Abstract
P-glycoprotein (P-gp) is an ATP-dependent drug pump that can transport a broad range of hydrophobic compounds out of the cell. The protein is clinically important because of its contribution to the phenomenon of multidrug resistance during AIDS/HIV and cancer chemotherapy. P-gp is a member of the ATP-binding cassette (ABC) family of proteins. It is a single polypeptide that contains two repeats joined by a linker region. Each repeat has a transmembrane domain consisting of six transmembrane segments followed by a hydrophilic domain containing the nucleotide-binding domain. In this mini-review, we discuss recent progress in determining the structure and mechanism of human P-glycoprotein.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
During cancer chemotherapy, it was found that tumors were capable of developing resistance to a broad range of cytotoxic agents (multidrug resistance) (Biedler & Riehm, 1970; Dano, 1972). Drug-resistant mammalian cell lines were then established for studying the phenomenon of multidrug resistance. Cell lines that were initially selected for resistance to one cytotoxic drug were later shown to display cross-resistance to other structurally unrelated cytotoxic compounds (Biedler & Riehm, 1970; Riordan & Ling, 1985; Shen et al., 1986). In nearly all cases, the drug-resistant cell lines showed over-expression of a 170 kDa glycosylated plasma membrane protein when compared to the drug-sensitive parent cell lines (Ling & Thompson, 1974; See et al., 1974). The protein was termed P-glycoprotein (P-gp) because it appeared to affect the permeability of the membrane to cytotoxic compounds (Juliano & Ling, 1976). It was subsequently shown that P-gp is an ATP-dependent drug pump that can transport a broad range of structurally unrelated compounds out of the cell (Gottesman & Pastan, 1993).
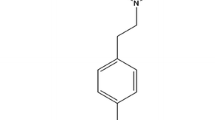
In 1986, three groups reported the cloning and sequencing of the gene responsible for P-gp-mediated drug resistance from hamster (Gerlach et al., 1986), human (Chen et al., 1986) and mouse (Gros et al., 1986) cell lines. The human P-gp (product of the MDR1 gene; ABCB1) has 1280 amino acids that are arranged as two homologous halves joined by a linker region. Each half begins with a transmembrane domain (TMD) containing six transmembrane (TM) segments followed by a hydrophilic region containing a nucleotide-binding domain (NBD) (see Fig. 1) (Chen et al., 1986; Kast et al., 1996; Loo & Clarke, 1995b). The presence of four domains and conserved sequences in the NBDs are characteristic of the ATP-binding cassette (ABC) family of transporters (Higgins, 1992). Sequencing of the human genome has shown that there are 48 members in the ABC family of transporters (Dean, Rzhetsky & Allikmets, 2001).
Schematic models of P-gp. (A) The white cylinders represent the TM segments in TMD1, while the grey cylinders represent TM segments within TMD2. The branched lines represent the glycosylation sites and the rounded rectangles represent the NBDs. The residues shown in the TM segments are predicted to be part of the drug-binding pocket because cysteines introduced at these positions in TMD1 can be cross-linked to cysteines introduced at the indicated positions in TMD2 with MXM cross-linkers that are substrates of P-gp (Loo & Clarke, 2001c). (B) Model of the organization of the TM segments based on cross-linking and cysteine-scanning mutagenesis studies. The common drug-binding pocket is at the interface between the TMDs.
Expression of P-gp in humans is quite variable, with the highest levels found in the apical membranes of the blood-brain/testes barrier, intestines, liver and kidney (Thiebaut et al., 1987). The physiological role of P-gp in humans is unknown. It probably prevents cytotoxic compounds in the environment and diet from entering the body and removes them by excretion into the bile and urine. Studies on P-gp knockout mice show the protein is not essential for viability or fertility and does not confer any obvious phenotypic abnormality other than hypersensitivity to drugs (Schinkel et al., 1994).
P-gp, however, can be a “double-edged” sword. While it can protect us from exogenous toxins, it can also affect the bioavailability of drugs during chemotherapy (Gottesman & Pastan, 1988). Overexpression of P-gp in cancer cells can undermine cancer chemotherapy regimens because of its ability to transport many of the drugs used in the treatment. For example, in most clinical trials in patients with acute myelogenous leukemia, there is good correlation between expression of P-gp and reduced remission rate and a greater incidence of refractory disease (Leith et al., 1999; van der Kolk et al., 2000). P-gp expression can also greatly affect the penetration of hydrophobic drugs into solid tumors (Martin et al., 2003). Similarly, the presence of P-gp in the intestine and the blood-brain barrier can affect the therapeutic levels of drugs in patients with HIV/AIDS (Lee et al., 1998). Therefore, the study of P-gp has been the subject of much research because of its clinical relevance. The ability of P-gp to transport a very broad range of unrelated compounds also makes the study of its mechanism very interesting.
Many excellent comprehensive reviews on P-gp have been published that describe the range of compounds that are substrates of P-gp, its contribution to multidrug resistance in cancer, P-gp polymorphisms and pharmacogenetics (Sharom, 1997; Hrycyna, 2001; Ambudkar et al., 2003; Schwab, Eichelbaum & Fromm, 2003). Although the P-gps from human, mouse and hamster are very similar with respect to their amino acid sequences, it is important to be aware that their transport properties are not identical. For example, it has been shown that human and mouse P-gps have different drug resistance profiles and sensitivities to modulators (Tang-Wai et al., 1995). Therefore, the focus of this review will be to summarize recent progress in understanding the mechanism of drug efflux by P-gp, with particular emphasis on the results obtained using cysteine mutagenesis and thiol-modification techniques on human P-gp.
The steps in the predicted transport cycle of P-gp are shown in Fig. 2. The first step in active efflux of drug substrate is binding of the compound to P-gp. P-gp differs from most other transport proteins (such as SERCA1) in that it interacts with substrates that have entered the lipid bilayer (Raviv et al., 1990; Homolya et al., 1993). The drug-binding domain appears to be located at the interface between the two TMDs of P-gp. The NBDs are not required because a truncated P-gp molecule that lacks both NBDs retains the ability to interact with drug substrates (Loo & Clarke, 1999b). The N-terminal- or C-terminal TMD alone cannot bind substrates, but co-expression of both TMDs results in a complex that can bind drug substrate (Loo & Clarke, 1998). Although P-gp can exist as monomers, dimers and higher oligomers (Poruchynsky & Ling, 1994), the minimum unit required for activity is a monomer (Loo & Clarke, 1996b). Similarly, CFTR has been reported to function as a monomer (Ramjeesingh et al., 2001; Chen et al., 2002; Zhang et al., 2005), while half -transporters such as ABCG2 (BCRP) (Allikmets et al., 1998; Doyle et al., 1998; Alien et al., 1999; Miyake et al., 1999), ABCG5 and ABCG8 (Graf et al., 2003) function as homo-or heterodimers.
Proposed transport cycle of P-gp based on the cross-linking pattern of Cys332(TM6). (A) In the absence of ATP or drug substrate (resting state), Cys332(TM6) can be cross-linked to Cys856(TM10) with the thiol-reactive cross-linker M8M that is also a substrate of P-gp. (B) When drug substrates (DRUG) are added, they diffuse into the lipid bilayer and enter the solvent-filled common drug-binding pocket through gates/portals formed by TMs 2 and 11 at one end and TMs 5 and 8 at the other end of the pocket. The cross-linking pattern is affected by the structure of the drug substrate (induced-fit mechanism). Binding of drug substrate changes the structure of the NBDs (circles), resulting in stimulation/inhibition of ATP hydrolysis. (C) ATP binding and hydrolysis cause rearrangement of the drug-binding pocket such as rotation/lateral movement of the TM segments and simultaneous efflux of drug substrate out of the cell or possibly into the outer leaflet with very hydrophobic substrates. ATP hydrolysis promotes interaction between the extracellular ends of TM6 and TM12 such that Cys332(TM6) can be cross-linked to Cys975(TM12) with a zero-length cross-linker. After efflux of substrate, P-gp returns to the resting state (A). It is not known whether ATP hydrolysis at the second NBD is required to return P-gp to the resting state. (D) Vanadate (Vi) trapping of nucleotide inhibits P-gp activity late in the transport cycle. In this conformation Cys332(TM6) can be cross-linked to Cys976(TM12) with the M6M cross-linker.
Characterization of the Drug-binding Domain
Several different approaches have been used to identify the location of the drug-binding site(s) in P-gp. In one method, P-gp was photolabeled with a photoactive analogue of a drug substrate and then peptides were generated from the labeled protein by chemical or proteolytic cleavage. The labeled peptides were identified using immunological methods (Bruggemann et al., 1992; Greenberger, 1993; Demmer et al., 1997; Demeule et al., 1998). The results from such studies suggested that several TM segments in TMD1 and TMD2 might play a role in substrate binding. Labeling of different TMs with the various substrate analogues suggested that different substrates might bind to different or overlapping binding sites on P-gp. Indeed, several studies have suggested that P-gp may have as many as four different drug-binding sites. Therefore, it was proposed that substrates occupy different sites during transport or that each type of substrate has a distinct binding site (Dey et al., 1997; Shapiro & Ling, 1997; Pascaud, Garrigos & Orlowski, 1998).
