Abstract
Cystic fibrosis (CF) transmembrane conductance regulator (CFTR) Cl− channel function is required for activating amiloride-sensitive epithelial Na+ channels (ENaC) in salt-absorbing human sweat duct. It is unclear whether ENaC channel function is also required for CFTR activation. The dysfunctional ENaC mutations in type-1 pseudohypoaldosteronism (PHA-1) provided a good opportunity to study this phenomenon of ion channel interaction between CFTR and ENaC. The PHA-1 ducts completely lacked spontaneous ENaC conductance (gENaC). In contrast, the normal ducts showed large spontaneous gENaC (46 ± 10 ms, mean ± SE). After permeabilization of the basolateral membrane with α-toxin, cAMP + ATP activation of CFTR Cl− conductance (gCFTR) or alkalinization of cytosolic pH (6.8 to 8.5) stimulated gENaC of normal but not PHA-1 ducts. In contrast, both spontaneous gCFTR in intact ducts and (cAMP + ATP)-activated gCFTR of permeabilized ducts appeared to be similar in normal and PHA-1 subjects. Lack of gENaC completely blocked salt absorption and caused dramatic reversal of skin potentials associated with pilocarpine-induced sweat secretion from significantly negative in normal subjects (−13 ± 7.0 mV) to significantly positive (+22 ± 11.0 mV) in PHA-1 patients. We conclude that virtual lack of ENaC in PHA-1 ducts had little effect on CFTR activity and that the positive skin potentials could potentially serve as a diagnostic tool to identify type-1 pseudohypoaldosteronism.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
We have recently shown that activation of CFTR increases gENaC in the native human reabsorptive sweat duct. Lack of CFTR function in the apical membranes of sweat ducts from homozygous ΔF508 CF patients resulted in significant loss of ENaC activity. These early observations indicated that CFTR Cl− channel function is required for activation of ENaC in absorptive sweat duct [20]. Since the CFTR and ENaC must function in concert during salt absorption, we asked whether ENaC could also influence CFTR function. Studies on heterologous systems indicated that ENaC expression significantly stimulated CFTR Cl− currents in Xenopus oocytes [12]. However, direct evidence of ENaC stimulation of CFTR Cl− conductance from a native human tissue is lacking. The sweat ducts from type-1 PHA patients that seem to lack ENaC conductance in the apical plasma membrane offered a good opportunity to investigate the role of ENaC in CFTR regulation. The autosomal recessive PHA-1 is caused by loss-of-function mutations in ENaC [5, 7, 8, 11, 27, 29]. Patients with this systemic form of PHA-1 suffer salt loss from multiple Na+-absorbing epithelia including kidneys, colon, salivary glands and sweat glands [10, 13, 27]. Based on studies of heterologous systems, mutant isoforms associated with this form of PHA-1 are thought to interfere with the normal trafficking of assembled ENaC channels to the plasma membranes [7, 27]. However, we do not fully understand the extent to which ENaC function is lost in vivo. If, in fact, the sweat ducts from PHA-1 patients have completely lost ENaC activity as predicted, these ducts might serve as an excellent model to investigate molecular interaction between ENaC and CFTR. Measuring the magnitude of gCFTR in these ducts may provide critical preliminary insights into several critical questions such as whether ENaC and CFTR interaction influence each other’s trafficking and expression and whether loss of Na+ transport activity affects the activity of the counter ion (Cl−) channel, CFTR, in vivo. Accordingly, we investigated the effect of ENaC mutations on sweat electrolyte concentration, skin potentials and the magnitude of gENaC in the apical membrane of sweat ducts from PHA-1 patients. We then compared the effect of ENaC activity on the properties of spontaneous gCFTR in intact ducts and cAMP-and ATP-activated gCFTR in basolaterally α-toxin-permeabilized ducts from PHA-1 patients and normal subjects. We show that native sweat ducts from PHA-1 patients completely lacked gENaC, yet the magnitude of gCFTR remains unaffected, suggesting that in contrast to ENaC (which requires CFTR for its activation), CFTR activity is independent of ENaC activity.
Materials and Methods
MICROPERFUSION OF SWEAT DUCTS
Sweat ducts were obtained from skin biopsies of subjects giving informed consent. Experiments were performed on ten normal and two PHA-1 subjects. Because PHA-1 is a very rare genetic disease only a limited number of patients were available to participate in this study. Sweat ducts were dissected and microperfused as described previously [19, 20]. Segments of ducts usually longer than 1 mm were microperfused with a double-barreled luminal micropipette that served to perfuse and record transepithelial voltage through one barrel and to pass constant current pulses through the other. This arrangement allowed estimation of the specific membrane conductance from the cable equation [19, 20].
