Abstract
Various studies have suggested that potassium depletion leads to acidosis and hypocitraturia. In Northeastern Thailand, for example, mild hypokalemia and mild hyperoxaluria are observed in most stone formers. However, there are limited reports about the direct link between potassium depletion and the formation of urinary stones, most of which are calcium oxalate stones. Therefore, we studied the direct effect of potassium depletion on the risk factors for calcium oxalate stone formation. Seventy-two rats were fed a control diet or a potassium-deficient diet for 1, 2, or 3 weeks (n = 12 per group). Twenty-four-hour urine collection was done for the measurement of potassium, calcium, oxalate, glycolate, citrate, phosphorus, and magnesium. Lactate dehydrogenase activity was also measured in order to assess renal tubular damage, and kidneys were harvested for histological examination. Furthermore, urinary supersaturation of calcium oxalate was calculated. With potassium depletion, the urinary concentrations of potassium, citrate, magnesium, and phosphorus decreased rapidly. There was no detectable renal damage, renal calcium deposition, and no significant increase of urinary oxalate or calcium. However, the urinary supersaturation index of calcium oxalate increased significantly in rats with potassium depletion. These findings indicate that potassium deficiency may increase the risk of stone formation through enhanced supersaturation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Urolithiasis is a very common urologic disease that affects 10–12% of the population worldwide and has a recurrence rate of 50% after 10 years and 75% after 20 years in persons who do not receive appropriate treatment [1]. The prevalence of nephrolithiasis has been increasing steadily in Thailand [2]. Approximately 80% of nephrolithiasis patients have calcium stones and the majority of these stones are primarily composed of calcium oxalate, either pure or mixed with other components [3, 4].
Urolithiasis has a high prevalence in Northeastern (NE) Thailand [2]. Bovornpadungkitti et al. [5] showed that the stone formers had a higher skeletal muscle content of potassium and magnesium when compared with non-stone formers. Studies performed in rats and humans have not produced consistent findings as to whether potassium deficiency causes renal tubulo-interstitial damage [6, 7]. Furthermore, vegetables with high oxalate content are generally available in that area. Thus, mild hyperoxaluria and oxalate stones are frequently found in NE Thai stone formers. Tosukhowong et al. [8] recently investigated the chemical composition of urinary stones obtained from patients in different areas of Thailand and found that calcium oxalate was the major component of their renal calculi, as is the case worldwide.
Urinary oxalate and calcium level are the key determinants of calcium oxalate stone formation, with many studies suggesting that hyperoxaluria is more important than hypercalciuria [9]. The etiologies of these stones involve multiple factors, including genetic factors, environmental factors, and dietary habits [10]. Studies of potassium deficiency have suggested that it may cause nephrolithiasis in addition to sudden unexplained death and muscle wasting [22, 23]. However, few studies have assessed the effect of potassium depletion on urolithiasis. Accordingly, we conducted the present study to determine the direct effect of potassium depletion on known risk factors for urinary stone formation in rats.
Materials and methods
Control and potassium-deficient diets
Laboratory diets were purchased from Nihon Clea Co., Ltd (Tokyo, Japan). According to the company’s information, the composition of the control diet and the potassium-deficient diet was similar except for the content of potassium (0.95 and 0% potassium content in the control and potassium-deficient diets, respectively). No metal substitution was made.
Study protocol
The study protocol was approved by the Ethics Committee of the University of the Ryukyus. Seventy-two male Wistar rats weighing 180–200 g were acclimatized for one week at the university animal center on the standard diet. The rats were randomly divided into six groups (n = 12 per group), after which the three control groups were fed the control diet for 1, 2, or 3 weeks, while the three potassium-depleted groups were fed the potassium-deficient diet for 1, 2, or 3 weeks. Water was provided ad libitum. A 24-h urine specimen (with 20% hibitane (chlorhexidine gluconate) as the preservative) was collected on the day before the experiment and 1, 2, or 3 weeks after starting the experiment. The animals were then anaesthetized and midline laparotomy was done. Next, blood samples were collected for the measurement of serum creatinine (SRL, Tokyo, Japan). The kidneys were removed, immersed immediately in 20% formalin solution, and later embedded with paraffin. Histological evaluation was done after staining with hematoxylin and eosin (SRL, Tokyo, Japan) or with the von Kossa technique for investigation of calcium deposits in the kidneys. Tissue samples were observed under light microscopy and polarized light microscopy.