Alternatively, others have used quantitative structure-activity relationship (QSAR) studies with a series of compounds to define a distinct region (pharmacophore) of P-gp that bound certain types of substrates (Seelig, 1998; Wiese & Pajeva, 2001; Ekins et al., 2002; Garrigues et al., 2002; Penzotti et al., 2002; Dearden et al., 2003; Wang et al., 2003). Certain types of drug substrates could then competitively bind to the same pharmacophore in P-gp. For example, Garrigues et al. (2002) characterized two different but partially overlapping pharmacophores in P-gp. Some substrates such as verapamil bound to one site (pharmacophore 1) in P-gp while others such as vinblastine bound to another region in P-gp (pharmacophore 2). The authors postulated that it was possible for two smaller substrates to bind at the same time, whereas a large substrate could occupy both pharmacophores. These types of studies could potentially provide insight into the nature of the interaction of substrate with residues in the drug-binding site(s).
To identify specific residues that line the drug-binding pocket, we used the Cys-less mutant of human P-gp to generate single cysteine mutants that were then reacted with a thiol-reactive substrate. P-gp contains seven endogenous cysteines (positions 137,431, 717, 956, 1077, 1125 and 1227) and removal of all the cysteines (Cys-less P-gp) still results in an active protein. Cysteines can then be introduced into the protein at most positions without significant loss of activity. Mutations that cause misfolding of P-gp such that they are retained in the endoplasmic reticulum (misprocessed) can be “rescued” with drug substrates such as cyclosporin A or verapamil, that act as specific chemical/pharmacological chaperones. The rescued proteins are correctly targeted to the plasma membrane and are active (Loo & Clarke, 1997a; Loo, Bartlett & Clarke, 2004d). Initially, we generated a library of 252 single cysteine mutants that represented every position in each TM segment of P-gp. Each mutant was then reacted with a thiol-reactive drug substrate such as dibromobimane (Loo & Clarke, 1997c, 1999a, 2000b), or a thiol-reactive analogue of a drug substrate, such as methanethiosulfonate (MTS)-verapamil (Loo & Clarke, 2001b) or MTS-rhodamine (Loo & Clarke, 2002a). The thiol-reactive compound was removed and the modified mutant was then assayed for drug-stimulated ATPase activity and compared to a sample that was not treated with thiol-reactive compound. Binding of drug substrate to P-gp can be easily tested because substrates can stimulate the ATPase activity of P-gp up to 20-fold (Loo & Clarke, 2001b). Finally, the mutants that were inhibited by reaction with thiol-reactive compounds were tested for protection by drug substrates. The rationale was that if a residue in the drug-binding pocket was modified by the thiol-reactive analogue of a drug substrate, then the presence of the drug substrate in the drug-binding pocket should protect the residue from being labeled. Similarly, different drug substrates could also inhibit labeling of a particular residue(s) in the drug-binding pocket if those residues are involved in the binding of many different drug substrates. The results from these thiol-modification and protection studies show that TMs 4,5,6 in TMD1 and TMs 9,10,11 and 12 in TMD2 contribute residues to the drug-binding pocket. An interesting observation was that some common residues in these TMs were labeled by dibromobimane, MTS-verapamil or MTS-rhodamine and protected by drug substrates. These results point to the presence of a common drug-binding pocket at the interface between TMD1 and TMD2 and that some residues could commonly be used in the binding of different drug substrates. Recently, Pleban et al. (2005) used a series of propafenone-type substrate photoaffinity ligands in conjunction with matrix-assisted laser desorption/ionization time-of-flight mass spectrometry to confirm that the drug-binding pocket is at the interface between TMD1 and TMD2.
We then proposed the “substrate-induced fit” mechanism to account for studies that predicted the presence of multiple drug-binding sites in P-gp (Loo & Clarke, 2000b). In this mechanism, a substrate could create its own binding site in the common drug-binding pocket by using a combination of residues from different TMs. Evidence for such an “induced-fit” mechanism has been obtained from cross-linking studies that show that some substrates promote cross-linking between particular residues in TMD1 and TMD2 while others either inhibit or have no effect on cross-linking (Loo, Bartlett & Clarke, 2003e; Loo & Clarke, 2000c). Inherently, the affinity of P-gp for a particular substrate would depend on the number and types of residues involved in its binding. Also, the TMs contributing to the drug-binding pocket must be quite mobile for a drug substrate to be able to form its own binding site. This is supported by cross-linking studies that showed that the number of cross-links between the TM segments was significantly reduced when thermal motion was decreased (4°C) (Loo & Clarke, 2000c).
The presence of a relatively large common drug-binding pocket formed at the interface between the TMDs and drug binding through an induced-fit mechanism may explain results from earlier mutational analysis studies of P-gp. These studies showed that discrete mutations within the TMs could alter affinity of P-gp for one drug substrate and not another. For example, mutation of Pro223 to alanine in TM 4 decreased the affinity of P-gp for colchicine but not vinblastine (Loo & Clarke, 1993b) while mutation of Phe335 to alanine decreased the affinity of P-gp for vinblastine but not for colchicine (Loo & Clarke, 1993a, 1994b). Similarly, mutation of residues outside the TMs that contribute to the drug-binding pocket also affected the affinity of P-gp. Mutation of Glyl85 (Choi et al., 1988) and other glycines in the intracellular loops (Loo & Clarke, 1994a) increased the affinity of P-gp for colchicine but not vinblastine. These discrete mutations likely affect the binding affinity through subtle changes in the TM segments such that different residues are exposed to the binding pocket and/or alter the mobility of a particular TM segment and thus restricting or enhancing (Omote et al., 2004) the ability of the drug substrate to fit into the pocket. Drug substrates that are not affected by these mutations likely do not use these residues/TMs for binding.
It was interesting that labeling of residues I306C(TM5) and F343C(TM6) by MTS-verapamil (Loo, Bartlett & Clarke, 2003c) and MTS-rhodamine (Loo, Bartlett & Clarke, 2003b) respectively, resulted in permanent activation of ATPase activity. These results were interpreted as covalent attachment of verapamil to Cys-306 or rhodamine to Cys-343, mimicking binding of verapamil or rhodamine to P-gp during the transport cycle, but vectorial transport has now been uncoupled from ATPase activity. Recently, Tran et al., (2005) determined that only 1 in 10,000 aprenavir, 1 in 30,000 quinidine and 1 in 5,000,000 loperamide that entered the drug-binding pocket was effluxed. The authors concluded that many molecules of drug substrates enter the drug-binding site/pocket but only the occasional bound substrate is transported. These results would then support the idea that a substrate can bind in more than one orientation in the common drug-binding pocket, but binding in only a particular orientation causes activation of ATPase activity and initiation of drug efflux. This may also explain why modification of some residues results in inhibition of ATPase activity, while modification of other residues results in activation of ATPase activity (Loo & Clarke, 2000b, 2001b, 2002a). Similar findings have been reported for the human xenobiotic nuclear receptor PXR. Crystal structure studies of PXR complexed with drug substrate showed that the substrate could assume multiple orientations in a large drug-binding pocket (Watkins et al., 2001).
What is the nature of the common drug-binding pocket? A model of the sites of interaction between the two TMDs is shown in Fig. 1B. This model is based on the results from disulfide cross-linking analysis of the drug-binding domain. These studies suggest the presence of a relatively large drug-binding pocket that is surrounded by a ring of TM segments (Loo, Bartlett & Clarke, 2004a, Loo & Clarke, 2004c, 2000a, 2000c). The drug-binding pocket is funnel shaped—narrow at the cytoplasmic end, 9–15 Å in the middle and wider still at the extracellular side (Loo & Clarke, 2001c). Similarly, Sauna et al. (2004) showed that stipiamide dimmers of 11–33 Å could fit in the drug-binding pocket. Results from low-resolution cryo-electron microscopy structures of P-gp indicate the presence of a relatively large chamber within P-gp when viewed from the extracellular side (Rosenberg et al., 1997).
The presence of such a large chamber suggested that the drug-binding pocket could accommodate more than one drug molecule. Cysteine-scanning mutagenesis and thiol-reactive compounds have been used to show that the P-gp drug-binding pocket can bind two different compounds simultaneously (Loo, Bartlett & Clarke, 2003d). A high-resolution crystal structure of a mammalian ABC-type multidrug transporter is unavailable. The high-resolution structure of the Escherichia coli proton-motive AcrB multidrug efflux pump, however, may provide clues about the structure of the drug-binding domain of P-gp (Murakami et al., 2002; Yu et al., 2003). The crystal structure of AcrB shows the presence of a large cavity (500 cubic Å) surrounded by α-helices. The chamber was large enough to bind several molecules at the same time.
The crystal structures of drug-binding regulatory proteins such as Bacillus subtilus transcriptional activator BmrR (Heldwein & Brennan, 2001) and Staphylococcus aureus represser QacR (Schumacher et al., 2001) also provide clues about the structures of multidrug-binding domains. The crystal structures of QacR showed the presence of separate but linked binding sites within one extended, multifaceted drug-binding domain (Schumacher et al., 2001).
