Abstract
Introduction
Superficial siderosis is presumably a consequence of recurrent bleeding into the subarachnoid space. The objective of this study was to assess the prevalence of superficial siderosis after singular, aneurysmal subarachnoid hemorrhage (SAH) in the long term.
Methods
We retrospectively identified all patients who presented with a singular, acute, aneurysmal SAH at our institution between 2010 and 2013 and in whom a magnetic resonance imaging (MRI) including T2*-weighted imaging was available at least 4 months after the acute bleeding event. MRI scans were judged concerning the presence and distribution of superficial siderosis. Influence of clinical data, Fisher grade, localization, and cause of SAH as well as the impact of neurosurgical interventions on the occurrence of superficial siderosis was tested.
Results
Seventy-two patients with a total of 117 MRIs were included. Mean delay between SAH and the last available MRI was 47.4 months (range 4–129). SAH was Fisher grade 1 in 2 cases, 2 in 4 cases, 3 in 10 cases, and 4 in 56 cases. Superficial siderosis was detected in 39 patients (54.2 %). In all patients with more than one MRI scan, localization and distribution of superficial siderosis did not change over time. Older age (p = 0.02) and higher degree of SAH (p = 0.03) were significantly associated with the development of superficial siderosis.
Conclusion
Superficial siderosis develops in approximately half of patients after singular, aneurysmal SAH and might be more common in patients with an older age and a greater amount of blood. However, additional factors must play a role in whether a patient is prone to develop superficial siderosis or not.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Superficial siderosis is defined as linear residues of blood degradation products in the superficial layers of the brain, spinal cord, and central parts of the cranial nerves. Magnetic resonance imaging (MRI) is the investigation of choice for the diagnosis of superficial siderosis in vivo [1, 2]. Due to the magnetic susceptibility effects of blood degradation products such as ferritin and hemosiderin, gradient-echo T2*-weighted sequences and susceptibility-weighted imaging (SWI) are best suited to delineate these deposits.
Regarding their clinical presentation and anatomical distribution, basically two different types of intracranial superficial siderosis are distinguished in literature to date. The “classical” superficial siderosis of the central nervous system (CNS) presents with slowly progressive gait ataxia with cerebellar dysarthria and sensorineural hearing impairment and mainly affects the brain stem and posterior fossa and is therefore also referred to as “infratentorial siderosis” [2]. A clinical history of symptomatic subarachnoid hemorrhage (SAH) is often not present in these patients [2]. The second type of intracranial superficial siderosis, the so-called cortical superficial siderosis, exclusively affects the supratentorial compartment, i.e., the cerebral convexities. Cerebral amyloid angiopathy (CAA) is considered the most common cause of this type of siderosis in elderly individuals, while reversible cerebral vasoconstriction syndrome is most frequently identified as an underlying cause in patients under the age of 60 years [3, 4]. Patients with cortical superficial siderosis characteristically present with transient focal neurological deficits [5] and or cognitive impairment [6].
To date, the detailed pathomechanism of intracranial superficial siderosis formation is not yet understood. In animal models, the classical, infratentorial form of siderosis develops after repeated intracisternal injections of autologous red blood cells or iron dextran [7]. Regarding the pathomechanism of cortical superficial siderosis, the second major type of intracranial siderosis, similar studies are lacking, but a comparable mechanism with recurrent bleeding into the subarachnoid space is widely thought to be responsible also in these cases.
Here, we aimed to address the question whether repeated and/or chronic SAHs are indeed required for siderosis formation in humans or if, and under which circumstances, siderosis might also occur after a singular episode of SAH as typically present in patients with an acute aneurysmal SAH.
Materials and methods
We declare that the study was approved by our Institutional Review Board and has therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. We declare that all patients gave informed consent prior to inclusion in this study.
Patient selection
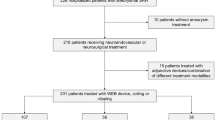
We included all patients who presented with a singular, acute, aneurysmal SAH at our institution between 2010 and 2013 and in whom an MRI, at least 4 months after the acute bleeding event, was available. To identify those patients, we searched our electronic in-hospital database of clinical records for the key words “subarachnoid hemorrhage,” “SAH,” “CT,” and “MRI.”
