Abstract
Management of cerebrospinal fluid (CSF) leak due to a variety of clinical conditions is a challenging problem for the neurosurgeon, and life-threatening complications can arise unless the CSF leak is handled appropriately. Numerous methods have been described and used for prevention of CSF rhinorrhea, including vascularized pedicle flaps, free vascularized flaps, grafts, and alloplastic materials. The primary objective of this study is to evaluate the role of Cortoss, which provides three-dimensional reconstruction with watertight and weight-bearing support in the treatment of anterior cranial base bony defects. Ten consecutive patients with anterior skull base defects including frontal bone, frontal sinus, cribriform plate, orbital roof, ethmoid sinus, planum sphenoidale, sphenoid sinus, secondary to tumor invasion or traumatic injury were included in this study. The surgical technique is simple and effective, and consists of filling the bony defect with Cortoss. Surgical glue was required for dural repair only. Lumbar CSF drainage in the postoperative period was performed in two patients. These patients had fractures in the lateral walls of their sphenoid sinuses, which were managed via intracranial route. At a mean postoperative follow-up time of 8.9 months, none of the patients had developed complications including infections, meningocele, or recurrent CSF fistula. The use of Cortoss in the case of anterior skull base defects seems to be safe, effective, quick, and a feasible method for reconstruction. This technique may eliminate the use of adjunct materials including fat, muscle, fascia, and bone.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Any defect in the skull base allowing communication between the intracranial contents and nasopharynx should have separation of these two distinct anatomical regions. Isolating the anterior cranial fossa from the contaminated areas is of extreme importance for the prevention of ascending infection. The majority of defects of the skull base are usually caused by a variety of conditions including invasive tumors and traumatic brain injuries. Several types of material have been used for anterior skull base reconstruction (ASBR), these include pericranium, temporalis fascia, fascia lata, muscle and fat grafts, synthetic/cadaveric dura, titanium mesh, hydroxyapatite bone cement (HAC), etc. [1, 10–12, 14, 16–18, 21, 23]. However, such traditional practice cannot prevent CSF leak in 100% of cases, and life-threatening infections and abscesses can still occur. A more rigid repair may be required for preventing the development of meningoencephalocele, lessening dead space and decreasing the risk of infection in patients with large cranial base defects.
Cortoss (Orthovita Inc., Malvern, Pa., USA) is a high-strength, self-setting, injectable synthetic bone void composite, which is engineered specifically to mimic the strength characteristics of human cortical bone. Cortoss is approved for sale in Europe for use in skull and vertebral augmentation procedures, including compression fractures caused by osteoporosis and invasive tumors [23]. Cortoss meets all the safety requirements of the International Standard Organization (ISO) 10993 and in Europe has been used successfully for the treatment of vertebral compression fractures (VCFs). The results of a European clinical study were presented in Helsinki at the EFORT Congress, August 2003 [23]. A new pilot study of Cortoss for repair of VCFs using a kyphoplasty technique to relieve pain and to restore the load-bearing capacity to fractured vertebrae will be conducted at four sites in the USA and will enroll 20 patients [23]. Cortoss is not currently available for commercial distribution in the USA.
In this paper, we report our experience in ten consecutive patients in whom Cortoss was used alone to reconstruct anterior skull base defects and for the obliteration of the frontal and sphenoid sinuses. This technique provides rigid support, is not associated with infection, and no CSF leak occurred in the follow-up period.
Clinical material and methods
This prospective and uncontrolled clinical study included ten consecutive patients who required anterior skull base reconstruction. All patients provided informed consent. The authors had no relevant financial interest in this material. Of the ten patients, seven and three were male and female, respectively, with a mean age of 33.4 years (range; 27–48 years). Table 1 shows the summary of the clinical data of the ten patients included here.
The skull base defects or the fractures were caused by trauma (due to traffic accidents) in four, tumor resection (enplaque meningioma involving the frontal sinus) in one, falling from a height in one, fight in one, occupational accident (blast injury) in one, gunshot wound in one, and iatrogenic (due to ear–nose–throat surgery) in one patient. Three patients showed signs of meningitis as an initial presentation at the time of hospital admission and after recovering from meningitis with medical treatment; they underwent reconstructive surgery.
Physical and neurological examinations showed CSF rhinorrhea in three patients, right eye amaurosis in one patient, and bilateral eye amaurosis in one patient. No abnormal findings were noted in the remaining patients.