PERMEABILZATION OF THE BASOLATERAL MEMBRANE
After confirming the integrity of the perfused tubule [19], we applied 1,000–5,000 units/ml of α-toxin fiom Staphylococcus aureus to the bath solution in order to selectively permeabilize the basolateral membrane [19, 20]. This procedure leaves the epithelium with an intact, functional apical membrane and a non-selective basal membrane, permeable to molecules of up to about 5,000 mwu including cAMP, ATP and other small solutes. We then determined the magnitude of gCFTR and gENaC before and after application of cAMP and ATP to the cytoplasmic bath by measuring the trans-apical membrane conductance as previously described [20].
PERFUSION SOLUTIONS
The luminal perfusion Ringer’s solutions contained (in mM) NaCl, 150; K, 5; PO4, 3.5; MgSO4, 1.2; CaCl2, 1; buffered to pH. 7.4. gENaC was blocked by luminal amiloride (0.1) as needed to measure the amiloride-sensitive conductance in the apical membrane. Cl−-free luminal Ringer’s solution was prepared by complete substitution of Cl− with the impermeant anion gluconate. The cytoplasmic / bath solution contained in mM: K+ 145, gluconate 140, PO−4 3.5, MgSO4 1.2, and 260 μM Ca2+ buffered with 2.0 mM EGTA (Sigma) to 80 nM free Ca2+, pH 6.8; ATP 5, and cAMP 0.1 were added to the cytoplasmic bath as needed. Statistical significance was determined with Student’s t-test. A P value of <0.05 was taken to be significantly different.
SWEAT ELECTROLYTES
Sweat glands of the forearm (25 cm2 area) were stimulated by iontophoretic application of 10−5 M pilocarpine for a duration of 5.00 min using DC current of 4.0 mA. Secreted sweat was collected from the stimulated area on a filter paper hermetically sealed under plastic film. The filter paper was weighed before and after sweat collection. The sweat was diluted by a fixed volume of deionized distilled water. K+, Na+ activities were measured using ion-sensitive electrodes (WPI Model: detectION). Cl− concentration was determined by using chloridometry.
SKIN POTENTIALS
Skin potentials from the pilocarpine-stimulated skin surface were recorded by placing an ECG electrode (KENDAL, Model: MEDITRACE 4603) presoaked in 150 mM KCl solution over a corner portion of the stimulated area. A similar reference electrode was placed over a small area of unstimulated skin that was lightly abrased to gain electrical contact with interstitial fluid. The electrical imbalance between the active recording electrode and the reference electrode, usually < 2 mV, were subtracted from the total potential difference between the two electrodes.
RT-PCR
Sweat ducts were freshly isolated from sweat glands and immediately processed for total RNA extraction. Total RNA was extracted by using Absolutely Nanoprep Kit (Stratagene, La Jolla, CA). RNA was reverse-transcribed using the Sensiscript RT Kit (QIAGEN Inc. CA). The resulting first-strand cDNA was directly used for PCR amplification (TaqPCR Core Kit, QIAGEN Inc. CA). The conditions for PCR reactions were: 3 min at 94°C (initial melt); 35 cycles of 1 min at 94°C, 1 min at 55–60°C, 1 min at 72°C and 72°C 10 min (final extension). For the negative control, RT-PCR was performed in the absence of RT. The PCR products were analyzed by agarose gel electrophoresis stained with ethidium bromide. The primers were constructed on the basis of the published cDNA sequences of CFTR and ENaC from GenBank. The pairs of primers for α-ENaC (accession: BC037417) were sense 5′-GAACAACTCCAACCTCTGGATGTC-3′ and antisense 5′-TGGTGCAGTCGCCATAAT-3′ to generate a 257-bp PCR product; for β-ENaC (NM000336) the primers were sense 5′-TGCTGTGCCTCATCGAGTTTG-3′ and antisense 5′-TGCAGACGCAGGGAGTCATAGTTG-3′ to generate a 277-bp PCR product; for γ-ENaC (X87160) they were sense 5′-TCAAGAAGAATCTGCCCGTGA-3′and antisense 5′-GGAAGTGGACTTTGATGGAAACTG-3′ to generate a 237-bp PCR product.
