Abstract
Purpose
To compare thalamic volume and cognitive functions of patients with mild autonomous cortisol secretion (MACS) with control subjects and patients with overt Cushing’s syndrome (CS).
Methods
In this cross-sectional study, volumes of regions of interest were assessed using 3 T magnetic resonance imaging and a voxel-based morphometry approach in 23 patients with MACS, 21 patients with active CS, 27 patients with CS in remission, and 21 control subjects. Cognitive functions were assessed using validated questionnaires.
Results
Patients with MACS had smaller left thalamic (F = 3.8, p = 0.023), left posterior thalamic (F = 4.9, p = 0.01), left medial thalamic (F = 4.7, p = 0.028), and right lateral thalamic (F = 4.1, p = 0.025) volumes than control subjects. Patients with active CS also had smaller left thalamic (F = 3.8, p = 0.044), left posterior thalamic (F = 4.9, p = 0.007), left medial thalamic (F = 4.7, p = 0.006), and right lateral thalamic (F = 4.1, p = 0.042) volumes compared to controls. Patients with CS in remission had smaller left medial (F = 4.7, p = 0.030) and right lateral thalamic (F = 4.1, p = 0.028) volumes than controls. Neuropsychological tests showed no difference between the groups.
Conclusion
MACS may decrease thalamic volume.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cushing’s syndrome (CS) is characterized by overt signs and symptoms of hypercortisolism [1]. Because of the widespread distribution of glucocorticoid receptors (GRs) throughout the body, exposure to hypercortisolism results in a wide range of physical, metabolic, reproductive, psychological, and cognitive impairments. Like many other organs, the brain has a high density of GR and mineralocorticoid receptors (MR), making it an important target for the neurotoxic effects of hypercortisolism [2]. Early structural magnetic resonance imaging (MRI) studies of the brain provided convincing evidence of overall brain atrophy in patients with CS [3]. With the novel techniques of neuroimaging, some areas of the brain that are related to cognition have been shown to be exclusively vulnerable to the toxic effects of overt hypercortisolism [4-9]. Since then, the number of studies reporting the relationship between CS, brain volume, and cognitive functions has increased [6, 10-12].
Mild autonomous cortisol secretion (MACS), formerly called “subclinical CS,” is characterized by subtle cortisol excess due to adrenal adenoma [13, 14]. The difference between overt CS and MACS is the severity of the biochemical and physical findings. Although to a lesser extent, this subtle form of cortisol excess also increases the risk of diabetes, hypertension, obesity, osteoporosis, morbidity, and mortality [15-18]. Therefore, vigilant screening of these comorbidities is recommended in patients with MACS. Intriguingly, data regarding the effect of MACS on brain structure and cognitive functions are scarce, and no consensus exists on screening. When the abundance of GR and MR in the brain is considered, it is tempting to speculate that brain abnormalities found in patients with CS also apply to patients with MACS, at least to a certain degree.
The studies of neuroimaging in patients with hypercortisolism have primarily sought to demonstrate the structural and functional alterations of the cortical gray matter (GM) and the limbic system over half a century [6, 7, 12, 19-23]. Nevertheless, the structural alterations of the thalamus have been relatively overlooked in patients with overt hypercortisolism and, to our knowledge, have never been assessed in patients with MACS. The thalamus is a subcortical structure composed of a heterogeneous group of nuclei which have distinct synaptic inputs and cortical connections [24]. It is now recognized as one of the main players in attention, memory, and language functions [25]. In the present exploratory study, our primary objective was to investigate whether patients with MACS have volumetric changes in the whole thalamus and thalamic nuclei and to demonstrate their reflections on attention, memory, and language functions. We also sought to assess whether the anticipated changes in thalamic volume and cognitive functions in patients with MACS differ from those in patients with overt hypercortisolism. To this end, we also compared the volume of the region of interest (ROI) and the neuropsychological performance of patients with CS, patients with MACS, and control subjects. Finally, we performed an exploratory analysis of the whole brain to identify unexpected structural changes in regions outside the priori-defined ROI in patients with CS and patients with MACS.
Materials and methods
Setting
The present study was approved by the Medical Research Ethics Committee (03.05.2021/45781) and was conducted between 2021 and 2022 in the Endocrinology, Metabolism, and Diabetes Outpatient Clinic.
Subjects and procedure
The study sample consisted of four groups: (i) patients with MACS, (ii) patients with active CS, (iii) patients with CS in remission, and (iv) a control group.
For this study, all patients with MACS monitored at our institute who had at least one clinical visit in 2020 (n = 41) were approached by phone. The response rate was 92.7%. Inclusion criteria were (i) age being between 18 and 65 years, (ii) right-handedness, (iii) being able to comprehend the Turkish language, and (iv) presence of consent to participate. Exclusion criteria were (i) presence of severe neurological and/or psychiatric disease, drug, and/or alcohol abuse, (ii) presence of intellectual disability, illiteracy, visual, and/or hearing impairment, (iii) presence of growth hormone (GH) deficiency, hypothyroidism, or hyperthyroidism, (iv) presence of brain damage or contraindication for MRI, (v) presence of acute illness (acute myocardial infarction, sepsis, etc.) or major organ failure (end-stage renal disease receiving renal replacement therapy, decompensated heart failure, liver failure, etc.), and (vi) individuals with acute or chronic inflammatory diseases (human immunodeficiency virus infection, systemic lupus erythematosus, etc.) that could confound the volumetric analyses of the ROI.
To investigate the effects of varying degrees of hypercortisolism on brain volumes, patients with pituitary-dependent CS (Cushing’s disease (CD) and adrenal-dependent CS were screened for eligibility. Subjects were selected from consecutive patients with CS who had a routine endocrinologic examination between April 2021 and December 2021 (n = 135). The inclusion and exclusion criteria for the patients with MACS were also applied to the remaining patients with CS.