How do substrates enter the common drug-binding pocket of P-gp? It has been proposed in the “vacuum cleaner” model for P-gp that the drug substrate becomes dehydrated as it diffuses from the extracellular medium into the lipid bilayer. P-gp then extracts the substrate from the lipid bilayer (Homolya et al., 1993; Raviv et al., 1990). Therefore, there must be portals/gates for entry of drug substrate from the lipid bilayer into the drug-binding pocket. It has been postulated that the drug substrates enter the drug-binding pocket through “gates” formed at the interface between TMD1 and TMD2 (Loo & Clarke, 2005; Pleban et al., 2005). The predicted gates/portals are formed between TM2 (in TMD1) and TM11 (in TMD2) at one end of the drug-binding pocket and between TM5 (in TMD1) and TM8 (in TMD2) at the other end. These TM segments were predicted from cross-linking studies to be close to each other (Stenham et al., 2003; Loo et al., 2004a, 2004c). In studies involving modification of cysteine residues with thiol-reactive substrates, it was found that the majority (>75%) of the residues that could not be protected from thiol-modification by drug substrates were concentrated in TMs 2, 5, 8 and 11. When the residues in TMs 2, 5, 8 and 11 are arranged as α-helical wheels, these non-protectable residues faced away from the common drug-binding pocket (Loo & Clarke, 2005). It was possible that these residues were not protected by substrates because of continuous flow of substrate past these residues. This would be consistent with the results from a recent study indicating “free flow” of drug substrates into the drug-binding pocket and subsequent transport of very few of these molecules (Tran et al., 2005). The drug molecules that were not transported were postulated to escape back into the apical membrane inner monolayer (Tran et al., 2005). The presence of gates/portals is also suggested from the studies of the bacterial ABC lipid transporter, MsbA (Reyes & Chang, 2005).
Coupling of ATP Hydrolysis to Drug Efflux
The next step in the transport cycle is ATP-dependent release of drug substrate into the extracellular medium. That P-gp has the ability to efflux drug substrates out of the lipid bilayer has been shown because purified hamster P-gp can actively generate a 5.6-fold concentration gradient of colchicine in reconstituted lipid vesicles (Sharom, Yu & Doige, 1993). Similarly, P-gp could transport spin-labeled verapamil into vesicles and generate at least a 13-fold gradient between the luminal and outside aqueous phases (Omote & Al-Shawi, 2002).
P-gp contains two NBDs. Both NBDs can bind and hydrolyze ATP (Loo & Clarke, 1994d; Urbatsch et al., 1995a). Both ATP-binding sites of hamster P-gp have low affinities for ATP (Km for Mg.ATP is about 0.8 mM) (Urbatsch, al-Shawi & Senior, 1994). Covalent modification of the cysteine residue within the Walker A site (GNSGCGKS in NBD1 and GSSGCGKS in NBD2) of either NBD (Doige, Yu & Sharom, 1992; al-Shawi & Senior, 1993; Loo & Clarke, 1995a), however, inhibits the activity of P-gp. Similarly, vanadate trapping of nucleotide by either NBD inactivates P-gp (Urbatsch et al., 1995b). Recent thermodynamic calculations indicate that hydrolysis of one ATP molecule is sufficient to efflux drug substrate (Al-Shawi et al., 2003) thus supporting the proposal that ATP hydrolysis occurs through an alternating site mechanism (Senior et al., 1995).
It has been proposed that the ATP sites of human P-gp are not identical (i.e., are asymmetric) (Hrycyna et al., 1998, 1999). This conclusion was based on the observation that the NH2- and COOH- halves of P-gp were differentially labeled with [α- 32P]-8-azido-ATP. There were, however, technical problems with these studies, as the amount of ATP used and the amount of photo-cleavage obtained (about 10%) were substoichiometric.
Evidence from disulfide cross-linking studies (Loo & Clarke, 2000a; Urbatsch et al., 2001; Loo, Bartlett & Clarke 2002, 2003a), fluorescence resonance energy transfer (FRET) studies (Qu & Sharom, 2001) and cryo-electron microscopy studies (Lee et al., 2002; Rosenberg et al., 2001) of P-gp suggests that the two catalytic sites are close to each other. Such close proximity can be demonstrated by cross-linking the endogenous cysteine residue within each Walker A site with a cysteine introduced into the “LSGGQ” signature sequence in the opposing NBD (Loo et al., 2002). Therefore, the two ATP molecules appear to bind at the interface between the two NBDs. The crystal structures of several bacterial ABC-type proteins, such as the DNA repair enzyme Rad50 (Hopfner et al., 2000), the bacterial vitamin B12 transporter BtuCD (Locher, Lee & Rees, 2002), the bacterial lipid transporter MsbA (Chang, 2003) and the inactive NBD of Methanococcus jannaschii MJ0796 (Smith et al., 2002) also show that the signature sequences are close to the Walker A sites and contribute to ATP binding. Analysis of the contact sites between the NBDs of BtuCD (Locher et al., 2002) shows that few interactions occur outside the Walker A/LSGGQ signature sites. Because these structures are only snapshots of a particular (resting) state, it is possible that other interactions between the NBDs may occur during the transport cycle.
P-gp has low basal ATPase activity in the absence of any drug substrate (Sarkadi et al., 1992). Several studies have suggested that P-gp may be able to transport certain lipids such as phosphatidylcholine, phosphatidylethanolamine, phosphatidylserine or sphingomyelin (Romsicki & Sharom, 2001). Thermodynamic studies on P-gp, however, suggest that the basal ATPase activity is an intrinsic property of the protein and is not due to transport of an endogenous lipid (Al-Shawi et al., 2003).
The basal ATPase activity of P-gp can be stimulated more than 20-fold upon binding of a drug substrate (Ambudkar et al., 1992; Doige et al., 1992; Sarkadi et al., 1992; Loo & Clarke, 1999a). Coupling of ATPase activity to drug binding indicates cross talk between the drug-binding pocket and the ATP-binding sites. To test for cross talk between the TMDs and NBDs, we examined the effect of drug binding on disulfide cross-linking between the cysteines located in the opposing Walker A and LSGGQ signature sites. It was shown that substrates that stimulated the ATPase activity of P-gp (e.g., verapamil, demecolcine and calcein-AM) increased the rate of cross-linking at both ATP-binding sites compared to cross-linking in the absence of drug substrate. By contrast, substrates such as Hoechst 33342 and cyclosporin A that inhibited ATPase activity, decreased the rate of cross-linking (Loo et al., 2003a). These results show that binding of drug substrate in the TMDs causes long-range conformational changes at the interfaces between the NBDs and thus controls the rate of hydrolysis. Such long-range conformational changes are supported by FRET analysis measurements that show that the ATP-binding sites and the drug-binding sites are at least 38 Å apart (Lugo & Sharom, 2005; Qu & Sharom, 2002).
ATP binding and hydrolysis then cause conformational changes in the TMDs (Loo & Clarke, 1997b, 2001a, 2002b; Mechetner et al., 1997; Sonveaux et al., 1999; Druley, Stein & Roninson, 2001; Rosenberg et al., 2001, 2005). It is still controversial whether ATP binding or ATP hydrolysis causes the greatest conformational changes in the TMDs. Several groups have used biochemical methods to show that ATP hydrolysis rather than binding of nucleotide causes conformational changes (Loo & Clarke, 1997b; Vigano et al., 2002; Al-Shawi et al., 2003; Qu, Chu & Sharom, 2003; Loo, Bartlett & Clarke, 2005). Cryo-electron microscopy of P-gp, however, shows that binding of AMP.PNP can cause large conformational changes in the TMDs (Rosenberg et al., 2005; Rosenberg et al., 2003). It is possible that both ATP binding and hydrolysis may cause distinct conformational changes in the TMDs. Both nucleotide binding and vanadate trapping of nucleotide by P-gp can affect labeling of residues in the drug-binding pocket (Rothnie et al., 2004; Loo & Clarke, 2002b). Therefore, it is possible that ATP binding together with substrate binding (through the induced-fit mechanism) may close the gates/portal to the drug-binding pocket while ATP hydrolysis causes rearrangement of the TM segments that facilitates release of drug substrate from P-gp.
MsbA, an ABC transporter from Escherichia coli is a lipid flippase. Its primary sequence shows 30% homology with P-gp. The initial crystal structure of MsbA showed that the NBDs were relatively far apart (50 Å; open state) and it was suggested that ATP hydrolysis brings them close together (Chang & Roth, 2001). More recent studies on the MsbA of Vibrio cholera, however, indicate that the two NBDs are close together (closed state) in the absence of nucleotide (Chang, 2003). How do these states correlate with that found in P-gp? Recent results from cross-linking studies indicate that the NBDs are close together in the absence of nucleotide. The conserved cysteine residue in the Walker A site in one NBD can be cross-linked to cysteines introduced into the Walker A site in the second NBD (Loo & Clarke, 2000a; Urbatsch et al., 2001). Cryo-electron microscopy studies of P-gp crystals in a lipid bilayer also indicate that the two NBDs are close together in the closed conformation in the absence of nucleotides (Lee et al., 2002). Therefore, the evidence clearly favors the NBDs of P-gp being close together (closed conformation) in the absence of nucleotide. In this respect, the orientation of the NBDs of P-gp may more closely resemble the crystal structure of the ABC transporter from Escherichia coli, BtuCD, which mediates vitamin B12 uptake (Locher et al., 2002). BtuCD consists of two TMDs (BtuC) and two NBDs (BtuD). The crystal structure of BtuCD in the nucleotide-free state shows that the two NBDs are aligned in a side-by-side arrangement in which the Walker A site of one subunit is directly across from the LSGGQ signature sequence of the second opposing subunit. This arrangement places the two ATP-binding sites between the NBDs. The formation of the correct interface between the NBDs appears to be critical for function. For example, mutation of the serine residues in the LSGGQ signature sequences affects the enzyme activity not by inhibiting Mg.ATP binding or release of Mg.ADP, but by hindering the formation of a catalytically productive NBD dimer (Loo et al., 2002; Tombline et al., 2004a). Mutation of each serine residue to alanine reduced the ATPase activity by 25%, while mutation of both serine residues resulted in almost complete inhibition of activity (Tombline et al., 2004a). Therefore, it appears that there is “co-operativity” between the NBDs to accommodate the two ATP molecules at the NBD dimer interface (Tombline et al., 2004a).
