lithotripsy (SWL), ureteroscopy lithotripsy (URSL), and endoscopic combined intrarenal surgery (ECIRS). Treatment decisions were made by the patients themselves after detailed counseling by their physicians. The inclusion criteria were age ≥ 18 years, Japanese as the mother tongue, mental ability to provide informed consent, and being scheduled for urinary stone treatment, including those who had experienced surgical treatment for urinary stones in the past. Meanwhile, the exclusion criteria were dementia, significant vision loss, and reoperation for residual stones, which disqualified patients from being recruited. Most patients scheduled for treatment were eligible for enrollment in the study. Among the few cases that were excluded, the main reason was a history of dementia and postoperative dropout.
J-WISQOL was used to assess for age, stone size and location, type of treatment, stone-free status, postoperative ureteral stent placement, hospital stay, and complications in all patients. Patients were divided into groups based on median age, stone size, and length of hospital stay, and stone location (kidney or ureter). The treatment results were determined by plain abdominal radiography, ultrasonography, or plane computed tomography in all patients 4 weeks after treatment. Residual stones were defined as the presence of residual fragments > 4 mm in diameter or calculi that were needed ancillary treatments.
Treatment
SWL was performed using Gemini (Dornier MedTech GmbH, Wessling, Germany) or Delta II (Dornier MedTech GmbH). The patients received an analgesic agent (intravenous pentazocine) and were treated with up to 3000 shocks for renal stones and 4000 shocks for mid- and distal ureteral stones. Patients without complications were discharged the following day.
URSL was performed under spinal or general anesthesia using a Holmium YAG laser through a semi-rigid (Olympus, Tokyo, Japan) or flexible ureteroscope (URF-V2® or URF-V3®, Olympus, Tokyo, Japan). A ureteral access sheath (10/12- or 12/14-Fr BI-FLEX EVO®, Rocamed, Monaco) was also used with a flexible ureteroscope. Furthermore, a 6-Fr ureteral stent was used in most patients after endoscopy and was removed within 4 weeks unless there was a reason for reoperation or complications.
ECIRS was performed under general anesthesia as previously reported [6, 7]. Two surgeons worked simultaneously to crush the renal stones: one performed percutaneous nephrolithotomy, and the other performed retrograde intrarenal surgery. A ureteral access sheath (10/12 Fr; Bi-Flex, Rocamed, Monaco) was placed to facilitate the frequent insertion of the flexible ureteroscope (URF-V2; Olympus Corporation, Tokyo, Japan). At the end of the surgery, a 6-Fr ureteral stent was routinely placed for 1–4 weeks, and as a rule, no nephrostomy tube was inserted.
J-WISQOL characteristics and statistical analysis
The J-WISQOL comprises 28 items with a score range of 1–5 points for each item. The total score ranges from 28 to 140 points, with higher scores indicating a higher HRQOL. The J-WISQOL also evaluated each domain of social, emotional, health, and vitality impacts in addition to the total score. Each domain is rated on a 100-point scale with the score modified according to the number of questions. Continuous data were recorded as median (interquartile range) and analyzed using the Mann–Whitney U-test and Kruskal–Wallis test. The longitudinal scores for each domain were compared between groups using the analysis of variance. Logistic regression was used for univariate and multivariate analyses. Statistical significance was set at p-values of < 0.05. All data were statistically analyzed by two urologists (TO and SH) using EZR for R [8].
Results
This study recruited 153 patients from July 2020 to January 2021, of whom 123 patients completed responses to the J-WISQOL before and after treatment (a flowchart outlining patient recruitment is shown in Fig. 1). There were 87 men and 36 women, with a median age of 55 (45–69) years. The urinary stones were located in the kidney in 35 patients and in the ureter in 88 patients, and the median stone size was 9.0 (6.0–15.0) mm. The treatment included SWL for 35 patients, URSL for 62, and ECIRS for 26 patients. Postoperative ureteral stent placement was performed in 82 patients, (56 URSL patients and 26 ECIRS patients, but not including ESWL patients); six URSL patients had lower ureteral stones treated with semi-rigid ureteroscopy and were in good ureteral condition and did not have ureteral stents placed. These patients underwent either URSL or ECIRS; no ureteral stents were placed in patients who underwent extracorporeal SWL. The median hospital stay was 5 (2–7) days. Residual stones were evaluated 4 weeks after treatment, and 104 patients were stone-free; the overall rate was 84.5%, with only 65.7, 95.2, and 84.6% for SWL, URSL, and ECIRS, respectively. There were no differences in stone-free rates for each treatment across centers. Perioperative complications were observed in eight patients. Most patients had fever associated with urinary tract infections, but all were below Grade II of the Clavien–Dindo classification. The patient background and treatment outcome data are summarized in Table 1.
