Abstract
The objective of this study was to compare the results of shock wave lithotripsy (SWL) between patients treated with optical coupling control (OCC) and those treated with “blind” coupling during SWL to treat renal stones. Enrolled in the study were patients with urinary stones who underwent SWL between January 2014 and February 2015. The lithotripter used in the study was an electromagnetic Dornier Compact Delta II UIMS. The closed envelope method was used to randomize the enroled patients to OCC (Group A) or “Blind” coupling group (Group B). The stone-free rates (SFRs) were determined using KUB film with or without ultrasonography after 3 months. Treatment failure was defined as radiologically confirmed persistence of the stone with no fragmentation after second SWL sessions. Complications during the intraoperative or post-operative periods were recorded. A total of 336 patients satisfied the inclusion criteria for the study, of which 169 patients were treated in the Group A and 167 in the Group B. There was no significant difference in patient and stone characteristics between the two groups (Table 1). The locations of treated stones are shown in Table 2. The treatment results were stratified by stone location in Table 3, significant differences existed in all treatment results between the two groups (P < 0.05). The overall stone-free rates after 3 months were 78.2 % for kidney stones and 81.7 % for ureteral stones in patients from Group A. The corresponding SFRs for patients in Group B were 62.8 and 67.9 % for stones in the kidneys and ureters, respectively. There were statistical differences in these results between the two groups (P < 0.05). The lithotripter with OCC had excellent shock wave transmission properties with the least possible loss of energy; it can lead to the optimization of SWL treatment outcome and reduce the incidence of SW-induced adverse effects. We are confident that the OCC used in this study should be a standard feature in future lithotripters.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In early lithotripters such as the Dornier HM3, the patient was immersed in a water tub, providing an ideal medium for SW propagation. Modern lithotripters on the other hand are dry-head devices in which the cushion of the treatment head must be coupled, usually with a gel or oil, to the skin of the patient. Unfortunately, air can get trapped at the coupling interface, and this interferes with SW transmission to the patient [1, 2]. The quality of acoustic coupling in shock wave lithotripsy (SWL) is often overlooked and may be one of the most important factors in energy transfer, and hence in the quality of stone fragmentation [3–7]. Air bubbles in the coupling area have a deleterious effect on the propagation of the SW and consequently on the disintegration capacity. Various in vitro studies have been done on the effect of air pockets in the coupling surface on disintegration capability [7–12]. Pishchalnikov et al. [9] found that only 2 % coverage by air pockets decreased stone breakage by 20–40 %.
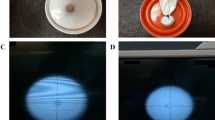
Although bubble-free coupling is essential, the coupling surface cannot be visually monitored with most lithotripters. Dornier devices with latest feature coupling—opticouple control detects the presence of imperfect coupling. Opticouple is an imaging technology that enables healthcare professionals to optically view the patient contact interface from within the therapy head. A video camera and a LED light were installed in the therapy head of Dornier newer lithotripter. It can check for air bubbles in the coupling area between the water cushion and the patient (Fig. 1).
In this study, we compared the treatment results using this optical coupling control (OCC) to the treatment results with “blind” coupling during SWL to treat renal stones. Our goal was to determine whether a coupling monitor could improve SWL.
Patients and methods
From January 2014 to February 2015, eligible patients with upper urinary tract stones referred to our institute were considered for this study. The upper urinary tract stones were initially diagnosed by abdominal ultrasound and plain abdominal X-ray for kidney, ureter and bladder (KUB). An unenhanced CT scan is performed when necessary. Stone size was recorded as the maximum diameter measured on a plain abdominal film. All procedures were performed by the same urologist.
The lithotripter used in the study was an electromagnetic Dornier Compact Delta II UIMS (Dornier Medical Systems, Germany). The calculi were fragmented under fluoroscopic or ultrasound guidance. In each treatment session, shock waves were delivered at a fixed pulse repetition frequency of 70 SW/min; shock wave power was increased gradually to reach 100 %. The closed envelope method was used to randomize the enroled patients to optical coupling control (OCC; Group A) or “blind” coupling (Group B).