Inclusion criteria were as follows:
-
(1)
Acute, aneurysmal SAH diagnosed according to clinical presentation, cranial computed tomography (CCT), and/or cerebral spinal fluid (CSF)
-
(2)
Initial CCT performed within 48 h of clinical onset
-
(3)
Identification of an aneurysm as the source of the bleeding by digital subtraction angiography (DSA)
-
(4)
3T MRI including T2*-weighted sequence and fluid-attenuated inversion recovery (FLAIR) imaging, performed at least 4 months after the acute SAH
Exclusion criteria were as follows:
-
(1)
Non-aneurysmal SAH, e.g., traumatic or unknown cause
-
(2)
Imaging quality insufficient for analysis
Imaging acquisition
At our institution, MRI is routinely performed on a 3T Scanner (Signa HDxt, GE Healthcare, Milwaukee, USA) according to a standardized protocol that we use for all patients with treated or untreated intracranial aneurysm. This protocol includes T2*-weighted and FLAIR imaging, as well as DWI, T2-weighted imaging, and contrast-enhanced magnetic resonance angiography (MRA).
Gradient-echo T2*-weighted sequences are acquired in the axial plane with repetition time (TR) = 540 ms, echo time (TE) = 14 ms, field of view (FOV) = 220 mm, matrix size = 256 × 256, slice thickness of 5 mm, and an acquisition time of 1 min 13 s. FLAIR sequences are likewise acquired in the axial plane with TR = 7000 ms, TE = 116 ms, FOV = 220 mm, matrix size = 320 × 320, slice thickness of 5 mm, and an acquisition time of 4 min 20 s.
Data analysis
Image interpretation was performed on a standard PACS workstation (Magic View VE42, Siemens Medical Solutions, Erlangen, Germany) by two neuroradiologists in consensus. CCT performed within 48 h of clinical onset was evaluated regarding the extent and distribution of the acute SAH. Grading was performed according to the Fisher scale [8]: 1 = no hemorrhage evident on CCT, 2 = SAH less than 1 mm thick, 3 = SAH more than 1 mm thick, and 4 = no SAH or SAH of any thickness with intraventricular hemorrhage or parenchymal extension. Localization of the ruptured aneurysm was determined on DSA, and the type of treatment (interventional, surgery) was noted. Furthermore, imaging and clinical records were checked regarding the fact, if patient needed an external ventricular drainage (EVD) in the acute stage of SAH. If available from the clinical records, clinical grade at the onset of acute SAH was given according to the World Federation of Neurological Surgeons (WFNS) grading scale ranging from I (minor neurologic deficits) to V (coma) [9].
Analysis of the MRIs was done in consensus by the same two neuroradiologists, blinded to all clinical and patient information data. If available, all follow-up MR examinations (including T2*-weighted imaging) of each patient were reviewed separately. FLAIR images were used to exclude that acute SAH was still evident. T2*-weighted images were systematically assessed for evidence of superficial siderosis, i.e., linear hypointensities along the gyral and/or brain stem surface. Side and localization (frontal, parietal, temporal, occipital, sylvian fissure, infratentorial) of superficial siderosis was noted. The extent of superficial siderosis in the hemispheric sulci was classified as either focal (restricted to ≤3 sulci) or disseminated (>3 sulci) [4]. Additionally, T2*-weighted images were evaluated regarding intraparenchymal hypointensities, e.g., along the channel of the EVD, along the surgical access after clipping, or within the arterial infarction. These signal alterations were also noted but were not judged as superficial siderosis consequential to SAH.
Statistical analysis
Patient age and time interval between acute SAH and date of MRI were expressed as mean (range). Percentages were calculated for the different localizations of SAH, superficial siderosis, WFNS, placement of an EVD, type of aneurysm, and treatment. Wilcoxon rank sum tests were used to evaluate the influence of (a) time between acute SAH and the last available MRI examination and (b) age of the patient at the event of SAH on the prevalence of superficial siderosis. Cochran-Armitage test was used to evaluate the influence of degree of acute SAH (expressed in Fisher grade) on the prevalence of superficial siderosis. To test differences regarding the presence of superficial siderosis in patients, (a) with versus without EVD, (b) any CSF-draining procedure (EVD and/or clipping) versus non-draining procedure (no EVD and/or coiling), and (c) aneurysmal treatment with coiling versus clipping, Fisher’s exact tests were adopted. Influence of gender on the development of superficial siderosis was likewise tested using Fisher’s exact test. Probability values p < 0.05 were considered statistically significant.