The control subjects were chosen among volunteers who came for routine medical board report for job application between April 2021 and December 2021 (n = 40). All the volunteers underwent a detailed examination to detect possible clinical signs and symptoms of CS. The subjects with overt signs and/or symptoms attributable to CS, subjects who had been exposed to exogenous glucocorticoids within the past 6 months, and subjects with diabetes and/or uncontrolled hypertension were excluded [26, 27]. Biochemical hypercortisolism was also excluded in each subject by showing both suppressed morning serum cortisol levels (< 1.8 μg/dl) after overnight dexamethasone test (DST) and normal late-night salivary cortisol (LNSC) level (see Supplementary Table 1). The inclusion and exclusion criteria described above for the MACS group were also applied to the control group. To minimize the effects of age and educational level on the comparisons of brain volumes and neuropsychological tests, the patients with CS and control subjects were matched to patients with MACS via Phyton 3-based computer program. The algorithm took the age, education level, eligibility, and study group as inputs and matched patients with active CS, patients with CS in remission, and control subjects to patients with MACS of a similar age and education level. The program did not remove the previously matched patients with MACS from a given list to achieve maximum pair of patients. A total of 23 patients with MACS, 21 patients with active CS, 27 patients with CS in remission, and 21 control subjects were included. The inclusion process was shown in Fig. 1.
A single study visit of approximately two and a half hours was scheduled for each eligible participant. The visit consisted of an MRI scan that took place between 2:00 and 3:00 pm, followed by a standardized interview by the single blind researcher (T.B.I.) for the administration of neuropsychological tests (60 min) and a detailed examination for the assessment of clinical data by an endocrinologist (C.S.) (30 min) (Fig. 1).
Clinical definitions
The diagnosis of MACS was defined as a morning cortisol level > 1.8 ng/dl after 1 mg DST in the absence of stigmata of CS (facial plethora, buffalo hump, violaceous abdominal striae, proximal muscle weakness, and fragile skin with bruising) in a patient with adrenal incidentaloma [28, 29]. In our center, patients with MACS are screened annually to detect the possible development of overt CS features, type 2 diabetes mellitus, hypertension, and asymptomatic vertebral fracture in accordance with the European Society of Endocrinology clinical practice guidelines [28].
The diagnosis, treatment, and follow-up of CD and adrenal-dependent CS were based on internationally agreed guidelines [30-33]. Patients with CD or adrenal-dependent CS were considered to have active CS in the presence of overt clinical signs and symptoms and biochemical tests including increased urinary excretion rates of free cortisol, decreased overnight suppression by 1 mg dexamethasone, and elevated LNSC. Patients with CD or adrenal-dependent CS were considered in remission in the absence of signs, symptoms, and positive biochemical tests of hypercortisolism [30].
Cortisol assay
The Elecsys Cortisol generation II electrochemiluminescence competitive immunoassays were run on the Cobas E602 (Roche Diagnostics, Indianapolis) to determine the serum cortisol and LNSC levels of the participants.
MRI data acquisition and post-processing
All neuroimaging was performed in our institute using a 3 T Philips Ingenia MR scanner (Philips, Best, the Netherlands) with a 16-channel head coil. The imaging protocol included the whole brain T1-weighted 3D TFE (Turbo Field Echo) high-resolution anatomical imaging with a repetition time of 8.2 ms, echo time of 3.7 ms, flip angle: 8°, FOV: 256 × 256, 1 mm isotropic resolution, and 200 slices. Acquisition time is approximately 5.5 min. Before preprocessing, all images were evaluated for any structural brain parenchyma lesions by a European board-certified neuroradiologist (SA), and patients with incidental lesions were excluded. All images were preprocessed on a Linux-based computing system through a standard, automated processing stream within Freesurfer 7.2.0 (https://surfer.nmr.mgh.harvard.edu) called “recon-all.” The recon-all pipeline consists of 29 distinct steps that ultimately lead to cortical reconstruction and volumetric segmentation. Briefly, the processing steps are as follows: (i) removal of non-brain tissue, (ii) Talairach transformation, (iii) segmentation of the subcortical deep GM structures (including the hippocampus, amygdala, thalamus, caudate, putamen), (iv) intensity normalization, (v) tessellation of the GM-white matter boundary along with automated topology correction, and (vi) intensity gradient-based surface deformation to optimally adjust the gray-white matter boundary and pial surface borders [34-40] (Fig. 2). The resulting surface models were then inflated and registered to a standard spherical surface atlas, allowing the parcellation of the cerebral cortex into specific gyral and sulcal units [41]. For all analyses, images were smoothed with a 10-mm full-width at half-maximum Gaussian distribution. Cortical volume values were computed for 34 Desikan-Killiany (DK) atlas regions per hemisphere [42]. Additionally, volumes of the subcortical structures and total intracranial volume (ICV) were obtained.
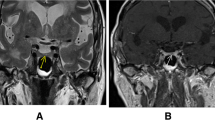
For the segmentation of the thalamus and other subcortical deep GM structures, we used automated modules provided in the FreeSurfer 7.2.0 software suite (HippocampalSubfieldsAndNucleiOfAmygdala and ThalamicNuclei, respectively). All the thalamic nuclei groups included in the analyses can be found in Fig. 3 and Supplementary Table 2. FreeSurfer subcortical deep GM segmentation algorithms use probabilistic atlases based on Bayesian inference and are built primarily upon ultra-high-resolution ex vivo MRI data from post-mortem specimens (~ 0.1–0.15 mm isotropic) to generate a fully automated segmentation. The technical details of all the steps in these modules were described in the original method articles [43, 44]. Before statistical analysis, all images were manually inspected by a senior neuroradiologist (SA) to ensure the accuracy of cortical parcellation and subcortical segmentation.
