Abstract
By partially replacing the corresponding omega-6 analogues in membrane phospholipids, omega-3 fatty acids have been shown to decrease the transcriptional activation of genes — e.g., adhesion molecules, chemoattractants, inflammatory cytokines — involved in endothelial activation in response to inflammatory and pro-atherogenic stimuli. This regulation occurs, at least in part, through a decreased activation of the nuclear factor-κB system of transcription factors, secondary to decreased generation of intracellular hydrogen peroxide. Such regulation by omega-3 fatty acids is likely linked to the presence of a higher number of double bonds in the fatty acid chain in omega-3 compared with omega-6 fatty acids. By similar mechanisms, omega-3 fatty acids have been recently shown to reduce gene expression of cyclooxygenase-2, an inflammatory gene involved, through the activation of some metalloproteinases, in plaque angiogenesis and plaque rupture. The quenching of gene expression of pro-inflammatory pro-atherogenic genes by omega-3 fatty acids has consequences on the extent of leukocyte adhesion to vascular endothelium, early atherogenesis and later stages of plaque development and plaque rupture, ultimately yielding a plausible comprehensive explanation for the vasculoprotective effects of these nutrients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
General Background: Nutrients as Ancestral Modulators of Gene Expression
The adaptation to environmental changes is a common feature of living organisms, from prokaryotes to higher organisms, and is a way of enhancing chances of survival in a changing environment. This adaptation is due—to a large extent—to the possibility of differentially regulating gene expression in response to external stimuli. Examples of environmental changes leading to changes in gene expression are variations in the intake of nutrients, changes in temperature [28], infections [85], the exposure to metals [64], light [70], or ionizing radiations [59] (see [36] for a general review on this issue).
In prokaryotes, mechanisms for phenotypic adaptation in response to changes in nutrients mostly consist of a transcriptional modulation capable of regulating the transcription rate of a specific messenger RNA (mRNA), which in turn determines the abundance of a translated protein or enzyme [81]. The control of mRNA stability has evolved later in the evolution of species [66]. Besides the long-term control of gene expression, bacteria are also able to effect a much more rapid change (from a total block to a dramatic enhancement) of the catalytic activity of an enzyme made either no longer necessary or indispensable for survival. These quicker adaptations occur through feedback inhibitions by the products of the enzymatic reaction [130].
Eukaryotes have evolved a much higher complexity of regulation, being capable of controlling the onset of transcription at the nuclear level through reversible modifications of DNA conformation. These include a regulation of the degree of DNA supercoiling (through control of the B to Z transition) [56, 115], chromatin status (degree of condensation, through variable phosphorylation of histone proteins) [83], or of DNA primary structure (degree of methylation) [94]. In addition, eukaryotic organisms can influence the amount of cytosplasmic mRNA available for translation through the regulation of maturation of primary transcripts in the nucleus [12] and of the transport of mature mRNA to the cytoplasm [23].
The quantity and quality of nutrients are an extraordinarily important trigger for changes in gene expression. Although in general not too much emphasized, nutrients are not just building blocks and sources of energy for our bodies, but can deeply modify our ability to react to exogenous stimuli. An understanding that nutrients may regulate gene expression is important in order to appreciate the possibility of favorably intervening in regulating pathological processes such as inflammation and atherosclerosis.
Gene Expression in Atherosclerosis and Inflammation
ENDOTHELIAL ACTIVATION AS AN EARLY CONTROLLING STEP IN ATHEROGENESIS
Atherosclerosis and inflammation share similar basic mechanisms, involving the adhesion of leukocytes to vascular endothelium in their early phases. Multiple protein families, each with a distinct function, provide “traffic signals” for leukocytes, determining their undisturbed flow in the blood or their transfer to the vessel wall. These include (a) the “selectin” family of adhesion molecules; (b) chemoattractants, some of which (“classical” chemoattractants), such as N-formyl peptides, complement components, leukotriene B4 and platelet-activating factor, act broadly on neutrophils, eosinophils, basophils and monocytes, while more recently described “chemokines”, such as monocyte chemoattractant protein-1 (MCP-1) and interleukin(IL)-8, have selectivity for leukocyte subsets; (c) the immunoglobulin superfamily members on the endothelium (comprising, among others, intercellular adhesion molecules (ICAM-1), ICAM-2, ICAM-3, and vascular cell adhesion molecule (VCAM)-1), recognizing “integrin” ligands on the leukocyte surface. For neutrophil and, probably, lymphocyte adhesion, selectins mediate the initial tethering of the circulating leukocyte over the endothelium, allowing it to roll over the endothelium, considerably slowing down its speed and allowing it to “sense” the presence of chemotactic gradients. Final firm attachment of the leukocyte to the endothelium requires the interaction of integrin ligands on the leukocyte surface with members of the immunoglobulin superfamily, expressed on the endothelium, such as ICAM-1 and VCAM-1. The multiple molecular choices available for each of these ligand-ligand interactions provide combinatorial diversity in signals, allowing, for example, the selective responses of different leukocyte classes to inflammatory agents, the preferential recirculation patterns of lymphocyte subpopulations, or the selective binding of monocytes to the arterial endothelium, this last a pivotal event during early phases of atherogenesis.
Since monocyte recruitment into the intima of large arteries is specific for atherosclerosis as compared to other forms of leukocyte-endothelial interactions, it was hypothesized that these localized monocyte-endothelium interactions reflect specific molecular changes in the adhesive properties of the endothelial surface, leading to surface expression of specific “athero-ELAMs”, i.e., endothelium-leukocyte adhesion molecules (ELAMs) expressed in the early phases of atherosclerosis. The first such protein, originally identified in the rabbit hypercholesterolemic model, is VCAM-1, a member of the immunoglobulin superfamily expressed on the human vascular endothelium at least in two molecular forms. Both forms are able to bind a heterodimeric integrin receptor, VLA4, whose leukocyte selectivity of expression, on monocytes and lymphocytes, but not on neutrophils, can explain the selectivity of monocyte recruitment in early atherogenesis [32]. Endothelial cells express VCAM-1 early during cholesterol feeding in the rabbit, before the appearance of macrophages/foam cells in the intima of a developing fatty streak, in a temporal pattern consistent with its pathogenetic role in lesion development. Pathophysiologically relevant stimuli for VCAM-1 expression in atherogenesis include minimally oxidized low density lipoproteins (LDL) or beta-very low density lipoproteins (VLDL), the advanced glycosylation end-products (AGEs) associated with diabetes, and perhaps lipoprotein (Lp) (a), or homocysteine, elevated in homocystinuria and in subtler forms of congenital or acquired enzyme defects in the homocysteine biosynthetic pathways. In addition to these humoral stimuli, the endothelial gene expression of VCAM-1 also responds to hemodynamic forces, potentially explaining the localization of atherosclerosis in particular sites of the arterial vasculature (for a general review on these issues, see [35]). A causal role of VCAM-1 in atherosclerosis is shown by the fact that a hypomorphic variant with reduced expression of VCAM-1 protects against atherosclerosis in the LDL receptor knockout mouse model [30].
METALLOPROTEINASE GENE EXPRESSION,INFLAMMATORY ANGIOGENESIS AND THE REGULATION OF PLAQUE STABILITY
Metalloproteinases (MPs) are endopeptidases able to hydrolyze peptide bonds in the inner regions of peptide chains [92]. They are characterized by an active site containing zinc and for this reason are also called zincins [13]. An important sub-family, containing a conserved methionine residue spatially located close to the zinc ion and therefore referred to as metzincins, seems to play a critical role in atherogenesis [55]. Metzincins are divided into 5 sub-groups: matrixins or matrix metalloproteinases (MMP), adamalysins, pappalysins, serralysins, and astacins [121], the first 3 of which have been found highly expressed in atherosclerotic plaques.
The MMP group is responsible for the degradation and remodeling of the extracellular matrix and is comprised of at least 24 members, the names of which are often based on their preferential substrates (e.g., gelatinase-A, -B, collagenase, etc.). They play an important role in development, wound healing, and the pathology of diseases as varied as arthritis, atherosclerosis and cancer [11].
Adamalysins are similar to MMP in their metalloproteinase domains, but contain a unique integrin receptor-binding disintegrin domain. The simultaneous presence of these two domains is the explanation of the name ADAM (A Disintegrin and Metalloproteinase) [111]. The domain structure of ADAMs actually consists of a prodomain, a metalloproteinase domain, a disintegrin domain, a cysteine-rich domain, an EGF-like domain, a transmembrane domain, and a cytoplasmic tail. At present, 30 members have been identified, comprising the ADAM proteases, found in atherosclerotic plaques [3], the ADAM-TS (where TS stands for thrombospondin-like), and the class III snake venom metalloproteinases (SVMPs) [111].
Pappalysins include pregnancy-associated plasma protein (PAPP)-A and PAPP-A2. They have received recent attention in vascular biology because of the discovery that PAPP-A is highly expressed in coronary plaques associated with acute coronary syndromes [9].
