Abstract
Purpose
Dysregulation of angiogenesis and inflammation play important roles in the development of atherosclerosis. Rosuvastatin (RST) was widely used in atherosclerosis therapy. Genetic variations of transporters may affect the rosuvastatin concentration in plasma and reflect different clinical treatment. The aim of this study was to explore the drug transport related single-nucleotide polymorphisms (SNPs) on RST pharmacokinetic and the further on pro-angiogenic and pro-inflammatory factors.
Methods
A total of 269 Chinese patients with hypercholesterolemia and diabetes mellitus were enrolled. They were treated with RST to lower cholesterol. The plasma concentration of RST was determined using a validated UPLC-MS/MS method. Seven single-nucleotide polymorphisms (SNPs) in six genes were genotyped using the Sanger dideoxy DNA sequencing method. The serum concentrations of inflammation markers were determined using ELISA kits.
Results
ABCG2 421C > A (rs2231142) and SLCO1B1 521 T > C (rs4149056) variations were highly associated with plasma concentrations of RST (P < 0.01, FDR < 0.05). The serum MCP-1, sVCAM-1, and TNF-α levels were significantly different between the ABCG2 421C > A and SLCO1B1 521 T > C genetic variation groups (P < 0.01). RST concentration was negatively correlated with sVCAM-1 concentration (r = 0.150, P = 0.008).
Conclusion
ABCG2 421C > A (rs2231142) and SLCO1B1 521 T > C (rs4149056) genetic variants affect RST concentration significantly and potentially affect serum levels of pro-inflammatory and pro-angiogenic markers. The effects on anti-inflammation might not be related to high plasma exposure of RST.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inhibitors of 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase (statins) are the most relevant drugs used to lower serum cholesterol levels [1]. They are highly effective in the prevention of cardiovascular events in atherosclerosis therapy [2]. Rosuvastatin (RST) is one of the most globally popular cholesterol-reducing drugs. It is used for atherosclerotic plaque stability, angiogenesis, and anti-inflammation [3, 4]. Genetic variant on transporters may influence the RST exposure in body and further on clinical results.
In previous studies, the anti-inflammatory effect of RST has been reported to reduce the activation of the mevalonate pathway by inhibiting HMG-CoA reductase [5]. Statins reduced the isoprenylated and geranylgeranylated protein levels, and in particular prenylated Ras level. The statin-induced Ras inhibition reduces the activity of the transcription factor nuclear factor kappa B (NF-kB) [6]. Some studies have indicated that statin therapy leads to suppression of NF-kB activity with further decrease in pro-inflammatory cytokines. Others have reported that statins decrease IL-6 and TNF-α production in monocytes of patients with hypercholesterolemia [7].
Atherosclerosis is responsible for several important adverse vascular events. Recent research has indicated that atherosclerosis might be associated with disregulation of neovascularization in diabetes [8, 9]. In patients with diabetes mellitus, atherosclerosis, which accounts for most cardiovascular morbidity and mortality, influences the disregulation of angiogenesis [10]. The serum levels of pro-angiogenic molecules such as MCP-1 and VCAM-1 are associated with neovascularization and inflammatory factor infiltration [11]. Rosuvastatin might exert anti-angiogenic and anti-inflammation effects by preventing atherosclerotic cardiovascular diseases.
High plasma exposure to RST and genetic factors play crucial roles in cholesterol-reduction and anti-inflammation outcomes. Rosuvastatin is metabolized by isoenzyme CYP2C9, and transporters play an important role in the disposition of RST [12]. Several studies have revealed that SLCO1B1, which encodes the OATP1B1 importer contributed to RST passive membrane permeability and the genotype variation exist frequently in East Asians. The ABC cassette transporter gene family including ABCG2 and ABCB1 are widely expressed on important physiological barriers [13,14,15,16]. The variation in genotype is a potentially crucial heredity factor in the pharmacokinetic of RST. Gene polymorphisms might influence the body’s exposure to RST and the concentrations of pro-inflammatory and pro-angiogenic cytokines.