Results
SPONTANEOUS ELECTRICAL PROPERTIES
Spontaneous transepithelial electrical conductance (Gt) and electrical potential (Vt) of microperfused ducts from both normal and PHA-1 subjects were measured with symmetrical 150 mM NaCl in lumen (± amiloride) and bath. Normal ducts showed significant spontaneous electrogenic transport potentials. In contrast, the PHA-1 ducts showed no spontaneous potentials (Fig.1 and 2). The mean values of the Gt and Vt in PHA-1 ducts were 51 ± 6.0 ms/cm2 and 1.8 ± 1.5 mV respectively (n = 5 ducts from two PHA patients) (Fig 2A). In contrast, the Gt and Vt were significantly larger (Gt = 103 ± 6.0 ms/cm2 and Vt = −16 ± 3 mV, n = 12 ducts from six subjects) in ducts from control subjects (Fig. 2A). However, after application of amiloride to the luminal surface of normal ducts, the values of Vt (−0.2 ± 0.3 mV, n = 4) and Gt (59 ± 5 ms/cm2, n = 5) were similar to those of PHA-1 ducts (Fig. 2B). Luminal amiloride had no detectable effect on the spontaneous electrical properties of ducts from PHA-1 patients (Fig. 1 and 2). Similarly, the PHA-1 ducts conspicuously lacked a gENaC (n = 5) as compared to normal ducts with large spontaneous gENaC (46 ± 10 ms, n = 4, 150 mM NaCl in lumen and bath, Fig.1 & 2C).
Electrical properties of intact microperfused normal and PHA-1 ducts:(A) Representative electrical trace of a normal duct showing large transepithelial potential due to luminal Cl− substitution by the impermeant anion gluconate (150 mM NaCl in the bath and 150 mM NaGlu in the lumen) and a relatively large amiloride-sensitive Na+ conductance indicated by the significant depolarization of Vt and the increased amplitude of transepithelial current pulse-induced voltage deflections caused by luminal amiloride in both the presence and absence of Cl− in the lumen (boxed data). (B) Representative electrical trace of an intact microperfused sweat duct from a PHA-1 patient. Notice that the Vt is relatively small even after complete luminal Cl− substitution. However, the Vt of the PHA-1 patient is comparable to that of normal ducts in the presence or absence of luminal Cl− when Na+ conductance of the normal ducts is blocked with amiloride. Also notice that amiloride has no effect on the electrical properties of PHA-1 ducts, indicating an almost complete loss of ENaC conductance in the apical plasma membrane. The downward voltage deflections are in response to 50 nA transepithelial constant current pulses the magnitude of which is inversely related to transepithelial conductance.
Summary of electrical properties of intact microperfused sweat ducts. (A) Effect of luminal amiloride on spontaneous electrical properties (150 mM NaCl in lumen and bath) of normal and PHA-1 ducts. Notice that Vt and Gt of normal ducts are significantly larger as compared to the values of PHA-1 ducts. However, Vt and Gt of amiloride-inhibited normal ducts are similar to those of PHA-1 ducts. (B) Effect of luminal amiloride on Vt and Gt after luminal Cl− substitution with gluconate (Glu, lumen and bath contained 150 mM NaCl and 150 mM NaGlu, respectively). Notice that the Vt and Gt of normal and PHA-1 ducts are similar only after blocking apical Na+ conductance with amiloride. (C) Amiloride-sensitive ENaC conductance in normal and PHA-1 ducts. Notice that there is a large amiloride-sensitive spontaneous Na+ conductance (150 mM NaCl in lumen and bath) in normal ducts, whereas PHA-1 ducts virtually lacked this conductance. The data represent mean ± standard error, n = 5 ducts each from normal and PHA-1 subjects)
EFFECT OF Cl− SUBSTITUTION IN THE LUMEN
In the absence of luminal amiloride, the Cl− diffusion potentials generated by complete luminal Cl− substitution with the impermeant anion gluconate (150 mM NaCl in the bath / 150 mM NaGlu in the lumen) were distinctly more negative in normal ducts (−83 ± 7 mV, n = 12) compared to PHA-1 ducts (−28 ± 3 mV, n = 5). However, the Vt of normal ducts (Vt = −34 ± 2 mV, n = 5) generated by complete luminal Cl− substitution in the presence of luminal amiloride is comparable to that of PHA-1 ducts in the absence (or presence of amiloride (Fig. 1 and 2B).
EFFECT OF CYTOSOLIC pH ON gENaC IN PERMEABILIZED DUCTS
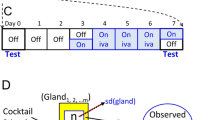
Alkalinization of cytosolic pH activated gENaC in normal ducts, both before and after activation of CFTR with cAMP and ATP (Figs. 3 and 4). In contrast, alkalinization of cytosolic pH had virtually no effect on amiloride-sensitive conductance in PHA ducts either before or after activation of CFTR (Figs. 3 and 4).