Some mutations in the NBDs appear to inhibit P-gp activity by promoting formation and stabilization of the NBD dimer, which then occludes nucleotide. An example is mutation of the putative “catalytic carboxylate” glutamate residues (E556 in NBD1 and E1202 in NBD2 of P-gp) within the Walker B sites. Mutation of residues E556 and E1202 to alanines inhibited P-gp ATPase activity (Sauna et al., 2002). Similarly, mutation of the equivalent residues in mouse MDR3 (E552A/E1197A) essentially abolished the activity of the enzyme (Tombline et al., 2004b, 2004c). It appears that the mutations inhibited activity by stabilizing dimer formation so that there is occlusion of bound nucleotide. Mutation of the equivalent glutamate residue in other ABC transporters, such as MJ0796 and MJ1267 from Methanococcus jannaschii (Karpowich et al., 2001; Yuan et al., 2001; Moody et al., 2002) and mitochondrial Mdl1p (Janas et al., 2003) also caused ATP-dependent dimerization of the NBDs.
Conformational Changes During the Transport Cycle
Interaction of ATP at the NBDs leads to drug efflux by shifting the drug-binding sites from a high-affinity to a low-affinity state. Since the common drug-binding pocket is relatively large and substrates bind through an induced-fit mechanism, the release of drug substrate will require conformational changes in the drug-binding pocket. Global changes in P-gp structure upon nucleotide binding have been detected spectroscopically (Sonveaux et al., 1999) and by cryo-electron microscopy (Rosenberg et al., 2005).
Conformational changes in the TM segments surrounding the common drug-binding pocket have also been detected using cysteine-scanning mutagenesis and thiol-reactive compounds. Initial studies on conformational changes in P-gp were concentrated around TM 6 and TM12 because both TMs contribute residues to the drug-binding pocket (Loo & Clarke, 1997c; Loo et al., 2003b). During ATP hydrolysis, conformational changes between TM6 and TM12 were detected by disulfide cross-linking between cysteines introduced at the extracellular ends of these TMs (residue L332C in TM6 and L975C in TM12) (Loo & Clarke, 1996a, 1997b). Cross-linking between L332C/L975C prevented conformational changes during ATP hydrolysis, resulting in inhibition of ATPase activity. The activity was restored, however, when the disulfide bond was broken with the reducing agent, dithiothreitol. Involvement of TM12 in conformational changes was also detected using a monoclonal antibody (Mechetner et al., 1997). It was subsequently shown through trapping of intermediates with the cross-linker substrate Tris-(2-maleimidoethyl)amine (TMEA), that ATP hydrolysis moved TM6 with respect to TM12 (Loo & Clarke, 2001a). In this study, it was shown that a cysteine in TM12 (Cys982) could be cross-linked to Cys339 in TM6 with TMEA. In the presence of ATP however, Cys982(TM12) could now be cross-linked to Cys343(TM6). The residues in TM6 and TM12 when arranged in α-helical wheels indicate that ATP hydrolysis caused TM6 to rotate and/or move laterally with respect to TM12.
Vanadate trapping of nucleotide also affected the pattern of cross-linking between cysteines in TM6 and other TMs (see Fig. 2). In the absence of nucleotide, residue Cys332(TM6) was cross-linked to Cys856(TM10) with a methanethiosulfonate (MTS)-type cross-linker substrate (M8M) (Loo & Clarke, 2002b). The cross-linking was inhibited upon vanadate trapping of nucleotide. Instead, Cys332(TM6) was now cross-linked to Cys976(TM12) with a smaller length MTS-type cross-linker substrate (M6M). Similarly, Rothnie et al. (2004) used fluorescence labeling to show that the pattern of labeling of cysteine residues introduced into TM6 changed in the basal state, when bound to AMP.PNP or during vanadate trapping of nucleotide. The results from these studies are consistent with the proposal that ATP binding causes changes in the TMs, while ATP hydrolysis results in rearrangement of the TMs surrounding the drug-binding pocket. Rearrangement of the TMs may shift the drug-binding site(s) to a low-affinity state with concomitant release of drug substrate.
Another reason that ATP hydrolysis may lead to drug release is because of potential hydration of the drug substrate. It has been postulated that the drug substrate becomes dehydrated upon entering the lipid bilayer (Raviv et al., 1990). The drug substrate diffuses into the common drug-binding pocket where it may be rehydrated before release into the extracellular medium. Recently, it was shown that the drug-binding pocket is accessible to the aqueous medium (Loo, Bartlett & Clarke, 2004b). This is consistent with cryo-electron microscopy studies that show the presence of a large chamber within P-gp that is open to the extracellular medium (Rosenberg et al., 1997) and the finding that a residue predicted to be within the drug-binding pocket (Cys343 in TM6) could be labeled with a hydrophilic thiol probe (Rothnie et al., 2004). Labeling of residues in the drug-binding pocket with the hydrophilic compound MTSES was enhanced during ATP hydrolysis (Loo et al., 2004b). This result suggested that the drug-binding pocket becomes more accessible to water during ATP hydrolysis. Rehydration of substrate must be an important step during the transport cycle, as it may prevent diffusion of the substrate back into the lipid bilayer and prepares the substrate to be released into an aqueous environment. Recent studies on MsbA also indicate that the entry of substrate into a solvent-filled internal chamber is a critical for transport (Dong, Yang & McHaourab, 2005; Reyes & Chang, 2005).
The exact mechanism of drug release by P-gp remains controversial. It was initially shown that photo-labeling of P-gp with the substrate analogue [125I]-iodoarylazidoprazosin (IAAP) was significantly reduced in the vanadate-trapped state (Ramachandra et al., 1998; Sauna & Ambudkar, 2000). A model was then proposed whereby ATP hydrolysis moved the drug substrate from an “ON” to an “OFF” site in P-gp (Ramachandra et al., 1998; Sauna & Ambudkar, 2000). By contrast, Qu et al. (2003) reported that the vanadate-trapped P-gp showed little change in affinity for a variety of drug substrates when compared to P-gp in the resting state. These authors proposed that P-gp operates by a concerted transport mechanism whereby release of drug substrate from the transporter precedes formation of the transition state. The results from studies using cross-linkable drug substrates supports the notion of an “ON to OFF” state during ATP hydrolysis because of significant rearrangement of the TMs surrounding the common drug-binding pocket, resulting in a change in the binding of the drug substrate (Loo & Clarke, 1997b, (2002b).
Another aspect of the mechanism of P-gp that needs resolving is the controversy of whether the drug substrates are transported directly out of the lipid bilayer or P-gp merely acts as a flippase to transport the substrate from the inner leaflet to the outer leaflet of the bilayer (Higgins & Gottesman, 1992). It has been demonstrated through electron paramagnetic resonance (EPR) studies with spin-labeled verapamil that P-gp reconstituted into vesicles can actively generate up to a 25-fold aqueous phase gradient (Omote & Al-Shawi, 2002). These results suggest that substrate is being actively transported out of the lipid bilayer. The results from FRET studies with nitrobenzo-2-oxa-1,3-diazole-labeled glycosphingolipids and phospholipids, however, suggest that P-gp acts as an outwardly-directed flippase (Romsicki & Sharom, 2001; Eckford & Sharom, 2005). Perhaps, P-gp functions both as a transporter and a flippase. It may be possible to reconcile both functions of P-gp. It is possible that P-gp transports glycosphingolipids/phospholipids out of the inner leaflet and into the extracellular medium. The transported glycosphingolipids/phospholipids in the external medium, however, may exist very transiently. Their hydrophobic nature may result in immediate diffusion back into the outer leaflet of the bilayer and thus making P-gp appear to function as a flippase. Therefore, stopped-flow methods and methods to capture the transiently exported lipid will have to be developed to test for these possibilities.