The genotype variation influence on the exposure to RST in Chinese Han people is unclear and the correlation between plasma concentration of RST and serum level of pro-inflammatory and pro-angiogenic cytokines in the course of atherosclerosis and diabetes are still unknown. The present study was designed to evaluate the concentrations of pharmacokinetic-related SNPs and subsequently assessed the angiogenic factors and pro-inflammatory cytokines in patients with hypercholesterolemia and diabetes mellitus.
Materials and methods
Patients
A total of 269 patients with hypercholesterolemia and diabetes mellitus (DM) were recruited between January 2018 and April 2019 from the China-Japan Friendship Hospital. All the patients were treated with RST (AstraZeneca, 10 mg daily) for hypercholesterolemia for more than 4 weeks. Patients’ baseline information, including demographics and biochemical measurements were obtained from the database of the hospital. All patients were with Chinese Han population genetic background. The study was approved by the Bioethical Committee of China-Japan Friendship Hospital and all the participants gave informed consent.
Hypercholesterolemia and diabetes mellitus were diagnosed according to the criteria of The American Diabetes Association (2014) and The European Society of Cardiology (ESC) (2013). The exclusion criteria were as follows: 1) RST combined with other statins for treatment or pretreated with other statins in 2 weeks; 2) age ≥ 80 years; 3) kidney and renal insufficiency (defined as serum CREA concentration is thrice greater than 345 μmol/L; serum alanine aminotransferase (ALT) concentration is thrice greater than 120 U/L; renal transplantation or cirrhosis diagnosis); and 4) inflammatory or malignant diseases.
Determination of RST concentration in plasma
Blood samples were collected from each eligible patient in the morning at 10–12 h after dosing RST and stained in EDTA-coated tubes. The plasma and blood cells were separated within 2 h. Centrifugated samples at 3000 rpm for 10 min at 4 °C and stored at −80 °C until further use.
A selective and sensitive ultra-performance liquid chromatography-tandem mass spectrometry (UPLC-MS/MS) method was established and validated for the simultaneous quantification of RST in human plasma. Liquid–liquid extraction using 600 μL of acetonitrile was adopted to extract RST and the internal standard (IS; RST-d6) from 200 μL of human plasma. The analytes were chromatographically separated using an Acquity UPLC BEH C18 column (2.1 mm × 50 mm, 1.7 μm) with 0.1% FA in acetonitrile and 1 mM ammonium formate in water. The mobile phase was produced with a gradient of 30%–70% 0.1% FA acetonitrile at a flow rate of 0.3 mL/min. The total run time was 5 min. The mass detection was performed using a Waters Xevo TQ-S triple-quadrupole mass spectrometer with the positive electro-spray ionization mode. The mass transitions selected were m/z 481.9 → 258.1 and m/z 487.9 → 264.1 to quantify RST and IS, respectively.
Genotyping
Genomic DNA was mainly isolated from the peripheral blood samples using the TIANamp Blood DNA Kit (TianGen Biotech, Beijing, China). The quality control of DNA was based on the absorbance ratio at A 260/A280 (1.8–2.0) and the concentration of DNA was determined using Nano Drop 2000. For genotyping, we adopted the Sanger dideoxy DNA sequencing method using the ABI 3730xl-full automatic sequencing instrument (ABI Co; Majorbio Biotechnology Co., Ltd., Beijing, China). Seven genes were detected in our research. ABCG2 421A, SLCO1B1 521C, ABCB1 3435G, ABCB1 2677C, SLCO1B3 334A, SLCO2B1 1457 T and CYP2C9 1075C were detected as variant alleles for the respective genes.
Detection of cytokine levels in plasma
The serum concentrations of IL-1β, IL-6, TNF-α, MCP-1, IFN-γ, and sVCAM-1 were measured using the Human ELISA kits (Invitrogen; Thermo Fisher Scientific, Inc.), according to the manufacturer’s instruction.
Statistical analysis
All data analyses were performed using SAS 9.4 (SAS Institute, Cary, NC, USA). Categorical data are presented as percentage and continuous variables are expressed as mean ± SD. The genotype frequencies were tested for Hardy–Weinberg equilibrium. Linear regression was used to assess the clinical baseline characteristic up on plasma exposure to RST. A logistic regression analysis was used to assess the effects of the baseline features and genotypes. The results with P values <0.05 were considered statistically significant. A univariate linear regression analysis was performed to assess the correlation of RST concentration with lipid profile and cytokines.