Effect of cytosolic pH on ENaC in normal and PHA-1 ducts before activation of CFTR. (A) Representative electrical trace recorded from normal duct after α-toxin permeabilization of basolateral membrane. Removal of amiloride from the luminal perfusate induced a lumen-negative transepithelial Na+ diffusion potential generated by 150 mM KGlu in the cytoplasmic bath and 150 mM NaCl in the lumen (indicated by Vt hyperpolarization). Notice that raising cytoplasmic pH from 6.8 to 8.5 further hyperpolarized Vt, indicating an increase in Na+ diffusion potentials and, hence, gENaC. (B) Representative electrical trace recorded from an α-toxin-permeabilized PHA-1 duct. In marked contrast to normal ducts, washing out luminal amiloride and raising cytoplasmic pH from 6.8 to 8.5 had no effect on Na+ diffusion potentials (no effect on Vt). The large increase in lumen-positive Cl− diffusion potentials (generated by 150 mM NaCl + 10−5 M amiloride in the lumen and 140 mM KGlu in the cytoplasmic bath) after activation of CFTR by adding 0.1 mM cAMP and 5 mM ATP to cytoplasmic bath demonstrates tissue integrity.
Effect of pH on ENaC in normal and PHA ducts after activation of CFTR. (A) Representative electrical trace recorded from normal duct after α-toxin permeabilization of basolateral membrane. Removal of amiloride from the luminal perfusate induced a lumen-negative tranepithelial Na+ diffusion potential under the same conditions as in Figs. 3 (indicated by Vt hyperpolarization). Activation of gCFTR by adding 0.1 mM cAMP + 5 mM ATP to the cytoplasmic bath increased lumen-positive Cl− diffusion potentials (150 mM NaCl + 10−5 M amiloride in the lumen and 140 mM KGlu in the cytoplasmic bath). Washing out amiloride after activation of CFTR hyperpolarized Vt, indicating an increase in Na+ diffusion potentials, which were hyperpolarized further by raising cytoplasmic pH from 6.8 to 8.5. (B) Representative electrical trace recorded from an α-toxin permeabilized PHA-1 duct. In marked contrast to normal ducts, washing out luminal amiloride and raising cytoplasmic pH from 6.8 to 8.5 had no effect on Na+ diffusion potentials (no effect on Vt) either before or after activation of CFTR Cl− conductance with cAMP+ATP. Also the lack of apical amiloride-sensitive ENaC conductance did not seem to affect cAMP+ATP activation of CFTR Cl− conductance in PHA-1 ducts.
cAMP-STIMULATED CFTR IN PERMEABILIZED DUCTS
We then investigated the effect of absence of gENaC in PHA-1 ducts on the cAMP + ATP regulation of CFTR Cl− conductance using basolaterally α-toxin-permeabilized sweat ducts [20, 26]. Application of cAMP and ATP significantly activated gCFTR in both PHA-1 and normal ducts (Figs. 3 and 4). However, no significant difference was noticed in the magnitude of (cAMP + ATP)-activated gCFTR between normal and PHA-1 ducts (Figs. 3, 4 and 5).
Activating gCFTR stimulates gENaC in normal, but not in PHA-1 ducts: Residual gENaC in normal ducts can be stimulated by an order of magnitude following activation of gCFTR by cAMP + ATP in normal ducts after α-toxin permeabilization of the basolateral membrane. In marked contrast, PHA-1 ducts have no gENaC either before or after activation of gCFTR.
EFFECT OF cAMP+ATP ON gENaC IN PERMEABILIZED DUCTS
Activation of gCFTR stimulated gENaC in normal ducts by an order of magnitude, but not in PHA ducts (Fig. 5). There was virtually no effect of amiloride on the electrical properties of the apical membrane of PHA ducts either before or after application of cAMP + ATP (Figs. 3, 4, and 5). In comparison, normal ducts always showed some degree of amiloride sensitivity (even in the complete absence of CFTR activity) that was stimulated further by activation of CFTR (Figs. 4 and 5).
SWEAT ELECTROLYTES
Pilocarpine-induced sweat electrolyte composition indicated that the PHA-1duct is virtually incapable of absorbing salt from isotonic sweat secreted by the secretory coil. The levels of Na+ and Cl− appearing on the skin surface remained isotonic (∼ 150 mM), whereas the sweat from normal subjects was significantly hypotonic (< 50 mM) (Fig. 6A).
Sweat electrolytes and skin potentials. (A) Sweat electrolyte concentrations from normal and PHA-1 patients. Isotonic concentrations of sweat Na+ and Cl− in PHA-1 patients indicated complete lack of salt absorption from the primary sweat secreted by the sweat gland secretory coil. In contrast, the fact that sweat salt concentration is significantly hypotonic in normal subjects indicates salt absorption by the normal sweat duct. (B) Reversal of pilocarpine-induced skin potentials in PHA-1 patients. The lack of ENaC in PHA-1 patients resulted in positive skin potentials in these subjects, whereas the skin potentials always remained significantly negative without any overlap between these two groups. These results suggest that skin potentials may serve as a diagnostic tool in identifying PHA-1 patients.