Radiological work-up included 1–2 mm contiguous coronal slices in bone windows computerized tomography with administration of low-dose contrast agent and magnetic resonance (MR), and cisternography with administration of gadolinium for accurate localization of the CSF fistula.
ASBR was performed by the same surgeon (G.Z.S.) in an identical manner in all patients by using the method described below.
Surgical technique
In each patient, a standard bifrontal low craniotomy was performed for ASBR. Briefly, a bicoronal skin incision was made and as the scalp was reflected anteriorly, special effort was made to avoid any damage to the pericranium. The pericranium was then cut a few centimeters behind the skin incision and bilaterally above the superior temporal lines and reflected anteriorly. Both temporal muscles were dissected from their superior temporal insertions. A bilateral low frontal craniotomy was then performed and the frontal sinus mucosa was coagulated and meticulously dissected from the walls of the sinuses. In cases of a posterior wall fracture of the frontal sinus, the wall was completely removed and the nasofrontal duct was plugged with temporal muscle. If the posterior wall was intact, we did not cranialize the sinus previously this was one of our “gold standards”.
The anterior skull base floor was exposed by extradural dissection. Reconstruction and closure began by suturing the dural tears or patching large dural holes with cadaveric dural material and fibrin glue. Small dural openings were closed with primary suturing and larger defects were left open until final closure. The anterior cranial area was kept as dry as possible with dry cottonoids and continuous suction. Cortoss was packed into the defects irrespective of the site. We prefer to fill the frontal sinus with Cortoss instead of ablating it; this decreases the dead space in the anterior skull base.
Linear skull base fractures were also plastered over with Cortoss. Following bone reconstruction, large dural openings were repaired by cadaveric dural material with fibrin glue. The craniotomy was closed in the standard fashion and the patients received antibiotic agents intravenously for 24 h postoperatively. In this technique, fibrin glue, galea frontalis, or other vascularized or non-vascularized flaps, and artificial flaps were not used for ASBR. Furthermore, only two patients required external CSF drainage in the postoperative period. Only surgical glue and cadaveric dural flaps were used for dural repair.
Results
All patients were available for follow-up review. At a mean follow-up of 8.9 months (range; 6–13 months), no adverse reaction related to Cortoss was observed. None of the patients developed meningitis and CSF leakage. The results from this study showed that the rate of postoperative infection and of postoperative CSF leakage were 0%. This is much lower than the literature pertaining to this area in which other techniques for anterior cranial base reconstruction have been reported [1, 10–12, 14, 16–18, 21, 23]. Lumbar CSF drainage during the postoperative period was performed in two patients, who needed sphenoid sinus packing plus Cortoss application inside their sinuses via intracranial route for the fractures in the lateral walls of the sphenoid sinuses. Furthermore, brain herniation or encephalocele formation was not encountered in any of our patients. The postoperative period of all patients was uneventful and the mean hospital stay was shorter than in the past.
Illustrative case
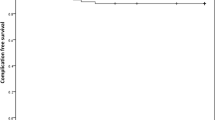
A 37-year-old woman (sixth patient in Table 1) complained of right nasal discharge for a year. She had a history of resection of a right nasal polyp 8 years before being admitted to our department. MR cisternography with intrathecal contrast agent revealed a defect on the lateral wall of the right sphenoid sinus (Fig. 1). The patient underwent surgery in which the lateral wall of the sphenoid sinus was augmented with a layer of cadaveric dura plus fibrin glue and the three-dimensional gap in the right side of the sphenoid sinus was filled by gradual injection of Cortoss. The ablated frontal sinus was also filled with Cortoss without the need for cranialization (Fig. 2a, b). The patient had an uncomplicated postoperative course, and there was no evidence of CSF leak or other complications after 7 months follow-up (Fig. 3a–c).
Postoperatively, (a) plain radiograph shows homogeneously radiopaque Cortoss filling the frontal and right sphenoid sinuses. (b) Axial CT scans showing complete filling of the right sphenoid sinus. (c) A photograph of the patient showing no cosmetic deformity at 7th month postoperatively. (The photograph was taken with the permission of the patient)
Discussion
In this study, the use of Cortoss in anterior cranial base defects has proved to be a simple and effective method of reconstruction. The use of this technique in ten consecutive patients with a variety of bony defects prevented infection and postoperative CSF leakage.
