Abstract
Purpose
Acute, isolated intracranial dissection (ICD) represents a rare and challenging cause of acute stroke. DSA is considered to be the gold standard imaging modality in patients with ICD. The role of novel, high-resolution (HR) compressed-sensing (CS) time-of-flight (TOF) MRA techniques in ICDs is unclear.
Methods
A 22-year-old male patient with an isolated right ICA/MCA intracranial dissection underwent “conventional” 3-T TOF MRA, HR CS TOF MRA and also DSA including digital rotational angiography.
Results
Unlike the “conventional” TOF MRA, HR CS TOF MRA provided comparable image quality to rotational angiography and a dissection membrane was clearly visible in both techniques.
Conclusion
In this single case study, we demonstrated the feasibility of a novel HR CS TOF in a case of an acute isolated intracranial ICA/MCA dissection, which needs to be validated in a larger case series.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Acute, isolated intracranial dissection (ICD) represents a rare and both diagnostically and therapeutically challenging cause of acute stroke. Compared with extracranial artery dissection, patients may present with not only ischemic stroke but also acute SAH, if the dissection involves the media/adventitia interface [1].
From the diagnostic point of view, current imaging techniques are often insufficient in demonstrating vessel wall hematoma and intimal flaps, as being commonly seen in extracranial artery dissections (ECDs). Beyond that, some of the imaging features commonly used to define cranial dissections are non-specific [2]. Currently, there is no evidence-based treatment strategy available. Therapeutic options include i.v. thrombolysis, angioplasty/stent, and antiaggregant therapy.
Acute anterior circulation ICD often involves the supraclinoid ICA segment, which represents the most common location of ICD [1]. Patients typically present with severe pain in the ipsilateral eye, forehead, and temple, often followed by acute contralateral hemiparesis [3]. Involvement of the proximal MCA and ACA segments has been described, especially in children.
Case report
A 22-year-old male suffered an acute stroke involving right-sided orbital pain and left-sided hemiparesis while skateboarding, without an obvious preceding fall/concussion.
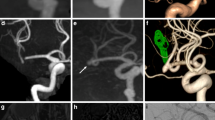
Non-contrast CT was unremarkable and CTA showed slight narrowing of the right terminal ICA segment (Fig. 1a). As an acute ischemic stroke was highly suspected with a persisting high NIHSS score (9), MRI was performed involving a parallel imaging 3D time-of-flight (TOF) MRA (in-plane resolution 0.5 × 0.5 mm, slice thickness 0.5 mm) acquired using a standard 20-channel head coil (3-T Siemens MAGNETOM Skyra). As only non-specific lumen ICA/M1 narrowing was detectable (Fig. 1b) and clinically an acute intracranial dissection was suspected, we performed a high-resolution (“HR”, in-plane resolution 0.27 × 0.4, slice thickness 0.3 mm; voxel size 0.03 mm3; TR 22.2 TE 4.1; PAT 6.3; acquisition time 5:54 min) compressed-sensing time-of-flight (TOF) MRA (Fig. 1c, e) [3] using a 64-channel head-neck coil (3-T Siemens MAGNETOM Prisma), which clearly verified a dissection flap extending from the ophthalmic ICA segment to the mid-M1 segment. Non-contrast black-blood imaging showed no intramural hematoma and no pathological vessel wall enhancement at the level of the stenosis. An inflammatory vasculopathy could not be corroborated neither clinically nor by CSF analysis.
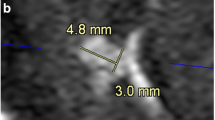
Acute right ICA/MCA dissection, perforator artery stroke, and upstream concentric vessel wall enhancement. a Initial CTA demonstrates subtle narrowing of the right ICA terminus (arrow). Comparison of standard time-of-flight MRA (b, axial plane) and high-resolution compressed-sensing time-of-flight MRA (c axial plane, E 3D maximum intensity projection (MIP)), revealing (c, arrow) a thin dissecting flap and double-lumen sign extending from the opthalmic ICA to the right M1 segment causing e a long irregular stenosis. d Diffusion-weighted MRI shows extensive right basal ganglia perforator and anterior choroideal artery infarctions. Neither a vessel wall hematoma nor a vasculitis-typical vascular wall enhancement was detectable on high-resolution black-blood post-contrast 3D T1w vessel wall imaging f
MRI findings were later confirmed with DSA and digital rotational angiography (Dyna-CT; Fig. 2).