Urine pH and volume were measured by standard methods and samples were stored at −80°C until further investigation. The detailed method of determining urinary oxalate, citrate, and glycolate were mentioned elsewhere [11]. Briefly, urinary samples were thawed and acidified at pH < 2. The acidified samples were filtered and diluted accordingly for oxalate determination, while the non-acidified urine samples were filtered and diluted accordingly for citrate and glycolate determinations. Urinary oxalate was determined by high performance capillary electrophoresis (HPCE, Hewlett-Packard, Germany) using a pH 7.7 HPCE buffer solution (Fluka Chemika, Switzerland), while urinary glycolate and citrate were measured by using a pH 5.6 HPCE organic buffer (Agilent Technologies, USA). Urinary levels of calcium, potassium, phosphorus, and magnesium were determined by inductively coupled plasma spectrophotometry (ICPS-7000, Shimadzu, Kyoto, Japan). Urinary creatinine was determined with Jaffe’s reaction and urinary lactate dehydrogenase activity was measured by an enzymatic method (SRL, Tokyo, Japan).
Analytical grade standards for oxalate, citrate, glycolate, calcium, magnesium, and potassium were obtained from Wako Pure Chemicals (Osaka, Japan). The standard for measuring phosphorus by ICPS was obtained from Kanto Chemical (Tokyo, Japan). Purified de-ionized water was prepared with a Milli Q system from Millipore (USA).
Calculations
In order to determine the risk of calcium oxalate stone formation, the relative supersaturation index for calcium oxalate (SS(CaOx)) was calculated with Finlayson’s EQUIL 2 computer program [12]. Creatinine clearance was calculated as the product of urine volume and urinary creatinine divided by the serum creatinine concentration and time.
Statistical methods
Statistical analysis was performed with the SPSS 12.0 program (Chicago, IL, USA). The Mann–Whitney U test was employed to make comparisons among experimental groups. Multiple regression analysis was done to assess risk factors, including the urine volume, urine pH, and urine levels of citrate, calcium, magnesium, potassium, phosphorus, creatinine, LDH, glycolate, and oxalate. Differences were considered significant at P < 0.05.
Results
The body weight of both groups of rats increased steadily over time. However, the weight gain of potassium-depleted rats was significantly less than that of control rats throughout the experiment (Fig. 1a). The creatinine clearance of the potassium-depleted groups was significantly lower than that of the control groups. There was also a significant difference of creatinine clearance between the week 1 and week 3 potassium-depleted groups (Fig. 1b).
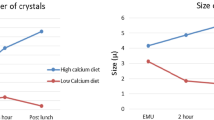
The most striking change observed was a rapid decrease of urinary citrate in the potassium-depleted groups by between 2 and 27-folds. Decreases of urinary potassium, and phosphorus were also seen in the potassium-depleted group, while magnesium decreased in potassium-depleted group and the first week of control group (Table 1). A significant decrease of urinary pH was observed in the week 2 and week 3 potassium-depleted groups compared with their respective baseline values, as well as in the week 3 potassium-depleted rats compared with the controls (6.52 ± 0.14 vs. 6.22 ± 0.35 (P < 0.01) for control and potassium-depleted rats, respectively). SS(CaOx) showed a significant increase in the potassium-depleted groups compared with control rats (Fig. 2). In comparison with baseline values, a significant increase of SS(CaOx) was also observed in potassium-depleted rats over time (Fig. 2b). In contrast, there was no significant change of SS(CaOx) in the control group (Fig. 2a).