Numerous methods for reconstruction of craniofacial defects, including metallic mesh, silicon, polymethylmethacrylate (PMMA), autogenous bone, HAC, vascularized pericranial flaps, postoperative CSF diversion, occlusion of sinuses with fat, muscle, and/or fibrin glue have been used [1, 14, 16–18, 21, 24]. However, each method has its own drawbacks, such as increased intraoperative time, postoperative infections, cosmetic deformities, recurrent CFS fistulae, and prolonged hospitalization.
Although some authors encourage the use of vascularized pericranium or bone flaps for cranial base defects, watertight bone reconstruction cannot be obtained in most cases, and if the patient has a large bony defect that may lead to meningocele and CSF leak. For this purpose, alloplastic materials have been developed, which led to a revolution in the treatment of craniofacial reconstruction. Titanium mesh, HAC, and PMMA are the commercially available and currently used materials, that allow easy contouring and/or application but have limitations [1, 9, 17, 24, 25].
Titanium mesh has been used for large anterior skull base defects over the last few years. Nevertheless, the risk of postoperative CSF leak, foreign body reactions, cosmetic deformities, and postoperative infections has not decreased with the use of titanium mesh. In addition, some authors have emphasized that the use of vascularized pericranium along with titanium mesh is essential for prevention of postoperative CSF leakage and cerebral infection [1, 20]. On the other hand, we believe that such adjunct materials increase the risk of infection and are time consuming.
After demonstrating the successful application and satisfactory results in animal models, numerous reports have described the use of HAC in humans [5, 17, 21, 24, 25]. Watertight closure of dead space after temporal bone surgery, successful reconstruction of the suboccipital craniotomy, and craniofacial reconstruction by HAC have been described in several reports [3, 17]. In such reports, the dead space obliteration with HAC seems to have a high rate of postoperative infection and failure. The important disadvantages that limit the use of HAC and require removal of cement are dissolution of implant, additional operative time awaiting setting, and anecdotal failure to prevent CSF fistula. HAC should be applied in a dry field because it washes out in the presence of blood, CSF, and other fluids. Some authors suggest that use of adjunct materials with HAC, such as titanium mesh, should be used for proper contouring and saving the material from the repetitive trauma of dural pulsations [17, 21, 24].
In our institution, we previously used HAC in three patients with anterior cranial fossa bone defect. After reconstitution of the material according to the manufacturer’s directions, the operative field had to be kept dry at least 30 min because oozing of blood, CSF, and other fluids into the operative field affected the settings and surgical outcome. As a result of this we decided that application of HAC alone was not enough to provide rigid support and so-called “gold standard” methods were added. These included the galea frontalis flap, frontal sinus cranialization, nasofrontal duct plugging with muscle, and reinforcement of dura with cadaveric dura in conjunction with fibrin glue. We think that such additive materials increase the infection rate and are time consuming in addition to increasing the cost.
Due to its elasticity, PMMAs have been used extensively in orthopedic and dental procedures for years. In neurosurgery, it was commonly used in the past for sealing the frontal sinus but was given up largely because of postoperative infection [4, 22]. It has been shown that hardening of PMMA is usually associated with an exothermic reaction that can lead to tissue necrosis and heat injury. In addition, it may show foreign body giant cell reactions due to becoming encased in a fibrous capsule over time. More importantly, it does not allow proper tissue incorporation [6].
Considering the disadvantages and/or complications related to the currently used alloplastic biomaterials described above, they do not differ from one another and these problems prompted us to develop a new technique that is simple, effective in providing rigid support, and was not associated with postoperative failure, infection, and cosmetic deformity.
The requirements of more stronger and rigid inelastic systems than the thermoplastic PMMA led to the development of bis-GMA (2, 2-bis[4-(2-hydroxymethacryloxypropyl) phenyl] propane) based composed system. Since bis-GMA based systems (thermoset system) are more durable and stronger than other alloplastic materials, several authors have used these in vertebral augmentations [7], repair of craniofacial defects [24], and stabilization of orthopedic prosthetics [10].