Results
Seventy-two consecutive patients with CCT and/or CSF-proven SAH were included in the study (mean age at date of SAH 52.2 years, range 29–73 years, 14 male, 58 female). WFNS grading was available in 48 patients: grade I in 20 cases, grade II in 6 cases, grade III in 5 patients, grade IV in 6 patients, and grade V in 11 patients. According to the Fisher grading, SAH was grade 1 in 2 cases, grade 2 in 4 cases, grade 3 in 10 cases, and grade 4 in 56 cases. The exact localizations of SAHs are summarized in Table 1.
The ruptured aneurysm was located in the anterior circulation in 31 patients (right/left internal carotid artery: n = 8/6, anterior communication artery: n = 13, right/left middle cerebral artery: n = 1/1, and anterior cerebral artery: n = 2). In 29 patients, the posterior circulation was involved (basilar artery: n = 12, right/left posterior communication artery: n = 5/2, left posterior inferior cerebellar artery: n = 6, right/left posterior cerebral artery: n = 1/1, superior cerebellar artery: n = 1, and vertebral artery: n = 1). In 12 patients, more than one aneurysm as possible bleeding source was found and treated (two aneurysms: n = 7, three aneurysms: n = 5). Overall, 7 patients underwent surgical aneurysm clipping, and 65 patients underwent interventional treatment (59 patients with coil embolization, 7 patients with a combination of stent implantation and coil embolization).
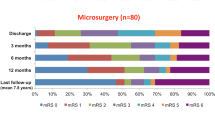
A total of 117 MR investigations were available for analysis in overall 72 patients. In 29 patients, more than one MRI was available (maximum 6 MRIs). The mean time interval between the first and last MRI in this subpopulation was 25.8 months (range 5–104). The mean time interval between symptom onset and MRI was 37.2 months (range 4–129) if the first available MRI was considered and 47.4 months (range 4–129) if the last available MRI was considered. Superficial siderosis was detected in a total of 39 patients (54.2 %). It involved 1 area in 13 cases (33.3 %); 2 areas in 10 cases (5.1 %); 3 and 4 areas in 5 cases (12.8 %), respectively; 5 areas in 1 case (2.6 %); and all 6 areas in 5 cases (12.8 %). Its extent with regard to the hemispheric sulci was focal in 15 cases (38.5 %) and disseminated in 24 cases (61.5 %). The exact localization of superficial siderosis is summarized in Table 1.
Regarding the 29 patients with more than one follow-up MRI scan, localization and extent of superficial siderosis did not change over time in any of these patients (Fig. 1). Thus, prevalence and extent of siderosis are given referring to the number of patients and not to the number of MR examinations.
CCT (a, b), DSA (c), and T2*-weighted images (d, e) of a 40-year-old female patient with extensive SAH Fisher grade 4 in the basal cisterns (a, white arrows) and supratentorially, especially in the sylvian fissure (b, white arrows). The underlying cause was rupture of an aneurysm of the right posterior communicating artery (c, thin white arrow). T2*-weighted images 24 months after the acute SAH (c, d) show extensive superficial siderosis infratentorially (c, black arrows) and supratentorially. On follow-up MRI (e) 51 months after the SAH, extent and distribution of superficial siderosis did not change
In six cases, T2*-hypointense signal alterations, not corresponding to superficial siderosis, were evident. They were located along the channel of the EVD in three cases, along the surgical access in two cases, and within a large infarction due to vasospasm in the territory of the middle cerebral artery in one case.
In 25 out of 34 (73.5 %) patients with bilateral supratentorial SAH, siderosis has well occurred on both sides supratentorially. There was one patient who did not show supratentorial SAH involvement on CCT in the acute stage but presented with supratentorial superficial siderosis on MRI performed 12 months later (Fig. 2). Infratentorial involvement of SAH was evident on CCT in 64 cases (88.9 %). Of these patients, only 14 patients (21.9 %) developed infratentorial superficial siderosis.