Assessment of psychopathology and cognitive functioning
Beck depression inventory (BDI)
It was developed by Beck et al. to measure the level of depressive symptoms [45]. It consists of 21 items on a 4-point Likert scale. Total scores can range from 0 to 63. Higher scores indicate increased depressive symptoms.
Beck anxiety inventory (BAI)
It is a screening for the detection of symptoms that constitute anxiety and discriminating them from depression symptoms [45]. It consists of 21 items on a 4-point Likert scale. The total score can range from 0 to 63. Higher scores indicate increased anxiety.
Montreal cognitive assessment (MoCA)
It is a useful screening tool with high specificity and sensitivity for assessing cognitive capacity and detecting mild cognitive impairment [46, 47]. MoCA measures concentration, executive functions, memory, language, visuospatial abilities, abstract thinking, calculation, and orientation domains. The maximum score is 30 [46]. Higher scores indicate better cognitive functions.
Selective reminding test (SRT)
It is a test designed to measure verbal learning and memory through the use of a list-learning procedure over multiple trials [48]. In the present study, the short adult version of SRT was used which involves reading the participant a list of 12 unrelated words and then expecting the participant immediately recall as many of these 12 words as possible for six trials [49]. Every trial after the first involves selectively presenting the words that were not recalled by the subject on the previous trial, and recall scores on each trial are noted. This test is suggested to distinguish between retrieval from long-term storage (LTS) and short-term recall (STR) by assessing the recall of items that are not presented on a given trial. The maximum score of SRT is 72. Higher scores indicate better verbal learning and memory. We also applied a delayed recall trial (SRT-DR) without any forewarning or clue 20 min after the completion of six trials.
10/36 spatial recall test (SPART)
It is a measure of visuospatial learning and memory. A 6 × 6 checkerboard containing a pattern of randomly organized 10 checkers is initially presented to a participant for 60 s. Thereafter, the participant is expected to replicate the original pattern on a blank checkerboard. This process is repeated two more times and followed by a delayed measure after the passage of 20 min. SPART immediate recall (SPARTT) score is the sum of the total number of correct responses (i.e., the number of correct checkers) of the three attempts. SPART delayed recall (SPARTD) score is the product of correct responses in the delayed condition [50]. The maximum scores of SPARTT and SPARTD are 30 and 10, respectively. Higher scores indicate better visuospatial learning and memory.
Symbol digit modalities test (SDMT)
It is a test that examines information processing speed, divided attention, visual scanning, and tracking [51, 52]. The participant sees a model in which the nine geometric symbols are labeled 1 to 9. The SDMT measures the time to match the symbols with corresponding numbers as quickly as possible in 120 s. The total number of correctly paired symbols in this time period reflects the speed of each participant needs for processing information. The maximum score is 60. Higher scores indicate better processing speed, divided attention, visual scanning, and tracking.
Word list generation test (WLG)
This test evaluates verbal fluency [52]. The participants are asked to spontaneously generate examples of either phonemic categories (words starting with letters K, A, or S for the Turkish language [WLG KAS]) or semantic categories (animals) within 60 s. The WLG score is the number of unique examples.
Statistical analyses
All analyses were performed with Statistical Package for the Social Sciences version 22.0 for macOS (IBM, 2013). Data were presented as numbers and percentages, means and standard deviations, or median and interquartile range. Normal distribution was analyzed using the Kolmogorov–Smirnov test. The assumption of equal variances was tested using Levene’s test. Clinical, laboratory, sociodemographic, and neuropsychological differences between the groups were analyzed using the Pearson chi-square test for the categorical variables, one-way analysis of variance for the normally distributed continuous variables, and Kruskal–Wallis hypothesis test for the non-normally distributed continuous variables. If necessary, differences between groups were analyzed with post hoc tests. P < 0.05 was considered as significant.
Inter-group comparisons of brain volumes
In this study, the residual method was used to explore the differences in brain volumes. The residual method uses the correlation between absolute parenchymal volumes (APV) and ICV in a linear regression equation to predict ICV-adjusted volumes for each area of interest and is based on a least squares solution which minimizes the error in predicted values. Therefore, the residual method generally provides advantages over other methods in voxel-based morphology (VBM) analysis [53].
In the present study, an analysis of covariance was performed with the variables group, ICV, and group × ICV to evaluate the effect of the interaction term for each observation. After the non-significant effect of the interaction term – in other words, “homogeneity of the regression slopes” – was ensured for a given instance, inter-group comparisons of the brain volumes were performed with a general linear model (GLM). In GLMs, APV was the dependent variable, the group was the fixed factor, and ICV was a covariate. The results were corrected according to the Bonferroni procedure to minimize the type I statistical errors. The level of significance was established at p < 0.05.
Sample size
With a significance level of 5% statistical power at 95% and allowing for a large effect size of 0.4, a sample size of 112 was required to detect the changes in volumes of ROI.
Results
Participant characteristics
The groups were similar in age, gender, and educational level. The demographic, clinical, and laboratory characteristics of the study groups are shown in Table 1.
The patients with MACS included 23 patients (17 females). The median 1 mg DST was 3.2 [IQR] 2–3.6 mcg/dl. The mean adrenocorticotrophic hormone was 7.6 ± 3.8 pg/ml.