To optically check for air bubbles in the coupling interface between the coupled water cushion and the patient, a video camera and light-emitting diode were installed in the therapy head of lithotripter (Fig. 1). For all patients we strictly adhered to guidelines for optimal coupling [4, 5]. A low viscosity ultrasound gel (Sun Ultrasound Transmission Gel, JianQu laboratories Inc., China) was scooped with a large spoon from a wide mouthed container and deposited in a generous amount in the center of the inflated water cushion. Coupling was found to be best when applying a large mound of bubble free gel from a large container. Poor results were obtained when applying the gel from a squeeze bottle [8]. The patient was then gently lowered onto the inflated cushion, thus spreading the gel radially and minimizing air entrapment [11]. In the OCC series, the air pockets in the coupling area could then be removed under visual control of the video camera. This was performed by gently swiping a hand between the patient and the inflated water cushion (Fig. 1). This gentle swiping movement was repeated until all air bubbles and/or folds in the water cushion membrane had disappeared. After targeting off the stone, a hand is gently swiped between the inflated water cushion and the patient to remove all the air pockets trapped in the coupling zone.
The preoperative evaluation included medical history, physical examination, laboratory investigations (urine analysis, urine culture and/or sensitivity, complete blood count, coagulation profile, blood urea nitrogen and serum creatinine levels) and radiologic investigations. Patients with a known urinary tract infection received specific antimicrobic culture before SWL until the urine culture turned to negative.
There was no statistically significant difference between the groups in the time from diagnosis to treatment. The stone-free rates (SFRs); defined as the complete absence of stone fragments were determined using KUB film with or without ultrasonography in 3 months. Treatment failure was defined as radiologically confirmed persistence of the stone with no fragmentation after second SWL sessions. Complications related to SWL during the intraoperative or post operated periods, were recorded.
Data were processed using SPSS 15 for Windows. The results are presented as mean ± standard deviation. All the parameters were analyzed statistically using the unpaired Student’s t test and χ2 test. A P value <0.05 was considered statistically significant.
Results
A total of 336 patients satisfied the inclusion criteria for the study, of which 169 patients were treated in the Group A and 167 in the Group B. There were no significant differences in stone characteristics between the two groups (Table 1). The stone locations in the treated patients are shown in Table 2. The treatment results were stratified by stone location in Tables 3, All treatment results differed significantly (P < 0.05) between the two groups. The overall SFRs after 3 months were 78.2 % for kidney stones and 81.7 % for ureteral stones in patients from Group A. The corresponding stone-free rates for patients in Group B were 62.8 and 67.9 % for stones in the kidneys and ureters, respectively (P < 0.05).
The number of shock waves ranged from 800 to 3000, pulse rate was 70 SW/min and the energy applied was between levels 1 and 4. Treatment time varied from 8 to 45 min (Table 4).
Nine clinically significant subcapsular hematomas were detected in Group B after lithotripsy. All nine patients were managed conservatively without blood transfusion. No clinically significant hematomas were detected in the Group B.
Discussion
Numerous studies have documented that second and third generation lithotripters may not be as effective as the first-generation Dornier HM3 [7–12]. Several of these reports attribute this discrepancy to the fact that the original Dornier HM3 had excellent coupling properties with the least possible loss of shock wave energy, as patients were lying in a water bath, providing an excellent medium for the transmission of acoustic energy. The HM4 Dornier machine (the first so called anesthesia free and dry shock head machine) had a camera inside the cushion to identify the air bubbles inside the cushion with a blade to allow removing the air bubbles, but there was a significant difference between the results of HM3 and HM4. Undoubtedly, the focal point and other factors played important roles.
With dry shock wave delivery, accomplished with the therapy head not immersed in water, the intention was to get a ‘cleaner’ SWL treatment. Patients did not get wet and had more privacy. Moreover, the equipment would be more patient and user friendly. However, greater than 99 % of a shock wave is reflected by an air pocket [3–9]. This necessitates the use of a coupling agent to eliminate air between the head of the lithotripter and the patient, ultimately providing a media have been utilized for shock wave transmission to the targeted calculus [13, 14]. A wide variety of coupling mediums were utilized for SWL, including creams, castor oil, petroleum jelly, ultrasonography gel, and other water-soluble lubricating jellies.