A potential problem with the studies using labeled glycosphingolipids and phospholipids is that the label (e.g., nitrobenzo-2-oxa-1,3-diazole) may convert the glycosphingolipids/phospholipids into a substrate of P-gp. If P-gp is indeed involved with lipid through transport or flippase activity, its interactions with lipid must be quite different from those involving drug substrates. For example, mutations can be introduced throughout different domains of P-gp that result in misfolding of the protein. The misfolded protein is recognized by the quality control mechanism in the endoplasmic reticulum (ER) and retained in the ER as a core-glycosylated intermediate with a shortened half-life (Loo & Clarke, 1994c). Addition of drug substrates during synthesis of the misfolded proteins rescues the proteins such that they become properly folded and are transported to the plasma membrane in an active form (Loo & Clarke, 1997a; Loo et al., 2004d). A possible mechanism for rescuing the misfolded mutants is that the drug-binding pocket is formed early in the folding intermediate during biosynthesis. The presence of drug substrate in the binding pocket may stabilize the folding intermediate in a “near-native’ conformation to allow proper folding of the complete molecule and thus allowing it to escape the cell’s quality control mechanism. The transient drug-binding pocket collapses in the absence of drug substrate and results in misfolding. This may explain why misfolded P-gp mutants, when isolated by nickel-chelate chromatography, cannot be rescued with drug substrate (unpublished data). Therefore, if natural lipids were indeed substrates of P-gp, then misfolded P-gp mutants should not have been detected.
In summary, many aspects of the structure and mechanism of P-gp have been determined. Many important goals, however, still need to be addressed. These include:
-
1.
Determining why ATP hydrolysis occurs at alternating sites. Other ABC transporters such as MRP only seem to require ATP hydrolysis at one site (Borges-Walmsley, McKeegan & Walmsley, 2003), although more work is needed on this subject.
-
2.
Determining the conformational changes in the drug-binding site during ATP binding and ATP hydrolysis.
-
3.
Determining the contribution of the large intracellular loops to the transport mechanism.
-
4.
Determining the interactions among the different domains of Pgp during the transport cycle.
-
5.
Determining the crystal structure of P-gp.
Abbreviations
- M6M,:
-
1,6-hexanediyl bismethanethiosulfonate;
- M8M,:
-
3,6-dioxaoctane-1,8-diyl bismethanethiosulfonate;
- NBD1,:
-
amino-terminal nucleotide binding domain;
- NBD2,:
-
carboxy-terminal nucleotide binding domain;
- P-gp,:
-
P-glycoprotein;
- TMD,:
-
transmembrane domain;
- TM,:
-
transmembrane
References
Al-Shawi M.K., Polar M.K., Omote H., Figler R.A. 2003. Transition state analysis of the coupling of drug transport to ATP hydrolysis by P-glycoprotein. J. Biol. Chem. 278:52629–52640
al-Shawi M.K., Senior A.E. 1993. Characterization of the adenosine triphosphatase activity of Chinese hamster P-glycoprotein. J. Biol. Chem. 268:4197–4206
Alien J.D., Brinkhuis R.F., Wijnholds J., Schinkel A.H. 1999. The mouse Bcrp1/Mxr/Abcp gene: amplification and overexpression in cell lines selected for resistance to topotecan, mitoxantrone, or doxorubicin. Cancer Res. 59:4237–4241
Allikmets R., Schriml L.M., Hutchinson A., Romano-Spica V., Dean M. 1998. A human placenta-specific ATP-binding cassette gene (ABCP) on chromosome 4q22 that is involved in multidrug resistance. Cancer Res. 58:5337–5339
Ambudkar S.V., Kimchi-Sarfaty C., Sauna Z.E., Gottesman M.M. 2003. P-glycoprotein: from genomics to mechanism. Oncogene 22:7468–7485
Ambudkar S.V., Lelong I.H., Zhang J., Cardarelli C.O., Gottesman M.M., Pastan. 1992. Partial purification and reconstitution of the human multidrug- resistance pump: characterization of the drug-stimulatable ATP hydrolysis. Proc. Natl. Acad. Sci. USA 89:8472–8476
Biedler J.L., Riehm H. 1970. Cellular resistance to actinomycin D in Chinese hamster cells in vitro: cross-resistance, radioautographic, and cytogenetic studies. Cancer Res. 30:1174–1184
Borges-Walmsley M.I., McKeegan K.S., Walmsley A.R. 2003. Structure and function of efflux pumps that confer resistance to drugs. Biochem. J. 376:313–338
Bruggemann E.P., Currier S.J., Gottesman M.M., Pastan I. 1992. Characterization of the azidopine and vinblastine binding site of P-glycoprotein. J. Biol. Chem. 267:21020–21026
Chang G. 2003. Structure of MsbA from Vibrio cholera: A Multidrug Resistance ABC transporter Homolog in a Closed Conformation. J. Mol. Biol. 330:419–430
Chang G., Roth C.B. 2001. Structure of MsbA from E. coli: a homolog of the multidrug resistance ATP binding cassette (ABC) transporters. Science 293:1793–1800
Chen C.J., Chin J.E., Ueda K., Clark D.P., Pastan I., Gottesman M.M., Roninson I.B. 1986. Internal duplication and homology with bacterial transport proteins in the mdrl (P-glycoprotein) gene from multidrug-resistant human cells. Cell 47:381–389
Chen J.H., Chang X.B., Aleksandrov A.A., Riordan J.R. 2002. CFTR is a monomer: biochemical and functional evidence. J. Membrane Biol. 188:55–71
Choi K.H., Chen C.J., Kriegler M., Roninson I.B. 1988. An altered pattern of cross-resistance in multidrug-resistant human cells results from spontaneous mutations in the mdr1 (P-glycoprotein) gene. Cell 53:519–529
Dano K. 1972. Cross resistance between vinca alkaloids and anthracyclines in Ehrlich ascites tumor in vivo. Cancer Chemother. Rep. 56:701–708
Dean M., Rzhetsky A., Allikmets R. 2001. The human ATP-binding cassette (ABC) transporter superfamily. Genome Res. 11:1156–1166
Dearden J.C., A1-Noobi A., Scott A.C., Thomson S.A. 2003. QSAR studies on P-glycoprotein-regulated multidrug resistance and on its reversal by phenothiazines. SAR QSAR Environ. Res. 14:447–454
Demeule M., Laplante A., Murphy G.F., Wenger R.M., Beliveau R. 1998. Identification of the cyclosporin-binding site in P-glycoprotein. Biochemistry 37:18110–18118
Demmer A., Thole H., Kubesch P., Brandt T., Raida M., Fislage R., Tummler B. 1997. Localization of the iodomycin binding site in hamster P-glycoprotein. J. Biol. Chem. 272:20913–20919
Dey S., Ramachandra M., Pastan I., Gottesman M.M., Ambudkar S.V. 1997. Evidence for two nonidentical drug-interaction sites in the human P-glycoprotein. Proc. Natl. Acad. Sci. USA 94:10594–10599
Doige C.A., Yu X., Sharom F.J. 1992. ATPase activity of partially purified P-glycoprotein from multidrug- resistant Chinese hamster ovary cells. Biochim. Biophys. Acta. 1109:149–160
Dong J., Yang G., McHaourab H.S. 2005. Structural basis of energy transduction in the transport cycle of MsbA. Science 308:1023–1028
Doyle L.A., Yang W., Abruzzo L.V., Krogmann T., Gao Y., Rishi A.K., Ross D.D. 1998. A multidrug resistance transporter from human MCF-7 breast cancer cells. Proc. Natl. Acad. Sci. USA 95:15665–15670
Druley T.E., Stein W.D., Roninson I.B. 2001. Analysis of mdr1 p-glycoprotein conformational changes in permeabilized cells using differential immunoreactivity. Biochemistry 40:4312–4322
Eckford P.D., Sharom F.J. 2005. The reconstituted P-glycoprotein multidrug transporter is a flippase for glucosylceramide and other simple glycosphingolipids. Biochem. J. 389: 517–526
Ekins S., Kim R.B., Leake B.F., Dantzig A.H., Schuetz E.G., Lan L.B., Yasuda K., Shepard R.L., Winter M.A., Schuetz J.D., Wikel J.H., Wrighton S.A. 2002. Application of three-dimensional quantitative structure-activity relationships of P-glycoprotein inhibitors and substrates. Mol. Pharmacol. 61:974–981
Garrigues A., Loiseau N., Delaforge M., Ferte J., Garrigos M., Andre F., Orlowski S. 2002. Characterization of two pharmacophores on the multidrug transporter P-glycoprotein. Mol. Pharmacol. 62:1288–1298
Gerlach J.H., Endicott J.A., Juranka P.F., Henderson G., Sarangi F., Deuchars K.L., Ling V. 1986. Homology between P-glycoprotein and a bacterial haemolysin transport protein suggests a model for multidrug resistance. Nature 324:485–489
Gottesman M.M., Pastan I. 1988. The multidrug transporter, a double-edged sword. J. Biol. Chem. 263:12163–12166