Patients with active CS included 21 patients (20 females): 18 were of pituitary origin, and 3 were of adrenal origin. Eight patients with active CD had a history of transsphenoidal surgery (TSS); 4 of them had persistent CD, and 4 patients had recurrent CD. Ten patients with active CD had no history of TSS; 9 of them were waiting for TSS, and one patient with active CD declined TSS and received stereotactic radiosurgery (Gamma Knife) 1 year prior to assessment. For the 3 patients with adrenal CS, unilateral adrenalectomy was scheduled. The median disease duration of patients with active CS was 24 [IQR] 15–81.5 months.
Patients with CS in remission included 27 patients (25 females): 25 were of pituitary origin, and 2 were of adrenal origin. All patients with CD have undergone TSS; 2 of them have received additional stereotactic radiosurgery (gamma knife), and 2 patients underwent additional bilateral adrenalectomy. Two patients with CS of adrenal origin underwent unilateral adrenalectomy. At the time of the assessments, 7 patients were on hydrocortisone replacement therapy. The median disease duration of the CS in the remission group was 79 [IQR] 59–96 months, and the median duration of remission was 50.5 [IQR] 10.5–70 months.
The control group consisted of 21 participants (18 females). None of them had overt Cushingoid features, diabetes, uncontrolled hypertension, and chronic/complex disease that would affect neuropsychological and radiological assessments (Table 1).
MRI analyses
Volumetric variations in ROI
Absolute mean volumes of the thalamus and thalamic nuclei groups are shown in Table 2. The results of the GLM indicated that patients with MACS had smaller left thalamus volume than controls (F = 3.8, p = 0.023) (Table 2, Fig. 4). Of the total six thalamic subregions of each hemisphere considered in the exploratory analyses, patients with MACS showed smaller volumes in the left posterior thalamus (F = 4.9, p = 0.01), left medial thalamus (F = 4.7, p = 0.028), and right lateral thalamus (F = 4.1, p = 0.025) in comparison to controls (Table 2, Fig. 4). In addition, we expanded our exploratory analyses to the volumes of the pulvinar and mediodorsal nuclei of the thalamus, which represent the two largest nuclei of the primate brain (see Fig. 5 and Supplementary Video). The results indicated that patients with MACS had smaller pulvinar (F = 6.1, p = 0.003), mediodorsal magnocellular (MDm) (F = 4.9, p = 0.035), and mediodorsal lateral parvocellular (MDl) (F = 3.5, p = 0.045) nuclei of the left hemisphere in relation to controls (Table 2, Fig. 4).
As in patients with MACS, patients with active CS also showed smaller volumes in the whole thalamus (F = 3.8, p = 0.044), posterior thalamic nuclei (F = 4.9, p = 0.007), and medial thalamic nuclei (F = 4.7, p = 0.006) of the left hemisphere and the lateral thalamic nuclei (F = 4.1, p = 0.042) of the right hemisphere when compared with controls (Table 2, Fig. 4). Moreover, patients with active CS had smaller volumes belonging to the pulvinar (F = 6.1, p = 0.002), MDm (F = 4.9, p = 0.003), and MDl (F = 3.5, p = 0.060) nuclei of the left hemisphere than controls (Table 2, Fig. 4).
Patients with CS in remission had smaller volumes of the left medial thalamic nuclei (F = 4.7, p = 0.030) and the right lateral thalamic nuclei (F = 4.1, p = 0.028) as compared to controls (Table 2, Fig. 4).
Inter-group comparisons of patients with MACS, patients with active CS, and patients with CS in remission yielded no significant difference in other subcortical deep GM structures (not shown).
Volumetric variations in the other cerebral and subcortical structures
The study groups did not significantly differ in volumes of other subcortical structures (hippocampus, amygdala, putamen, and caudate) and cortex (Supplementary Tables 3 and 4).
Psychopathology and cognitive functioning
Although the patients with MACS and active CS demonstrated higher levels of depression and anxiety symptoms and lower scores in WLG KAS, no significant differences were found in psychopathology and cognitive functioning between the groups (Table 3).
Discussion
The results of this study showed that patients with mild autonomous cortisol secretion and patients with active Cushing’s syndrome had significantly smaller volumes of the left whole thalamus, left posterior thalamic nuclei, left medial thalamic nuclei, and right lateral thalamic nuclei in relation to control subjects. The absolute volumes of the thalamus and thalamic subregions were more severely affected in patients with active Cushing’s syndrome and less severely affected in patients with Cushing’s syndrome in remission as compared to patients with mild autonomous cortisol secretion. Albeit the patients with mild autonomous cortisol secretion and patients with active Cushing’s syndrome performed relatively worse in verbal fluency, the cognitive functions were comparable between the study groups.
It is acknowledged that overt CS is associated with reduced thalamic volume. The thalamic changes caused by overt CS might not be reversible despite treatment [22, 54-56]. It is therefore important to detect the thalamic detriment as early as possible. Contrary to overt CS, the effects of MACS on thalamic volume have been overlooked. Given the broad range of neurotoxic effects of increased cortisol [4, 57-59], we speculated that chronic exposure to low-grade hypercortisolism could also reduce thalamic volume as overt hypercortisolism. We confirmed our hypothesis. Understanding the effects of MACS on thalamic volumes is of value for several reasons. Firstly, it can be inferred that even a low grade of cortisol excess may be capable of inducing structural thalamic alterations. We can also conclude that structural thalamic alterations may present even in the absence of overt signs of hypercortisolism.