Metzincins having the ability of degrading all components of the extracellular matrix, their activity is tightly regulated. The regulation of matrix metalloproteinase activity, for example, is achieved firstly by a tight regulation of gene transcription: most MMPs are indeed only expressed in activated cells under the influence of inflammatory cytokines (IL-1β and tumor necrosis factor (TNF)-α), hormones, growth factors and oncogene products, in most cases through the induction of a few transcription factors, including nuclear factor (NF)-κB as well as the c-fos and c-jun proto-oncogenes [20, 92]. Secondly, all MMPs are expressed as inactive zymogens, which require proteolytic processing (by plasmin or by MMPs themselves) to expose the active catalytic site. Thirdly, the activity of MMPs is controlled by interactions with specific inhibitors, known as tissue inhibitors of metalloproteinases (TIMPs). The highly conserved N-terminal region of TIMPs binds to the catalytically active site of MMPs [91], and this is thought to be critical for MMP inhibition.
Atherosclerotic plaques show enhanced expression and activity of many MMPs [51, 54], ADAM-9 and ADAM-15 [3], pappalysins [9], and neutrophil elastase [41]. Although the infiltrating macrophages are the principal and best-known protease sources, also the common components of the vascular wall, such as smooth muscle cells, endothelial cells and fibroblasts, can produce MMPs [52, 53, 100], ADAMs [3] and PAPP-A [9]. The primary cause of this disregulation remains unknown, but both increased transcription and protease activation, as well as decreased protease inhibition may play important roles.
From early stages of vascular disease to the formation of advanced plaques, increased levels of MMPs, through multiple and complex mechanisms, contribute to plaque remodeling, cell invasion, migration and proliferation, as well as angiogenesis, all phenomena linked to plaque growth and destabilization. Histological studies have indeed revealed that the structure of atherosclerotic plaques is extremely variable. Plaque composition may determine whether a plaque is more or less prone to rupture [119]. The balance between the de novo synthesis of extracellular matrix and its degradation by MMPs is likely crucial for plaque stability, since fibrous plaques, where extracellular matrix deposition prevails over reabsorption, are essentially stable, whilst plaques that are macrophage- and lipid-rich and have thin fibrous caps are prone to rupture [47, 112]. The shoulder region, located at the edge of the overlying fibrous cap, is the most common site of plaque rupture, and characteristically contains numerous macrophages, which are an important source of MMPs. The abundance of MMP-1 [54], MMP-3 [54], MMP-7 [62], MMP-9 [54, 87], MMP-11 [109], MMP-12 [62] MMP-13 [122] and membrane type 1-MMP [101] in these macrophage-rich areas supports the hypothesis of a pathogenetic role of MMPs in plaque stability.
MMPs also appear, however, to play a role in early atherogenesis: the invasion of the intimal subendothelial space of the vessel wall by both leukocytes coming from the vessel lumen and smooth muscle cells mostly deriving from the intima, as well as their migration and proliferation, all require the digestion of extracellular matrix. A degradation of the basement membrane is required for the migration of the circulating leukocytes through the endothelial monolayer, and this step seems to be mediated by the release of MMPs directly induced by the physical interaction of leukocyte ligands with endothelial leukocyte adhesion molecules [84, 103].
Finally, MMPs appear to orchestrate plaque angiogenesis. Normal coronary arteries have well-developed adventitial vasa vasorum. However most human atherosclerotic plaques also contain areas of neovascularization, which consist of small irregular vessels arising primarily from the adventitial vasa vasorum [134]. The possibility that the neovasculature might play a role in the pathogenesis of atherosclerosis was first hypothesized by Winternitz [132] and by Geringer [57] in the late 1930s and 1940s, and definitively demonstrated by Barger et al., in the middle 1980s, through the finding that the plaque “malignant” neovascularization in coronary arteries preferentially originates from the advential vasa vasorum, while in the healthy segments of the same vessel there is no apparent angiogenesis [8]. Several recent reports have again pointed out that plaque angiogenesis highly contributes to plaque instability, showing an association between angiogenesis and symptomatic carotid occlusive disease [86, 89], as well as between the density of coronary adventitial vessels reaching the intima and the extent of luminal stenosis [77]. Plaque neovascularization may be a direct cause of plaque instability as a source of intraplaque hemorrhage [129]. Similar to the vessels in proliferative diabetic retinopathy, the intimal vessels are mechanically weak and more prone to bleed. Furthermore, these capillaries localize in areas rich in macrophages, T cells, and mast cells. Their close proximity to inflammatory infiltrates and their augmented expression of adhesion molecules, such as VCAM-1, ICAM-1, and E-selectin, suggest that these neovessels may actively recruit inflammatory cells into the lesions [96, 97], thus allowing the establishment of a positive feedback loop whereby inflammatory cells stimulate plaque angiogenesis, and new vessels promote further recruitment of inflammatory cells. MMPs are implicated in many stages of angiogenesis, including matrix degradation, endothelial migration and proliferation, and the release of angiogenic growth factors from the extracellular matrix. Endothelial cells, upon stimulation, also secrete MMPs [65]. Antibodies against MMP-2 and MMP-9 inhibit endothelial cell tube formation [108], implicating the production of these enzymes, by either proliferating endothelial cells or by infiltrating leukocytes, as pathogenetically relevant in neovessel formation and, by extension, in plaque instability.
Finally, numerous endothelial growth factors demonstrated in human atherosclerotic lesions, among which belongs vascular endothelial growth factor (VEGF), positively correlate with the number of intimal blood vessels in human atherosclerotic arteries [93], and can stimulate the endothelial release of several MMPs in vitro [135].
Omega-3 Fatty Acids as Inhibitors of Endothelial Activation
Highly unsaturated fatty acids (FA) and, particularly, omega-3 FA, are currently receiving increasing attention as potential anti-atherogenic and anti-inflammatory agents. The epidemiological association between dietary omega-3 FA and protection from cardiovascular disease [4, 6, 67, 73, 75, 76, 88, 113] results at least in part from a decreased extent of atherosclerosis. Numerous animal studies have shown decreased atherosclerosis in animals treated with omega-3 FA (reviewed in [37, 39, 117]). More recent evidence has been obtained about such effects in humans, through autopsy studies in Alaskan natives (consuming high amounts of fish-derived products) and non-natives, mostly consuming Western-type diets. In the study by Newman and coworkers, reporting decreased percent of intima covering with fatty streaks and raised lesion in Alaskan natives, with a high omega-3 FA dietary intake [88], vs non-natives, the magnitude of difference in fatty streak development appears larger in younger age groups [95], suggesting an effect of diet mainly in the early events leading to fully developed atherosclerotic lesions. A study of omega-3 FA supplementation after coronary bypass surgery indicated that such treatment significantly reduces vein graft stenosis [46], a process which may be regarded as an accelerated form of atherosclerosis (for more details on these issues, see [37, 39]).
MODULATION OF ENDOTHELIAL-LEUKOCYTEINTERACTIONS AND ENDOTHELIAL ACTIVATION BYOMEGA-3 FA
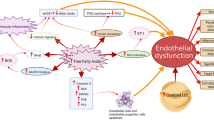
Our own research has disclosed potential mechanistic explanations for the preventive or therapeutic use of omega-3 FA in this regard. We hypothesized that omega-3 FA may modulate atherogenesis by affecting processes of early atherosclerotic development leading to the formation of fatty streak. Such processes are mostly comprised under the name of “endothelial activation”. We used human adult saphenous vein endothelial cells or human umbilical vein endothelial cells activated by cytokines, in an in vitro model of these early steps in atherogenesis, first assessing the effects of various FA on the surface expression of endothelial leukocyte adhesion molecules, and subsequently characterizing mechanisms and functional relevance of such effects. One omega-3 fatty acid, docosahexaenoic acid (DHA), when added to cultured endothelial cells hours to days before the stimulation with cytokines, early enough to allow a significant incorporation of this FA in cell membrane phospholipids, significantly inhibited events connected with endothelial activation, including the expression of adhesion molecules such as VCAM-1 (Fig. 1, upper panels), E-selectin and, to a lesser extent, ICAM-1, after stimulation with virtually any stimulus able to elicit the coordinated expression of such genes [32, 33]. Thus, this inhibition could be demonstrated with IL-1α and β, TNF-α, IL-4 and bacterial lipopolysaccharide (LPS) as stimuli. Inhibition of adhesion molecule expression occurred in a range of DHA concentrations compatible with nutritional supplementation of this FA to a normal Western diet, occurred at any time point after the appearance of cytokine effect, modifying the kinetics of surface expression of adhesion molecules, and was strictly related in magnitude to the extent of incorporation into total cell lipids. Indeed, the extent of VCAM-1 inhibitory effect paralleled the incorporation of DHA and the overall increase in incorporation of omega-3 FA, and was inversely related to the content of omega-6 FA. Experiments following the fate of 14C-labelled DHA into cell phospholipids showed a significant incorporation of DHA into the phosphatidyl ethanolamine pool, i.e., in a specific and not particularly abundant phospholipid pool, likely in the inner plasma membrane, and therefore in a possibly strategic position to alter intracellular signal transduction pathways. This effect was not limited to the expression of transmembrane molecules involved in leukocyte recruitment, but appeared to occur also for other cytokine-activated products, such as the soluble proteins IL-6 and IL-8, involved in either the amplification of the inflammatory response (IL-6), or in the specific chemoattraction for granulocytes (IL-8), and was accompanied by a functional counterpart, i.e., a reduced monocyte or monocytoid cell adhesion to cytokine-activated endothelium. Compared with DHA, eicosapentaenoic acid (EPA) was a weaker inhibitor of the expression of these molecules and of monocyte adhesion, although still more potent than other FA. We also showed that DHA’s effects on VCAM-1 expression are accompanied by parallel reductions in VCAM-1 mRNA steady-state levels, as assessed by Northern analysis (see [32, 33]). Similar results, in experiments with remarkably similar design, were later reported by Weber et al. [131]. These authors also carried these investigations one step further, demonstrating, by electrophoretic mobility shift assay, an inhibition by DHA of the activation of the NF-κB system of transcription factors [131], which control the coordinated expression of adhesion molecules and of leukocyte-specific chemoattractants upon cytokine stimulation [24, 25].
