Abstract
We examined MRI of two patients with progressive multifocal leukoencephalopathy (PML), including diffusion-weighted imaging (DWI), with calculation of apparent diffusion coefficients (ADC). The pathology findings of one patient were compared with those of MRI. The lesions had different ADC and DWI appearances, depending on the stage of the disease. Newer lesions and the advancing edge of large lesions had normal-to-low ADC and gave high signal on DWI. Older lesions and the centre of large lesions had increased ADC and gave low signal. High signal on DWI and low ADC mark the regions of active infection and cell swelling, distinguishing them from areas of reparative gliosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Progressive multifocal leukoencephalopathy (PML) is a fatal, progressive disease due to infection by the JC Papova virus. The infection is probably acquired early in life, but remains latent. Interference with the immune system, such as human immunodeficiency virus infection, malignancy or immunosuppressive drugs, reactivates the virus and may lead to the disease.
The JC virus affects oligodendrocytes almost exclusively, causing demyelination. Symptoms include progressive focal and diffuse deficits (visual, motor, cognitive deficits and memory loss, personality change), leading to death a few months after diagnosis. PML should be suspected in any immunocompromised patient with progressive focal neurological deficits [1], a rearranged regulatory region of JC virus DNA detected in cerebrospinal fluid (CSF) by a polymerase chain reaction [2] and typical lesions on MRI [3]. Pathological findings include multiple foci of demyelination, with macrophage infiltrates, which tend to converge, and finally gliosis. Histological demonstration of viral particles in the nuclei of oligodendrocytes is diagnostic [4]. High sensitivity and lack of invasiveness make MRI the most feasible diagnostic method [3, 5, 6]. Different techniques, in particular magnetization-transfer, have been used for more precise correlation with pathology [7, 8]. Diffusion-weighted MRI (DWI) were rarely reported [9, 10, 11], even without pathological correlations. We describe two patients with PML studied by DWI, and report pathological correlates of the MRI findings in one.
Case reports
Case 1
A 68-year-old man presented with memory loss and personality change for 1 month. He had systemic non-Hodgkin’s lymphoma 3 years previously, thought to be cured after radiotherapy and cytostatics. He had a mild sensory dysphasia, apraxia and acalculia, suggesting bilateral parietal dysfunction. The tendon reflexes were normal, as were power and coordination. Routine laboratory investigations, examination of the CSF, bone-marrow biopsy, chest and abdominal CT were normal. Brain CT scan showed multiple low-density cerebral lesions.
MRI was obtained, including DWI (TR 6600 TE 160 ms, field of view 275 mm; matrix 128×96), with b of 0 and 1000 s/mm2 in the three axes. Multiple lesions in frontal and parietal white matter gave very high signal on T2- and low signal on T1-weighted images. They involved the most peripheral, subcortical white matter, with a sharply defined border between lesion and cortex. The abnormal signal changed more gradually to normal along their medial border with the normal white matter (Fig. 1a). The cortex, basal ganglia, brain stem and cerebellum were not affected.
Patient 1. a Axial T2-weighted image showing bilateral high-signal lesions in frontal and parietal white matter, with well-defined borders towards the cortex, and blurred borders with the normal white matter. There is no mass effect. b Axial diffusion-weighted imaging (DWI) shows the lesions as high signal, definitely higher on their medial borders
On DWI, the lesions gave high signal, especially on their medial borders (Fig. 1b). There was no mass effect or contrast enhancement. ADC calculation on 2×2 pixel regions-of-interest showed different regions within the lesions: the medial border had normal-to-low diffusion (0.74±0.12 mm2/s) while the centre had increased diffusion (1.89±0.15 mm2/s).
