Abstract
Purpose
The aim of the present paper is to study which prescription pain medications are most commonly dispensed to people with chronic headache (CH), particularly those with medication-overuse headache (MOH).
Methods
This cross-sectional study analysed prescription pain medications dispensed within 1 year to 68,518 respondents of a national health survey. Participants with headache ≥15 days per month for 3 months were classified as having CH. Those with CH and over-the-counter analgesic use ≥15 days per month or purchase of ≥20 or ≥30 defined daily doses (DDDs) of prescription pain medication per month (depending on the drug) were classified as having MOH. Associations between CH and other chronic pain conditions were analysed by logistic regression.
Results
Among those with CH (adjusted prevalence 3.3 %, CI 3.2–3.5 %), pain medications most commonly dispensed were paracetamol, tramadol, ibuprofen and codeine. CH was associated with osteoarthritis, back pain, and rheumatoid arthritis. Among those with MOH, 32.4 % were dispensed an opioid at least once within 1 year. Only 5.1 % of people with CH were dispensed triptans.
Conclusions
High prevalence of opioid use among people with CH may be due to inappropriate headache treatment or development of MOH among those treated for other pain conditions. While there were cases of triptan overuse, triptans remain underutilized among those with CH, suggesting that migraine may be under-recognized and inappropriately treated, leading to overuse of other medications. Education of physicians on appropriate headache management is essential for MOH prevention. There is a need to increase universal awareness about MOH as an adverse effect of long-term analgesic use.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The benefits of frequent analgesic use must always be weighed against risks [1]. An often unrecognized adverse effect of analgesic use is medication-overuse headache (MOH) [2–4]. In MOH, headache is paradoxically caused by medication that is supposed to relieve it and inadequate relief is addressed by further escalation in pain medication use. MOH prevalence is 1.0–2.0 % globally, with several countries reporting higher numbers and is estimated as 1.8 % in Denmark [5]. MOH is associated with ill health and disability [4–7] and is among the most costly neurologic diseases [8]. These individual and societal costs are unnecessary because MOH is preventable and treatable [3, 4, 7].
MOH is described in the International Classification of Headache Disorders (ICHD-3 beta, Table 1) [9]. Not everyone who frequently takes analgesics will develop MOH. Those with a predisposition to headache, particularly migraine, appear to be at highest risk [2, 4].
Most MOH cases are attributed to use of simple or combination analgesics [10]. MOH due to triptans, ergotamines, or opioids is less common but more difficult to treat [4, 11]. Reliable data on pain medication use is difficult to elicit in population-based studies because of limitations in recall. With regard to prescription pain medications, a large-scale study in Denmark showed that agreement between self-reported data and prescription records was lowest for opioids (kappa 0.49), other analgesics (kappa 0.46), and antimigraine preparations (kappa 0.39) [12]. This is likely because pain medications are used as needed, and not as regularly as drugs for the cardiovascular system or diabetes, for example.
Prescription registries are useful tools in identifying MOH cases because these are not subject to recall bias. These registries have been used to study MOH incidence in Norway and [13] prevalence in Denmark [5].
The aims of the present paper are to study which prescription pain medications are most commonly dispensed to people with chronic headache (CH) using data from a national prescription registry and to examine the average amount of prescription pain medications dispensed to those with MOH, those with CH but no medication overuse (CHnoO), and the general population without CH.
We hypothesized that certain prescription pain medications were more frequently dispensed to people with MOH than those with CHnoO or the general population.
Methods
This cross-sectional population-based study is based on data gathered from the Danish National Health Survey (DNHS) and the Danish National Prescription Registry (DNPR) which were linked at the individual level.
The DNHS used a self-administered questionnaire to gather data on chronic illness and health-related behaviour from a randomly selected, representative sample of the national population aged ≥16 years. Sampling methods have been previously described [5, 14]. A total of 129,150 individuals were invited to participate.
Participants with headache occurring ≥15 days per month in the last 3 months were classified as having CH. This case definition corresponds to ICHD-3 beta criterion A for chronic migraine and chronic tension-type headache [9]. There were no other questions on headache characteristics; therefore, specific headache diagnoses could not be made.