Immunocytochemical analysis of the effect of DHA on the stimulated expression of VCAM-1 (panel A), and COX-2 (panel B) in endothelial cells. Human umbilical vein endothelial cells (HUVEC) were grown in 24-well plates for 20 h, and treated with 25 μmol/L DHA for 48 h before stimulation with IL-1β 10 ng/mL for 16 h. After incubations, monolayers were fixed, and immunostained with anti-VCAM-1 and anti-COX-2 monoclonal antibodies, respectively. Immunocytochemistry with a non-immune IgG, as a control, revealed no staining (not shown). A reduction of VCAM-1 and COX-2 expression occurs in cells pre-exposed to DHA (right column). Panel C: HUVEC were pretreated with 25 μmol/L DHA for 48 h and then stimulated with 10 ng/mL IL-1α for 1 h. Monolayers were then washed and loaded for 30 min with reduced dichloro-fluorescein diacetate. This is a non-polar compound that readily diffuses into the cells, where it is hydrolyzed, by intracellular esterases, to the non-fluorescent derivative 2′7′-dichlorofluorescein, which is polar and trapped within the cells. In the presence of intracellular hydrogen peroxide (H2O2) or some of its downstream product, this compound is oxidized to the highly fluorescent compound 2′7′-dichlorofluoresceine (DCF). The fluorescence measured is therefore proportional to the H2O2 (reactive oxygen species, ROS) produced. DHA treatment reduces the fluorescence intensity and therefore the production of reactive oxygen species (photo at right).
THE DOUBLE BOND AS THE MINIMUM NECESSARY AND SUFFICIENT REQUIREMENT FOR THE INHIBITION OF ENDOTHELIAL ACTIVATION BY UNSATURATED FA
We further analyzed endothelial effects of various FA differing in chain length, number, position (omega-3 vs. omega-6 vs. omega-9) and cis/trans configuration of the double bonds. From a large number of such experiments, using VCAM-1 surface expression (by enzyme immunoassay or flow-cytometry) as readout, we concluded that (a) saturated FA are inactive; (b) potency of polyunsaturated FA increases with the number of unsaturations; (c) potency does not depend on chain length; (d) the single double bond present in the monounsaturated FA oleic acid is indeed sufficient to produce all the effects obtainable with higher unsaturated FA, albeit at higher concentrations; (e) for such an effect to occur, even the configuration (cis vs trans) of the double bond does not really matter, since oleic acid (19:1 n-9 cis) and its trans stereoisomer elaidic acid are of equal potency [31]. Indeed, also inhibition of NF-κB activation could be reproduced upon incubation of endothelial cells with oleic acid [18].
POSSIBLE MECHANISMS BY WHICH UNSATURATED FA INHIBIT ENDOTHELIAL ACTIVATION
In order to ascertain mechanisms for these effects, we confirmed the inhibition of NF-κB activation by DHA (the most potent FA inhibitor of endothelial activation), but also demonstrated this in parallel with measurements of production of hydrogen peroxide by cultured endothelial cells. This reactive oxygen species (or one of more of its unstable downstream products) appears to be a critical mediator of NF-κB activation. Indeed, we had previously shown that treatment of endothelial cells with poly-ethylene glycol (PEG)-complexed superoxide dismutase (a cell membrane-permeable form of this enzyme, catalyzing the conversion of superoxide anion to hydrogen peroxide) does not much affect VCAM-1 mRNA production, contrary to a treatment with PEG-catalase, which acts by accelerating the degradation of hydrogen peroxide [32]. These results suggested that some specific reactive oxygen species (hydrogen peroxide or some downstream products) are involved more directly than others (e.g., superoxide anion) in the activation of NF-κB. We assessed the production of extracellular hydrogen peroxide by endothelial cells stimulated with the cytokine transforming growth factor-β (TGF-β) and, more pertinent to results described above, the production of intracellular hydrogen peroxide (and/or its downstream products) by measuring the intracellular fluorescence after endothelial cell loading with dichloro-fluoresceine before or after stimulation with IL-1 (Fig. 1, lower panels). In both these experimental systems we could document a decrease in baseline production of hydrogen peroxide (or some of its downstream products) after cell membrane enrichment with DHA, and an even more pronounced dampening of the increase produced by stimulation with cytokines. Saturated FA served as a negative control in these experiments. This suggests that a property related to FA peroxidability (the presence of multiple double bonds), and usually regarded as a detrimental consequence of polyunsaturated FA enrichment of cell membranes, is indeed also directly related to inhibitory properties in the release of some reactive oxygen species crucial for cell responsiveness to cytokines. A tentative model of the site of action of omega-3 fatty acids in inhibiting endothelial activation is shown in Fig. 2.
A model of the putative site of action of omega-3 polyunsaturated fatty acids (FA), the most potent of which appears to be docosahexaenoic acid (DHA), in inhibiting endothelial activation, thus potentially decreasing early atherogenesis. Omega-3 FA would act downstream to receptors for various atherogenic stimuli (such as minimally modified LDL (mmLDL), the advanced glycation endproducts (AGEs) or inflammatory cytokines), likely at the level of reactive oxygen species (ROS), the most relevant of which appears to be hydrogen peroxide (H2O2). This would activate the nuclear factor-κB (NF-κB) system of transcription factors, likely through the activation of the degradation of the inhibitor I-κB, allowing the free active NF-κB heterodimers (rel A-p50) to translocate into the nucleus, bind to specific consensus sequences in a number of NF-κB-responsive genes (including genes for vascular cell adhesion molecule-1 (VCAM-1), intercellular adhesion molecule-1 (ICAM-1), E-selectin, monocyte chemoattractant protein-1 (MCP-1), interleukin(IL)-6 and IL-8, and cyclooxygenase-2 (COX-2), driving their increased transcription (see text for details).
These results also appear to have relevance in explaining the effects of omega-3 FA in the modulation of inflammation and of some immune responses. Since all these effects could be confirmed to occur even in the presence of inhibitors of metabolic conversion of FA to eicosanoids, they provide a novel explanation for the modulating effect of omega-3 FA in atherogenesis, distinct from the “classical” hypothesis of substrate substitution [43]. The results with oleic acid might also be an explanation for at least some of the beneficial effects of olive-oil rich (Mediterranean) diets on atherogenesis. It is noteworthy, in this regard, that oleic acid mostly appears to incorporate at the expense of saturated FA, thus disclosing the possibility of additive effects with omega-3 FA, which mostly substitute less unsaturated FA in the membrane phospholipid pools. If extended to cell types different from endothelial cells, such as the monocyte-macrophage, also undergoing “activation” phenomena upon cytokine or LPS stimulation, such results may provide a coherent explanation for a number of previous observations, including the inhibition of cytokine formation from LPS-activated macrophages [45]. As to the mechanism(s) involved, these effects are likely linked to polyunsaturated FA peroxidability, usually regarded as a detrimental effect of higher unsaturated FA, but which might actually be key to their effects. Future research will have to further elucidate molecular aspects of these phenomena as well as the greater scope of this research line in explaining many biological effects of unsaturated FA as modulators of biological responses to cytokines.
Omega-3 FA and Plaque Stability
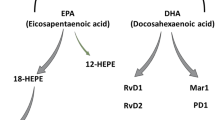
A recent study has disclosed a potential for omega-3 FA to promote a decrease in the risk of atherosclerotic plaques to rupture in patients awaiting carotid endarterectomy [126]. In this study, plaques from patients taking fish oil featured a clear incorporation of omega-3 FA into plaque lipids, and this correlated with a reduced macrophage infiltration and thicker fibrous caps compared with plaques from patients consuming sunflower oil-enriched control capsules [126]. We are, however, not aware of any study specifically looking at the effects of omega-3 FA on angiogenesis and metalloproteinase expression in atherosclerosis. Such studies are available in the area of cancer and tumor angiogenesis, from which a number of paradigms are more and more nowadays transferred to cardiovascular medicine [90]. In the early 1990’s, Rose and Connolly found that dietary omega-3 FA inhibited the growth and development of metastases from transplanted MDA-MB-435 human breast cancer cells in athymic nude mice [26]. The invasive potential of these cells, when evaluated in vitro, also appeared to be reduced when the cells were incubated with eicosapentaenoic acid (EPA) and DHA [105]. The same authors subsequently expanded these results, showing that the effect of DHA on tumor growth could be explained by the reduction of tumor angiogenesis (microvessel count) and the production of prostaglandin (PG) E2 (an arachidonic-acid metabolite through cyclooxygenases), known to affect MMP release [104]. In this study, the release of MMP was not assessed, but using similar cancer cell transplantation in the nude mouse model, Suzuki et al. later showed that the inhibition of lung metastasis of a colon cancer cell line by EPA and DHA was associated with a reduced activity of MMP-9. Conversely, MMP-2 activity was not affected by the presence of omega-3 FA in the diet [123]. Such a reduction in MMP-9 activity was also found by Harris et al. in the uterus, placenta and liver of rats fed diets enriched with DHA [63]. These authors at that time explained their findings according to the known competition hypothesis of omega-3 FA with omega-6 FA (mostly arachidonic acid) for being substrates for cyclooxygenase. This would have consequently changed the production of PGE2, thus in turn affecting MMP activity. A direct anti-angiogenic activity of omega-3 FA was also shown in vitro by Kanayasu et al. [74], as well as by Tsujii et al. [128], on bovine carotid artery endothelial cells. Omega-3 FA might negatively affect angiogenesis, also reducing the tumor production of the angiogenic factor vascular endothelial growth factor (VEGF) [17] and/or the endothelial expression of the VEGF receptor Flk-1 [133].