Within a month the patient was decerebrate, and died of pneumonia. Neuropathological examination demonstrated typical features of PML in the brain. Macroscopically, there were large lesions of the frontal and parietal white matter on both sides, more marked in the left hemisphere, and many confluent foci of demyelination (Fig. 2a–c). Microscopically, there was diffuse loss of myelin with many macrophages, especially at the borders of the lesions, large and bizarre cells, with many oligodendrocytes. The latter, most frequent at the borders of the lesions, had large, deeply staining nuclei. At the centre of the lesions the extracellular spaces were large, with sparse oligodendrocytes, macrophages and reactive astrocytes. (Fig. 2d–f). Axonal disruption was more evident at the centre of the lesions.
Patient 1. a Coronal pathological section (Luxol fast blue). Demyelinated areas appear brighter. b Coronal T2-weighted section grossly corresponding to a. The high-signal lesions correspond to the demyelinated areas. c Low magnification view (Luxol fast blue, original magnification ×20) of the border of a lesion, with multiple bright demyelinated areas. d Lesion border with large, dark oligodendrocytes, sparse macrophages and reactive astrocytes. The oligodendrocytes are infected but still viable; macrophages are responsible for myelin catabolism (haematoxylin and eosin stain, original magnification ×200). e As d, with predominant macrophages, suggesting active demyelination. f As d, at core of lesion, with large extracellular spaces, oligodendrocytes and reactive astrocytes
Case 2
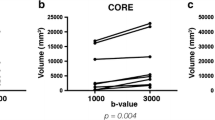
A 32-year-old man with human immunodeficiency virus infection for 14 years had a 4-week history of increasing left hemiparaesthesiae, ataxic gait, dysarthria and inco-ordination; examination revealed dysmetria, dysdiadochokinesis and an ataxic gait. The CD4+ lymphocyte count was 114/mm3. MRI at 0.5 tesla showed asymmetrical areas of high signal on T2-weighted images in the right cerebellar hemisphere, vermis and bilateral frontal and right temporoparietal subcortical white matter, without mass effect or contrast enhancement. The deep grey matter structures were spared. Over the following months, despite antiretroviral therapy, the patient deteriorated, with disorientation and memory impairment. MRI at 3 tesla, including DWI (TR 2800 TE 78 ms) with b 0 and 1000 in the three axes showed an extension of the abnormal signal to the right cerebellar peduncle and pons. The cerebellar lesions seen on the first MRI gave higher signal on T2-weighted images and signal less than that of the newer lesions on DWI (Fig. 3a): their ADC were high (1.26±13.2 mm2/s), whereas the new lesions had lower ADC (0.91±8.1 mm2/s) (Fig. 3b). PML was suspected on the basis of clinical signs, course and typical MR imaging. Brain biopsy was planned, but could not be performed because of worsening of the patient’s clinical condition; he died 2 weeks later. His family did not consent to autopsy.
Patient 2. a T2-weighted axial section, showing high-signal lesions in the white matter of the right cerebellar hemisphere, cerebellar peduncle and pons. The cerebellar lesion was present on a previous examination, when the peduncle and pons were not involved. b Axial DWI. The lesions give high signal, particularly the newer lesions
Discussion
The MRI picture of PML is well known [3, 5, 6], but their correlation with pathology and ultimately with prognosis is still to be elucidated. Nonspecific signal changes on T1- and T2-weighted images are due to the abnormal water/fat ratio in the damaged tissue. In PML the loss of fat-rich myelin, replaced by gliotic tissue, probably plays a major role, but other processes, such as demyelination, cell death and fluid extravasation may be relevant. Magnetization transfer ratio is reduced in PML lesions, probably due to myelin loss [7, 8]. Mass effect and contrast-enhancement, absent in the majority of cases, are seen with a rapid course and poorer prognosis. Their appearance after effective antiretroviral therapy has been interpreted as evidence of an active reaction against the infection, with a slower course or stabilisation [12, 13, 14].