SKIN POTENTIALS
After pilocarpine stimulation of sweat secretion, skin potentials always remained significantly negative (−13 ± 7.0 mV, n = number of human subjects = 6) in normal subjects. In marked contrast, skin potentials remained significantly positive (+22 ± 11, n = 2) in PHA-1 subjects (Fig. 6B).
mRNA IS EXPRESSED IN PHA DUCTS
Even though the ENaC function was not observed in the apical membrane of the PHA ducts, the mRNA for all the three subunits (α,β,γ) of ENaC was expressed (Fig. 7B). However, surprisingly the mRNA signal for β-ENaC was observed in both PHA-1 patients, whereas an mRNA signal for β-ENaC was detected in only one out of five normal subjects (Fig. 7A).
Expression of mRNA for ENaC subunits in normal and PHA ducts. RT-PCR shows that ducts from normal and PHA-1 ducts express mRNA for all three (α, β, γ) subunits of ENaC that are normally expressed in other Na+-absorbing epithelia such as airways and kidney. These results also show that lack of amiloride-sensitive ENaC in PHA-1 ducts is not due to lack of mRNA expression in these ducts.
Discussion
FUNCTIONAL INTERACTION BETWEEN ENaC AND CFTR
Most salt (NaCl)-absorbing epithelial cells depend on the activities of ENaC and CFTR in the apical plasma membrane for transporting Na+ and its co-ion Cl− across the apical membrane. Early studies indicated close coordination between these two principal epithelial ion channel activities even though the nature of such coordination may be tissue-specific [20, 30]. In the reabsorptive sweat duct, not only are these two channels activated simultaneously, but also the activity of CFTR seems to stimulate ENaC activity [20]. Paradoxically, the activities of CFTR and ENaC are thought to be reciprocal in airway epithelium., that is, CFTR seems to exert inhibitory control over ENaC so that lack of CFTR function in the apical plasma membrane of CF airway epithelial cells apparently enhances ENaC activity [9, 30]. While these observations indicate that CFTR regulates ENaC activity, we do not know whether ENaC activity regulates CFTR function. Ex vivo studies suggested that ENaC expression might stimulate CFTR Cl− currents [12]. However, whether such regulation occurs in vivo is unknown. In order to address this question, we turned to native human sweat ducts from patients with the systemic form of type-1 PHA. Early studies indicated that sweat glands were affected by mutations in the ENaC channels as indicated by elevated sweat salt concentration. Even though these mutations seem to affect trafficking of the ENaC to the plasma membrane [7, 27], the magnitude to which gENaC is affected in sweat duct is not known. Accordingly, we investigated the affect of PHA mutations on the functional expression of ENaC in this tissue.
VIRTUAL LACK OF ENaC FUNCTION IN PHA-1 SWEAT DUCTS
Active transepithelial salt transport generates a significant luminal negative transepithelial potential (−10 to −20 mV) in symmetric bilateral 150 mM NaCl due to electrogenic salt absorption in this tissue [21]. Blocking gENaC with amiloride completely eliminates salt absorption as well as the spontaneous transepithelial electrical potential (Figs.1 and 2A) [16, 22]. Therefore, the almost complete absence of transepithelial potential, the virtual lack of effect of amiloride on transepithelial potential, and the lower transepithelial conductance (Figs. 1 and 2A) all reflect the total absence of electrogenic transport due to the absence of gENaC in the apical membrane in PHA-1 patients. Complete loss of ENaC function results in salt-wasting hypotension and hyperkalemia in pHA-1 patients [5, 13, 27]. Since these autosomal recessive, loss-of-function mutations seem to interfere with normal trafficking of assembled ENaC channels [7, 27], the lack of effect of amiloride is likely due to the absence of at least one of the functional subunits of ENaC in the plasma membrane. Alternatively, mutant ENaC channels may escape the cellular quality control and traffic to the plasma membrane, but remain inactive. If the latter were the case, stimulation of mutant ENaC channels might have potential therapeutic value if these channels retain some Na+ channel function. Therefore we investigated whether the channel could be stimulated.
gENaC IN PHA DUCTS CANNOT BE ACTIVATED
Previously we showed that ENaC activity requires CFTR channel function in this tissue [20]. Accordingly, we maximally activated gCFTR with cAMP + ATP after α-toxin permeabilization of the basolateral membrane to stimulate gENaC. Figs. 3, 4 and 5 show that gENaC stimulation following CFTR activation occurs only in normal, but not in PHA-1 ducts. Furthermore, we previously reported that gENaC is activated by cytosolic alkaline pH in normal ducts [25]. Alkaline pH activation of gENaC appears to be independent of ENaC activation by CFTR in the presence of cAMP and ATP in normal ducts [25] (Fig. 3 and 4). However, gENaC was not activated by alkaline pH in ducts from PHA-1 patients irrespective of the status of CFTR activity (Figs. 3 and 4). These results indicate either that, as expected, there is virtually no ENaC expressed in the plasma membrane [7] or that, even if some ENaC escapes to the plasma membrane, it is dysfunctional.