Gottesman M.M., Pastan I. 1993. Biochemistry of multidrug resistance mediated by the multidrug transporter. Annu. Rev. Biochem. 62:385–427
Graf G.A., Yu L., Li W.P., Gerard R., Tuma P.L., Cohen J.C., Hobbs H.H. 2003. ABCG5 and ABCG8 are obligate heterodimers for protein trafficking and biliary cholesterol excretion. J. Biol. Chem. 278:48275–48282
Greenberger L.M. 1993. Major photoaffinity drug labeling sites for iodoaryl azidoprazosin in P- glycoprotein are within, or immediately C-terminal to, transmembrane domains 6 and 12. J. Biol. Chem. 268:11417–11425
Gros P., Ben Neriah Y.B., Croop J.M., Housman D.E. 1986. Isolation and expression of a complementary DNA that confers multidrug resistance. Nature 323:728–731
Heldwein E.E., Brennan R.G. 2001. Crystal structure of the transcription activator BmrR bound to DNA and a drug. Nature 409:378–82
Higgins C.F. 1992. ABC transporters: from microorganisms to man. Annu. Rev. Cell Biol. 8:67–113
Higgins C.F., Gottesman M.M. 1992. Is the multidrug transporter a flippase? Trends. Biochem. Sci. 17:18–21
Homolya L., Hollo Z., Germann U.A., Pastan I., Gottesman M.M., Sarkadi B. 1993. Fluorescent cellular indicators are extruded by the multidrug resistance protein. J. Biol. Chem. 268:21493–21496
Hopfner K.P., Karcher A., Shin D.S., Craig L., Arthur L.M., Carney J.P., Tainer J.A. 2000. Structural biology of Rad50 ATPase: ATP-driven conformational control in DNA double-strand break repair and the ABC-ATPase superfamily. Cell 101:789–800
Hrycyna C.A. 2001. Molecular genetic analysis and biochemical characterization of mammalian P-glycoproteins involved in multidrug resistance. Semin. Cell Dev. Biol. 12:247–256
Hrycyna C.A., Ramachandra M., Ambudkar S.V., Ko Y.H., Pedersen P.L., Pastan I., Gottesman M.M. 1998. Mechanism of action of human P-glycoprotein ATPase activity. Photochemical cleavage during a catalytic transition state using orthovanadate reveals cross-talk between the two ATP sites. J. Biol. Chem. 273:16631–16634
Hrycyna C.A., Ramachandra M., Germann U.A., Cheng P.W., Pastan I., Gottesman M.M. 1999. Both ATP sites of human P-glycoprotein are essential but not symmetric. Biochemistry 38:13887–13899
Janas E., Hofacker M., Chen M., Gompf S., van der Does C., Tampe R. 2003. The ATP hydrolysis cycle of the nucleotide-binding domain of the mitochondrial ATP-binding cassette transporter Mdllp. J. Biol. Chem. 278:26862–26869
Juliano R.L., Ling V. 1976. A surface glycoprotein modulating drug permeability in Chinese hamster ovary cell mutants. Biochim. Biophys. Acta 455:152–162
Karpowich N., Martsinkevich O., Millen L., Yuan Y.R., Dai P.L., MacVey K., Thomas P.J., Hunt J.F. 2001. Crystal structures of the MJ1267 ATP binding cassette reveal an induced- fit effect at the ATPase active site of an ABC transporter. Structure (Camb) 9:571–586
Kast C., Canfield V., Levenson R., Gros P. 1996. Transmembrane organization of mouse P-glycoprotein determined by epitope insertion and immunofluorescence. J. Biol. Chem. 271:9240–9248
Lee C.G., Gottesman M.M., Cardarelli C.O., Ramachandra M., Jeang K.T., Ambudkar S.V., Pastan I., Dey S. 1998. HIV-1 protease inhibitors are substrates for the MDR1 multidrug transporter. Biochemistry 37:3594–3601
Lee J.Y., Urbatsch I.L., Senior A.E., Wilkens S. 2002. Projection structure of P-glycoprotein by electron microscopy. Evidence for a closed conformation of the nucleotide binding domains. J. Biol. Chem. 271:40125–40131
Leith C.P., Kopecky K.J., Chen I.M., Eijdems L., Slovak M.L., McConnell T.S., Head D.R., Weick J., Grever M.R., Appelbaum F.R., Willman C.L. 1999. Frequency and clinical significance of the expression of the multidrug resistance proteins MDR1/P-glycoprotein, MRP1, and LRP in acute myeloid leukemia: a Southwest Oncology Group Study. Blood 94:1086–1099
Ling V., Thompson L.H. 1974. Reduced permeability in CHO cells as a mechanism of resistance to colchicine. J. Cell Physiol. 83:103–116
Locher K.P., Lee A.T., Rees D.C. 2002. The E. coli BtuCD structure: a framework for ABC transporter architecture and mechanism. Science 296:1091–1098
Loo T.W., Bartlett M.C., Clarke D.M. 2002. The “LSGGQ” motif in each nucleotide-binding domain of human P-glycoprotein is adjacent to the opposing walker A sequence. J. Biol. Chem. 277:41303–41306
Loo T.W., Bartlett M.C., Clarke D.M. 2003a. Drug binding in human P-glycoprotein causes conformational changes in both nucleotide-binding domains. J. Biol. Chem. 278:1575–1578
Loo T.W., Bartlett M.C., Clarke D.M. 2003b. Methanethiosulfonate derivatives of rhodamine and verapamil activate human P-glycoprotein at different sites. J. Biol. Chem. 278:50136–50141
Loo T.W., Bartlett M.C., Clarke D.M. 2003c. Permanent activation of the human p-glycoprotein by covalent modification of a residue in the drug-binding site. J. Biol. Chem. 278:20449–20452
Loo T.W., Bartlett M.C., Clarke D.M. 2003d. Simultaneous binding of two different drugs in the binding pocket of the human multidrug resistance P-glycoprotein. J. Biol. Chem. 278:39706–39710
Loo T.W., Bartlett M.C., Clarke D.M. 2003e. Substrate-induced conformational changes in the transmembrane segments of human P-glycoprotein. Direct evidence for the substrate-induced fit Mechanism for drug binding. J. Biol. Chem. 278:13603–13606
Loo T.W., Bartlett M.C., Clarke D.M. 2004a. Disulfide cross-linking analysis shows that transmembrane segments 5 and 8 of human P-glycoprotein are close together on the cytoplasmic side of the membrane. J. Biol. Chem. 279:7692–7697
Loo T.W., Bartlett M.C., Clarke D.M. 2004b. The drug-binding pocket of the human multidrug resistance P-glycoprotein is accessible to the aqueous medium. Biochemistry 43:12081–12089
Loo T.W., Bartlett M.C., Clarke D.M. 2004c. Residues V133 and C137 in transmembrane segment 2 are close to residues A935 and G939 in transmembrane segment 11 of human P-glycoprotein. J. Biol. Chem. 279:18232–18238
Loo T.W., Bartlett M.C., Clarke D.M. 2004d. Thapsigargin or curcumin does not promote maturation of processing mutants of the ABC transporters, CFTR, and P-glycoprotein. Biochem. Biophys. Res. Commun. 325:580–585
Loo T.W., Bartlett M.C., Clarke D.M. 2005. ATP hydrolysis promotes interactions between the extracellular ends of transmembrane segments 1 and 11 of human multidrug resistance P-glycoprotein. Biochemistry 44:10250–10258
Loo T.W., Clarke D.M. 1993a. Functional consequences of phenylalanine mutations in the predicted transmembrane domain of P-glycoprotein. J. Biol. Chem. 268:19965–19972
Loo T.W., Clarke D.M. 1993b. Functional consequences of proline mutations in the predicted transmembrane domain of P-glycoprotein. J. Biol. Chem. 268:3143–3149
Loo T.W., Clarke D.M. 1994a. Functional consequences of glycine mutations in the predicted cytoplasmic loops of P-glycoprotein. J. Biol. Chem. 269:7243–7248
Loo T.W., Clarke D.M. 1994b. Mutations to amino acids located in predicted transmembrane segment 6 (TM6) modulate the activity and substrate specificity of human P-glycoprotein. Biochemistry 33:14049–14057
Loo T.W., Clarke D.M. 1994c. Prolonged association of temperature-sensitive mutants of human P- glycoprotein with calnexin during biogenesis. J. Biol. Chem. 269:28683–28689
Loo T.W., Clarke D.M. 1994d. Reconstitution of drug-stimulated ATPase activity following co- expression of each half of human P-glycoprotein as separate polypeptides. J. Biol. Chem. 269:7750–7755
Loo T.W., Clarke D.M. 1995a. Covalent modification of human P-glycoprotein mutants containing a single cysteine in either nucleotide-binding fold abolishes drug- stimulated ATPase activity. J. Biol. Chem. 270:22957–22961
Loo T.W., Clarke D.M. 1995b. Membrane topology of a cysteine-less mutant of human P-glycoprotein. J. Biol. Chem. 270:843–848
Loo T.W., Clarke D.M. 1996a. Inhibition of oxidative cross-linking between engineered cysteine residues at positions 332 in predicted transmembrane segments (TM) 6 and 975 in predicted TM12 of human P-glycoprotein by drug substrates. J. Biol. Chem. 271:27482–27487
Loo T.W., Clarke D.M. 1996b. The minimum functional unit of human P-glycoprotein appears to be a monomer. J. Biol. Chem. 271:27488–27492