Preoperative J-WISQOL
The median total score for the preoperative J-WISQOL was 111.0 (95.5–127.0) points. Regarding each domain, median preoperative J-WISQOL scores for social, emotional, disease, and vitality impact were 81.3 (67.2–96.9), 71.4 (57.1–85.7), 68.8 (56.3–84.4), and 75.0 (58.3–91.7) points, respectively, suggesting that onset and symptoms of urinary stones reduced the total HRQOL score and the score in all domains (Table 2).
Patients with stones in the ureter had significantly lower social impact (D1) and disease impact (D3) than those with kidney stones (p = 0.005 and p = 0.045, respectively). There were no significant differences in HRQOL for age or stone size (Table 2).
Postoperative J-WISQOL
The median total score for the postoperative J-WISQOL was 113.0 (102.0–129.0) points. The median postoperative J-WISQOL scores for social, emotional, disease, and vitality impact were 87.5 (68.8–96.9), 71.4 (64.3–89.3), 75.0 (62.5–84.4), and 75.0 (58.3–91.7) points, respectively.
There were no significant differences in J-WISQOL with respect to age, stone size and location, type of treatment, residual stones, postoperative ureteral stent placement, length of hospital stay, or complications.
Difference of pre- and postoperative J-WISQOL
The change in J-WISQOL due to treatment was measured by subtracting the preoperative WISQOL from the postoperative J-WISQOL, which was then examined based on patient characteristics. Regarding postoperative ureteral stent placement, patients without stent placement scored significantly higher than those with placement in terms of social impact D1 (p = 0.007) and disease impact D3 (p < 0.001). Regarding the length of hospital stay, patients with below-median length had significantly higher social impact D1 (p = 0.001) and disease impact D3 (p < 0.001) than those with above-median length. SWL significantly improved the total score (p = 0.015), social impact D1 (p = 0.017), and disease impact D3 (p = 0.004) compared with other treatments. The emotional impact D2 and vitality impact D4 showed no significant differences in any of the characteristics (Table 3).
Multivariate analysis was used to examine the factors that led to the recovery of HRQOL before and after treatment. Achieving stone-free status was a significant factor associated with the recovery of emotional impact D2. Meanwhile, postoperative ureteral stent placement was a significant factor in the recovery from disease impact (Table 4).
Comparison of J-WISQOL in the SWL and URSL groups
Patient background and pre- and postoperative J-WISQOL scores were compared and examined in the SWL and URSL groups. HRQOL related to patient background was different by sex, age, stone size, postoperative placement of ureteral stent, and stone-free status but not by stone location and perioperative complications. The patient background and treatment outcome data are summarized in Table 5. Both pre- and postoperative J-WISQOL scores were not significantly different between the SWL and URSL groups for any impact. In contrast, when comparing pre- and postoperative score changes for each impact and total score, social impact D1, disease impact D3, and total score were significantly improved in the SWL group (Table 5).
Discussion
This study examined HRQOL before and after treatment in patients with urinary stones and found that stone location significantly affected HRQOL before the surgical procedure. In contrast, SWL, ureteral stent placement, and hospital stay significantly influenced the changes in HRQOL with treatment. These results are presented for the first time using the J-WISQOL to evaluate treatment-induced changes in HRQOL.
Urinary stones significantly reduce HRQOL in patients with symptoms such as back pain [3]. The incidence is higher in the working-age population [9], and its impact on social life is greater than that of other diseases. Moreover, the impact on HRQOL is even greater if surgical treatment is required. The impact of treatment on HRQOL has been reported in several previous studies [10, 11]. Using SF-36v2, we have shown that although SWL has poorer outcomes than URSL, HRQOL is higher in all categories [12].
In this study, preoperative J-WISQOL social and disease domains were significantly affected in patients with stones in the ureter. This may be due to ureteral stones causing hydro-nephrosis and colic pain, affecting their social life. A previous study using the SF-36 also reported significantly lower HRQOL in pain and social functioning when comparing patients with stones in the ureter to healthy controls [13].
Previous studies have reported that SWL preserves HRQOL compared to other techniques [14], which is consistent with our previous findings using SF-36 [12]. In contrast, the results of present study were inconsistent with those previous findings. Herein, postoperative J-WISQOL was examined 4 weeks after treatment, and pain and complications had already improved in patients who had undergone URSL and ECIRS. Therefore, it is possible that these effects were not reflected in the HRQOL results.