In the cardiovascular literature, we found only one study reporting that omega-3 FAs inhibit hypoxia-reoxygenation-induced lactate deshydrogenase release, a marker of cardiac injury [21]. On isolated rat cardiac cells, the beneficial effects of EPA were associated with a reduced expression and activity of MMP-1. These authors observed that lipid peroxidation was reduced in EPA-treated cells, and inferred that peroxidation was here a key factor. They did not, however, evaluate the activity of other MMPs [21].
EFFECTS OF OMEGA-3 FA ON ENDOTHELIAL COX-2 EXPRESSION
Prostaglandins and thromboxanes are modulators of vascular tone and hemostasis in both physiological and pathophysiological conditions. The production of these eicosanoids is regulated by the availability of arachidonic acid and other FA precursors, and the activity of PGH synthase (PGHS), also known as cyclooxygenase (COX) [116]. Liberation of arachidonate from membrane phospholipids is mediated through phospholipases. Once arachidonate is released, it is converted to PGH2 by COX. COX is a rate-limiting enzyme that exhibits a cyclooxygenase activity, catalyzing the incorporation of two molecules of oxygen into arachidonic acid to form PGG2, and a peroxidase activity, catalyzing a 2-electron reduction of PGG2 to PGH2. Cell-specific isomerization or reduction of PGH2 produces biologically active end products, such as prostacyclin and thromboxane [116]. There are now two known isoforms of COX, COX-1 and -2. The 22 kb housekeeping COX-1 gene is located on chromosome 9. Its product is a 69-kDa protein constitutively expressed in many tissues, including the vascular endothelium, monocytes, platelets, renal collecting tubules and seminal vesicles [124]. Recently, an alternative splice variant of COX-1, which is selectively inhibited by acetaminophen, has been identified and termed COX-3 [19]. In contrast to COX-1, COX-2 is undetectable in many tissues in baseline conditions, but its expression can be induced rapidly in response to inflammatory and mitogenic stimuli [116]. In the vascular endothelium, COX-2 expression is upregulated by growth factors [61], LPS [2] and cytokines [71] through traditional signaling pathways only partially specific for the inducer. For example, IL-1β has been shown to induce COX-2 through a mechanism mediated by the activation of the extracellular signal-regulated kinases (ERKs), C-Jun N-terminal kinase/stress-activated protein kinase (JNK/SAPK) and p38 mitogen-activated protein (MAP) kinases [60]. Lysophosphatidylcholine, a component of oxidized LDL, activates COX-2 expression by p38 MAP kinase activation and the transcription factors cAMP-responsive element binding protein (CREB) and activating transcription factor (ATF)-1 [102]. Finally, phorbol-myristate acetate (PMA), an activator of protein kinase C (PKC), induces COX-2 primarily through the activation of ERK1/2 [68].
The COX-2 gene promoter contains sequences responsive to traditional transcriptional factors, including NF-κB, activator protein (AP)-2, NF-IL6 and CREB protein [124]. Along with the transcriptional regulation, there appears to be a tight post-transcriptional control of COX-2 by the 3′-untranslated region of its mRNA, because of multiple copies of AU-rich elements that regulate mRNA turnover and inhibit translation [40].
The specific roles of vascular COX-1 vs. COX-2, and their contribution to the pathophysiology of atherosclerosis are controversial. Studies have demonstrated that both mRNA and protein for COX-2 are present in atherosclerotic plaques in macrophages and smooth muscle cells, whereas COX-1 and COX-2 are present in the endothelium of both atherosclerotic and healthy vessels [110, 120]. Accumulating lines of evidence, however, indicate a key role for COX-2 in inflammatory cytokine-induced angiogenesis [78], through PG-mediated pro-angiogenic effects [72, 114]. The molecular mechanisms of this phenomenon are complex and not yet fully explained. There appears, however, to be a tight relationship between COX-2 activity and the release of some MMPs, since an enhanced MMP production through PGE/cAMP-dependent pathways has been shown in macrophages [27] and, more recently, the use of specific COX-2 inhibitors inhibited the release of MMP-9 and MMP-2 promoted by COX-2 overexpression in hepatocytes [16]. In atherosclerotic lesions obtained from patients with symptomatic carotid artery disease, the simultaneous overexpression of functionally coupled COX-2, PGE synthase and MMPs [22], as well as a co-localization of COX-2, MMP-9 and membrane type-1 MMP, have been reported in the endothelial lining of vasa vasorum in human atherosclerotic aortas [69]. Thus, enhanced expression and activity of endothelial COX-2 in atherosclerotic lesions would promote plaque instability, directly producing and releasing MMP and, indirectly, promoting plaque angiogenesis.
The opportunity to inhibit COX-2 activity in atherosclerosis has been investigated using murine models of atherosclerosis. The results have so far been controversial: treatment with selective COX-2 inhibitors has been reported to decrease, increase or have no impact on atherosclerosis [10, 14, 15, 99, 106]. These studies suggest that the role of COX-2 in atherosclerosis is complex and may vary with lesion stage or the animal model. A critical review of the experimental design of the studies so far reported reveals several plausible explanations for the variability of the results. Studies reporting a beneficial effect of selective COX-2 inhibition on atherosclerosis mostly looked at the impact of treatment on early atherosclerotic lesion formation, whereas studies showing no effect evaluated the impact on advanced lesions. Thus, one can hypothesize that COX-2 contribution in atherogenesis varies temporally according to the stage of atherosclerotic lesion formation.
The effect of omega-3 FA on COX-2 expression and activity in the vascular tissue has not been extensively studied. In the murine monocytic cell line RAW264.7, DHA [79, 80], but not EPA [5], reduced the stimulated COX-2 expression. Similarly, results obtained using cultured endothelial cells have been variable. Gilbert et al. showed that DHA treatment of bovine aortic endothelial cells potentiated COX-2 expression induced by PMA [58]. Conversely EPA, but not DHA, greatly decreased IL-1β-induced COX-2 expression in human microvascular endothelial cells [1].
Using both human saphenous vein and umbilical vein endothelial cells, we have recently observed that DHA treatment before IL-1β stimulation reduces COX-2 expression and activity, by a mechanism involving a reduced production/release of reactive oxygen species (Fig. 1, middle panels). This effect seems also interpretable on basis of an interference by DHA treatment with the assembly of the enzymatic complex generating superoxide anion, NADPH oxidase, on plasma membrane. The NADPH oxidase complex consists of several subunits: two of them, p22phox and the gp91phox endothelial homologue, are integral membrane proteins. The p47phox and p67phox subunits, conversely, are located in the cytosol. Upon activation, p47phox is phosphorylated by PKC and, in complex with p67phox, translocates to the plasma membrane, constituting the active complex [107]. Barbieri et al. have recently shown that NADPH oxidase activity is involved in the regulation of COX-2 expression [7], and our preliminary data suggest that DHA treatment before PMA stimulation most likely alters plasma membrane composition and the physical status of the plasma membrane preventing p47phox translocation and activation.
UNIQUENESS OF OMEGA-3 FATTY ACIDS COMPARED WITH OTHER ANTI-INFLAMMATORY ANDANTITHROMBOTIC DRUGS AFFECTING COX
COX-2 inhibitors (coxibs), initially developed as anti-inflammatory drugs with the potential of lesser gastric toxicity because of the spared production of gastro-protective prostaglandins, have recently become the focus of a fierce debate in the medical literature because of their reported adverse effects on the incidence of myocardial infarction and death, likely because of an increased incidence of thrombosis [49, 50, 98, 127]. This is at best interpreted at the moment as due to the inhibitory effects of coxibs on vascular prostacyclin, the production of which, under conditions of shear stress occurring on the inner vessel surface, is mostly due to COX-2 [44]. On the other hand, omega-3 FA, now extensively used in cardiovascular medicine for decades, appear to be remarkably safe [125]. Can we reconcile the notion that the inhibitory effect of omega-3 FA on vascular COX-2 gene expression is not detrimental? Although it may be that the balance of favorable and detrimental effects of omega-3 FA is leaning towards the former, several differences among classical non-steroidal anti-inflammatory drugs, coxibs, and omega-3 FA have to be highlighted (Table 1).