Dyna-CT (a, b axial recons) and DSA (c, lateral) confirming intimal flap in the right cavernous/terminal ICA (c, arrows) and double lumen in a the right MCA M1 segment and b carotid terminus. Interestingly, the intimal flap in the M1 segment is barely visible on Dyna-CT (a, arrow) but clearly delimitable on HR CS TOF MRA (see Fig. 1c, arrow)
Discussion
Our case fulfills current diagnostic criteria of an acute ICD [4] as an intimal flap and double lumen were clearly demonstrated by using a novel TOF-MRA technique.
Parallel imaging is commonly being used for k-space undersampling during acquisition of TOF MRA, but acceleration factors are usually limited to 2× to 3×, as noise and aliasing rapidly increase at higher acceleration factors. Compressed sensing exploits the underlying sparsity in the appropriate transform domain and by that allows for higher acceleration factors and improved image quality at acceptable acquisition time [5,6,7,8,9]. Furthermore, vessel wall imaging using T1w post-contrast imaging benefits from higher spatial coverage an potential 3D reformatability, if current CS technique is being used [10, 11].
CS TOF MRA has recently been evaluated in 7-T MRA [4] and also been used to shorten the time of examination at constant resolution or to increase the resolution at (conventional TOF MRA) constant examination time [5, 6, 12]. CS TOF techniques have also been evaluated in different vessel pathologies as, e.g., vessel stenosis [7, 8] and aneurysms [9].
DSA is considered to be the gold standard imaging modality in patients with ICD. Stroke-related complications during DSA are reported to occur in about 1% of cases, which has for example led to TOF MRA becoming the primary modality for post-coiling aneurysm follow-up. The use of CT is limited on the one hand by the achievable resolution and on the other hand by associated (potentially high) radiation dose. The role of different MRA techniques in ICD is unclear and most studies lack a comparable imaging standard.
Our modified 3-T HR CS TOF MRA delivered comparable image quality to Dyna-CT as intimal flap and double lumen were clearly demonstrated. Thus, we hypothesize that 3-T HR CS TOF MRA constitutes an ideal contrast-free method to clarify patients with suspected intracranial dissection or dissecting aneurysm. In addition, this technique also appears to be suitable for monitoring patients with known intracranial dissection with regard to the degree of luminal stenosis and extent of dissection, as frequently a secondary increase of the degree of stenosis may occur.
The value of the CS TOF-MRA technique should be further validated in a larger case series. Considering the rarity of ICD, the role of not only advanced (compressed-sensing) MRI techniques but also medical and endovascular treatments remains to be further elucidated, ideally in a prospective multicentric approach.
Conclusion
3-T high-resolution compressed-sensing time-of-flight (TOF) MRA was in this case of an isolated intracranial dissection superior to conventional TOF MRA and not inferior to Dyna-CT in demonstrating an intimal flap in the right MCA M1 segment. This novel, clinically available technique can demonstrate specific findings of an ICD, which may otherwise require more invasive DSA and thus has the potential to improve the diagnostic specificity in patients presenting with acute intracranial arteriopathy.