Results
Effects of genotypes on the plasma concentration of RST
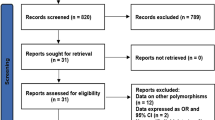
In this study, the 269 patients were successfully genotyped. The genotype distribution of the seven SNPs is summarized in Table 1. The frequency distribution of all the SNPs was consistent with Hardy–Weinberg equilibrium. The RST concentration in the plasma of patients with the seven different SNPs ranged from 8.68 ± 4.69 to 16.74 ± 2.77 ng/mL.
The mean concentration of RST was significantly higher in the patients carrying ABCG2 421A than in non-carriers of this allele. The effects of this allele remained significant even after being adjusted by the baseline characteristics and FDR (P = 5.75 × 10−4, FDR = 0.0086). For SLCO1B1, patients with one or two copies of the variant allele had a significantly high plasma exposure to RST. The significance was found even after multiple testing (P = 0.001, FDR = 0.015). These results are listed in Table 1 and Fig. 1.
The gene-dose effect was not observed in the three genotypes of the two SNPs. In addition, plasma exposure to RST in patients with ABCB1, SLCO1B3, SLCO2B1 and CYP2C9 was not significantly different (P > 0.01, FDR > 0.05).
Effects of genotypes on plasma cytokine levels
On the basis of genetic variations, the 269 eligible patients were divided into different groups. The patients were divided into ABCG2 421A carriers and non-carriers; SLCO1B1 521C carriers and non-carriers. The clinical baseline characteristics and group information are summarized in Table 2. There were no significant differences detected in terms of age, sex, BMI, medical history, and drug combinations. The HbA1c, HDL-cholesterol, LDL-cholesterol, and triglyceride serum concentrations among the genetic variation groups were not statistically different.
The cytokine concentrations in the plasma are shown in Table 3. Among the six groups, the serum levels of factors, TNF-α, MCP-1, and sVCAM-1 showed a significant difference in patients carrying ABCG2 421A or SLCO1B1 521C (Fig. 1). As shown in Table 3, the serum TNF-α level was 7.98 ± 3.13 pg/mL in the ABCG2 421AA and ABCG2 421 AC groups and 15.11 ± 5.13 pg/mL in the ABCG2 421 CC group. The serum MCP-1 level was significantly lower in the ABCG2 421AA and AC group compared to ABCG2 421CC group (99.39 ± 37.16 vs. 126.44 ± 44.11 pg/mL). The serum sVCAM-1 level was also significantly lower in the ABCG2 421AA and AC group compared to ABCG2 421CC group (1043.43 ± 249.27 vs. 1194.36 ± 263.95 ng/mL). Patients carrying the SLCO1B1 521C allele produced significantly lower serum levels of TNF-α, MCP-1, and sVCAM-1. The serum level of the three factors was 7.27 ± 3.60 pg/mL, 79.92 ± 29.18 pg/mL, and 984.51 ± 183.98 ng/mL in the SLCO1B1 521 CC and SLCO1B1 521 TC groups and 12.08 ± 5.39 pg/mL, 124.24 ± 44.96 pg/mL, and 1187.08 ± 276.81 ng/mL in the SLCO1B1 521TT group, respectively.
The concentration of IL-1β, IL-6, and IFN-γ in the plasma is shown in Table 3. There were no significant differences between the genotype groups.
Correlation analysis
The univariate regression analysis results between RST concentration and lipid profile such as HDL-cholesterol, LDL-cholesterol, and triglyceride serum concentrations and pro-angiogenic and pro-inflammatory factors such as TNF-α, MCP-1, and sVCAM-1 are shown in Fig. 2. No significant correlations were observed between RST concentration and triglyceride, CK, and HbAlc levels. The results show a positive correlation between RST concentration and HDL-cholesterol levels and a negative correlation between RST concentration and LDL-cholesterol levels. A negative correlation between RST concentration and sVCAM-1 level was found between the ABCG2 and SLCO1B1 genotype groups (r = −0.150, p = 0.008 for AC and AA group; r = −0.171, p = 0.003 for CC group and r = −0.170, p = 0.003 for TC and CC group; r = −201, p = 0.007 for TT group, respectively).