A major drawback of the previous studies exploring the effect of hypercortisolism on the brain was that they have considered the thalamus as a single anatomical structure and reported an overall change in thalamic volume [22, 54-56]. Nonetheless, the thalamus has several anatomical subregions with each connected with specific basal ganglia and cortical regions. This structural organization determines the unique function of each thalamic subregion [60-65]. Given this structural and functional thalamic heterogeneity, we speculated that more detailed segmentation of the thalamus might capture more structural alterations. Our results indicate that MACS might relate to selective volumetric changes of posterior, medial, and lateral thalamic nuclei in addition to the whole thalamus. In animal models, the nuclei in the posterior, medial, and lateral thalamus have been shown to have moderate-to-high densities of GR mRNA-containing cells [66]. The increased density of the GR in these thalamic subregions might have rendered these nuclei groups particularly susceptible to the effects of long-standing subtle hypercortisolism also in humans.
We have also reported reductions in the volumes of the left pulvinar, left MDl, and left MDm in patients with MACS in relation to controls. The pulvinar is one of the higher-order thalamic nuclei that has extensive connections with several brain regions and comprises approximately one-third of the whole thalamus [25, 67-69]. As is true for pulvinar, MD nuclei have diverse connections with other parts of the brain [70]. The importance of MD and pulvinar nuclei in cognition is rooted in these connections. The reduced volumes of the left-sided thalamic nuclei might have particular relevance in cognitive functions. Previously, left thalamic lesions have been specifically associated with impaired verbal fluency [71]. In the present study, although inter-group comparisons of cognitive function tests showed no significant difference, relatively low absolute scores of WLG KAS in the MACS group in relation to the control group could be partly explained by alterations of thalamic nuclei clustered in the left side. Nevertheless, in the absence of strong evidence, the results of the present study might indicate a dissociation between function and structure of these subcortical nuclei and is subject to further investigation.
Another unique asset of the current study was that it provided the first piece of evidence regarding structural abnormalities in thalamic subregions in addition to the whole thalamus in patients with CS. Similar to the patients with MACS, the results of the volumetric analyses indicated that patients with active CS also had smaller volumes of the whole thalamus and the posterior, medial, and lateral thalamic nuclei than controls. The shared structural abnormalities of these thalamic subregions further supported their particular vulnerability to glucocorticoid excess. Given the longer disease duration in patients with MACS in comparison to patients with active CS in our study sample, another interpretation might be that exposure to the long duration of mild hypercortisolism has induced the same thalamic alterations as in the relatively shorter duration of severe hypercortisolism. It is noteworthy to mention that the increased prevalence of diabetes mellitus and hypertension in patient groups might have also contributed to structural changes. Contrary to patients with active CS, the structural alterations of the thalamus and its subregions were less evident in patients with CS in remission in comparison to patients with active CS. These findings were in agreement with the previous reports indicating the partial reversibility of the structural brain alterations upon correction of the hypercortisolism [72].
The influence of the degree of cortisol secretion on cognitive functions has been proposed to be a complex phenomenon, mimicking an inverted U-shaped dose–response curve [73]. According to this hypothesis, mild hypercortisolism corresponds to the central, optimal range of the curve, causing positive hyperactivity of the central nervous system [74-78]. This was supported by a previous study where the authors found a better performance of patients with MACS in cognition as compared to controls [79]. Contrarily, a recent study reported impaired cognitive functions in patients with MACS [80]. The findings of our study suggested no significant difference in various items of cognitive function between MACS and the control group. Taken together, it can be argued that data regarding the effects of MACS on cognition is conflicting. We also did not observe a significant difference in cognitive functions between patients with CS and control subjects which was not in line with the quite extensive previous literature. This may have several explanations. Although all the questionnaires used for the assessment of cognitive functioning in the present study have been validated repeatedly, there is no substitute for extensive neuropsychological testing which might have to delineate more subtle changes and therefore provide a more accurate representation of cognitive functioning. Furthermore, given the trend for lower absolute scores in the language domain of cognition in patients with active CS and MACS as compared to control subjects, analyses of a larger sample size might have yielded a significant difference between groups. Another alternative explanation could be that a greater change in the thalamic volume might be required for the cognitive impairment to become detectable by the questionnaires used in this study.
The impact of CS on hippocampal volume has been of special interest due to its high density of GR and important roles in cognitive functions [10, 20, 81]. Although a number of studies demonstrated hippocampal volume loss in patients with CS, a recent meta-analysis of 18 studies did not detect any strong evidence of reduced hippocampal volumes related to CS [10, 12, 20]. This was consistent with the results of the present study. Contrary to CS, the effect of MACS on hippocampal volume has never been assessed before. Our study did not suggest an overall reduction of hippocampal volume in patients with MACS or CS relative to control subjects. Based on previous reports, it can be speculated that our results concerning the hippocampal volumes might have been underpowered by the relatively small size of the control group [82]. Toward this end, the comparable hippocampus volumes between our study groups should be cautiously judged.
In the present study, the clear-cut lateralized effect of hypercortisolism on thalamic volumes was noteworthy. This finding was consistent with preliminary evidence, suggesting an inverse relation of plasma cortisol with left thalamic volume [83]. One speculation for this observation is that GR and/or MR may be more densely expressed in the left thalamus in comparison to the right thalamus. Another possible explanation for the laterality might indeed be related to the unique features of our patient groups. The studies that suggested bilateral rather than unilateral thalamic changes included homogenous patient groups that were purely composed of patients with CD [22, 84, 85]. However, we included patients with hypercortisolism, either of pituitary or non-pituitary origin, which rendered our sample a bit heterogeneous. Volumetric analysis of a homogenous patient group might have yielded bilateral thalamic changes. It is also important to note that the patients included in the present study were approximately 10 years older than patients included in other studies which reported bilateral thalamic changes [22, 84, 85]. Previously, a regional-specific reduction in GRs in the brain during aging has been speculated [86]. In other words, the excess cortisol may have differential effects on specific regions as the patient ages. Therefore, left-sided thalamic changes in our study population may be explained by side-specific reduction of thalamic GRs related to aging. We also acknowledge that different functional and/or neurobiological alterations in thalamic hemispheres in response to cortisol excess might also play a role in laterality to some extent. But nevertheless, all of these suggestions are deeply hypothetical and require more empirical studies to confirm.