Loo T.W., Clarke D.M. 1997a. Correction of defective protein kinesis of human P-glycoprotein mutants by substrates and modulators. J. Biol. Chem. 272:709–712
Loo T.W., Clarke D.M. 1997b. Drug-stimulated ATPase activity of human P-glycoprotein requires movement between transmembrane segments 6 and 12. J. Biol. Chem. 272:20986–20989
Loo T.W., Clarke D.M. 1997c. Identification of residues in the drug-binding site of human P- glycoprotein using a thiol-reactive substrate. J. Biol. Chem. 272:31945–31948
Loo T.W., Clarke D.M. 1998. Superfolding of the partially unfolded core-glycosylated intermediate of human P-glycoprotein into the mature enzyme is promoted by substrate- induced transmembrane domain interactions. J. Biol. Chem. 273:14671–14674
Loo T.W., Clarke D.M. 1999a. Identification of residues in the drug-binding domain of human P-glycoprotein: Analysis of transmembrane segment 11 by cysteine-scanning mutagenesis and inhibition by dibromobimane. J. Biol. Chem. 274:35388–35392
Loo T.W., Clarke D.M. 1999b. The transmembrane domains of the human multidrug resistance P- glycoprotein are sufficient to mediate drug binding and trafficking to the cell surface. J. Biol. Chem. 274:24759–24765
Loo T.W., Clarke D.M. 2000a. Drug-stimulated ATPase activity of human P-glycoprotein is blocked by disulfide cross-linking between the nucleotide-binding sites. J. Biol. Chem. 275:19435–19438
Loo T.W., Clarke D.M. 2000b. Identification of residues within the drug-binding domain of the human multidrug resistance P-glycoprotein by cysteine-scanning mutagenesis and reaction with dibromobimane. J. Biol. Chem. 275:39272–39278
Loo T.W., Clarke D.M. 2000c. The packing of the transmembrane segments of human multidrug resistance P-glycoprotein is revealed by disulfide cross-linking analysis. J. Biol. Chem. 275:5253–5256
Loo T.W., Clarke D.M. 2001a. Cross-linking of human multidrug resistance P-glycoprotein by the substrate, Tris-(2-maleimidoethyl)amine, is altered by ATP hydrolysis: Evidence for rotation of a transmembrane helix. J. Biol. Chem. 276:31800–31805
Loo T.W., Clarke D.M. 2001b. Defining the drug-binding site in the human multidrug resistance P- glycoprotein using MTS-verapamil. J. Biol. Chem. 276:14972–14919
Loo T.W., Clarke D.M. 2001c. Determining the dimensions of the drug-binding domain of human P-glycoprotein using thiol cross-linkers as molecular rulers. J. Biol. Chem. 276:36877–36880
Loo T.W., Clarke D.M. 2002a. Location of the rhodamine-binding site in the human multidrug resistance P-glycoprotein. J. Biol. Chem. 277:44332–44338
Loo T.W., Clarke D.M. 2002b. Vanadate trapping of nucleotide at the ATP-binding sites of human multidrug resistance P-glycoprotein exposes different residues to the drug-binding site. Proc. Natl. Acad. Sci. USA 99:3511–3516
Loo T.W., Clarke D.M. 2005. Do drug substrates enter the common drug-binding pocket of P-glycoprotein through “gates”? Biochem. Biophys. Res. Commun. 329:419–422
Lugo M.R., Sharom F.J. 2005. Interaction of LDS-751 with P-glycoprotein and mapping of the location of the R drug binding site. Biochemistry 44:643–655
Martin C., Walker J., Rothnie A., Callaghan R. 2003. The expression of P-glycoprotein does influence the distribution of novel fluorescent compounds in solid tumour models. Br. J. Cancer 89:1581–1589
Mechetner E.B., Schott B., Morse B.S., Stein W.D., Druley T., Davis K.A., Tsuruo T., Roninson I.B. 1997. P-glycoprotein function involves conformational transitions detectable by differential immunoreactivity. Proc.Natl. Acad. Sci. USA 94:12908–12913
Miyake K., Mickley L., Litman T., Zhan Z., Robey R., Cristensen B., Brangi M., Greenberger L., Dean M., Fojo T., Bates S.E. 1999. Molecular cloning of cDNAs which are highly overexpressed in mitoxantrone-resistant cells: demonstration of homology to ABC transport genes. Cancer Res. 59:8–13
Moody I.E., Millen L., Binns D., Hunt J.F., Thomas P.J. 2002. Cooperative, ATP-dependent association of the nucleotide binding cassettes during the catalytic cycle of ATP-binding cassette transporters. J. Biol. Chem. 277:21111–21114
Murakami S., Nakashima R., Yamashita E., Yamaguchi A. 2002. Crystal structure of bacterial multidrug efflux transporter AcrB. Nature 419:587–593
Omote H., Al-Shawi M.K. 2002. A novel electron paramagnetic resonance approach to determine the mechanism of drug transport by P-glycoprotein. J. Biol. Chem. 277:45688–45694
Omote H., Figler R.A., Polar M.K., Al-Shawi M.K. 2004. Improved energy coupling of human P-glycoprotein by the glycine 185 to valine mutation. Biochemistry 43:3917–3928
Pascaud C., Garrigos M., Orlowski S. 1998. Multidrug resistance transporter P- glycoprotein has distinct but interacting binding sites for cytotoxic drugs and reversing agents. Biochem. J. 333:351–8
Penzotti J.E., Lamb M.L., Evensen E., Grootenhuis P.D. 2002. A computational ensemble pharmacophore model for identifying substrates of P-glycoprotein. J. Med. Chem. 45:1737–1740
Pleban K., Kopp S., Csaszar E., Peer M., Hrebicek T., Rizzi A., Ecker G.F., Chiba P. 2005. P-glycoprotein substrate binding domains are located at the transmembrane domain/transmembrane domain interfaces: a combined photoaffinity labeling-protein homology modeling approach. Mol. Pharmacol. 67:365–374
Poruchynsky M.S., Ling V. 1994. Detection of oligomeric and monomeric forms of P-glycoprotein in multidrug resistant cells. Biochemistry 33:4163–4174
Qu Q., Chu J.W., Sharom F.J. 2003. Transition state P-glycoprotein binds drugs and modulators with unchanged affinity, suggesting a concerted transport mechanism. Biochemistry 42:1345–1353
Qu Q., Sharom F.J. 2001. FRET analysis indicates that the two ATPase active sites of the P- glycoprotein multidrug transporter are closely associated. Biochemistry 40:1413–1422
Qu Q., Sharom F.J. 2002. Proximity of bound Hoechst 33342 to the ATPase catalytic sites places the drug binding site of P-glycoprotein within the cytoplasmic membrane leaflet. Biochemistry 41:4744–4752
Ramachandra M., Ambudkar S.V., Chen D., Hrycyna C.A., Dey S., Gottesman M.M., Pastan I. 1998. Human P-glycoprotein exhibits reduced affinity for substrates during a catalytic transition state. Biochemistry 37:5010–5019
Ramjeesingh M., Li C., Kogan I., Wang Y., Huan L.J., Bear C.E. 2001. A monomer is the minimum functional unit required for channel and ATPase activity of the cystic fibrosis transmembrane conductance regulator. Biochemistry 40:10700–10706
Raviv Y., Pollard H.B., Bruggemann E.P., Pastan I., Gottesman M.M. 1990. Photosensitized labeling of a functional multidrug transporter in living drug-resistant tumor cells. J. Biol. Chem. 265:3975–3980
Reyes C.L., Chang G. 2005. Structure of the ABC transporter MsbA in complex with ADP-vanadate and lipopolysaccharide. Science 308:1028–1031
Riordan J.R., Ling V. 1985. Genetic and biochemical characterization of multidrug resistance. Pharmacol. Ther. 28:51–75
Romsicki Y., Sharom F.J. 2001. Phospholipid flippase activity of the reconstituted P-glycoprotein multidrug transporter. Biochemistry 40:6937–6947
Rosenberg M.F., Callaghan R., Ford R.C., Higgins C.F. 1997. Structure of the multidrug resistance P-glycoprotein to 2.5 nm resolution determined by electron microscopy and image analysis. J. Biol. Chem. 272:10685–10694
Rosenberg M.F., Callaghan R., Modok S., Higgins C.F., Ford R.C. 2005. Three-dimensional structure of P-glycoprotein: the transmembrane regions adopt an asymmetric configuration in the nucleotide-bound state. J. Biol. Chem. 280:2857–2862
Rosenberg M.F., Kamis A.B., Callaghan R., Higgins C.F., Ford R.C. 2003. Three-dimensional structures of the mammalian multidrug resistance P-glycoprotein demonstrate major conformational changes in the transmembrane domains upon nucleotide binding. J. Biol. Chem. 278:8294–8299
Rosenberg M.F., Velarde G., Ford R.C., Martin C., Berridge G., Kerr I.D., Callaghan R., Schmidlin A., Wooding C., Linton K.J., Higgins C.F. 2001. Repacking of the transmembrane domains of P-glycoprotein during the transport ATPase cycle. EMBO J. 20:5615–5625