Discussion
Our study revealed that genotype variation in ABCG2 421C > A and SLCO1B1 521 T > C were associated with the high systemic exposure to RST. Low dose of RST can reduce serum levels of pro-inflammatory cytokines and a significant difference was among genotype variations. To the best of our knowledge, we identified for the first time the relationship between RST concentration and pro-inflammatory cytokines in patients with hypercholesterolemia and diabetes mellitus.
The human ABCG2 gene belonging to the ABC gene family encoded BCRP/ABCG2 protein. BCRP/ABCG2 protein is a key transporter driving the efflux of diverse drugs, leading the drug resistance in target cells and mediating the drug pharmacokinetic and toxicokinetic profiles [14]. ABCG2 plays important physiological roles in limiting drug’s absorption, distribution, elimination and excretion. SLCO1B1 encoded OATP1B1 protein. OATP1B1 is almost exclusively expressed in human hepatocytes. It accepts widely therapeutic drugs, as its substrates, suggesting that OATP1B1 plays a crucial role in the hepatic uptake and clearance of these therapeutic drugs [17].
Among all SNPs in our study, the polymorphisms of ABCG2 421C > A played important roles in the systemic exposure of RST (P < 0.01, FDR < 0.05). The mutation frequency of ABCG2 421C > A was obviously higher in East Asians than in Caucasians [18]. The variation in ABCG2 was proved to be the primary genetic determinant of the pharmacokinetic difference in RST exposure in Chinese population. SLCO1B1 521 T > C was significantly correlated with RST-induced myopathy in previous studies [19]. This might be due to the transporters such as OATP1B1 encoded by SLCO1B1. In our study, subjects carrying SLCO1B1 521C showed significantly higher serum concentrations than those of non-carriers (P < 0.01, FDR < 0.05). The transporters were involved in the disposition of RST, and gene polymorphisms played important roles in the pharmacokinetics of RST.
According to the ABCG2 and SLCO1B1 genotypes, the patients were divided into different groups in our study. The results proved that the effect of RST on the potent pro-angiogenic factors MCP-1 and sVCAM-1 is different. MCP-1 and sVCAM-1 levels in the serum were significantly lower in patients with hypercholesterolemia and diabetes mellitus carrying the ABCG2 421A or SLCO1B1 521C alleles than in the non-carriers. Furthermore, in the correlation analysis, positive results were observed between RST concentration and sVCAM-1 level. Previous studies have showed anti-angiogenic effect of statins in patients suffering from inflammation-dependent pathologies, diabetes type 2, and atherosclerosis without current ischemic episodes without hypoxia [20,21,22]. The pro- and anti-angiogenic effect of statins might be related to the systemic exposure and affected by gene polymorphism.
Atherosclerosis is a chronic inflammatory arterial disease. Statin therapy leads to the suppression of NF-KB activity with a further decrease in pro-inflammatory cytokines [23]. In our study, the TNF-α concentration in the plasma was significantly lower in the ABCG2 421A and SLCO1B1 521C groups (P < 0.001). There were no differences among the genetic variation groups in the IL-6, IL-1b, and IFN-γ concentrations. Statins were found to have an inhibitory effect on the NF-KB signaling pathway. They effectively suppress NF-KB activity and inflammatory pathways to decrease inflammation in the vascular and non-vascular systems [6]. According to our results, significant differences were observed in the TNF-α concentration among the genotype variants, while the correlation between RST concentration and pro-inflammatory factor serum levels was not detected. These results indicated that the gene polymorphisms of ABCG2 421C > A and SLCO1B1 521 T > C influence on serum cytokine levels may be not relate to RST concentration singly. Genetic variants and other baseline characteristics (such as physician disease and inflammation response) may affect the anti-inflammation of RST multiplicate.
There is overwhelming evidence that inflammation and angiogenic markers such as MCP-1, sVCAM-1, IL-1b, TNF-, IL-6, and IFN-γ play a critical role in the development of atherosclerosis. In patients with type 2 diabetes, they are produced at high levels with acute coronary syndrome. It could be associated with increased risk of atherosclerosis development in patients with diabetes [24, 25]. Gene polymorphisms affect the pharmacokinetic and metabolism profiles of RST. The correlation between RST concentration and inflammation markers was only observed for sVCAM-1. The effect of gene polymorphism on RST anti-inflammation should be validated by future studies in a large sample.