There were no significant differences of renal histology among all groups (data not shown). In addition, no calcium or calcium oxalate deposits were observed in any of the von Kossa-stained specimens (data not shown). Consistent with the histological results, there was no significant increase of LDH activity in any of the groups (Table 1).
Discussion
Depletion of potassium causes disorders of the neuromuscular and cardiovascular systems, as well as the derangement of various tissues and malfunction of organs. A recent study by Youngjermchan et al. [13] reported that hypocitraturia, defined as urinary citrate excretion less than 250 mg/day (100%) and hypokaliuria, defined as urinary potassium excretion lower than 30 mEq/day (79.4%) were greatly higher among renal stone formers in central Thailand than healthy subjects (normal value of urinary potassium excretion is 40–60 mEq/day). In NE Thailand where urinary stones are endemic, potassium deficiency is considered to be one of the five major abnormalities responsible for nephrolithiasis. A previous study suggested that the major causes of potassium deficiency in NE Thailand were low dietary intake and excessive loss due to sweating [14]. Many authors have investigated the effect of potassium deficiency on various diseases, including sudden death [6, 7, 15, 16]. However, there have been few investigations into the effect of potassium depletion on urolithiasis. To the best of our knowledge, the present study is the first time to demonstrate an effect of potassium deficiency on nephrolithiasis and to show that potassium depletion significantly increases the risk of calcium oxalate stone formation over time.
There is growing evidence that acidic urine or hypokalemia is problematic in patients with urinary stones [17]. Generally, potassium depletion results in rapid changes of the body’s acid/base balance. After chronic acidosis and intracellular acidosis have developed, urinary citrate resorption is increased via Na/citrate co-transport. This causes hypocitraturia, which affects 18–40% of renal stone formers [18]. Urinary citrate is one of the most important inhibitors of nephrolithiasis. Citrate forms soluble complexes with calcium as well as inhibiting other steps of stone formation, including crystal growth and agglomeration [19]. Recent studies by Domrongkitchaiporn et al. [20] and Stitchantrakul et al. [21] showed the positive correlation between urinary citrate and urinary potassium in idiopathic calcium stone formers and recurrent stone formers in Thailand. In the present study, we found that urinary citrate was decreased significantly after one week of potassium depletion, although the urinary pH (luminal pH) remained normal. These results may demonstrate renal sensitivity in detecting intracellular changes of the acid/base balance. Moreover, potassium depletion may alter the citrate clearance directly through an unknown mechanism in citrate transport. Therefore, marked resorption of citrate will occur rapidly in persons with potassium depletion. The study performed by Levi et al. [15] in Spargue–Dawley rats also showed that urinary potassium and citrate were decreased significantly while urine volume was increased after 1 week of potassium depletion.
We found that the body weight and creatinine clearance of the potassium-depleted groups were significantly lower compared with those of the control groups. Moreover, we observed a lesser body mass gain in the potassium-depleted groups. Since creatinine reflects the body’s skeletal muscle mass, the lower body weights and creatinine clearance may have been caused by the loss of skeletal muscle. The study by Thongboonkerd et al. [22] showed that the prolonged potassium depletion caused alterations in various muscle proteins in mice which related with several metabolic mechanisms of bioenergetics. Moreover, the study of vastus lateralis muscle of potassium-depleted cadaveric subjects showed several altered proteins responsible not only for the bioenergetics but also for acid–base regulation, oxidative stress response, and muscle contractility [23]. Napradit et al. [16] reported that polyuria occurred in potassium-depleted rats, and they suggested that this might be caused by polydipsia or by defective renal concentration of urine. Lack of a significant difference in urine volume may be due to the different diets used in this study (K = 0% in the potassium-depleted diet) comparing to the diets used in the other studies.