Participants with CH who self-reported overuse of over-the-counter (OTC) pain medication or had registry evidence of overuse of prescription pain medications were classified as having MOH.
OTC analgesic overuse was defined as use ≥15 days per month in the last 3 months. The type of OTC drug purchased was not specified in the questionnaire. Triptans are not available OTC in Denmark.
Prescription pain medication overuse was assessed by reviewing participants’ DNPR records [15] on the following Anatomical Therapeutic Chemical (ATC) groups [16] for year 2009: M01A (anti-inflammatory and antirheumatic products), N02A (opioids), N02B (other analgesics and antipyretics), and N02C (antimigraine preparations). Codeine in combination with paracetamol or aspirin is classified as N02A and N02B, respectively. Plain codeine preparations are classified in R05D (cough suppressants).
For those with chronic headache, defined daily doses (DDDs) of drugs of interest were calculated as an average per month spanning at least 3 months to approximate the diagnostic criteria of overuse for more than 3 months (Table 1). One DDD is the typical dose required by an adult per day for a drug’s main indication [16]. To increase the likelihood that medication use was concurrent with self-report of chronic headache during the survey period (January to April 2010), the last purchase should have been on 1 October 2009 or later [5].
The cutoff for overuse was ≥30 DDDs per month for simple analgesics or ≥20 DDDs per month for opioids, triptans, combination preparations, or combinations of medications from different classes.
Respondents with CH who did not meet the criteria for OTC or prescription drug overuse were classified as having CH without medication overuse (CHnoO).
Prevalences of CH, MOH, and several chronic pain conditions (osteoarthritis, discus prolapse/back problem, rheumatoid arthritis, osteoporosis, and cancer) were calculated and adjusted for stratified sampling and non-response. Weights were calculated by Statistics Denmark based on register information [5, 14].
Associations between CH and chronic pain conditions were analysed separately for the sexes using logistic regression adjusted for age, civil status, ethnicity, income, work status, and highest educational attainment. The prevalence of CH varies significantly across categories of these sociodemographic variables [5], and therefore, these were included as possible confounders in the regression analyses.
For medications with at least 100 prescriptions dispensed to people with CH, DDDs per person (1 year) were calculated as an average for the headache groups (CHnoO and MOH). For triptans, medians and ranges were also computed, since there were relatively fewer users of this drug class. Total drug purchases were summarized as DDDs per 1000 inhabitants per day.
National drug utilization data for 2009 (publicly available in medstat.dk) were analysed for the four most commonly dispensed pain medications to explore the possible effect of non-response to the survey. Available data for those aged ≥15 years were summarized as DDDs per 1000 inhabitants per day and compared to summary data from the sample (aged ≥16 years).
SAS software (version 9.3, SAS Institute Inc., Cary, NC, USA) was used for data management and analysis. Microsoft Excel 2010 was used for some supplementary DDD analyses.
To protect the anonymity of respondents, Statistics Denmark encrypted 10-digit codes used to select respondents in the Civil Registration System [17] and replaced these with 12-digit personal identification numbers used to link data from the DNHS and DNPR. Authors MLW and CG had access to the data for analysis purposes. Informed consent for use of data was given by respondents upon return of the questionnaire.
Results
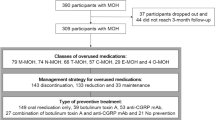
There were 68,518 respondents (53.1 % response) and 2087 were identified as having CH (Table 2). The adjusted prevalence of CH was 3.3 % (CI 3.2–3.5 %) and for MOH 1.8 % (CI 1.7–1.9 %). Both CH and MOH were more prevalent among women (ratio of 1.9:1 for MOH). About half of men and half of women with CH overused pain medications, with no significant difference between the sexes. MOH is most prevalent among the middle aged. Among all the MOH cases identified, 96.2 % reported overuse of OTC analgesics. Those who overused prescribed medications exclusively were aged 35 years or older (Table 2). Detailed sociodemographic data have been previously reported [5].