Conclusions
Gene polymorphisms of ABCG2 421C > A (rs2231142) and SLCO1B1 521 T > C (rs4149056) affect RST concentration significantly and potentially affect the serum levels of pro-inflammatory and pro-angiogenic markers in patients with hypercholesterolemia and diabetes mellitus treated with RST. The genotype effects on anti-inflammation were not related to the high plasma exposure of RST. These findings offer further insight into the anti-inflammatory mechanism of RST.
References
Ioannidis JPA (2014) More than a billion people taking statins? Potential implications of the new cardiovascular guidelines[J]. JAMA 311(5):463–464
Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH et al (2014) 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association task force on practice guidelines. J Am Coll Cardiol 63:2889–2934
Shin SK, Cho JH, Kim EJ, Kim EK, Park DK, Kwon KA, Chung JW, Kim KO, Kim YJ (2017) Anti-inflammatory and anti-apoptotic effects of rosuvastatin by regulation of oxidative stress in a dextran sulfate sodium-induced colitis model. World J Gastroenterol 23(25):4559–4568
Kırzıoğlu FY, Tözüm Bulut M, Doğan B, Fentoğlu Ö, Özmen Ö, Çarsancaklı SA, Ergün AG, Özdem M, Orhan H (2017) Anti-inflammatory effect of rosuvastatin decreases alveolar bone loss in experimental periodontitis. J Oral Sci 59(2):247–255
Volonte D, Liu Z, Musille PM, Stoppani E, Wakabayashi N, Di YP, Lisanti MP, Kensler TW, Galbiati F (2013) Inhibition of nuclear factor-erythroid 2-related factor (Nrf2) by caveolin-1 promotes stress-induced premature senescence. Mol Biol Cell 24(12):1852–1862
Rashidian A, Muhammadnejad A, Dehpour AR, Mehr SE, Akhavan MM, Shirkoohi R, Chamanara M, Mousavi SE, Rezayat SM (2016) Atorvastatin attenuates TNBS-induced rat colitis: the involvement of the TLR4/NF-kB signaling pathway. Inflammopharmacology. 24(2–3):109–118
Shen DZ, Xin SL, Chen C, Liu T (2013) Effect of atorvastatin on expression of TLR4 and NF-κB p65 in atherosclerotic rabbits. Asian Pac J Trop Med 6(6):493–496
Martínez-Hervás S, Sánchez-García V, Herrero-Cervera A, Vinué Á, Real JT, Ascaso JF, Burks DJ, González-Navarro H (2019) Type 1 diabetic mellitus patients with increased atherosclerosis risk display decreased CDKN2A/2B/2BAS gene expression in leukocytes. J Transl Med 17(1):222
Rastad H, Parsaeian M, Shirzad N, Mansournia MA, Yazdani K (2019) Diabetes mellitus and cancer incidence: the atherosclerosis risk in communities (ARIC) cohort study. J Diabetes Metab Disord 18(1):65–72
Katakami N (2018) Mechanism of development of atherosclerosis and cardiovascular disease in diabetes mellitus. J Atheroscler Thromb 25(1):27–39
Dworacka M, Krzyżagórska E, Wesołowska A, Zharmakhanova G, Iskakova S, Dworacki G (2014) Circulating monocyte chemotactic protein 1 (MCP-1), vascular cell adhesion molecule 1 (VCAM-1) and angiogenin in type 2 diabetic patients treated with statins in low doses. Eur J Pharmacol 740:474–479
Arrigoni E, Del Re M, Fidilio L, Fogli S, Danesi R, Di Paolo A (2019) Pharmacogenetic foundations of therapeutic efficacy and adverse events of statins. Expert Opin Drug Metab Toxicol 15(4):313–328
Wan Z, Wang G, Li T, Xu B, Pei Q, Peng Y, Sun H, Cheng L, Zeng Y, Yang G, Zhu YS (2015) Marked alteration of Rosuvastatin pharmacokinetics in healthy Chinese with ABCG2 34G>a and 421C>a homozygote or compound heterozygote. J Pharmacol Exp Ther 354(3):310–315