A glass–ceramic reinforced composite, Cortoss (Orthovita Inc., Malvern, Pa., USA) is a new synthetic bone void filler and is terpolymer, which is primarily composed of bis-GMA, a bifunctional monomer providing high viscosity and high strength, and bis-EMA (2,2-bis[4-(2-methacryloxyethoxy)] phenylpropane). It is a bifunctional monomer providing low viscosity and high strength. Additionally, triethylene glycol dimethacrylate (TEGDMA) is a reactive diluent that is also used in this system to provide flexibility to the material. These matrix materials in Cortoss form the polymer matrix, immediate load bearing, and cortical bone void filler [13, 19].
The isothermal analysis conducted in the 40°C site has shown that the Cortoss yields polymerization and no exothermic reactions were noted. This temperature is closest to biological conditions (37°C) and this explains why Cortoss does not cause tissue necrosis and heat injury [19]. Studies by several researchers have indicated that the maximum exothermic temperature of Cortoss is 24% lower than that of PMMA (typically 55–65°C versus 90–120°C, respectively). Besides, it attains peak exotherm for a short period of time (1–2 min) whereas PMMA remains above 51°C for up to 8 min [2, 16, 20]. Cortoss does not contain volatile monomers, which are found in PMMA that can migrate within the body in an uncontrollable fashion. Histopathological studies in sheep have illustrated that Cortoss achieves two stages of fixation: immediate mechanical interlocking into porous bone, followed by intimate bone ingrowth along the contours of the surface without an intervening fibrous layer [8]. In addition, the calcium phosphate-rich (Ca–P) layer allows adjacent bone to integrate into and along the Cortoss surface. Cortoss was well tolerated in all (rabbit, sheep, and rat) preclinical safety studies. It demonstrated no significant biological reactions and no systemic or long-term toxicity. It is non-mutagenic, non-pyrogenic, non-clastogenic, and non-hemolytic [8, 15]. Erbe et al. [8] showed that new periosteal and endosteal bones were formed within defect sites filled with either Cortoss or PMMA, but initial response was greater with Cortoss in rabbit and sheep tibia. Subsequently, the periphery of Cortoss implants was invaded by new blood vessels that supported reparative osteogenesis. The authors pointed out that the greater stability of the bone/Cortoss interface was attributed to a faster initial bone response and a greater degree of mineralization around Cortoss. A study using rat tibia showed that Cortoss contacted the bone directly through a Ca–P rich layer without an intervening fibrous layer [15].
The complete Cortoss system includes high surface area inorganic fillers, which are activated with a silane-coupling agent that is terminated with a methacrylate group to covalently link the cross-linking polymer framework formed from the reaction of the bifunctional monomers (Bis-GMA, Bis-EMA, and TEGDMA) with the inorganic fillers. This property provides reinforcement of the polymer matrix. Other reinforcing components includes synthetic combeite glass–ceramic particles that increases direct bonding to bone, improves mechanical strength, baria-boroalumino-silicate glass, which improves inherent radiopacity, and silica, which improves viscosity, and handling [16, 20].
This is the first preliminary clinical study showing the effectiveness and appropriateness of Cortoss in the treatment of CSF fistula secondary to anterior skull base defects. We achieved successful watertight closure of bone defects and obliteration of dead spaces and/or sinuses. No adverse reaction and/or complication related to the material was noted.
Our experience showed that preparation, and application of Cortoss were very simple, and contouring the defects was easier than with other currently available materials. We have not seen significant contour changes developed postoperatively. The operative time was not increased and oozing of fluids into the surgical field did not affect the setting when compared to other techniques. Mix-on-demand delivery of Cortoss facilitates fast, easy handling, negating the need for longer setting time. It sets in 5–8 min, less than half the time of PMMA and the setting time is temperature-dependent and decreases as the site temperature increases [8, 15, 16, 20]. All patients showed no infection or recurrent CSF leak. Therefore, its healing properties and extremely low rate of morbidity are its great advantages. In addition, Cortoss was strong enough to provide rigid support alone and eliminated the use of adjunct alloplastic materials or vascularized/non-vascularized flaps, and postoperative CSF drainage. Thus it is cost effective, time saving, and has decreased the risk of postoperative infection.