First, one has to appreciate that, compared to coxibs, omega-3 FA also exert some inhibition of platelet TX production, likely mostly due to the fact that EPA is a worse substrate for platelet COX than arachidonic acid, and DHA is a true false substrate [29, 42, 48]. In addition, any potential TXA3, arising from EPA metabolization, is practically inactive as a platelet activator [29, 42]. Although the effects of omega-3 FA on reducing platelet TX production are clearly of much lesser magnitude than the near complete inhibition occurring with aspirin, they compare favorably with the unaltered TX production occurring under treatment with coxibs.
Second, the effect of omega-3 FA on prostaeyclin production is far away from the near-complete inhibition occurring with coxibs, high-dose aspirin and classical non-steroidal anti-inflammatory drugs. Capacity of prostacyclin production from vessel wall fragments obtained at surgery from patients treated long-term with omega-3 FA supplementation actually showed increased production [34], contrary to the inhibition repeatedly observed in studies on cultured cells [118].
Third, omega-3 FA are unique, among the drugs here being discussed, in interfering with the production and/or activity of leukotrienes [82], recently emerged as potential important pathogenetic actors in atherosclerosis, most likely through the chemoattractive properties of leukotriene B4 [38].
Last but not least, omega-3 FA, acting in these pathways at the level of gene expression more than at the level of enzyme inhibition, have a much wider range of activity on pro-atherogenic, pro-inflammatory mediators than the allegedly “magic bullets” represented by all the other drugs here being discussed. It is likely that this gentle nudging of production of mediators, intracellular signaling pathways and gene expression towards a phenotype of better quenched reactivity against environmental stimuli will prove as the best comprehensive strategy today available to fight against cardiovascular disease.
Conclusions
From the examples given above, an appropriate nutritional intervention, such as increasing the nutritional intake of omega-3 FA, either through the diet or through pharmacological supplements, can be seen as a refined way to intervene in restoring appropriate biological responses to quantitatively or qualitatively inappropriate environmental challenges, as much as wrong dietary habits can lead to disease by acting, in the wrong way, on the same fine biological mechanisms. The notion that biological processes, such as the gene expression of pro-atherogenic pro-inflammatory genes, can be finely tuned down by nutritional interventions such as omega-3 FA, may have far-reaching consequences at a time dominated by the occasionally unwise quest for more and more “intelligent” bullets for more-and-more selective targets in biological systems too often too complex for our ability to fully anticipate the ultimate results of their complete ablation.
References
Ait-Said F., Elalamy I., Werts C., Gomard M.T., Jacquemin C., Couetil J.P., Hatmi M. 2003. Inhibition by eicosapentaenoic acid of IL-1beta-induced PGHS-2 expression in human microvascular endothelial cells: involvement of lipoxygenase-derived metabolites and p38 MAPK pathway. Biochim. Biophys. Acta. 1631:77–84
Akarasereenont P., Bakhle Y.S., Thiemermann C., Vane J.R. 1995. Cytokine-mediated induction of cyclo-oxygenase-2 by activation of tyrosine kinase in bovine endothelial cells stimulated by bacterial lipopolysaccharide. Br. J. Pharmacol. 115:401–408
Al-Fakhri N., Wilhelm J., Hahn M., Heidt M., Hehrlein F.W., Endisch A.M., Hupp T., Cherian S.M., Bobryshev Y.V., Lord R.S., Katz N. 2003. Increased expression of disintegrin-metalloproteinases ADAM-15 and ADAM-9 following upregulation of integrins alpha5beta1 and alphavbeta3 in atherosclerosis. J. Cell Biochem. 89:808–823
Arthaud B. 1970. Cause of death in 339 Alaskan natives as determined by autopsy. Arch. Pathol. 90:433–438
Bagga, D., Wang, L., Farias-Eisner, R., Glaspy, J.A., Reddy, S.T. 2003. Differential effects of prostaglandin derived from omega-6 and omega-3 polyunsaturated fatty acids on COX-2 expression and IL-6 secretion. Proc. Natl. Acad. Sci USA 100:1751–1756. Epub 2003 Feb 1710
Bang H.O., Dyerberg J., Hjorne N. 1976. The composition of food consumed by Greenland Eskimos. Acta Med. Scand. 200:69–73
Barbieri S.S., Cavalca V., Eligini S., Brambilla M., Caiani A., Tremoli E, Colli S. 2004. Apocynin prevents cyclooxygenase 2 expression in human monocytes through NADPH oxidase and glutathione redox-dependent mechanisms. Free Radic. Biol. Med. 37:156–165
Barger A.C., Beeuwkes R., 3rd, Lainey L.L., Silverman K.J. 1984. Hypothesis: vasa vasorum and neovascularization of human coronary arteries. A possible role in the pathophysiology of atherosclerosis. N. Engl. J. Med. 310:175–177
Bayes-Genis A., Conover C.A., Overgaard M.T., Bailey K.R., Christiansen M., Holmes D.R., Jr., Virmani R., Oxvig C., Schwartz R.S. 2001. Pregnancy-associated plasma protein A as a marker of acute coronary syndromes. N. Engl. J. Med. 345:1022–1029
Bea F., Blessing E., Bennett B.J., Kuo C.C., Campbell L.A., Kreuzer J., Rosenfeld M.E. 2003. Chronic inhibition of cyclooxygenase-2 does not alter plaque composition in a mouse model of advanced unstable atherosclerosis. Cardiovasc. Res. 60:198–204
Beaudeux J.L., Giral P., Bruckert E., Foglietti M.J., Chapman M.J. 2004. Matrix metalloproteinases, inflammation and atherosclerosis: therapeutic perspectives. Clin. Chem. Lab. Med. 42:121–131
Bechler K. 1997. Influence of capping and polyadenylation on mRNA expression and on antisense RNA mediated inhibition of gene expression. Biochem Biophys. Res. Commun. 241:193–199
Bode W., Grams F., Reinemer P., Gomis-Ruth F.X., Baumann U., McKay D.B., Stocker W. 1996. The metzincin-superfamily of zinc-peptidases. Adv. Exp. Med. Biol. 389:1–11
Burleigh M.E., Babaev V.R., Gates J.A., Harris R.C., Gautam S., Riendeau D., Marnett L.J., Morrow J.D., Fazio S., Linton M.F. 2002. Cycloxygenase-2 promotes early atherosclerotic lesion formation in LDL receptor-deficient mice. Circulation 105:1816–1823
Burleigh M.E., Babaev V.R., Yancey P.G., Major A.S., McCaleb J.L., Gates J.A., Morrow J.D., Fazio S., Linton M.F. 2005. Cyclooxygenase-2 promotes early atherosclerotic lesion formation in ApoE-deficient and C57BL/6 mice. J. Mol. Cell. Cardiol. 21:21
Callejas N., Casado M., Diaz-Guerra M., Bosca L., Martin-Sanz P. 2001. Expression of cyclooxygenase-2 promotes the release of matrix metalloproteinase-2 and -9 in fetal rat hepatocytes. Hepatology 33:860–867
Calviello G., Di Nicuolo F., Gragnoli S., Piccioni E., Serini S., Maggiano N., Tringali G., Navarra P., Ranelletti F.O., Palozza P. 2004. n-3 PUFAs reduce VEGF expression in human colon cancer cells modulating the COX-2/PGE2 induced ERK-1 and -2 and HIF-1alpha induction pathway. Carcinogenesis 25:2303–2310
Carluccio M.A., Massaro M., Bonfrate C., Siculella L., Maffia M., Nicolardi G., Distante A., Storelli C., De Caterina R. 1999. Oleic acid inhibits endothelial activation: A direct vascular antiatherogenic mechanism of a nutritional component in the mediterranean diet. Arterioscler. Thromb. Vasc. Biol. 19:220–228
Chandrasekharan N.V., Dai H., Roos K.L., Evanson N.K., Tomsik J., Elton T.S., Simmons D.L. 2002. COX-3, a cyclooxygenase-1 variant inhibited by acetaminophen and other analgesic/antipyretic drugs: cloning, structure, and expression. Proc. Natl. Acad. Sci. U S A 99:13926–13931
Chase A.J., Bond M., Crook M.F., Newby A.C. 2002. Role of nuclear factor-kappa B activation in metalloproteinase-1, -3, and -9 secretion by human macrophages in vitro and rabbit foam cells produced in vivo. Arterioscler. Thromb. Vasc. Biol. 22:765–771
Chen H., Li D., Roberts G.J., Saldeen T., Mehta J.L. 2003. Eicosapentanoic acid inhibits hypoxia-reoxygenation-induced injury by attenuating upregulation of MMP-1 in adult rat myocytes. Cardiovasc. Res. 59:7–13