Safar Z, Kis E, Erdo F, Zolnerciks JK, Krajcsi P (2019) ABCG2/BCRP: variants, transporter interaction profile of substrates and inhibitors. Expert Opin Drug Metab Toxicol 15(4):313–328
Bai X, Zhang B, Wang P, Wang GL, Li JL, Wen DS, Long XZ, Sun HS, Liu YB, Huang M, Zhong SL (2019) Effects of SLCO1B1 and GATM gene variants on rosuvastatin-induced myopathy are unrelated to high plasma exposure of rosuvastatin and its metabolites. Acta Pharmacol Sin 40(4):492–499
Gelissen IC, McLachlan AJ (2014) The pharmacogenomics of statins. Pharmacol Res 88:99–106
Shitara Y, Maeda K, Ikejiri K, Yoshida K, Horie T, Sugiyama Y (2013) Clinical significance of organic anion transporting polypeptides (OATPs) in drug disposition: their roles in hepatic clearance and intestinal absorption. Biopharm Drug Dispos 34(1):45–78
Lee HK, Hu M, Lui S, Ho CS, Wong CK, Tomlinson B (2013) Effects of polymorphisms in ABCG2, SLCO1B1, SLC10A1 and CYP2C9/19 on plasma concentrations of rosuvastatin and lipid response in Chinese patients. Pharmacogenomics. 14(11):1283–1294
Xiang Q, Chen SQ, Ma LY, Hu K, Zhang Z, Mu GY, Xie QF, Zhang XD, Cui YM (2018) Association between SLCO1B1 T521C polymorphism and risk of statin-induced myopathy: a meta-analysis. Pharmacogenomics J 18(6):721–729
Barkas F, Elisaf M, Liberopoulos E, Liamis G, Ntzani EE, Rizos EC (2019) Atherogenic dyslipidemia increases the risk of incident diabetes in statin-treated patients with impaired fasting glucose or obesity. J Cardiol. https://doi.org/10.1016/j.jjcc.2019.02.009
Kurihara O, Thondapu V, Kim HO, Russo M, Sugiyama T, Yamamoto E, Fracassi F, Minami Y, Wang Z, Lee H, Yonetsu T, Jang IK (2019) Comparison of vascular response to statin therapy in patients with versus without diabetes mellitus. Am J Cardiol 123(10):1559–1564
Reddy S, Amutha A, Rajalakshmi R, Bhaskaran R, Monickaraj F, Rangasamy S, Anjana RM, Abhijit S, Gokulakrishnan K, Das A, Mohan V, Balasubramanyam M (2017) Association of increased levels of MCP-1 and cathepsin-D in young onset type 2 diabetes patients (T2DM-Y) with severity of diabetic retinopathy. J Diabetes Complicat 31(5):804–809
Bahrami A, Parsamanesh N, Atkin SL, Banach M, Sahebkar A (2018) Effect of statins on toll-like receptors: a new insight to pleiotropic effects. Pharmacol Res 135:230–238
Taleb S (2016) Inflammation in atherosclerosis. Arch Cardiovasc Dis 109(12):708–715
Tousoulis D, Oikonomou E, Economou EK, Crea F, Kaski JC (2016) Inflammatory cytokines in atherosclerosis: current therapeutic approaches. Eur Heart J 37(22):1723–1732
Funding
This study was supported by the National Natural Science Foundation of China (Grant no. 81503339).
Author information
Authors and Affiliations
Contributions
DZ: analyzed data and wrote the manuscript. YMD, XXW, WYX, WWD and WQC: contributed to the development, interpretation of results. XLZ and PML revision of the manuscript.
Corresponding author
Ethics declarations
The protocol for study was approved by the Bioethical Committee of China-Japan Friendship Hospital and all the participants gave informed consent.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 16 kb)
Rights and permissions
About this article
Cite this article
Zhang, D., Ding, Y., Wang, X. et al. Effects of ABCG2 and SLCO1B1 gene variants on inflammation markers in patients with hypercholesterolemia and diabetes mellitus treated with rosuvastatin. Eur J Clin Pharmacol 76, 939–946 (2020). https://doi.org/10.1007/s00228-020-02882-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-020-02882-4