It has been emphasized that reconstruction of bone defects in the cranial base should preferably be done with the help of bone, particularly the use of a bone flap based on a vascularized pedicle. However, necrosis and resorption are the common problems encountered with free bone grafts. In addition, cosmetic deformities may be seen after bone flaps if particularly associated with vascularized pedicle. Molding and contouring such flaps over cranial defects is usually difficult. Postoperative hematoma as around the bone flaps is another important issue that may increase the risk of postoperative infection. Soft tissue flaps with or without bone frequently require additional materials that increase the cost and operative time. Such techniques are not structurally strong enough to prevent CSF leak and infection. Cosmetic deformities are also seen in techniques using soft tissue flaps. Some recent reports documented that galeofrontalis flaps often produce visible irregularities on the forehead and leave the forehead skin very thin and vulnerable to breakdown [18, 21, 24]. Another pitfall arises if patients have a history of previous surgery and trauma, which causes injury to the pericranial galeal flaps, or bone so that there may not be intact or sufficient tissues for reconstruction. The majority of such techniques using soft tissues alone or in combination with bone flaps usually require external CSF drainage in the postoperative period.
It is obvious that prevention of herniation of the brain matter through the defect is possible by using materials that are more rigid and thus potentially offer better long-term results. The most crucial advantage of our technique with Cortoss, when compared with others, is the creation of a watertight bony separation between the contents of the anterior cranial fossa and the upper aerodigestive tract. Resistance to infections of Cortoss may come from its decreased porosity that renders it impermeable to cells and infectious agents, particularly to bacteria [8, 15, 19]. However, we must point out that this is a study with a rather limited number of patients and with a very short follow-up period (mean 8.9 months). The potential for complications such as infection may still occur in the long-term follow-up period. Therefore, we need clinical studies with a large patient population in which Cortoss is used and need long-term follow-up (at least 8–10 years) in order to exclude long-term complications definitely.
The recess that continues to the frontonasal duct in the frontal sinus is obliterated; this eliminates the need for the use of fibrin glue or additional tissues for watertight seal of the defects. Additionally, normal anatomy is well preserved with our technique, since it does not cause any cosmetic deformity.
In conclusion, we have found Cortoss to be a simple and effective material for treatment of anterior skull base defects and the obliteration of the frontal and ethmoid sinuses. CSF is a very “mean” liquid, if not handled according to its natural behavior pattern. There is no place for “wishful thinking” in this type of surgery. The possibility of dural tears and bony gaps, particularly after trauma, should be taken into consideration. In such highly problematic cases, the surgery should be done once and for all. The dura overlying the anterior fossa should be examined for any tears under the illumination and magnification, preferably with the operating microscope. If found and if possible, it should be sutured. Nevertheless, if not possible, the area must be augmented with dural substitutes such as solvent dehydrated Tutoplast Bovine Pericardium (Tutogen Medical Gmbh, Parsippany, N.J., USA) and reinforced with fibrin glue. The worse scenario is an unnoticed dural tear situated deeply, associated with a bony fracture crossing the planum sphenoidale. This is why we believe there is no place for “assumptions”. In cases of fractures traversing the olfactory groove and planum sphenoidale, the surgeon should not hesitate to dissect the dura. We claim that ASBR with Cortoss will eliminate the need for intradural explorations. The bony floor from the frontal through the sphenoid sinuses can be plastered and/or filled with Cortoss, even in the presence of dural tears reaching to the sella floor. Thus, watertight bony closure can be achieved, and deeply located dural tears, which are difficult to reach for suturing, do not interfere with the surgeon’s sleep.