Cipollone F., Prontera C., Pini B., Marini M, Fazia M., De Cesare D., Iezzi A., Ucchino S., Boccoli G., Saba V., Chiarelli F., Cucurullo F., Mezzetti A. 2001. Overexpression of functionally coupled cyclooxygenase-2 and prostaglandin E synthase in symptomatic atherosclerotic plaque as a basis of prostaglandin E2-dependent plaque instability. Circulation 104:921–927
Cole C.N. 2000. mRNA export: the long and widing road. Nat. Cell Biol. 2:E55–E58
Collins T. 1993. Endothelial nuclear factor-κB and the initiation of the atherosclerotic lesion. Lab. Invest. 68:499–508
Collins T., Read M.A., Neish A.S., Whitley M.Z., Thanos D., Maniatis T. 1995. Transcriptional regulation of endothelial cell adhesion molecules: NF-kappa B and cytokine-inducible enhancers. FASEB J. 9:899–909
Connolly J.M., Gilhooly E.M., Rose D.P. 1999. Effects of reduced dietary linoleic acid intake, alone or combined with an algal source of docosahexaenoic acid, on MDA-MB-231 breast cancer cell growth and apoptosis in nude mice. Nutr. Cancer 35:44–49
Corcoran M., Stetler-Stevenson W., DeWitt D., Whal L. 1994. Effect of cholera toxin and pertussis toxin on prostaglandin H synthase-2, prostaglandin E2 and matrix metalloproteinase production by human monocytes. Arch. Biochem. Biophys. 310:481–488
Crawford D.L., Powers D.A. 1992. Evolutionary adaptation to different thermal environment via transcriptional regulation. Mol. Biol. Evol. 9:806–813
Culp B.R., Titus B.G., Lands W.E. 1979. Inhibition of prostaglandin biosynthesis by eicosapentaenoic acid. Prostaglandins Med. 3:269–278
Cybulsky M.J., Iiyama K., Li H., Zhu S., Chen M., Iiyama M., Davis V.M., Gutierrez-Ramos J.-C., Connelly P.W., Milstone D.S. 2001. A major role for VCAM-1, but not ICAM-1, in early atherosclerosis. J. Clin. Invest. 107:1255–1262
De Caterina R., Bernini W., Carluccio M., Liao J., Libby P. 1998. Structural requirements for inhibition of cytokine-induced endothelial activation by unsaturated fatty acids. J. Lipid Res. 39:1062–1070
De Caterina R., Cybulsky M.A., Clinton S.K., Gimbrone M.A., Jr., Libby P. 1995. Omega-3 fatty acids and endothelial leukocyte adhesion molecules. Prostagl. Leukotr. Ess. Fatty Acids. 52:191–195
De Caterina R., Cybulsky M.I., Clinton S.K., Gimbrone M.A., Jr., Libby P. 1994. The omega-3 fatty acid docosahexaenoate reduces cytokine-induced expression of pro-atherogenic and pro-inflammatory proteins in human endothelial cells. Arterioscl. Thromb. 14:1829–1836
De Caterina R., Giannessi D., Mazzone A., Bernini W., Lazzerini G., Maffei S., Cerri M., Salvatore L., Weksler B. 1990. Vascular prostacyclin is increased in patients ingesting omega-3 polyunsaturated fatty acids before coronary artery bypass surgery. Circulation 82:428–438
De Caterina, R., Gimbrone, M.A., Jr. 1995. Leukocyte-endothelial interactions and the pathogenesis of atherosclerosis. In: n-3 Fatty Acids — Prevention and Treatment in Vascular Disease. Kristensen, SD., Schmidt, EB., De Caterina, R., Endres, S., eds. pp 9–24, Springer Verlag
De Caterina R., Madonna R., Hassan J., Procopio A.D. 2001. Nutrients and gene expression. World Rev. Nutr. Diet 89:23–52
De Caterina R., Zampolli A. 2001. n-3 fatty acids:antiatherosclerotic effects. Lipids 36:S69–S78
De Caterina R., Zampolli A. 2004. From asthma to atherosclerosis — 5-lipoxygenase, leukotrienes, and inflammation. N. Engl. J. Med. 350:4–7
De Caterina, R., Zampolli, A., Del Turco, S., Madonna, R., Massaro, M. 2006. Nutritional mechanisms that influence cardiovascular disease. Am. J. Clin. Nutr. in press
Dixon D.A., Kaplan C.D., McIntyre T.M., Zimmerman G.A., Prescott S.M. 2000. Post-transcriptional control of cyclooxygenase-2 gene expression. The role of the 3′-untranslated region. J. Biol. Chem. 275:11750–11757
Dollery C.M., Owen C.A., Sukhova G.K., Krettek A., Shapiro S.D., Libby P. 2003. Neutrophil elastase in human atherosclerotic plaques: production by macrophages. Circulation 107:2829–2836
Dyerberg J., Bang H.O. 1978. Dietary fat and thrombosis. Lancet 1:152
Dyerberg J., Bang H.O., Stofferson E., Moncada S., Vane J.R. 1978. Eicosapentaenoic acid and prevention of thrombosis and atherosclerosis. Lancet 117–119
Egan K.M., Lawson J.A., Fries S., Koller B., Rader D.J., Smyth E.M., Fitzgerald G.A. 2004. COX-2-derived prostacyclin confers atheroprotection on female mice. Science 306:1954–1957
Endres S., Ghorbani R., Kelley V.E., Georgilis K., Lonneman G., van der Meer J.W.M., Cannon J.G., Rogers T.S., Klemper M.S., Weber P.C., Schaefer E.J., Woff S.M., Dinarello C.A. 1989. The effect of dietary supplementation with n-3 polyunsaturated fatty acids on the synthesis of interleukin-1 and tumor necrosis factor by mononuclear cells. N. Engl. J. Med. 320:265–271
Eritsland J., Arnesen H., Grønseth K., Field N.B., Abdelnoor M. 1994. Effect of supplementation with n-3 fatty acids on graft patency in patients undergoing coronary artery bypass operation. Results from the SHOT study. Eur Heart J. 15:29
Falk E., Shah P.K., Fuster V. 1995. Coronary plaque disruption. Circulation 92:657–671
Fischer S., von, Schacky C., Siess W., Strasser T., Weber P.C. 1984. Uptake, release and metabolism of docosahexaenoic acid (DHA, c22:6 omega 3) in human platelets and neutrophils. Biochem. Biophys. Res. Commun. 120:907–918
Fitzgerald G.A. 2004. Coxibs and cardiovascular disease. N. Engl. J. Med. 351:1709–1711
Furberg C.D., Psaty B.M., FitzGerald G.A. 2005. Parecoxib, valdecoxib, and cardiovascular risk. Circulation 111:249
Galis Z.S., Muszynski M., Sukhova G.K., Simon-Morrissey E., Libby P. 1995. Enhanced expression of vascular matrix metalloproteinases induced in vitro by cytokines and in regions of human atherosclerotic lesions. Ann. N. Y. Acad. Sci. 748:501–507
Galis Z.S., Muszynski M., Sukhova G.K., Simon-Morrissey E., Unemori E.N., Lark M.W., Amento E., Libby P. 1994. Cytokine-stimulated human vascular smooth muscle cells synthesize a complement of enzymes required for extracellular matrix digestion. Circ. Res. 75:181–189
Galis Z.S., Sukhova G.K., Kranzhofer R., Clark S., Libby P. 1995. Macrophage foam cells from experimental atheroma constitutively produce matrix-degrading proteinases. Proc. Natl. Acad. Sci. USA 92:402–406
Galis Z.S., Sukhova G.K., Lark M.W., Libby P. 1994. Increased expression of matrix metalloproteinases and matrix degrading activity in vulnerable regions of human atherosclerotic plaques. J. Clin. Invest. 94:2493–2503
Garcia-Touchard A., Henry T.D., Sangiorgi G., Spagnoli L.G., Mauriello A., Conover C., Schwartz R.S. 2005. Extracellular proteases in atherosclerosis and restenosis. Arterioscler. Thromb. Vasc. Biol. 25:1119–1127
Gartenberg M.R., Wang J.C. 1992. Positive supercoiling of DNA greatly diminishes mRNA synthesis in yeast. Proc. Natl. Acad. Sci. USA 89:11461–11465
Geiringer E. 1951. Intimal vascularization and atherosclerosis. J. Pathol. Bacteriol. 63:201–211
Gilbert M., Dalloz S., Maclouf J., Lagarde M. 1999. Differential effects of long chain n-3 fatty acids on the expression of PGH synthase isoforms in bovine aortic endothelial cells. Prostaglandins Leukot. Essent. Fatty Acids. 60:363–365
Gong B., Chen Q., Almasan A. 1998. Ionizing radiation stimulates mitochondrial gene expression and activity. Radiat. Res. 150:505–512
Guan Z., Buckman S.Y., Pentiand A.P., Templeton D.J., Morrison A.R. 1998. Induction of cyclooxygenase-2 by the activated MEKK1→SEK1/MKK4→p38 mitogen-activated protein kinase pathway. J. Biol. Chem. 273:12901–12908
Habib A., Creminon C., Frobert Y., Grassi J., Pradelles P., Maclouf J. 1993. Demonstration of an inducible cyclooxygenase in human endothelial cells using antibodies raised against the carboxyl-terminal region of the cyclooxygenase-2. J. Biol. Chem. 268:23448–23454
Halpert I., Sires U.I., Roby J.D., Potter-Perigo S., Wight T.N., Shapiro S.D., Welgus H.G., Wickline S.A., Parks W.C. 1996. Matrilysin is expressed by lipid-laden macrophages at sites of potential rupture in atherosclerotic lesions and localizes to areas of versican deposition, a proteoglycan substrate for the enzyme. Proc. Natl. Acad. Sci. USA 93:9748–9753