Signal intensity and ADC were different in asynchronous lesions. Similar findings were reported in two patients examined by DWI [9, 11]. The patient reported by Henderson et al. [11] had a frontoinsular lesion with a high-signal rim on DWI, similar to our first patient. ADC were reduced in this rim. In the other patient [9] infratentorial lesions had borders with high signal on DWI, which decreased during follow-up, with an inverse increase in signal on T2-weighted images, with a final picture closely resembling that of our second patient. These different signals and ADC probably reflect different stages of the disease. In old lesions or at the centre of large lesions normal brain tissue, including axons, is completely lost. Macrophage catabolism and glial reparative responses generate gliotic tissue, with sparse cells and a large extracellular space, a common reaction to different kinds of lesion (Fig. 2c).
MRI signal intensity derives from the water and lipid content: increase in water and reduction in lipids increase T2 and decrease T1. The loss of spatial organisation and increase in extracellular space are probably responsible for the increased ADC, as in the massive brain destruction in stable infarcts [15].
Newer lesions and the edges of large lesions contain swollen oligodendrocytes with intranuclear inclusions and partially destroyed myelin, whereas axons are relatively spared (Fig. 2d). Dead cells are removed by macrophages. This partially damaged tissue gives signal on T1- and T2-weighted images which is intermediate between that of normal and completely destroyed tissue. ADC at the edges of lesions were normal or low, not intermediate, compared to normal tissue and to the centre of the lesions. This may have different causes. First, the amount of tissue destruction may be not be such as to affect ADC in the early stages of the disease, when axons are relatively spared. Alternatively, a process specifically present at the border of the lesion may be responsible for restricted diffusion. Viral intranuclear inclusions, demyelination, macrophages and cell swelling, all occurring at the borders of the lesions, are possible candidates.
It is not known if viral inclusion particles affect water diffusion. It has been suggested that extensive deposition of prion protein reduces diffusion in different diseases [16]. The amount of viral nuclear inclusions in oligodendrocytes is extremely limited compared to the amount of tissue overall, and a relevant influence on water diffusion would not be expected (Fig. 2d). It is not clear if demyelination affects diffusion. The constant presence of extracellular oedema in inflammatory [17] and noninflammatory [18, 19] demyelination, causing increased diffusion, makes it difficult to identify the net effect of myelin catabolism. Although the extracellular oedema may be a confounding factor, demyelination per se probably does not affect diffusion [20].
Reduced diffusion is said to mark acute, irreversible cell damage in arterial ischaemia [21], although there are exceptions [22]. Cell swelling due to irreversible cytotoxic oedema represents the most likely pathological correlate of restricted diffusion [15, 21]. Pathology demonstrates swollen oligodendrocytes only at the borders of PML lesions, suggesting that swelling of oligodendrocytes, like neuronal necrosis in other diseases, reduces diffusion.
ADC and T2 shine-through phenomenon lead to a notable appearance of the lesions on DWI in our patient and in other reported cases, with high-signal and isointense to low-signal regions, due to different pathological stages. This mixed diffusion pattern, in particular the high signal on DWI around a low-signal centre might be useful in differential diagnosis.