The present study has limitations. The small sample size, which is an unavoidable challenge to rare diseases such as CS, might have prevented to detect the anticipated changes in cognitive functions. Furthermore, a longitudinal design with an observation period of at least one year would have better identified the progress of the structural alterations of the brain and evaluated if these alterations translate into cognitive deficits in time [7, 11]. A larger sample size and prospective follow-up would also have provided more robust evidence concerning the laterality difference in thalamic volume. Exploring the functional brain characteristics with the help of functional MRI would have shed more light on the impact of the MACS on the cortex and will be our next important step.
Conclusion
The knowledge about the structural brain alterations related to MACS is almost lacking. The present exploratory study provided the first piece of evidence on the role of MACS on brain volumes. We revealed that exposure to even a mild degree of endogenous cortisol secretion could elicit structural alterations in the whole thalamus. We also showed that some thalamic nuclei may be more vulnerable to mild cortisol secretion. MACS-related structural alterations of the brain should merit further investigation.
References
Nieman LK, Chrousos GP, Kellner C et al (1985) Successful treatment of Cushing’s syndrome with the glucocorticoid antagonist RU 486. J Clin Endocrinol Metab 61:536–540
De Kloet E (2005) Joels M, Holsboer F. Nat Rev Neurosci 6:463
Momose KJ, Kjellberg RN, Kliman B (1971) High incidence of cortical atrophy of the cerebral and cerebellar hemispheres in Cushing’s disease. Radiology 99:341–348
De Kloet ER, Vreugdenhil E, Oitzl MS et al (1998) Brain corticosteroid receptor balance in health and disease. Endocr Rev 19:269–301
Starkman MN, Giordani B, Gebarski SS et al (1999) Decrease in cortisol reverses human hippocampal atrophy following treatment of Cushing’s disease. Biol Psychiat 46:1595–1602
Starkman MN, Gebarski SS, Berent S et al (1992) Hippocampal formation volume, memory dysfunction, and cortisol levels in patients with Cushing’s syndrome. Biol Psychiat 32:756–765
Starkman MN, Giordani B, Gebarski SS et al (2007) Improvement in mood and ideation associated with increase in right caudate volume. J Affect Disord 101:139–147
Santos A, Resmini E, Crespo I et al (2014) Small cerebellar cortex volume in patients with active Cushing’s syndrome. Eur J Endocrinol 171:461–469
Andela CD, Van der Werff S, Pannekoek JN et al (2013) Smaller grey matter volumes in the anterior cingulate cortex and greater cerebellar volumes in patients with long-term remission of Cushing’s disease: a case-control study. Eur J Endocrinol 169:811–819
Frimodt-Møller KE, Møllegaard Jepsen JR, Feldt-Rasmussen U et al (2019) Hippocampal volume, cognitive functions, depression, anxiety, and quality of life in patients with Cushing syndrome. J Clin Endocrinol Metab 104:4563–4577
Hook JN, Giordani B, Schteingart DE et al (2007) Patterns of cognitive change over time and relationship to age following successful treatment of Cushing’s disease. J Int Neuropsychol Soc 13:21–29
Resmini E, Santos A, Gomez-Anson B et al (2012) Verbal and visual memory performance and hippocampal volumes, measured by 3-Tesla magnetic resonance imaging, in patients with Cushing’s syndrome. J Clin Endocrinol Metab 97:663–671
Reincke M (2000) Subclinical Cushing’s syndrome. Endocrinol Metab Clin North Am 29:43–56
Terzolo M, Bovio S, Reimondo G et al (2005) Subclinical Cushing’s syndrome in adrenal incidentalomas. Endocrinol Metab Clin 34:423–439
Chiodini I (2011) Diagnosis and treatment of subclinical hypercortisolism. J Clin Endocrinol Metab 96:1223–1236
Di Dalmazi G, Vicennati V, Garelli S et al (2014) Cardiovascular events and mortality in patients with adrenal incidentalomas that are either non-secreting or associated with intermediate phenotype or subclinical Cushing’s syndrome: a 15-year retrospective study. Lancet Diabetes Endocrinol 2:396–405
Di Dalmazi G, Vicennati V, Rinaldi E et al (2012) Progressively increased patterns of subclinical cortisol hypersecretion in adrenal incidentalomas differently predict major metabolic and cardiovascular outcomes: a large cross-sectional study. Eur J Endocrinol 166:669–677
Nieman LK (2015) Update on subclinical Cushing’s syndrome. Curr Opin Endocrinol Diabetes Obes 22:180–184
Starkman M (1999) Giordani B, Gebarski SS, Berent S, Schork MA, and Schteingart DE. Decrease in cortisol reverses human hippocampal atrophy following treatment of Cushing’s disease Biol Psychiatry 46:1595–1602
Starkman MN, Giordani B, Gebarski SS et al (2003) Improvement in learning associated with increase in hippocampal formation volume. Biol Psychiat 53:233–238
Andela CD, van Haalen FM, Ragnarsson O et al (2015) Mechanisms in endocrinologY: Cushing’s syndrome causes irreversible effects on the human brain: a systematic review of structural and functional magnetic resonance imaging studies. Eur J Endocrinol 173:R1–R14
Jiang H, Yang W, Sun Q et al (2021) Trends in regional morphological changes in the brain after the resolution of hypercortisolism in Cushing’s disease: a complex phenomenon, not mere partial reversibility. Endocr Connect 10:1377–1386