References
Caplan LR (2008) Dissections of brain-supplying arteries. Nat Clin Pract Neurol 4:34–42. https://doi.org/10.1038/ncpneuro0683
Debette S, Compter A, Labeyrie M, Uyttenboogaart M, Metso TM, Majersik JJ, Goeggel-Simonetti B, Engelter ST, Pezzini A, Bijlenga P, Southerland AM, Naggara O, Béjot Y, Cole JW, Ducros A, Giacalone G, Schilling S, Reiner P, Sarikaya H, Welleweerd JC, Kappelle LJ, de Borst GJ, Bonati LH, Jung S, Thijs V, Martin JJ, Brandt T, Grond-Ginsbach C, Kloss M, Mizutani T, Minematsu K, Meschia JF, Pereira VM, Bersano A, Touzé E, Lyrer PA, Leys D, Chabriat H, Markus HS, Worrall BB, Chabrier S, Baumgartner R, Stapf C, Tatlisumak T, Arnold M, Bousser MG (2015) Epidemiology, pathophysiology, diagnosis, and management of intracranial artery dissection. Lancet Neurol 14:640–654. https://doi.org/10.1016/S1474-4422(15)00009-5
Chaves C, Estol C, Esnaola MM, Gorson K, O’Donoghue M, De Witt LDCL (2002) Spontaneous intracranial internal carotid artery dissection: report of 10 patients. Arch Neurol 59:977–981
Meixner CR, Liebig P, Speier P, Forman C, Hensel B, Schmidt M, Saake M, Uder M, Doerfler A, Heidemann RM, Schmitter S, Nagel AM (2019) High resolution time-of-flight MR-angiography at 7 T exploiting VERSE saturation, compressed sensing and segmentation. Magn Reson Imaging 63:193–204. https://doi.org/10.1016/J.MRI.2019.08.014
Mönch S, Sollmann N, Hock A, Zimmer C, Kirschke JS, Hedderich DM (2019) Magnetic resonance imaging of the brain using compressed sensing – quality assessment in daily clinical routine. Clin Neuroradiol. https://doi.org/10.1007/s00062-019-00789-x
Greve T, Sollmann N, Hock A, Hey S, Gnanaprakasam V, Nijenhuis M, Zimmer C, Kirschke JS (2019) Highly accelerated time-of-flight magnetic resonance angiography using spiral imaging improves conspicuity of intracranial arterial branches while reducing scan time. Eur Radiol 30:855–865. https://doi.org/10.1007/s00330-019-06442-y
Lu SS, Qi M, Zhang X et al (2018) Clinical evaluation of highly accelerated compressed sensing time-of-flight MR angiography for intracranial arterial stenosis. Am J Neuroradiol 39:1833–1838. https://doi.org/10.3174/ajnr.A5786
Yamamoto T, Okada T, Fushimi Y et al (2018) Magnetic resonance angiography with compressed sensing : an evaluation of moyamoya disease. PLoS One 13:e0189493. https://doi.org/10.1371/journal.pone.0189493
Fushimi Y, Fujimoto K, Okada T, Yamamoto A, Tanaka T, Kikuchi T, Miyamoto S, Togashi K (2016) Compressed sensing 3-dimensional time-of-flight magnetic resonance angiography for cerebral aneurysms: optimization and evaluation. Investig Radiol 51:228–235. https://doi.org/10.1097/RLI.0000000000000226
Eiden S, Beck C, Venhoff N et al (2019) High-resolution contrast-enhanced vessel wall imaging in patients with suspected cerebral vasculitis: prospective comparison of wholebrain 3D T1 SPACE versus 2D T1 black blood MRI at 3 Tesla. PLoS One 14:1–14. https://doi.org/10.1371/journal.pone.0213514
Guggenberger K, Krafft AJ, Ludwig U, Vogel P, Elsheik S, Raithel E, Forman C, Dovi-Akué P, Urbach H, Bley T, Meckel S (2019) High-resolution compressed-sensing T1 black-blood MRI: a new multipurpose sequence in vascular neuroimaging? Clin Neuroradiol. https://doi.org/10.1007/s00062-019-00867-0
Lin Z, Zhang X, Guo L, Wang K, Jiang Y, Hu X, Huang Y, Wei J, Ma S, Liu Y, Zhu L, Zhuo Z, Liu J, Wang X (2019) Clinical feasibility study of 3D intracranial magnetic resonance angiography using compressed sensing. J Magn Reson Imaging 50:1843–1851. https://doi.org/10.1002/jmri.26752
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in the studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Demerath, T., Bonati, L., El Mekabaty, A. et al. High-resolution compressed-sensing time-of-flight MRA in a case of acute ICA/MCA dissection. Neuroradiology 62, 753–756 (2020). https://doi.org/10.1007/s00234-020-02395-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-020-02395-y