Rothnie A., Storm J., Campbell J., Linton K.J., Kerr I.D., Callaghan R. 2004. The topography of transmembrane segment six is altered during the catalytic cycle of P-glycoprotein. J. Biol. Chem. 279:34913–34921
Sarkadi B., Price E.M., Boucher R.C., Germann U.A., Scarborough G.A. 1992. Expression of the human multidrug resistance cDNA in insect cells generates a high activity drug-stimulated membrane ATPase. J. Biol. Chem. 267:4854–4858
Sauna Z.E., Ambudkar S.V. 2000. Evidence for a requirement for ATP hydrolysis at two distinct steps during a single turnover of the catalytic cycle of human P-glycoprotein. Proc. Natl. Acad. Sci. USA 97:2515–2520
Sauna Z.E., Andrus M.B., Turner T.M., Ambudkar S.V. 2004. Biochemical basis of polyvalency as a strategy for enhancing the efficacy of P-glycoprotein (ABCB1) modulators: stipiamide homodimers separated with defined-length spacers reverse drug efflux with greater efficacy. Biochemistry 43:2262–2271
Sauna Z.E., Muller M., Peng X.H., Ambudkar S.V. 2002. Importance of the conserved Walker B glutamate residues, 556 and 1201, for the completion of the catalytic cycle of ATP hydrolysis by human P-glycoprotein (ABCB1). Biochemistry 41:13989–4000
Schinkel A.H., Smit J.J., van Tellingen O., Beijnen J.H., Wagenaar E., van Deemter L., Mol C.A., van der Valk M.A., Robanus-Maandag E.G., te Riele H.P., Berns A.J.M., Borst P. 1994. Disruption of the mouse mdr1a P-glycoprotein gene leads to a deficiency in the blood-brain barrier and to increased sensitivity to drugs. Cell 77:491–502
Schumacher M.A., Miller M.C., Grkovic S., Brown M.H., Skurray R.A., Brennan R.G. 2001. Structural mechanisms of QacR induction and multidrug recognition. Science 294:2158–2163
Schwab M., Eichelbaum M., Fromm M.F. 2003. Genetic polymorphisms of the human MDR1 drug transporter. Annu. Rev. Pharmacol. Toxicol. 43:285–307
See Y.P., Carlsen S.A., Till J.E., Ling V. 1974. Increased drug permeability in Chinese hamster ovary cells in the presence of cyanide. Biochim. Biophys. Acta 373:242–252
Seelig A. 1998. A general pattern for substrate recognition by P-glycoprotein. Eur. J. Biochem. 251:252–261
Senior A.E., al-Shawi M.K., Urbatsch I.L. 1995. The catalytic cycle of P-glycoprotein. FEBS Lett. 377:285–289
Shapiro A.B., Ling V. 1997. Extraction of Hoechst 33342 from the cytoplasmic leaflet of the plasma membrane by P-glycoprotein. Eur. J. Biochem. 250:122–129
Sharom F.J. 1997. The P-glycoprotein efflux pump: how does it transport drugs? J. Membrane Biol. 160:161–175
Sharom F.J., Yu X., Doige C.A. 1993. Functional reconstitution of drug transport and ATPase activity in proteoliposomes containing partially purified P-glycoprotein. J. Biol. Chem. 268:24197–24202
Shen D.W., Cardarelli C., Hwang J., Corawell M., Richert N., Ishii S., Pastan I., Gottesman M.M. 1986. Multiple drug-resistant human KB carcinoma cells independently selected for high-level resistance to colchicine, adriamycin, or vinblastine show changes in expression of specific proteins. J. Biol. Chem. 261:7762–7770
Smith P.C., Karpowich N., Millen L., Moody I.E., Rosen J., Thomas P.J., Hunt J.F. 2002. ATP binding to the motor domain from an ABC transporter drives formation of a nucleotide sandwich dimer. Mol. Cell 10:139–149
Sonveaux N., Vigano C., Shapiro A.B., Ling V., Ruysschaert J.M. 1999. Ligand-mediated tertiary structure changes of reconstituted P-glycoprotein. A tryptophan fluorescence quenching analysis. J. Biol. Chem. 274:17649–17654
Stenham D.R., Campbell J.D., Sansom M.S., Higgins C.F., Kerr I.D., Linton K.J. 2003. An atomic detail model for the human ATP binding cassette transporter P-glycoprotein derived from disulfide cross-linking and homology modeling. FASEB J. 17:2281–2289
Tang-Wai D.F., Kajiji S., DiCapua F., de Graaf D., Roninson I.E., Gros P. 1995. Human (MDR1) and mouse (mdr1, mdr3) P-glycoproteins can be distinguished by their respective drug resistance profiles and sensitivity to modulators. Biochemistry 34:32–39
Thiebaut F., Tsuruo T., Hamada H., Gottesman M.M., Pastan I., Willingham M.C. 1987. Cellular localization of the multidrug-resistance gene product P- glycoprotein in normal human tissues. Proc. Natl. Acad. Sci. USA 84:7735–7738
Tombline G., Bartholomew L., Gimi K., Tyndall G.A., Senior A.E. 2004a. Synergy between conserved ABC signature Ser residues in P-glycoprotein catalysis. J. Biol. Chem. 279:5363–5373
Tombline G., Bartholomew L.A., Tyndall G.A., Gimi K., Urbatsch I.L., Senior A.E. 2004b. Properties of P-glycoprotein with mutations in the “catalytic carboxylate” glutamate residues. J. Biol. Chem. 279:46518–46526
Tombline G., Bartholomew L.A., Urbatsch I.L., Senior A.E. 2004c. Combined mutation of catalytic glutamate residues in the two nucleotide binding domains of P-glycoprotein generates a conformation that binds ATP and ADP tightly. J. Biol. Chem 279:31212–31220
Tran T.T., Mittal A., Aldinger T., Polli J.W., Ayrton A., Ellens H., Bentz J. 2005. The elementary mass action rate constants of P-gp transport for a confluent monolayer of MDCKII-hMDR1 cells. Biophys. J. 88:715–738
Urbatsch I.L., al-Shawi M.K., Senior A.E. 1994. Characterization of the ATPase activity of purified Chinese hamster P- glycoprotein. Biochemistry 33:7069–7076
Urbatsch I.L., Gimi K., Wilke-Mounts S., Lerner-Marmarosh N., Rousseau M.E., Gros P., Senior A.E. 2001. Cysteines 431 and 1074 are responsible for inhibitory disulfide cross- linking between the two nucleotide-binding sites in human P- glycoprotein. J. Biol. Chem. 276:26980–26987
Urbatsch I.L., Sankaran B., Bhagat S., Senior A.E. 1995a. Both P-glycoprotein nucleotide-binding sites are catalytically active. J. Biol. Chem. 270:26956–26961
Urbatsch I.L., Sankaran B., Weber J., Senior A.E. 1995b. P-glycoprotein is stably inhibited by vanadate-induced trapping of nucleotide at a single catalytic site. J. Biol. Chem. 270:19383–19390
van der Kolk D.M., de Vries E.G., van Putten W.J., Verdonck L.F., Ossenkoppele G.J., Verhoef G.E., Vellenga E. 2000. P-glycoprotein and multidrug resistance protein activities in relation to treatment outcome in acute myeloid leukemia. Clin. Cancer Res. 6:3205–3214
Vigano C., Julien M., Carrier I., Gros P., Ruysschaert J.M. 2002. Structural and functional asymmetry of the nucleotide-binding domains of P-glycoprotein investigated by attenuated total reflection Fourier transform infrared spectroscopy. J. Biol. Chem. 277:5008–5016
Wang R.B., Kuo C.L., Lien L.L., Lien E.J. 2003. Structure-activity relationship: analyses of p-glycoprotein substrates and inhibitors. J. Clin. Pharm. Ther. 28:203–228
Watkins R.E., Wisely G.B., Moore L.B., Collins J.L., Lambert M.H., Williams S.P., Willson T.M., Kliewer S.A., Redinbo M.R. 2001. The human nuclear xenobiotic receptor PXR: structural determinants of directed promiscuity. Science 292:2329–33
Wiese M., Pajeva I.K. 2001. Structure-activity relationships of multidrug resistance reversers. Curr. Med. Chem. 8:685–713
Yu E.W., McDermott G., Zgurskaya H.I., Nikaido H., Koshland D.E., Jr. 2003. Structural basis of multiple drug-binding capacity of the AcrB multidrug efflux pump. Science 300:976–980
Yuan Y.R., Blecker S., Martsinkevich O., Millen L., Thomas P.J., Hunt J.F. 2001. The crystal structure of the MJ0796 ATP-binding cassette. Implications for the structural consequences of ATP hydrolysis in the active site of an ABC transporter. J. Biol. Chem. 276:32313–32321
Zhang Z.R., Cui G., Liu X., Song B., Dawson D.C., McCarty N.A. 2005 Determination of the functional unit of the cystic fibrosis transmembrane conductance regulator chloride channel. One polypeptide forms one pore. J. Biol. Chem. 280:458–468
Acknowledgment
This work was supported by grants from the National Cancer Institute of Canada through the Canadian Cancer Society and from the Canadian Institutes of Health Research. DMC is the recipient of the Canada Research Chair in Membrane Biology.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Loo, T., Clarke, D. Recent Progress in Understanding the Mechanism of P-Glycoprotein-mediated Drug Efflux. J Membrane Biol 206, 173–185 (2005). https://doi.org/10.1007/s00232-005-0792-1
Received:
Revised:
Issue Date:
DOI: https://doi.org/10.1007/s00232-005-0792-1