References
Brooks B, Walker D (1984) Progressive multifocal leukoencephalopathy. Neurol Clin 2: 299–313
McGuire D, Barhite S, Hollander H, Miles M (1995) JC virus DNA in the cerebrospinal fluid of human immuno-deficiency virus-infected patients: predictive value for progressive multifocal leukoencephalopathy. Ann Neurol 37: 395–399
Mark A, Atlas S (1989) Progressive multifocal encephalopathy in patients with AIDS: appearance on MRI images. Radiology 173: 517–520
Esiri MM, Kennedy PG (1997) Viral diseases. In: Graham D, Lantos P (eds) Greenfield’s neuropathology, vol 2, 6th edn. Arnold, London, pp 42–46
Guilleux MH, Steiner RE, Young IR (1986) MR imaging in progressive multifocal leukoencephalopathy. AJNR 7: 1033–1035
Levy JD, Cottingham KL, Campbell RJ, et al (1986) Progressive multifocal leukoencephalopathy and magnetic resonance imaging. Ann Neurol 19: 399–401
Kasner SE, Galetta SL, McGowan JC, Grossman RI (1997) Magnetization transfer imaging in progressive multifocal leukoencephalopathy. Neurology 48: 534–536
Ernst T, Chang L, Witt M, et al (1999) Progressive multifocal leukoencephalopathy and human immunodeficiency virus–associated white matter lesions in AIDS: magnetization transfer MR imaging. Radiology 210: 539–543
Ohta K, Obara K, Sakauchi M, Obara K, Takane H, Yogo Y (2001) Lesion extension detected by diffusion-weighted magnetic resonance imaging in progressive multifocal leukoencephalopathy. J Neurol 248: 809–811
Oguz KK, Oguz B, Cila A (2002) Diffusion weighted imaging (DWI) of progressive multifocal leukoencephalopathy (PML) at 3T imager. J Neuroradiol 29: S141
Henderson RD, Smith MG, Mowat P, Read SJ (2002) Progressive multifocal leukoencephalopathy. Neurology 58: 1825
Donovan Post M, Yiannoutsos C, Simpson D, et al (1999) Progressive multifocal leukoencephalopathy in AIDS: are there any MR findings useful to patient management and predictive of patient survival? AJNR 20: 1896–1906
Arbusow V, Strupp M, Pfister HW, Seelos KC, Bruckmann H, Brandt T (2000) Contrast enhancement in progressive multifocal leukoencephalopathy: a predictive factor for long-term survival? J Neurol 247: 306–308
Thurnher M, Donovan Post J, Rieger A, Kleibl-Popov C, Loewe C, Schindler E (2001) Initial and follow-up MR imaging findings in AIDS-related progressive multifocal leukoencephalopathy treated with highly active antiretroviral therapy. AJNR 22: 977–984
Schaefer PW, Grant PE, Gonzalez RG (2000) Diffusion-weighted MR imaging of the brain. Radiology 217: 331–345
Bahn MM, Parchi P (1999) Abnormal diffusion-weighted magnetic resonance images in Creutzfeldt-Jakob disease. Arch Neurol 56: 577–583
Horsfield MA, Larsson HB, Jones DK, Gass A (1998) Diffusion magnetic resonance imaging in multiple sclerosis. J Neurol Neurosurg Psychiatry 64 [Suppl 1]: S80–S84
Cramer SC, Stegbauer KC, Schneider A, Mukai J, Maravilla KR (2001) Decreased diffusion in central pontine myelinolysis. AJNR 22: 1476–1479
Provenzale JM, Petrella JR, Cruz LC Jr, Wong JC, Engelter S, Barboriak DP (2001) Quantitative assessment of diffusion abnormalities in posterior reversible encephalopathy syndrome. AJNR 22: 1455–1461
Schaefer PW (2000) Diffusion-weighted imaging as a problem-solving tool in the evaluation of patients with acute stroke like syndromes. Top Magn Reson Imaging 11: 300–309
Moseley ME, Kucharczyk J, Mintorovitch J, et al (1990) Diffusion-weighted MR imaging of acute stroke: correlation with T2-weighted and magnetic susceptibility-enhanced MR imaging in cats. AJNR 11: 423–429
Oppenheim C, Stanescu R, Dormont D, et al (2000) False-negative diffusion-weighted MR findings in acute ischemic stroke. AJNR 21: 1434–1440
Author information
Authors and Affiliations
Corresponding author
Additional information
Presented in part at the XVII Symposium Neuroradiologicum, Paris, August 2002
Rights and permissions
About this article
Cite this article
Bergui, M., Bradac, G.B., Oguz, K.K. et al. Progressive multifocal leukoencephalopathy: diffusion-weighted imaging and pathological correlations. Neuroradiology 46, 22–25 (2004). https://doi.org/10.1007/s00234-003-1115-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-003-1115-9