Tirosh A, RaviPrakash H, Papadakis GZ et al (2020) Computerized analysis of brain MRI parameter dynamics in young patients with Cushing syndrome—a case-control study. J Clin Endocrinol Metab 105:e2069–e2077
Giraldo-Chica M, Woodward ND (2017) Review of thalamocortical resting-state fMRI studies in schizophrenia. Schizophr Res 180:58–63
Halassa MM, Kastner S (2017) Thalamic functions in distributed cognitive control. Nat Neurosci 20:1669–1679
Association AD (2020) 6. Glycemic targets: standards of medical care in diabetes-2020. Diabetes Care 43:S66–S76
James PA, Oparil S, Carter BL et al (2014) 2014 Evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 311:507–520
Fassnacht M, Arlt W, Bancos I et al (2016) Management of adrenal incidentalomas: European Society of Endocrinology Clinical Practice Guideline in collaboration with the European Network for the Study of Adrenal Tumors. Eur J Endocrinol 175:G1-g34
Bancos I, Prete A (2021) Approach to the patient with adrenal incidentaloma. J Clin Endocrinol Metab 106:3331–3353
Nieman LK, Biller BMK, Findling JW et al (2008) The diagnosis of Cushing’s syndrome: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 93:1526–1540
Fleseriu M, Hashim IA, Karavitaki N et al (2016) Hormonal replacement in hypopituitarism in adults: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 101:3888–3921
Nieman LK, Biller BM, Findling JW et al (2015) Treatment of Cushing’s syndrome: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 100:2807–2831
Molitch ME, Clemmons DR, Malozowski S et al (2011) Evaluation and treatment of adult growth hormone deficiency: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 96:1587–1609
Ségonne F, Dale AM, Busa E et al (2004) A hybrid approach to the skull stripping problem in MRI. Neuroimage 22:1060–1075
Fischl B, Salat DH, van der Kouwe AJ et al (2004) Sequence-independent segmentation of magnetic resonance images. Neuroimage 23(Suppl 1):S69-84
Fischl B, Salat DH, Busa E et al (2002) Whole brain segmentation: automated labeling of neuroanatomical structures in the human brain. Neuron 33:341–355
Fischl B, Liu A, Dale AM (2001) Automated manifold surgery: constructing geometrically accurate and topologically correct models of the human cerebral cortex. IEEE Trans Med Imaging 20:70–80
Ségonne F, Pacheco J, Fischl B (2007) Geometrically accurate topology-correction of cortical surfaces using nonseparating loops. IEEE Trans Med Imaging 26:518–529
Fischl B, Dale AM (2000) Measuring the thickness of the human cerebral cortex from magnetic resonance images. Proc Natl Acad Sci U S A 97:11050–11055
Sled JG, Zijdenbos AP, Evans AC (1998) A nonparametric method for automatic correction of intensity nonuniformity in MRI data. IEEE Trans Med Imaging 17:87–97
Fischl B, Sereno MI, Dale AM (1999) Cortical surface-based analysis. II: Inflation, flattening, and a surface-based coordinate system. Neuroimage 9:195–207
Desikan RS, Ségonne F, Fischl B et al (2006) An automated labeling system for subdividing the human cerebral cortex on MRI scans into gyral based regions of interest. Neuroimage 31:968–980
Iglesias JE, Augustinack JC, Nguyen K et al (2015) A computational atlas of the hippocampal formation using ex vivo, ultra-high resolution MRI: application to adaptive segmentation of in vivo MRI. Neuroimage 115:117–137
Iglesias JE, Insausti R, Lerma-Usabiaga G et al (2018) A probabilistic atlas of the human thalamic nuclei combining ex vivo MRI and histology. Neuroimage 183:314–326
Beck AT, Epstein N, Brown G et al (1988) An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol 56:893
Nasreddine ZS, Phillips NA, Bédirian V et al (2005) The Montreal cognitive assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc 53:695–699
Kang JM, Cho YS, Park S et al (2018) Montreal cognitive assessment reflects cognitive reserve. BMC Geriatr 18:261
Buschke H (1973) Selective reminding for analysis of memory and learning. J Verbal Learn Verbal Behav 12:543–550
Larrabee GJ, Trahan DE, Levin HS (2000) Normative data for a six-trial administration of the verbal selective reminding test. Clin Neuropsychol 14:110–118
Rao SM, Leo GJ, Bernardin L et al (1991) Cognitive dysfunction in multiple sclerosis. I. Frequency, patterns, and prediction. Neurology 41:685–691
CAMPBELL JR AL, Bogen JE, Smith A, (1981) Disorganization and reorganization of cognitive and sensorimotor functions in cerebral commissurotomy: compensatory roles of the forebrain commissures and cerebral hemispheres in man. Brain 104:493–511
Boringa JB, Lazeron RH, Reuling IE et al (2001) The brief repeatable battery of neuropsychological tests: normative values allow application in multiple sclerosis clinical practice. Mult Scler 7:263–267
Sanfilipo MP, Benedict RH, Zivadinov R et al (2004) Correction for intracranial volume in analysis of whole brain atrophy in multiple sclerosis: the proportion vs. residual method. Neuroimage 22:1732–1743
Jiang H, He NY, Sun YH et al (2017) Altered spontaneous brain activity in Cushing’s disease: a resting-state functional MRI study. Clin Endocrinol 86:367–376
Khiat A, Yared Z, Bard C et al (2001) Long-term brain metabolic alterations in exogenous Cushing’s syndrome as monitored by proton magnetic resonance spectroscopy. Brain Res 911:134–140