CCT (a, b) and T2*-weighted images (c, d) of a 45-year-old male patient with basal SAH Fisher grade 4 (b, white arrows) without involvement of the central sulcus (a, white arrows) due to rupture of a basilar artery aneurysm. T2*-weighted images 12 months after the acute SAH show no signs of superficial siderosis infratentorially (d) but focal superficial siderosis at the central sulcus bilaterally (c, black arrow)
There was no significant difference regarding the time interval between acute SAH and the last available MRI scan in patients with (mean 42.9 months, range 4–123 months) versus patients without (mean 42.9 months, range 12–129 months) superficial siderosis (p = 0.6). Results for differences between patients with and without superficial siderosis regarding age, amount of SAH in the acute stage (Fisher grade), and CSF-draining procedures are summarized in Table 2.
Discussion
Our data show that superficial siderosis is detectable in approximately half of the patients (54 %) after one singular, acute aneurysmal SAH. An older age at the time of acute SAH and a greater amount of initial subarachnoid blood, as well as an initial SAH involvement of the supratentorial compartment, were associated with siderosis formation in our series.
Prevalence and localization of siderosis after singular acute aneurysmal SAH
Theoretically, an acute subarachnoidal blood clot is supposed to be washed out with CSF with time. Blood residues, including deoxyhemoglobin, that are not washed out with CSF will physiologically be converted to hemosiderin within a few months, which then might deposit on the brain surface and persist as abnormal low intensity on T2*-weighted imaging and present as superficial siderosis on MRI [10, 11].
Available data on the prevalence of siderosis after singular acute SAH is sparse and somewhat contradictory. Some authors report a gradual normalization of abnormal signal loss on T2*-weighted images within 90 days after the onset of an acute aneurysmal SAH [10]. Another rather small series with limited follow-up interval found any subarachnoid hemosiderin deposition on T2*-weighted MRI in 66.7 % (8 of 12 patients) and 76.2 % (16 of 21 patients) at 4 to 12 and 12 to 18 months after acute aneurysmal SAH, respectively [12]. Symptomatic infratentorial superficial siderosis has been reported to be extremely uncommon after a singular SAH regardless of how massive it is [13, 14].
In our larger series of 72 patients with singular, aneurysmal SAH, superficial siderosis was evident in 54 % of cases on long-term follow-up MRI performed at a mean time interval of 47.4 months after the acute bleeding event. Thus, only approximately one half of patients developed a certain degree of siderosis on long-term follow-up, while the other half did not.
In accordance with a previous study [12], superficial siderosis was preferentially but not exclusively found in areas near the ruptured aneurysms and at the localization of the acute SAH in our series. All patients who initially presented with supratentorial involvement of SAH developed supratentorial superficial siderosis later, and most patients with bilateral supratentorial SAH involvement developed superficial siderosis likewise on both sides supratentorially. On the contrary, only 36 % of our patients with infratentorial involvement in the acute stage developed infratentorial superficial siderosis. We did not observe any siderosis involvement of the cranial nerves in our patients. Accordingly, Imaizumi et al. found that ventricles and cisterns, even if close to the site of the aneurysmal rupture, rarely displayed T2* signal alterations [12]. They hypothesize that abundant CSF flow as present in the ventricles and cisterns might disturb hemosiderin deposition, whereas trapped hematoma fluid due to narrow adjacent structures (like supratentorial gyri) may promote it [12]. This hypothesis would be in accordance with the observation that cortical superficial siderosis seems to be a frequent finding in CAA patients with focal convexity SAHs, although the SAHs in these patients are typically restricted to a few cortical sulci [12]. On the contrary, a primarily infratentorial distribution of siderosis with frequent involvement of the cranial nerves is the hallmark of the classical, symptomatic form of CNS siderosis and results in the typical clinical triad of hearing loss, ataxia, and cerebellar dysarthria [12]. Our observation that infratentorial siderosis is not as frequently observed as expected after a singular acute aneurysmal SAH indirectly indicates that additional pathophysiological conditions must contribute to siderosis formation in patients with the classical symptomatic form of CNS siderosis.
Factors influencing siderosis formation
We particularly aimed to identify factors which might influence siderosis formation in the setting of acute aneurysmal SAH, hypothesizing that those might also apply for siderosis of other etiologies.
One obvious potential influencing factor might be the initial amount of blood in acute SAH, as suggested by Imaizumi et al. [12] who found more severe hemosiderin deposition in patients with SAH with a high Fisher grade. In interpreting their results, it has to be taken into account that the time between SAH and MRI was less than 4 months in almost half of their cases. Within this time period, the blood clot following extensive SAH might often not be fully washed out yet and differentiation between deoxyhemoglobin and hemosiderin (both resulting in a hypointense signal) is not possible using T2*-weighted imaging at this stage. However, our long-term follow-up examinations (mean = 47.4 months) confirm this hypothesis, as we also found a higher probability of siderosis formation with a rising amount of acute SAH stage as expressed by Fisher grade.