CFTR ACTIVITY IS INDEPENDENT OF ENaC
Complete Cl− substitution by gluconate in the lumen generated relatively smaller transepithelial potentials in PHA-1 ducts as compared to that of normal ducts (Figs. 1 and 2B). This could be either due to reduced gCFTR or to the loss of gENaC and the corresponding Na+ EMF (electromotive force) causing apical membrane hyperpolarization and transepithelial potential depolarization [21, 23], or both. However, the luminal Cl− substitution-induced trans- epithelial potentials in normal and PHA-1 ducts appeared to be almost identical after blocking ENaC of normal ducts with amiloride (Figs.1 and 2B). These results show that the loss of Na+-EMF, but not the loss of gCFTR across the apical membrane is primarily responsible for smaller Cl− substitution-induced transepithelial potentials in PHA-1 ducts.
In addition, the spontaneous transepithelial conductance with 150 mM NaCl in the lumen and bath of normal ducts appeared to be almost double that of PHA-1 ducts (Fig. 2A). These results seem to reflect a lack of gENaC rather than decreased gCFTR in PHA-1 ducts. The fact that gCFTR in amiloride-inhibited normal ducts appears to be almost the same as that of PHA-1 ducts (Fig. 2A) supports this conclusion. However, comparing the magnitude of spontaneous gCFTR between normal and PHA-1 ducts may not be fully appropriate because CFTR might not be spontaneously maximally activated [23]. Hence, we permeabilized the basolateral membrane so that the magnitude of fully activated apical gCFTR could be compared between normal and PHA-1 ducts. Fig. 5 shows no significant difference in the magnitude of (cAMP+ATP)-activated gCFTR between normal and PHA-1 ducts. These results taken together with the facts that CFTR can be normally activated after blocking ENaC with amiloride in normal ducts (Figs. 3A and 4A) or in the absence of ENaC in secretory epithelial cells [2] indicate that ENaC function is not required for normal CFTR activity in sweat duct epithelial cells.
COMPLETELY ELECTROCONDUCTIVE ENaC-DEPENDENT Na+ ABSORPTION
Transepithelial salt absorption requires simultaneous activities of both CFTR and ENaC channels in order to maintain electroneutrality during transport activity [20]. Hence, loss of function in one channel prevents absorption of Na+ as well as Cl− [18]. The almost complete lack of salt absorption in the face of normal CFTR Cl− conductance in PHA-1 ducts (Figs. 3B, 4B and 5) indicates that there is neither an alternative Na+ channel nor a functional carrier transporter (such as Na/Cl or Na+/K+/2Cl− co-transport) [22, 26] to accommodate Na+ absorption, which evidently occurs exclusively through the ENaC elctroconductive pathway.
REVERSED SKIN POTENTIALS AS A DIAGNOSTIC PROPERTY
Sweat salt concentration is elevated in both CF as well as PHA-1 patients [3, 13]. Hence the classic sweat test for elevated electrolyte concentrations cannot distinguish between these two groups. However, even though a loss in either CFTR or ENaC results in the same functional consequence (i.e., elevated sweat salt concentration), we know that the electrical signals generated by inhibition of either one of these two ion channels are strikingly opposite. That is, inhibition of CFTR either by blockers or by mutation increases transepithelial potentials [17, 24], while inhibition of ENaC either by amiloride [21] (Figs. 1 and 2A] or by mutation decreases transepithelial potentials (Figs. 1 and 2). Since ductal electrogenic transport activity appears to be the predominant source of skin potential associated with sweat secretion [3], we investigated the effect of the lack of ENaC activity on the skin potentials associated with pilocarpine-induced sweat secretion in normal as well as PHA-1 patients. Surprisingly, in both PHA-1 patients the skin potentials were dramatically opposite to normal as well as CF patients (Fig. 6) [27]. Inhibition of ENaC either by amiloride, as in normal ducts, or by mutations, as in PHA-1 ducts, merely abolishes transepithelial potential in isolated ducts under microperfused conditions (150 mM NaCl in lumen and bath, Figs. 1 and 2A). Therefore, one would not expect such large positive skin potentials in PHA-1 patients. However, it must be noted that these are the proximal ducts that are intertwined with the secretory coil. We speculate that the straight portions of the sweat duct leading to the skin surface, which are very narrow and difficult to microperfuse, may have different physiological properties with respect to their ability to secrete either proton or K+ that might be pronounced in PHA-1 much more than in normal ducts, contributing to these distinctly positive skin potentials. Even though identification of the exact physiological basis of large positive skin potentials in PHA-1 patients requires further investigation, these empirical observations show that skin potential measurement could be a useful diagnostic tool to distinguish PHA-1 patients from normal individuals and CF patients.