Harris M.A., Hansen R.A., Vidsudhiphan P., Koslo J.L., Thomas J.B., Watkins B.A., Allen K.G. 2001. Effects of conjugated linoleic acids and docosahexaenoic acid on rat liver and reproductive tissue fatty acids, prostaglandins and matrix metalloproteinase production. Prostaglandins Leukot. Essent. Fatty Acids. 65:23–29
Hennecke H. 1990. Regulation of bacterial gene expression by metal-protein complexes. Mol. Microbiol. 4:1621–1628
Herron G.S., Banda M.J., Clark E.J., Gavrilovic J., Werb Z. 1986. Secretion of metalloproteinases by stimulated capillary endothelial cells. II. Expression of collagenase and stromelysin activities is regulated by endogenous inhibitors. J. Biol. Chem. 261:2814–2818
Higgins C.F., Peltz S.W., Jacobson A. 1992. Turnover of mRNA in prokaryotes and lower eukaryotes. Curr. Opin. Genet. Dev. 2:739–747
Hirai A., Hamazaki T., Terano T. 1980. Eicosapentaenoic acid and platelet function in Japanese. Lancet 2:1132–1133
Hirai K., Ezumi Y., Nishida E., Uchiyama T., Takayama H. 1999. Comparative study of vanadate- and phorbol ester-induced cyclo-oxygenase-2 expression in human endothelial cells. Thromb. Haemost. 82:1545–1552
Hong B.K., Kwon H.M., Lee B.K., Kim D., Kim I.J., Kang S.M., Jang Y., Cho S.H., Kim H.K., Jang B.C., Cho S.Y., Kim H.S., Kim M.S., Kwon H.C., Lee K. 2000. Coexpression of cyclooxygenase-2 and matrix metalloproteinases in human aortic atherosclerotic lesions. Yonsei Med. J. 41:82–88
Inaba T., Nagano Y., Reid J.B., Sasaki Y. 2000. A 12 bp cis-regulatory element sufficient to confer dark-inducible and light down expression to a minimal promoter in pea. J. Biol. Chem. 88:22056–22060
Jones D.A., Carlton D.P., McIntyre T.M., Zimmerman G.A., Prescott S.M. 1993. Molecular cloning of human prostaglandin endoperoxide synthase type II and demonstration of expression in response to cytokines. J. Biol. Chem. 268:9049–9054
Jones M.K., Wang H., Peskar B.M., Levin E, Itani R.M., Sarfeh I.J., Tarnawski A.S. 1999. Inhibition of angiogenesis by nonsteroidal anti-inflammatory drugs: insight into mechanisms and implications for cancer growth and ulcer healing. Nat. Med. 5:1418–1423
Kagawa Y., Nishizawa M., Suzuki M. 1982. Eicosapolyenoic acid of serum lipids of Japanese islanders with low incidence of cardiovascular diseases. J. Nutr. Sci. Vitaminol. (Tokyo). 28:441–453
Kanayasu T., Morita I., Nakao-Hayashi J., Asuwa N., Fujisawa C., Ishii T., Ito H., Murota S. 1991. Eicosapentaenoic acid inhibits tube formation of vascular endothelial cells in vitro. Lipids. 26:271–276
Kromann N., Green A. 1980. Epidemiological studies in the Upernavik district, Greenland. Acta Med. Scand. 208:401–406
Kromhout D., Bosschieter E.B., De Lezenne Coulander C. 1985. The inverse relation between fish consumption and 20-year mortality from coronary heart disease. N. Engl. J. Med. 312:1205–1209
Kumamoto M., Nakashima Y., Sueishi K. 1995. Intimal neovascularization in human coronary atherosclerosis: its origin and pathophysiologieal significance. Hum. Pathol. 26:450–456
Kuwano T., Nakao S., Yamamoto H., Tsuneyoshi M., Yamamoto T., Kuwano M., Ono M. 2004. Cyclooxygenase 2 is a key enzyme for inflammatory cytokine-induced angiogenesis. FASEB J. 18:300–310
Lee J.Y., Plakidas A., Lee W.H., Heikkinen A., Chanmugam P., Bray G., Hwang D.H. 2003. Differential modulation of Toll-like receptors by fatty acids: preferential inhibition by n-3 polyunsaturated fatty acids. J. Lipid Res. 44:479–486
Lee J.Y., Ye J., Gao Z., Youn H.S., Lee W.H., Zhao L., Sizemore N., Hwang D.H. 2003. Reciprocal modulation of Toll-like receptor-4 signaling pathways involving MyD88 and phosphatidylinositol 3-kinase/AKT by saturated and polyunsaturated fatty acids. J. Biol. Chem. 278:37041–37051
Lewin B. 1997. Genes VI. Oxford University Press, Oxford, New York, Tokyo
Lewis R.A., Austen K.F., Soberman R.J. 1990. Leukotrienes and other products of the 5-lipoxygenase pathway. Biochemistry and relation to pathobiology in human diseases. N. Engl. J. Med. 323:645–655
Li Q., Wrange O., Eriksson P. 1997. The role of chromatin in transcriptional regulation. Int. J. Biochem. Cell Biol. 29:731–742
Madri J.A., Graesser D., Haas T. 1996. The roles of adhesion molecules and proteinases in lymphocyte transendothelial migration. Biochem. Cell Biol. 74:749–757
Manger I.D., Relman D.A. 2000. How the host ‘sees’ pathogen: global gene expression responses to infection. Curr. Opin. Immunol. 12:215–218
McCarthy M.J., Loftus I.M., Thompson M.M., Jones L., London N.J., Bell P.R., Naylor A.R., Brindle N.P. 1999. Angiogenesis and the atherosclerotic carotid plaque: an association between symptomatology and plaque morphology. J. Vasc. Surg. 30:261–268
McMillan W.D., Patterson B.K., Keen R.R., Shively V.P., Cipollone M., Pearce W.H. 1995. In situ localization and quantification of mRNA for 92-kD type IV collagenase and its inhibitor in aneurysmal, occlusive, and normal aorta. Arterioseler.Thromb. Vasc. Biol. 15:1139–1144
Middaugh J.P. 1990. Cardiovascular deaths among Alaskan natives 1980–1986. Am. J. Public Health 80:282–285
Mofidi R., Crotty T.B., McCarthy P., Sheehan S.J., Mehigan D., Keaveny T.V. 2001. Association between plaque instability, angiogenesis and symptomatic carotid occlusive disease. Br. J. Surg. 88:945–950
Moulton K.S. 2002. Plaque angiogenesis: its functions and regulation. Cold Spring Harb. Symp. Quant. Biol. 67:471–482
Nagase H. 1997. Activation mechanisms of matrix metalloproteinases. Biol. Chem. 378:151–160
Nagase H., Woessner J.F. Jr. 1999. Matrix metalloproteinases. J. Biol. Chem. 274:21491–21494
Nakagawa K., Chen Y.X., Ishibashi H., Yonemitsu Y., Murata T., Hata Y., Nakashima Y., Sueishi K. 2000. Angiogenesis and its regulation: roles of vascular endothelial cell growth factor. Semin. Thromb. Hemost. 26:61–66
Newell-Price J., Clark A.J., King P. 2000. DNA methylation and silencing of gene expression. Trends Endocrinol. Metab. 11:142–148
Newman W.P., Middaugh J.P., Propst M.T., Rogers D.R. 1993. Atherosclerosis in Alaska natives and non-natives. Lancet 341:1056–1057
O’Brien K.D., Alien M.D., McDonald T.O., Chait A., Harlan J.M., Fishbein D., McCarty J., Ferguson M., Hudkins K., Benjamin C.D., et al. 1993. Vascular cell adhesion molecule-1 is expressed in human coronary atherosclerotic plaques. Implications for the mode of progression of advanced coronary atherosclerosis. J. Clin. Invest. 92:945–951
O’Brien K.D., McDonald T.O., Chait A., Alien M.D., Alpers C.E. 1996. Neovascular expression of E-selectin, intercellular adhesion molecule-1, and vascular cell adhesion molecule-1 in human atherosclerosis and their relation to intimal leukocyte content. Circulation 93:672–682
Okie S. 2005. Raising the safety bar—the FDA’s coxib meeting. N. Engl. J. Med. 352:1283–1285
Pratico D., Tillmann C., Zhang Z.B., Li H., FitzGerald G.A. 2001. Acceleration of atherogenesis by COX-1-dependent prostanoid formation in low density lipoprotein receptor knockout mice. Proc. Natl. Acad. Sci. USA 98:3358–33631
Rajavashisth T.B., Liao J.K., Galis Z.S., Tripathi S., Laufs U., Tripathi J., Chai N.N., Xu X.P., Jovinge S., Shah P.K., Libby P. 1999. Inflammatory cytokines and oxidized low density lipoproteins increase endothelial cell expression of membrane type 1-matrix metalloproteinase. J. Biol. Chem. 274:11924–11929
Rajavashisth T.B., Xu X.P., Jovinge S., Meisel S., Xu X.O., Chai N.N., Fishbein M.C., Kaul S., Cercek B., Sharifi B., Shah P.K. 1999. Membrane type 1 matrix metalloproteinase expression in human atherosclerotic plaques: evidence for activation by proinflammatory mediators. Circulation 99:3103–3109
Rikitake Y., Hirata K., Kawashima S., Takeuchi S., Shimokawa Y., Kojima Y., Inoue N., Yokoyama M. 2001. Signaling mechanism underlying COX-2 induction by lysophosphatidylcholine. Biochem. Biophys. Res. Commun. 281:1291–1297
Romanic A.M., Madri J.A. 1994. The induction of 72-kD gelatinase in T cells upon adhesion to endothelial cells is VCAM-1 dependent. J. Cell Biol. 125:1165–1178