Khiat A, Bard C, Lacroix A et al (1999) Brain metabolic alterations in Cushing’s syndrome as monitored by proton magnetic resonance spectroscopy. NMR in Biomedicine: an International Journal Devoted to the Development and Application of Magnetic Resonance In Vivo 12:357–363
McEwen BS, Sapolsky RM (1995) Stress and cognitive function. Curr Opin Neurobiol 5:205–216
Sapolsky RM (1994) The physiological relevance of glucocorticoid endangerment of the hippocampus a. Ann N Y Acad Sci 746:294–304
Tjuvajev J, Uehara H, Desai R et al (1996) Corticotropin-releasing factor decreases vasogenic brain edema. Can Res 56:1352–1360
Golden EC, Graff-Radford J, Jones DT et al (2016) Mediodorsal nucleus and its multiple cognitive functions. Neurology 87:2161–2168
Shine JM, Hearne LJ, Breakspear M et al (2019) The low-dimensional neural architecture of cognitive complexity is related to activity in medial thalamic nuclei. Neuron 104:849-855.e843
Van der Werf YD, Jolles J, Witter MP et al (2003) Contributions of thalamic nuclei to declarative memory functioning. Cortex 39:1047–1062
Zhou H, Schafer RJ, Desimone R (2016) Pulvinar-cortex interactions in vision and attention. Neuron 89:209–220
Mitchell AS, Chakraborty S (2013) What does the mediodorsal thalamus do? Front Syst Neurosci 7:37
Hong W, Li M, Liu Z et al (2021) Heterogeneous alterations in thalamic subfields in major depression disorder. J Affect Disord 295:1079–1086
Morimoto M, Morita N, Ozawa H et al (1996) Distribution of glucocorticoid receptor immunoreactivity and mRNA in the rat brain: an immunohistochemical and in situ hybridization study. Neurosci Res 26:235–269
Sherman SM (2007) The thalamus is more than just a relay. Curr Opin Neurobiol 17:417–422
Benarroch EE (2015) Pulvinar: associative role in cortical function and clinical correlations. Neurology 84:738–747
Robinson DL, Petersen SE (1992) The pulvinar and visual salience. Trends Neurosci 15:127–132
Goldman-Rakic PS, Porrino LJ (1985) The primate mediodorsal (MD) nucleus and its projection to the frontal lobe. J Comp Neurol 242:535–560
Schmahmann JD (2003) Vascular syndromes of the thalamus. Stroke 34:2264–2278
Andela CD, Van Haalen FM, Ragnarsson O et al (2017) Cushing’s syndrome causes irreversible effects on the human brain: a systematic review of structural and functional MRI studies. Eur J Endocrinol 173:R1–R14
Chrousos GP (2009) Stress and disorders of the stress system. Nat Rev Endocrinol 5:374–381
Baker S, Rogers R, Owen AM et al (1996) Neural systems engaged by planning: a PET study of the Tower of London task. Neuropsychologia 34:515–526
Gaillard WD, Hertz-Pannier L, Mott SH et al (2000) Functional anatomy of cognitive development: fMRI of verbal fluency in children and adults. Neurology 54:180–180
Rossi AF, Pessoa L, Desimone R et al (2009) The prefrontal cortex and the executive control of attention. Exp Brain Res 192:489–497
Pivonello R, Simeoli C, De Martino M, et al (2015) Neuropsychiatric disorders in Cushing’s syndrome. Front Neurosci 9 129
Tiemensma J, Andela CD, Biermasz NR et al (2016) Mild cognitive deficits in patients with primary adrenal insufficiency. Psychoneuroendocrinology 63:170–177
Morelli V, Ghielmetti A, Caldiroli A et al (2021) Mental health in patients with adrenal incidentalomas: is there a relation with different degrees of cortisol secretion? J Clin Endocrinol Metab 106:e130–e139
Liu MS, Tian ZY, Zhang Z, et al (2022) Impaired cognitive function in patients with autonomous cortisol secretion in adrenal incidentalomas. J Clin Endocrinol Metab
Lupien SJ, De Leon M, De Santi S et al (1998) Cortisol levels during human aging predict hippocampal atrophy and memory deficits. Nat Neurosci 1:69–73
Pell GS, Briellmann RS, Chan CHP et al (2008) Selection of the control group for VBM analysis: influence of covariates, matching and sample size. Neuroimage 41:1324–1335
Buhl CS, Stødkilde-Jørgensen H, Videbech P et al (2018) Escitalopram ameliorates hypercortisolemia and insulin resistance in low birth weight men with limbic brain alterations. J Clin Endocrinol Metab 103:115–124
Jiang H, He NY, Sun YH et al (2017) Altered spontaneous brain activity in Cushing’s disease: a resting-state functional MRI study. Clin Endocrinol (Oxf) 86:367–376
Zhang Y, Zhou T, Feng S et al (2021) The chronic effect of cortisol on orchestrating cerebral blood flow and brain functional connectivity: evidence from Cushing’s disease. Metabolism 115:154432
Lau WKW, Leung MK, Law ACK et al (2017) Moderating effects of cortisol on neural-cognitive association in cognitively normal elderly subjects. Front Aging Neurosci 9:163
Funding
This study was funded by The Scientific and Technological Research Council of Turkiye (Project No: 220S794).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The present study was approved by the Medical Research Ethics Committee of Cerrahpasa Medical Faculty (03.05.2021/45781).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file2 (MP4 2734 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sulu, C., Koca, O., Icli, T.B. et al. Altered thalamic volume in patients with mild autonomous cortisol secretion: a structural brain MRI study. Neuroradiology 65, 1037–1051 (2023). https://doi.org/10.1007/s00234-023-03156-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-023-03156-3