IMPLICATIONS
Complete lack of electrogenic salt transport [13], virtual loss of ENaC activity, and the expression of mRNA for the α,β,γ ENaC subunits in the human sweat duct, airways and kidney [4, 13, 27] indicate that the same ENaC channel is expressed in all these tissues. Therefore, reciprocal inhibition of ENaC in the airways as opposed to the simultaneous activation of ENaC in the sweat duct by CFTR must reflect different cell-specific intracellular signaling mechanisms rather than differences in the Na+ channels [20, 30].
Normal CFTR activity in the complete absence of ENaC in PHA-1 ducts suggests that these two important ion channels critical to salt absorption can be trafficked to the plama membrane independently of each other. More significantly, virtual loss of transepithelial transport activity does not seem to affect normal expression of CFTR in PHA-1 patients. These results suggest that unlike ENaC whose activity is closely tied to the Na+ transport demand and aldosterone levels [27], CFTR expression may not be strictly tied to transepithelial Cl− absorption alone. Besides Cl− transport, CFTR seems involved in other vital physiological functions such as HCO −3 permeability [14, 15, 26, 28] and regulation of Na+ /H+ [1] and C1−/HCO − 3 (6) exchangers. Therefore, exclusive linkage of CFTR expression to Cl− transport activity could derail other regulatory functions of CFTR. Hence, it appears that the aforementioned CFTR-dependent vital transport functions may have been relatively unaffected owing to normal expression of this regulatory ion channel protein in the face of virtual absence of salt transport activity in type-1 pseudohypoaldosteronism
References
A. Bagorda L. Guerra F. Di Sole C. Hemle-Kolb R. Cardone T. Fanelli S.J. Reshkin S.M. Gisler H. Murer V.J. Casavola (2002) ArticleTitleReciprocal protein kinase A regulatory interactions between cystic fibrosis transmembrane conductance regulator and Na+/H+ exchanger isoform 3 in renal polarized epithelial cell model J. Biol. Chem. 277 21480–21488
C.L. Bell P.M. Quinton (1993) ArticleTitleRegulation of CFTR Cl− conductance in secretion by cellular energy levels Am. J. Physiol. 264 C925–C931
J. Bijman P.M. Quinton (1984) ArticleTitleInfluence of abnormal Cl− impermeability on sweating in cystic fibrosis Am. J. Physiol. 247 C3–C9
L. H. Burch C.R. Talbot M.R. Knowles C.M. Canessa B.C. Rossier R.C. Boucher (1995) ArticleTitleRelative expression of the human epithelial Na+ channel subunits in normal and cystic fibrosis airways Am. J. Physiol. 269 C511–C518
S.S. Chang S. Grander A. Hanukoglu A. Rosler P.M. Mathew I. Hanukoglu L. Schild Y. Lu R.A. Shimkets N.C. Williums B.C. Rossier R.P. Lifton (1996) ArticleTitleMutations in subunits of the epithelial sodium channel cause salt wasting with hyperkalaemic acidosis, pseudohypoaldosteronism type-1 Nat. Genet. 12 248–253
J.Y. Choi D. Muallem K. Kiselyov M.G. Lee P.J. Thomas (2001) ArticleTitleAberrant CFTR-dependent HCO −3 transport in mutations associated with cystic fibrosis Nature 410 94–97
D. Firsov I. Gautschi L. Schild (1998) ArticleTitleThe heterotetrameric architecture of the epithelial sodium channel (ENaC) EMBO J. 17 344–352
D. Firsov R.M. Nicoud S. Gruender L. Schild B.C. Rossier. (1999) ArticleTitleMutational analysis of cystine-rich domains of the epithelium sodium channel (ENaC). Identification of cysteines essential for channel expression at the cell surface J. Biol. Chem. 274 2743–2749
B.R. Grubb R.N. Vick R.C. Boucher (1994) ArticleTitleHyperabsorption of Na+ and raised Ca2+ mediated Cl− secretion in nasal epithelia of CF mice Am. J. Physiol. 266 C1478–C1483
A. Hanukoglu T. Bistritzer Y. Rakover A. Mandelberg (1994) ArticleTitlePseudohypoaldosteronism with increased sweat and saliva electrolyte values and frequent lower respiratory tract infections mimicking cystic fibrosis J. Pediatr. 125 752–755
E. Hummler J.D. Horisberger (1999) ArticleTitleGenetic disorders of membrane transport. V. The epithelial sodium channel and its implication in human disease Am. J. Physiol. 276 IssueID3 G567–G571