Calcium phosphate precipitate is one of frequently associated events with calcium oxalate stone formation [24]. Previous study reported a trend of higher excretion of calcium and phosphate in calcium oxalate and magnesium ammonium phosphate stone formers in Thailand [13]. Moreover, our recent study showed that, in Thailand, calcium oxalate mixed with calcium phosphate stone (47.66%) was more prevalent than pure calcium oxalate stone (21.09%) [8]. Significant decrease (two- to three-folds) of phosphate was observed throughout this study. Our finding is similar to the previous findings of decreased urinary phosphate excretion in renal stone formers in the NE Thailand [14]. The latest study by Breusegen et al. [25] reported that dietary potassium deficiency causes phosphaturia in rats through the decrease in BBM abundance of the sodium/phosphate co-transporters. Further studies are required to confirm it.
Calculation of the supersaturation index for calcium oxalate showed that there was a linear trend for an increased risk of stone formation after potassium depletion (y = 0.6335x + 0.2744, r = 0.9996, P < 0.01). SS(CaOx) increased over time due to the severity of potassium depletion as well as the changes in the urinary levels of inhibitors and promotors (Fig. 2). Although various factors influence the risk of forming stones, the prime factors for potassium-depleted rats observed in this study were low citrate, low pH, and low potassium. There is no doubt that high calcium and high oxalate are considered to be core factors for calcium oxalate stone formation, however, we found no significant changes of either urinary oxalate or calcium. This result suggested that there might not be any direct effect of potassium deficiency on calcium or oxalate levels. A study by Tosukhowong et al. [14] also found that non-stone formers with hypokalemia and hypokaliuria might have a high risk of stone formation when challenged with high oxalate (or oxalate precursors) and a high calcium diet. Due to the lack of a significant change of urinary pH during the first week of potassium depletion, we hypothesized that the initial increase of SS(CaOx) may be secondary to the decrease of urinary citrate.
Many studies have indicated that potassium depletion causes renal tubular injury [7, 26, 27]. However, we found no significant histological abnormalities, although possible minor changes may not have been detected. Urinary LDH activity reflects the renal cell damage and its level also, showed no significant changes. This may have been due to the time constraints of the present study.
We acknowledge the limitations in this study. The study was conducted only in male Wistar rats and for a short duration. The results, therefore, are limited to the urine biochemical changes only. The effect of potassium depletion on renal tissue may require longer duration. Moreover, as demonstrated in this study that potassium depletion increases the SS(CaOx), a long-term study with addition of hyperoxaluric groups may provide conclusive evidence regarding the effect of potassium deletion on kidney stone formation.
In conclusion, the present study was the first to demonstrate that potassium depletion causes an increase in SS(CaOx) which may, consequently, increase the risk of urinary calcium oxalate stone formation over time by reducing the urinary pH, citrate, magnesium, and potassium.
References
Sutherland JW, Parks JH, Coe FL et al (1985) Recurrence after a single renal stone in a community practice. Miner Electrolyte Metab 11(4):267–269
Yanagawa M, Kawamura J, Onishi T et al (1997) Incidence of urolithiasis in northeast Thailand. Int J Urol 4(6):537–540
Coe FL, Evan A, Worcester E et al (2005) Kidney stone disease. J Clin Invest 115(10):2598–2608
Hossain RZ, Ogawa Y, Hokama S et al (2003) Urolithiasis in Okinawa, Japan: a relatively high prevalence of uric acid stones. Int J Urol 10(8):411–415
Bovornpadungkitti S, Sriboonlue P, Tavichakorntrakul R et al (2000) Potassium, sodium and magnesium contents in skeletal muscle of renal stone-formers: a study in an area of low potassium intake. J Med Assoc Thai 83(7):756–763