Despite advances in coupling properties, the results are variable. The SFRs of the reference machine, the Dornier HM3, have never been reached again by the other newer machine.
Everyone knows that coupling is important and different methods have been tried. McClain [15] demonstrated that the process of coupling produced air pockets ranging from 1.5 to 19 % of the coupling surface area, causing a 20 % mean reduction in shock wave amplitude. In fact, air pockets covering 2 % of the coupling area diminished stone fragmentation by 20–40 %. Jain and Shah [1] utilized high-resolution photographs to show that decreased bubble contents of gel significantly increased depth and volume of stone craters in vitro (P < 001). Neucks and associates [16] used digital imaging for the detection of coupling defects in an effort to determine the best methods for gel application. They found that the best technique was to dispense a large volume of gel directly from a stock jug onto the lithotripter water cushion, as the gel was then allowed to spread during stepwise inflation of the lithotripter water cushion. The same group has found that the coupling interactions at the central portion of the water cushion are most important [17].
Before introduction of optical control, multiple bubbles, incomplete coupling and cushion wrinkling could not be observed (Fig. 2). The fact that the coupling interface remains invisible still posed a practical problem in locating and removing possible air pockets. A surveillance mechanism could aid in the discovery and subsequent elimination of air pockets, thereby optimizing the coupling during SWL treatment. Bohris and associates [2] demonstrated the potential benefits of this strategy. They used a video camera integrated into a lithotripter to detect air pockets in coupling gels during SWL. Air ratios in the coupling area were measured and lithotripter fragmentation was assessed at varying air ratios. Their results showed that the mean number of shock waves needed for effective stone fragmentation increases with greater air ratios.
The new feature OCC was incorporated in Dornier lithotripters with the aim of optimizing treatment results. Tailly and associates [3] have done to check for air bubbles in the coupling interface, a video camera was installed in the therapy head of Dornier Gemini lithotripter: all air bubbles observed in the coupling zone could then be removed under visual control. They evaluated the effect of this optically controlled coupling (OCC) on treatment results and compared these to the results obtained in a ‘‘blind’’ coupling mode. Their work showed that the optically controlled removal of air bubbles from the coupling area reduced the required number of shock waves with 25.4 % for renal stones and 25.5 % for ureteral stones. Energy level was reduced by 23.1 % for renal stones and by 22.5 % for ureteral stones. For renal stones, total applied energy was thus reduced by 42.9 %. So they consider this an important step toward better and safer shock wave lithotripsy, and would therefore, advocate the standard incorporation of an OCC system in all new lithotripters. Their work is the first clinical study to evaluate the effects of OCC on actual in vivo treatment results. Although they already paid careful attention to optimal coupling, they were astonished by the video camera visualization of the number and location of air pockets still present in the coupling zone.
The lithotripter we used in the study was an electromagnetic Dornier Compact Delta II UIMS. The lithotripter with an integrated video camera for coupling monitoring (Fig. 1). Camera view showing trapped air bubbles. Shock waves are disrupted by the increased presence of air bubbles and affect the efficacy of ESWL treatments requiring an increase in the number of shock wave pulses per treatment. Video monitoring of the coupling area with optically controlled removal of all air bubbles significantly reduced the required number of SWL and the total treatment time.
In our study, the overall SFRs after 3 months were 78.2 % for stones in the kidney and 81.7 % for stones in the ureter in patients from Group A. The corresponding SFRs for patients in Group B were 62.8 and 67.9 % for stones in the kidneys and ureters, respectively (P < 0.05). A camera is ideal for this optimizing efficiency in SWL coupling, since it allows the operator to monitor coupling and improve it as needed. Operators can locate possible regions of inadequate patient coupling throughout SWL treatments and improve outcomes. Inline ultrasound can be used in a similar way [18, 19]. However, a camera is better suited since it presents the whole coupling area at a glance. With inline ultrasound, the transducer must be rotated for a complete scan. Therefore, evaluating the magnitude of air inclusions and removing the disturbance by manual wiping becomes more difficult.