Patient age at the time point of acute SAH is another assumed influencing factor on the development of superficial siderosis [12]. Accordingly, in our series, patients who developed superficial siderosis were significantly older compared to those who did not. To explain the influence of patient’s age, some authors hypothesize that secondary enlargement of the subarachnoid space in patients with age-related cortical atrophy might influence the extent of subarachnoid hematoma and thus the extent of hemosiderin deposition [12]. For CAA-related cortical superficial siderosis, it has been suggested that those patients who develop superficial siderosis might be intrinsically less able to clear hemorrhage from their brain [15], possibly due to (genetic) differences in heme and iron metabolism [15].
In this context, it could also be hypothesized that the washout of subarachnoid blood during a neurosurgical operation, i.e., clipping and/or placement of an EVD in the acute stage of SAH, would accelerate the clearance of blood from the subarachnoid space and thus would have a considerable effect on the extent of hemosiderin deposition. However, our results as well as previous studies [12] demonstrate that no kind of CSF-draining procedure (clipping and/or EVD) in the acute stage of SAH did reduce the occurrence of superficial siderosis. Contrarily, the prevalence of superficial siderosis was somewhat higher (although not statistically significant) in patients who underwent a CSF-draining procedure in the acute stage of SAH compared to those who did not (80 versus 61 % for EVD alone; 82 versus 67 % for any CSF-draining procedure). Based on these results, it could be contrariwise assumed that the need for external CSF drainage by EVD placement is indicative for dysfunction of CSF circulation and resorption and may thus lead to a reduced washout effect and prolonged presence of blood and blood degradation products in the subarachnoid space. However, further studies including histopathologic correlation are needed to definitely determine the detailed role of aging and CSF circulation in the mechanism of siderosis formation.
Limitations of the study
As a limiting factor of this investigation, linear low signal intensities on T2*-weighted MRI are not specific for hemosiderin deposits but might also be caused by some mimics, as e.g., calcifications, vessels, particularly veins, and venous thrombosis [16]. Therefore, we tried to exclude causes other than hemosiderin by not only considering the T2*-weighted imaging but by also referring to the CCT and FLAIR images. Another limitation of this study is the lack of certainty that superficial siderosis was indeed a consequence of the acute aneurysmal SAH in each individual case, as superficial siderosis is found in a small percentage of individuals in the general elderly population (0.7 % in [15]), in approximately 6 % of patients with cognitive impairment [17], and in a large percentage of patients with CAA (60.5 % in [4]). However, considering the mean age of our patients (52.2 years), which would be rather young for CAA, and the lack of any clinical history indicating other potential causes of superficial siderosis, the chance that we included one or more patients with preexisting superficial siderosis is rather low.
Conclusions
In summary, our data show that superficial siderosis does not necessarily require repeated or continuous bleeding into the subarachnoid space but develops in approximately half of patients after singular, aneurysmal SAH. An older age and a greater amount of blood seem to be associated with a higher risk of developing superficial siderosis. However, our findings indicate that additional factors must play a role in whether a patient is prone to develop superficial siderosis or not. Further studies are needed to determine these contributors and to identify additional imaging characteristics that might allow further conclusions regarding the underlying cause of siderosis in an individual patient.