Lelamali K, Khunkitti W, Yenrudi S et al (2003) Potassium depletion in a healthy north-eastern Thai population: no association with tubulo-interstitial injury. Nephrology 8:28–32
Ray EP, Suga SI, Liu XH et al (2001) Chronic potassium depletion induces renal injury, salt sensitivity, and hypertension in young rats. Kidney Int 59:1850–1858
Tosukhowong P, Boonla C, Ratchanon S et al (2007) Crystalline composition and etiologic factors of kidney stone in Thailand. Asian Biomed 1(1):89–97
Robertson WG (1986) Pathophysiology of stone formation. Urol Int 41(5):329–333
López M, Hoppe B (2008) History, epidemiology, and regional diversities of urolithiasis. Pediatr Nephrol. doi:10.10071/s00467-008-0960-5
Morozumi M, Hossain RZ, Yamakawa K et al (2006) Gastrointestinal oxalic acid absorption in calcium-treated rats. Urol Res 34(3):168–172
Milosević D, Batinić D, Blau N et al (1998) Determination of urine saturation with computer program EQUIL 2 as a method for estimation of the risk of urolithiasis. J Chem Inf Comput Sci 38(4):646–650
Youngjermchan P, Pumpaisanchai S, Ratchanon S et al (2006) Hypocitraturia and hypokaliuria: major metabolic risk factors for kidney stone disease. Chula Med J 50(9):605–621
Tosukhowong P, Sriboonlue P, Tungsanga K et al (2001) Potassium status of Northeast Thai constructors in three different geographic locations. J Med Assoc Thai 84(Suppl 1):S163–S172
Levi M, McDonald LA, Preisig PA et al (1991) Chronic K depletion stimulates rat renal brush-border membrane Na-citrate cotransproter. Am J Physiol Renal Physiol 261:767–773
Napradit P, Pholpramool C, Jariyawat S et al (1995) Extrarenal potassium homeostasis after chronic potassium deficiency in rats. In: Japanese and Thai collaborative study group (ed) Lai Tai, sudden unexplained death syndrome, Tokyo, pp 71–104
Halperin ML, Dhadli SC, Kamel KS (2006) Physiology of acid–base balance: links with kidney stone prevention. Semin Nephrol 26:441–446
Pak CYC (1994) Citrate and renal calculi; new insights and future directions. Am J Kidney Dis 17:420–425
Hamm LL (1990) Renal handling of citrate. Kidney Int 38(4):728–735
Domrongkitchaiporn S, Stitchantrakul W, Kochakarn W (2006) Causes of hypocitraturia in recurrent calcium stone formers: focusing on urinary potassium excretion. Am J Kidney Dis 48:546–554
Stitchantrakul W, Kochakarn W, Ruangraksa C et al (2007) Urinary risk factors for recurrent calcium stone formation in Thai stone formers. J Med Assoc Thai 90(4):688–698
Thongboonkerd V, Kanlaya R, Sinchaikul S et al (2006) Proteomic identification of altered proteins in skeletal muscle during chronic potassium depletion: implications for hypokalemic myopathy. J Proteome Res 5:3326–3335
Tavichakorntrakool R, Sriboonlue P, Prasongwattana V et al (2009) Metabolic enzymes, antioxidants, and cytoskeletal proteins are significantly altered in vastus lateralis muscle of K-depleted cadaveric subjects. J Proteome Res 8:2586–2593
Kahn SR (1998) Importance of calcium phosphates in the development of calcium urolithiasis. In: Zahid Amjad (ed) Calcium phosphates in biological and industrial systems, USA, pp 253–275
Breusegerm S, Takahashi H, Giral-Arnal H et al (2009) Differential regulation of the renal sodium/phosphate co-transporters NaPi-IIa, NaPi-IIC and PiT-2 in dietary potassium deficiency. Am J Physiol Renal Physiol. doi:10.1152/ajprenal.90765.2008
Suga SI, Phillips MI, Ray PE et al (2001) Hypokalemia induces renal injury and alterations in vasoactive mediators that favor salt sensitivity. Am J Physiol Renal Physiol 281:F620–F629
Tolins JP, Hostetter MK, Hostetter TH (1987) Hypokalemic nephropathy in the rat: role of ammonia in chronic tubular injury. J Clin Invest 79:1447–1458
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yachantha, C., Hossain, R.Z., Yamakawa, K. et al. Effect of potassium depletion on urinary stone risk factors in Wistar rats. Urol Res 37, 311–316 (2009). https://doi.org/10.1007/s00240-009-0220-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00240-009-0220-6