Type of treatment, no ureteral stent placement after surgery, and shorter hospitalization improved the social and disease impact scores. A previous study reported that HRQOL was preserved postoperatively with no ureteral stent placement postoperatively [10]. In addition, it has been reported that ureteral stent placement may increase the incidence of urinary tract infections, the need for analgesics, and late postoperative complications [15, 16]. In the present study, most patients with URSL and ECIRS underwent postoperative ureteral stent placement; extended hospitalization may have affected this result. The median change in J-WISQOL scores before and after treatment was negative only in patients with perioperative complications. Furthermore, there was no significant difference in J-WISQOL between patients with and without complications. These results indicate that lithotripsy for urinary stones improves HRQOL in all patients.
Multivariate analysis revealed that stone-free status and postoperative ureteral stent placement affected the disease impact and vitality impact scores, respectively. A previous study also reported that, while there was no significant difference in WISQOL scores between patients with residual stones and those without, additional surgical treatment for residual stones significantly reduced WISQOL [17]. The current study suggests that stone-free status can improve the disease impact dimension of HQROL, which may be accounted for the lack of pain following the removal of stones.
In this study, the SWL group showed superior improvement in HRQOL, despite a significantly lower stone-free status, compared to the URSL group. This suggests that for patients undergoing SWL and URSL, the invasiveness of treatment, indicated by the length of hospital stay and postoperative ureteral stent placement, is more strongly related to HRQOL than being stone-free. Our previous study with SF-36 also showed that hospitalization and postoperative pain reduced HRQOL in URSL compared with SWL [12]. These results are similar to those of the present study.
In this study, lithotripsy treatment improved HRQOL. However, the factors involved in this improvement varied depending on the content of the impaired HRQOL, including the social, psychological, and physical aspects. This aspect had not been sufficiently investigated in the study using SF-36v2, and WISQOL is considered useful as a urinary stone-specific questionnaire. Based on the results of the J-WISQOL, individualized treatment plan would better contribute to improving patients’ HRQOL.
This study had several limitations. First, we evaluated the effectiveness of the J-WISQOL only in patients scheduled for urinary stone treatment. Thus, patients undergoing medical expulsive therapy were not included, which limits the generalizability of the findings to this population. Second, J-WISQOL was performed twice: preoperatively and 4 weeks after surgery. Therefore, hospitalization and long-term HRQOL have not yet been evaluated. Third, all treatments for urinary stones tend to require longer hospital stays than in the West, and day treatment is not common for SWL either. In Japan, the universal health insurance system and the Diagnosis Procedure Combination, a method of billing hospitalization costs, tend to lengthen hospital stay not only for the treatment of urinary stones but also for other diseases. This lengthening of hospital stay may have a different impact on HRQOL than in the West. Fourth, the sample size was small, the treatment modalities were not uniform, and there were differences in patient backgrounds. In particular, men accounted for 70% of the total sample, which may be inadequate for assessing HRQOL in women. Further large-scale studies are needed to examine the perioperative changes in HRQOL during lithotripsy in detail.
Conclusion
This study evaluated pre- and postoperative HRQOL changes in patients with urinary stones using the J-WISQOL for the first time. With the preoperative J-WISQOL, the presence of stones in the ureter significantly reduced HRQOL, whereas with the postoperative J-WISQOL, there was no significant reduction in HRQOL. Comparing pre- and postoperative J-WISQOL, SWL, ureteral stent placement, and hospital stay had an impact on HRQOL.
Assessment of HRQOL using WISQOL may be useful in surgical selection and patient decision-making.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
Karimi M, Brazier J (2016) Health, health-related quality of life, and quality of life: what is the difference? Pharmacoeconomics 34:645649. https://doi.org/10.1007/s40273-016-0389-9
Khan SR, Pearle MS, Robertson WG, Gambaro G, Canales BK, Doizi S, Traxer O, Tiselius HG (2016) Kidney stones. Nat Rev Dis Primers 25:16008. https://doi.org/10.1038/nrdp.2016.8