References
Bracchi M, Savoiardo M, Triulzi F, Daniele D, Grisoli M, Bradac GB, Agostinis C, Pelucchetti D, Scotti G (1993) Superficial siderosis of the CNS: MR diagnosis and clinical findings. AJNR Am J Neuroradiol 14(1):227–236
Kumar N (2010) Neuroimaging in superficial siderosis: an in-depth look. AJNR Am J Neuroradiol 31(1):5–14. doi:10.3174/ajnr.A1628
Linn J, Herms J, Dichgans M, Bruckmann H, Fesl G, Freilinger T, Wiesmann M (2008) Subarachnoid hemosiderosis and superficial cortical hemosiderosis in cerebral amyloid angiopathy. AJNR Am J Neuroradiol 29(1):184–186. doi:10.3174/ajnr.A0783
Linn J, Halpin A, Demaerel P, Ruhland J, Giese AD, Dichgans M, van Buchem MA, Bruckmann H, Greenberg SM (2010) Prevalence of superficial siderosis in patients with cerebral amyloid angiopathy. Neurology 74(17):1346–1350. doi:10.1212/WNL.0b013e3181dad605
Charidimou A, Peeters A, Fox Z, Gregoire SM, Vandermeeren Y, Laloux P, Jager HR, Baron JC, Werring DJ (2012) Spectrum of transient focal neurological episodes in cerebral amyloid angiopathy: multicentre magnetic resonance imaging cohort study and meta-analysis. Stroke J Cereb Circ 43(9):2324–2330. doi:10.1161/strokeaha.112.657759
Zonneveld HI, Goos JD, Wattjes MP, Prins ND, Scheltens P, van der Flier WM, Kuijer JP, Muller M, Barkhof F (2014) Prevalence of cortical superficial siderosis in a memory clinic population. Neurology. doi:10.1212/WNL.0000000000000150
Iwanowski L, Olszewski J (1960) The effects of subarachnoid injections of iron-containing substances on the central nervous system. J Neuropathol Exp Neurol 19:433–448
Fisher CM, Kistler JP, Davis JM (1980) Relation of cerebral vasospasm to subarachnoid hemorrhage visualized by computerized tomographic scanning. Neurosurgery 6(1):1–9
Teasdale GM, Drake CG, Hunt W, Kassell N, Sano K, Pertuiset B, De Villiers JC (1988) A universal subarachnoid hemorrhage scale: report of a committee of the World Federation of Neurosurgical Societies. J Neurol Neurosurg Psychiatry 51(11):1457
Inoue T, Takada S, Shimizu H, Niizuma K, Fujimura M, Sato K, Endo H, Tominaga T (2013) Signal changes on T2*-weighted magnetic resonance imaging from the acute to chronic phases in patients with subarachnoid hemorrhage. Cerebrovasc Dis 36(5–6):421–429. doi:10.1159/000355897
Takada S, Inoue T, Niizuma K, Shimizu H, Tominaga T (2011) Hemosiderin detected by T2*-weighted magnetic resonance imaging in patients with unruptured cerebral aneurysms: indication of previous bleeding? Neurol Med Chir 51(4):275–281
Imaizumi T, Chiba M, Honma T, Niwa J (2003) Detection of hemosiderin deposition by T2*-weighted MRI after subarachnoid hemorrhage. Stroke J Cereb Circ 34(7):1693–1698. doi:10.1161/01.STR.0000075771.88719.CE
Kumar A, Aggarwal S, Willinsky R, TerBrugge KG (1993) Posterior fossa surgery: an unusual cause of superficial siderosis. Neurosurgery 32(3):455–457, discussion 457
Miliaras G, Bostantjopoulou S, Argyropoulou M, Kyritsis A, Polyzoidis K (2006) Superficial siderosis of the CNS: report of three cases and review of the literature. Clin Neurol Neurosurg 108(5):499–502. doi:10.1016/j.clineuro.2005.01.014
Vernooij MW, Ikram MA, Hofman A, Krestin GP, Breteler MM, van der Lugt A (2009) Superficial siderosis in the general population. Neurology 73(3):202–205. doi:10.1212/WNL.0b013e3181ae7c5e
Atlas SW, Mark AS, Grossman RI, Gomori JM (1988) Intracranial hemorrhage: gradient-echo MR imaging at 1.5 T. Comparison with spin-echo imaging and clinical applications. Radiology 168(3):803–807. doi:10.1148/radiology.168.3.3406410
Wollenweber FA, Buerger K, Mueller C, Ertl-Wagner B, Malik R, Dichgans M, Linn J, Opherk C (2014) Prevalence of cortical superficial siderosis in patients with cognitive impairment. J Neurol 261(2):277–282. doi:10.1007/s00415-013-7181-y
Ethical standards and patient consent
We declare that the study was approved by our Institutional Review Board and has therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. We declare that all patients gave informed consent prior to inclusion in this study.
Conflict of interest
We declare that we have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lummel, N., Bernau, C., Thon, N. et al. Prevalence of superficial siderosis following singular, acute aneurysmal subarachnoid hemorrhage. Neuroradiology 57, 349–356 (2015). https://doi.org/10.1007/s00234-014-1480-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-014-1480-6