References
Badie B, Preston JK, Hartig GK (2000) Use of titanium mesh for reconstruction of large anterior cranial base defects. J Neurosurg 93:711–714
Bowman CN, Peppas NA (1991) Coupling kinetics and volume relaxation during polymerizations of multiacrylates and multimethacrylates. Macromolecules 24:1914–1920
Bronson JG (2003) Tissue transplantation and engineering: what is happening? Orthop Technol Rev 5(5). http://www.orthopedictechreview.com
Costantino PD, Friedman CD, Jones K, Chow LC, Sisson GA (1992) Experimental hydroxyapatite cement cranioplasty. Plast Reconstr Surg 90:174–185
Costantino PD, Friedman CD, Jones K, Chow LC, Pelzer HJ, Sisson GA (1999) Hydroxyapatite cement, I: basic chemistry and histologic properties. Arch Otolaryngol Head Neck Surg 117:379–384
Costantino PD, Chaplin JM, Wolpoe ME et al. (2000) Applications of fast-setting hydroxyapatite cement: cranioplasty. Otolaryngol Head Neck Surg 123:409–412
Costantino PD, Hiltzik DH, Sen C et al. (2001) Sphenoethmoid cerebrospinal fluid leak repair with hydroxyapatite cement. Arch Otolaryngol Head Neck Surg 127:588–593
Deramond H, Depriester C, Galibert P, Le Gars D (1998) Percutaneous vertebroplasty with polymethylmethacrylate, technique, indications, and results. Radiol Clin N Am 36:533–546
Erbe EM, Clineff TD, Gualtieri G (2001) Comparison of a new bisphenol-a-glycidyl dimethacrylate-based cortical bone void filler polymethyl methacrylate. Eur Spine J 10:S147–S152
Goel A, Gupta S (2000) Reconstruction of the skull base: a review of personal technique. Neurol India 48:208–215
Jackson IT, Adham NM, Marsh WR (1986) Use of the galea frontalis myofacial flap in craniofacial surgery. Plast Reconstr Surg 77:905–910
Jones NF, Sekar LN, Schramm VL (1986) Free rectus abdominis muscle flap reconstruction of the middle and posterior cranial base. Plast Reconstr Surg 78:471–477
Kawanabe K, Tamura J, Yamamuro T, Nakamura T, Kokubo T, Yoshihara S (1993) A new bioactive bone cement consisting of bis-GMA resin and bioactive glass powder. J Appl Biomater 4:135–141
Kawaura M, Nameki H, Fujii M, Kanzaki J (1997) Use of vertical median forehead flap in the reconstruction of the anterior skull base: report of two cases. Auris Nasus Larynx 24:379–383
Kobayashi M, Nakamura T, Tamura J, Kikutani T, Nishiguchi S, Mousa WF, Takahashi M, Kokubo T (1999) Osteoconductivity and bone-bonding strength of high- and low-viscous bioactive bone cements. J Biomed Mater Res (Appl Biometer) 48:265–276
Krishman KG, Winkler PA, Müller A, Grevers G, Steiger HJ (2000) Closure of recurrent frontal skull base defects with vascularized flaps: a technical report. Acta Neurochir (Wien) 142:1353–1358
Mathur K, Tatum SA, Kellman RM (2003) Carbonated apatite and hydroxyapatite in craniofacial reconstruction. Arch Facial Plast Surg 5:379–383
Mori K, Nakajima M, Maeda M (2003) Simple reconstruction of frontal sinus opened during craniotomy using small autogeneous bone piece: technical note. Surg Neurol 60:326–328
Pomrink GJ, DiCicco MP, Clineff TD, Erbe EM (2003) Evaluation of the reaction kinetics of Cortoss, a thermoset cortical bone void filler. Biomaterials 24:1023–1031
Price JC, Loury M, Carson B, et al. (1998) The pericranial flap for reconstruction of anterior skull base defects. Laryngoscope 98:1159–1164
Ross DA, Marentette LJ, Thompson G, Haller J (1999) Use of bone cement to prevent cerebrospinal fluid leakage through the frontal sinus: technical report. Neurosurgery 45:401–403
Senyuva C, Yucel A, Okur I, Cansız H, Sanus GZ (1996) Free rectus abdominis muscle flap for the treatment of complications after neurosurgical procedures. J Craniofac Surg 7(4):317–321
Shindo ML, Costantino PD, Friedman CD, Chow JC (1993) Facial skeletal augmentation using hydroxyapatite cement. Arch Otolaryngol Head Neck Surg 119:185–190
Weissman JL, Synderman CH, Hirsch BE (1996) Hydroxyapatite cement to repair skull base defects: radiologic appearance. Am J Neuroradiol 17:1569–1574
Yamamuro T, Nakamura T, Iida H, Kawanabe K, Matsuda Y, Ido K, Tamura J, Senaha Y (1998) Development of bioactive bone cement and its clinical applications. Biomaterials 19:1479–1482
Author information
Authors and Affiliations
Corresponding author
Additional information
An erratum to this article can be found at http://dx.doi.org/10.1007/s00238-005-0807-2
Rights and permissions
About this article
Cite this article
Sanus, G.Z., Tanriverdi, T., Kafadar, A.M. et al. Use of Cortoss for reconstruction of anterior cranial base: a preliminary clinical experience. Eur J Plast Surg 27, 371–377 (2005). https://doi.org/10.1007/s00238-004-0711-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00238-004-0711-1