Rose D.P., Connolly J.M. 1999. Antiangiogenicity of docosahexaenoic acid and its role in the suppression of breast cancer cell growth in nude mice. Int. J. Oncol. 15:1011–1015
Rose D.P., Connolly J.M., Coleman M. 1996. Effect of omega-3 fatty acids on the progression of metastases after the surgical excision of human breast cancer cell solid tumors growing in nude mice. Clin. Cancer Res. 2:1751–1756
Rott D., Zhu J., Burnett M.S., Zhou Y.F., Zalles-Ganley A., Ogunmakinwa J., Epstein S.E. 2003. Effects of MF-tricyclic, a selective cyclooxygenase-2 inhibitor, on atherosclerosis progression and susceptibility to cytomegalovirus replication in apolipoprotein-E knockout mice. J. Am. Coll. Cardiol. 41:1812–1819
Rueckschloss U., Duerrschmidt N., Morawietz H. 2003. NADPH oxidase in endothelial cells: impact on atherosclerosis. Antioxid. Redox Signal 5:171–180
Schnaper H.W., Grant D.S., Stetler-Stevenson W.G., Fridman R., D’Orazi G., Murphy A.N., Bird R.E., Hoythya M., Fuerst T.R., French D.L., et al. 1993. Type IV collagenase(s) and TIMPs modulate endothelial cell morphogenesis in vitro. J. Cell Physiol. 156:235–246
Schonbeck U., Mach F., Sukhova G.K., Atkinson E., Levesque E., Herman M., Graber P., Basset P., Libby P. 1999. Expression of stromelysin-3 in atherosclerotic lesions: regulation via CD40-CD40 ligand signaling in vitro and in vivo. J. Exp. Med. 189:843–853
Schonbeck U., Sukhova G.K., Graber P., Coulter S., Libby P. 1999. Augmented expression of cyclooxygenase-2 in human atherosclerotic lesions. Am. J. Pathol. 155:1281–1291
Seals D.F., Courtneidge S.A. 2003. The ADAMs family of metalloproteases: multidomain proteins with multiple functions. Genes Dev. 17:7–30
Shah P.K., Falk E., Badimon J.J., Fernandez-Ortiz A., Mailhac A., Villareal-Levy G., Fallon J.T., Regnstrom J., Fuster V. 1995. Human monocyte-derived macrophages induce collagen breakdown in fibrous caps of atherosclerotic plaques. Potential role of matrix-degrading metalloproteinases and implications for plaque rupture. Circulation 92:1565–1569
Shekelle R., Missel L., Paul O., MacMillan-Schryock A., Stamler J. 1985. Fish consumption and mortality from coronary heart disease (Letter). N. Engl. J. Med. 313:820
Shtivelband M.I., Juneja H.S., Lee S., Wu K.K. 2003. Aspirin and salicylate inhibit colon cancer medium- and VEGF-induced endothelial tube formation: correlation with suppression of cyclooxygenase-2 expression. J. Thromb. Haemost. 1:2225–2233
Smith G.R. 1981. DNA supercoiling: another level for regulating gene expression. Cell. 24:599–600
Smith W.L., Garavito R.M., DeWitt D.L. 1996. Prostaglandin endoperoxide H synthases (cyclooxygenases)-1 and -2. J. Biol Chem. 271:33157–33160
Soei, L., Lamers, J., Sassen, L., van Tol, A., Scheek, L., Dekkers, D., van Meegen, J., Verdouw, P. Fish oil: a modulator of experimental atherosclerosis in animals. In: n-3 Fatty Acids: Prevention and Treatment in Vascular Disease. Kristensen, S., Endres, S., De Caterina, R., Schmidt, E., eds. pp 77–84. Springer Verlag
Spector A.A., Kaduce T.L., Figard P.H., Norton K.C., Hoak J.C., Czervionke R.L. 1983. Eicosapentaenoic acid and prostacyclin production by cultured human endothelial cells. J. Lipid Res. 24:1595–1604
Stary H.C., Chandler A.B., Dinsmore R.E., Fuster V., Glagov S., Insull W., Jr., Rosenfeld M.E., Schwartz C.J., Wagner W.D., Wissler R.W. 1995. A definition of advanced types of atherosclerotic lesions and a histological classification of atherosclerosis. A report from the Committee on Vascular Lesions of the Council on Arteriosclerosis, American Heart Association. Circulation 92:1355–1374
Stemme V., Swedenborg J., Claesson H., Hansson G.K. 2000. Expression of cyclo-oxygenase-2 in human atherosclerotic carotid arteries. Eur. J. Vasc. Endovasc. Surg. 20:146–152
Stocker V., Grams F., Baumann U., Reinemer P., Gomis-Ruth F.X., McKay D.B., Bode W. 1995. The metzincins—topological and sequential relations between the astacins, adamalysins, serralysins, and matrixins (collagenases) define a superfamily of zinc-peptidases. Protein Sci. 4:823–840
Sukhova G.K., Schonbeck U., Rabkin E., Schoen F.J., Poole A.R., Billinghurst R.C., Libby P. 1999. Evidence for increased collagenolysis by interstitial collagenases-1 and -3 in vulnerable human atheromatous plaques. Circulation 99:2503–2509
Suzuki I., Iigo M., Ishikawa C., Kuhara T., Asamoto M., Kunimoto T., Moore M.A., Yazawa K., Araki E., Tsuda H. 1997. Inhibitory effects of oleic and docosahexaenoic acids on lung metastasis by colon-carcinoma-26 cells are associated with reduced matrix metalloproteinase-2 and -9 activities. Int. J. Cancer. 73:607–612
Tanabe T., Tohnai N. 2002. Cyclooxygenase isozymes and their gene structures and expression. Prostaglandins Other Lipid Mediat. 68–69:95–114
The GISSI-Prevenzione Investigators: 1999. Dietary supplementation with n-3 polyunsaturated fatty acids and vitamins E after myocardial infarction: results of the GISSI-Prevenzione trial. Lancet 354:447–455
Thies F., Garry J.M., Yaqoob P., Rerkasem K., Williams J., Shearman C.P., Gallagher P.J., Calder P.C., Grimble R.F. 2003. Association of n-3 polyunsaturated fatty acids with stability of atherosclerotic plaques: a randomised controlled trial. Lancet 361:477–485
Topol E.J. 2004. Failing the public health—rofecoxib, Merck, and the FDA. N. Engl. J. Med. 351:1707–1709
Tsuji M., Murota S.I., Morita I. 2003. Docosapentaenoic acid (22:5, n-3) suppressed tube-forming activity in endothelial cells induced by vascular endothelial growth factor. Prostaglandins Leukot. Essent. Fatty Acids 68:337–342
van der Wal A.C., Decker A.E., van der Loos C.M., Das P.K. 1994. Site of intimal rupture or erosion of thrombosed coronary atherosclerotic plaques is characterized by an inflammatory process irrespective of the dominant plaque morphology. Circulation 89:36–44
Verderber E., Lucast L.J., Van Dehy J.A., Cozart P., Etter J.B. 1997. Role of the hemeA gene product and delta aminolevulinic acid in regulation of Escherichia Coli heme synthasis. J. Bacteriol. 179:4583–4590
Weber C., Erl W., Pietsch A., Danesch U., Weber P. 1995. Docosahexaenoic acid selectively attenuates induction of vascular cell adhesion molecule-1 and subsequent monocytic cell adhesion to human endothelial cells stimulated by tumor necrosis factor-alpha. Arterioscler. Thromb. Vasc. Biol. 15:622–628
Winternitz, M., Thomas, R., LeCompte, P. 1938. The Biology of Atherosclerosis. Thomas, C.C., ed. Springfield
Yang S.P., Morita I., Murota S.I. 1998. Eicosapentaenoic acid attenuates vascular endothelial growth factor-induced proliferation via inhibiting Flk-1 receptor expression in bovine carotid artery endothelial cells. J. Cell Physiol. 176:342–349
Zhang Y., Cliff W.J., Schoefl G.I., Higgins G. 1993. Immunohistochemical study of intimal microvessels in coronary atherosclerosis. Am. J. Pathol. 143:164–172
Zucker S., Mirza H., Conner C.E., Lorenz A.F., Drews M.H., Bahou W.F., Jesty J. 1998. Vascular endothelial growth factor induces tissue factor and matrix metalloproteinase production in endothelial cells: conversion of prothrombin to thrombin results in progelatinase A activation and cell proliferation. Int. J. Cancer. 75:780–786
Acknowledgment
We are indebted to all our former and current collaborators at the Laboratory for Thrombosis and Vascular Research at the CNR Institute of Clinical Physiology in Pisa, the Laboratory for Atherosclerosis Research at the CNR Institute of Clinical Physiology in Lecce, and the Experimental Cardiology Laboratory at the “G. d’Annunzio” Foundation in Chieti, for the experimental data on which most of the considerations here highlighted are based.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
De Caterina, R., Massaro, M. Omega-3 Fatty Acids and the Regulation of Expression of Endothelial Pro-Atherogenic and Pro-Inflammatory Genes. J Membrane Biol 206, 103–116 (2005). https://doi.org/10.1007/s00232-005-0783-2
Received:
Issue Date:
DOI: https://doi.org/10.1007/s00232-005-0783-2