H.L. Ji M.L. Chalfant B.J. Jovov P. Lockhart S.B. Parker C.M. Fuller B.A. Stanton D.J. Benos (2000) ArticleTitleThe cytosolic termini of the beta- and gamma-ENaC subunits are involved in the functional interactions between cystic fibrosis transmembrane conductance regulator and epithelial sodium channel J. Biol. Chem. 275 27947–27956
E. Kerem T. Bistritzer A. Hanukoglu T. Hofmann Z. Zhou W. Bennett E. MacLaughlin P. Barker M. Nash L. Quittel R. Boucher M.R. Knowles (1999) ArticleTitlePulmonary epithelial sodium channel dysfunction and excess airway liquid in pseudohypoaldosteronism The New Engl. J. Med. 341 156–162
D.B. Luckie C.N. Singh J.J. Wine J.H. Wilterding (2001) ArticleTitleCFTR activation raises extracellular pH of NIH/3T3 mouse fibroblasts and C127 epithelial cells J. Membrane Biol. 179 275–284
J.H. Poulsen H. Fischer B. Illek T.E. Machen (1995) ArticleTitleBicarbonate conductance and pH regulatory capability of cystic fibrosis transmembrane conductance regulator Proc. Natl. Acad. Sci. USA 91 5340–5344
P.M. Quinton (1981) ArticleTitleEffects of some ion transport inhibitors on reabsorption in intact and perfused single human sweat glands Pfluegers Arch. 391 309–313
P.M. Quinton (1983) ArticleTitleChloride impermeability in cystic fibrosis Nature 301 421–422
P.M. Quinton (1999) ArticleTitlePhysiological basis of cystic fibrosis: A historic perspective Physiol. Rev 79 S3–S22
P.M. Quinton M.M. Reddy (1992) ArticleTitleControl of CFTR Cl conductance by ATP levels through non-hydrolytic binding Nature 360 79–81
Reddy, M.M., Light, M.J., Quinton, P.M. Activation of the epithelial Na+ channel (ENaC) requires CFTR Cl− channel function. Nature 402: 301–304
M.M. Reddy P.M. Quinton (1999) ArticleTitleIntracellular potentials of microperfused human sweat duct cells Pfluegers Arch 410 471–475
M.M. Reddy P.M. Quinton (1991) ArticleTitleIntracellular potassium activity and the role of potassium in transepithelial salt transport J. Membrane. Biol. 119 199–210
M.M. Reddy P.M. Quinton (1992) ArticleTitlecAMP activation of CF-affected Cl− conductance in both cell membranes of an absorptive epithelium J. Membrane. Biol. 130 49–62
M.M. Reddy P.M. Quinton (1999) ArticleTitleBumetanide blocks CFTR GC1 in the native sweat duct Am. J. Physiol. 276 C231–C237
M.M. Reddy P.M. Quinton (2000) ArticleTitleCFTR independent cytosolic basic pH activation of ENaC in the native sweat duct Ped. Pulmonol. 20 IssueIDSuppl 2000
M.M. Reddy P.M. Quinton (2003) ArticleTitleControl of dynamic CFTR selectivity by glutamate and ATP in epithelial cells Nature 423 756–759
J.A. Schafer (2002) ArticleTitleAbnormal regulation of ENaC: syndromes of salt retention and salt wasting by the collecting duct Am. J. Phyiol. 283 F221–F235
Y. Sohma M.A. Gray Y. Imai B. Argent (2000) ArticleTitleHCO −3 transport in a mathematical model of the pancreatic ductal epithelium J. Membrane. Biol. 176 77–100
S.S. Strautnieks R.J. Thompson R.M. Gardiner E. Chung (1996) ArticleTitleA novel splice site mutation in the gamma subunit of the epithelial sodium channel gene in three type-1 pseudohypoaldosteronism type 1 families Nat. Genet. 13 248–250
M.J. Stutts C.M. Canessa J.C. Olsen M. Hamrick J.A. Cohn B.C. Rossier R.C. Boucher (1995) ArticleTitleCFTR as a cAMP-dependent regulator of sodium channels Science 269 847–850
Acknowledgments
We thank K. Tayler and Sucharitha Reddy for technical assistance and Mrs. Joanne Albrecht for clerical assistance. This work was funded by grants from the USPHS-NIH, USCF Foundation, The Olmsted Trust, and The Cystic fibrosis Research, Inc.
Author information
Authors and Affiliations
Corresponding author
Additional information
An erratum to this article is available at http://dx.doi.org/10.1007/s00232-006-1003-4.
Rights and permissions
About this article
Cite this article
Reddy, M., Wang, X., Gottschalk, M. et al. Normal CFTR Activity and Reversed Skin Potentials in Pseudohypoaldosteronism. J Membrane Biol 203, 151–159 (2005). https://doi.org/10.1007/s00232-005-0740-0
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/s00232-005-0740-0