New F, Somani BK (2016) A complete world literature review of quality of life (QOL) in patients with kidney stone disease (KSD). Curr Urol Rep 17:88. https://doi.org/10.1007/s11934-016-0647-6
Penniston KL, Antonelli JA, Viprakasit DP, Averch TD, Sivalingam S, Sur RL, Pais VM Jr, Chew BH, Bird VG, Nakada SY (2017) Validation and reliability of the Wisconsin stone Quality of Life Questionnaire. J Urol 197:1280–1288. https://doi.org/10.1016/j.juro.2016.11.097
Okada T, Hamamoto S, Taguchi K, Okada S, Inoue T, Fukuta H, Chew BH, Penniston K, Okada A, Yasui T (2012) Validation of the Japanese version of the Wisconsin stone Quality of Life Questionnaire: results from SMART study group. J Endourol 35:1852–1856. https://doi.org/10.1089/end.2021.0292
Hamamoto S, Yasui T, Okada A, Takeuchi M, Taguchi K, Shibamoto Y, Iwase Y, Kawai N, Tozawa K, Kohri K (2014) Developments in the technique of endoscopic combined intrarenal surgery in the prone split-leg position. Urology 84:565–570. https://doi.org/10.1016/j.urology.2014.04.020
Inoue T, Kinoshita H, Okada S, Hamamoto S, Taguchi M, Murota T, Matsuda T; SMART Study Group (2016) Wideband Doppler ultrasound-guided mini-endoscopic combined intrarenal surgery as an effective and safe procedure for management of large renal stones: a preliminary report. Urology 95:60–66. https://doi.org/10.1016/j.urology.2016.05.038
Kanda Y (2013) Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant 48:452–458. https://doi.org/10.1038/bmt.2012.244
Sakamoto S, Miyazawa K, Yasui T, Iguchi T, Fujita M, Nishimatsu H, Masaki T, Hasegawa T, Hibi H, Arakawa T, Ando R, Kato Y, Ishito N, Yamaguchi S, Takazawa R, Tsujihata M, Taguchi M, Akakura K, Hata A, Ichikawa T (2019) Chronological changes in epidemiological characteristics of lower urinary tract urolithiasis in Japan. Int J Urol 26:96–101. https://doi.org/10.1111/iju.13817
Sonmez G, Demir F, Keske M, Karadag MA, Demirtas A (2021) Comparison of the effects of four treatment techniques commonly used in ureteral stone treatment on patients’ daily physical functioning: an observational randomized-controlled study. J Endourol 35:8–13. https://doi.org/10.1089/end.2020.0659
de Sousa MN, Pereira JP, Mota P, Carvalho-Dias E, Torres JN, Lima E (2019) Percutaneous nephrostomy vs ureteral stent for hydronephrosis secondary to ureteric calculi: impact on spontaneous stone passage and health-related quality of life-a prospective study. Urolithiasis 47:567–573. https://doi.org/10.1007/s00240-018-1078-2
Hamamoto S, Unno R, Taguchi K, Naiki T, Ando R, Okada A, Inoue T, Okada S, AbdelRazek M, Kohri K, Yasui T; SMART Study Group (2018) Determinants of health-related quality of life for patients after urinary lithotripsy: ureteroscopic vs. shock wave lithotripsy. Urolithiasis 46:203–210. https://doi.org/10.1007/s00240-017-0972-3
Rabah DM, Alomar M, Binsaleh S, Arafa MA (2011) Health related quality of life in ureteral stone patients: post-ureterolithiasis. Urol Res 39:385–388. https://doi.org/10.1007/s00240-011-0375-9
Constanti M, Calvert RC, Thomas K, Dickinson A, Carlisle S (2020) Cost analysis of ureteroscopy (URS) vs extracorporeal shockwave lithotripsy (ESWL) in the management of ureteric stones <10 mm in adults: a UK perspective. BJU Int 125:457–466. https://doi.org/10.1111/bju.14938
Chen YT, Chen J, Wong WY, Yang SS, Hsieh CH, Wang CC (2002) Is ureteral stenting necessary after uncomplicated ureteroscopic lithotripsy? A prospective, randomized controlled trial. J Urol 167:1977–1980. https://doi.org/10.1016/S0022-5347(05)65066-5
Pengfei S, Yutao L, Jie Y, Wuran W, Yi D, Hao Z, Jia W (2011) The results of ureteral stenting after ureteroscopic lithotripsy for ureteral calculi: a systematic review and meta-analysis. J Urol 186:1904–1909. https://doi.org/10.1016/j.juro.2011.06.066
Streeper NM, Galida M, Boltz S, Li S, Nakada SY, Raffin EP, Brown DR, Pais VM, Chan JYH, Scotland KB, Chew BH, Penniston KL (2021) Is stone-free status after surgical intervention for kidney stones associated with better health-related quality of life? A multicenter study from the North American stone quality of life consortium. Urology 148:77–82. https://doi.org/10.1016/j.urology.2020.09.058
Acknowledgements
We would like to thank Editage (www.editage.com) for the English language editing.
Funding
No funding was received.
Author information
Authors and Affiliations
Consortia
Contributions
T.O. and S.H. conducted the literature search and wrote the manuscript. K.T., S.O., and T.I. obtained informed consent and collected the WISQOL data. R.A., A.O., and T.Y. revised the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Okada, T., Hamamoto, S., Taguchi, K. et al. Quality of life after urinary stone surgery based on Japanese Wisconsin Stone Quality of Life questionnaire: multicenter analysis from SMART study group. Urolithiasis 51, 113 (2023). https://doi.org/10.1007/s00240-023-01486-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00240-023-01486-8