Conclusion
The lithotripter with OCC had excellent shock wave transmission properties with the least possible loss of energy; it can lead to the optimization of SWL treatment outcome and reduce the incidence of SW-induced adverse effects. We are confident that the OCC used in this study should be a standard feature in future lithotripters.
References
Jain A, Shah TK (2007) Effect of air bubbles in the coupling medium on efficacy of extracorporeal shock wave lithotripsy. Eur Urol 51:1680–1687
Bohris C, Roosen A, Dickmann M et al (2012) Monitoring the coupling of the lithotripter therapy head with skin during routine shock wave lithotripsy with a surveillance camera. J Urol 187(1):157–163
Tailly GG, Tailly-Cusse MM (2014) Optical coupling control: an important step toward better shock wave lithotripsy. J Endourol 28:1368–1373
Chaussy C, Tailly GG, Forssmann B et al (2013) Extracorporeal shockwave lithotripsy in a nutshell. In: Chaussy C, Tailly G eds. Booklet presented to European Association of Urology.
Tailly GG (2013) Optical coupling control in SWL: first clinical experience. Poster MP07–13 presented at World Congress of Endourology; October 22–26, New Orleans
Lingeman JE, McAteer JA, Gnessin E, Evan AP (2009) Shock wave lithotripsy: advances in technology and technique. Nature Rev Urol 6:660–670
Rassweiler JJ, Knoll T, Kohrmann KU, McAteer JA et al (2011) Shock wave technology and application: an update. Eur Urol 59:784–796
Bergsdorf T, Chaussy C, Thueroff S (2010) Coupling gel viscosity: a relevant factor for efficient shock wave coupling in SWL. J Urol 183(suppl):e704
Pishchalnikov YA, Neucks JS, VonDerHaar RJ et al (2006) Air pockets trapped during routine coupling in dry head lithotripsy can significantly decrease the delivery of shock wave energy. J Urol 176:2706–2710
Bergsdorf T, Chaussy C, Thueroff S (2008) Energy coupling in extracorporeal shock wave lithotripsy—the impact of coupling quality on disintegration efficacy. J Endourol 22:A161
Bergsdorf T, Chaussy C, Thueroff S (2009) The significance of accurate shock wave coupling in extracorporeal shock wave lithotripsy. J Endourol 23:1042
Bohris C (2010) Quality of coupling in ESWL significantly affects the disintegration capacity—how to achieve good coupling with ultra-sound gel. In: Chaussy C, Haupt G, Jocham D, Köhrmann KU (eds) Therapeutic energy applications in urology II: standards and recent developments. Thieme; Stuttgart, Germany, pp 61–64
Chaussy CG, Fuchs GJ (1989) Current state and future developments of noninvasive treatment of human urinary stones with extracorporeal shock wave lithotripsy. J Urol 141(3 Pt 2):782–789
Clayman RV, McClennan BL, Garvin TJ et al (1989) Lithostar: an electromagnetic acoustic shock wave unit for extracorporeal lithotripsy. In: Lingeman JE (ed) Shock wave lithotripsy 2: urinary and biliary lithotripsy. Springer, Berlin, New York, NY, pp 403–409
McClain PD, Lange JN, Assimos DG (2013) Optimizing shock wave lithotripsy: a comprehensive review. Rev Urol 15(2):49–60
Neucks JS, Pishchalnikov YA, Zancanaro AJ et al (2008) Improved acoustic coupling for shock wave lithotripsy. Urol Res 36:61–66
Li G, Williams JC Jr, Pishchalnikov YA, McAteer JA (2012) Size and location of defects at the coupling interface affect lithotripter performance. BJU Int 110:871–877
Bohris C, Jensen H, Bayer T et al (2006) A new integrated ultrasound system for shockwave lithotripsy. J Endourol 20:863
Neucks JS, Pishchalnikov YA, Zancanaro AJ et al (2008) Improved acoustic coupling for shock wave lithotripsy. Res Urol 36(1):61
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Jian Lin Lv declares that he has no conflict of interest. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration, and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Lv, J.L. A new optical coupling control technique and application in SWL. Urolithiasis 44, 539–544 (2016). https://doi.org/10.1007/s00240-016-0874-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00240-016-0874-9