The prevalences of several chronic pain conditions are summarized in Table 3. Osteoarthritis, back pain, rheumatoid arthritis, and osteoporosis (but not cancer) was significantly more common among people with CH than those without. Associations between CH and osteoarthritis, back pain, and rheumatoid arthritis were strong in both sexes.
Half (49.2 %) of those with CH purchased prescription pain medications at least once during the year (Fig. 1).
All drug codes are based on the Anatomical Therapeutic Chemical (ATC) classification system. DNHS Danish National Health Survey, NSAIDs non-steroidal anti-inflammatory drugs, Rx number of dispensed prescriptions. a Among 68,518 respondents, 2087 reported chronic headache. b There were in total 660,691 prescriptions dispensed to all respondents, of which 37,687 (5.8 %) were to people with chronic headache. c The sum total of respondents below is greater than 1026 since some respondents were dispensed more than one type of medication. d The combined total for opioid purchases (N02A plus R05DA04) is Rx = 3052 and n = 474 respondents
Compared to the CHnoO group, the MOH group was more likely to purchase opioids (32.4 vs. 11.4 %), NSAIDs (36.6 vs. 21.0 %), and other analgesics (26.9 vs. 6.8 %; Table 4).
Among people with CH, 5.1 % purchased triptans, with only a small absolute difference in proportions between the MOH and CHnoO groups (6.2 vs. 3.9 %; Table 5). The four pain medications most commonly prescribed to people with CH were paracetamol, tramadol, ibuprofen, and codeine (Table 4). The MOH and CHnoO groups differed markedly in their purchases of these four drugs. For example, tramadol was purchased by one in six people with MOH, and by one in 21 people with CHnoO. People with MOH purchased larger amounts on average compared to people with CHnoO. The amount of pain medications dispensed to those with CHnoO paralleled that of the general population without CH, particularly for paracetamol, tramadol, ibuprofen, and codeine (Table 4). However, for these four drugs, amounts dispensed to the MOH group were 11, 18, 4, and 8 times higher, respectively, than amounts dispensed to those with CHnoO. For example, the amount of codeine purchased by those without CH and those with CHnoO was 3.38 DDDs per 1000 inhabitants per day. The corresponding amount was 28.65 DDDs per 1000 inhabitants per day for the MOH group.
Our sample’s drug utilization data were consistent with, though slightly lower than, the national data. Utilization of plain codeine for the entire sample was 3.79 DDDs per 1000 people per day. The equivalent for the national population was 3.2 DDDs per 1000 inhabitants per day and an estimated 3.88 DDDs per 1000 inhabitants per day for those ≥15 years. Comparisons for the other three drugs were as follows for the sample (aged ≥16 years) vs. national data (for those aged ≥15 years): paracetamol, 25.72 vs. 33.09; tramadol, 6.89 vs. 9.22; and ibuprofen, 17.15 vs. 19.22 DDDs per 1000 inhabitants per day.
Discussion
Use of prescription drug registries for estimating total prevalence or incidence of MOH has so far only been attempted in Norway [13] and Denmark [5]. There have been comprehensive prescription registry studies on triptan overuse since the late 1990s [18, 19], but these did not correlate medication purchases with headache symptomatology and did not consider the concurrent use of other pain medications, particularly OTC analgesics.
Among people with CH, about half overused analgesics purchased without prescription and in addition purchased larger amounts of prescribed pain medications. The other half purchased much less prescribed pain medications and in amounts that paralleled those of the general population. It is possible that a subset of people with CH took pain medications more frequently because of comorbid chronic pain. However, it is important to consider that frequent analgesic use for other pains could cause MOH.
Opioids for headache?
One in five people with CH—and one in three with MOH—were dispensed an opioid at least once during the year. This is a high proportion considering that opioids are not included in national treatment guidelines for headache [20]. Opioids are not recommended for CH because few improve in terms of function or sustained pain reduction, and in the long run, the risk of dependence outweighs benefits [21, 22]. There were no significant differences in the prevalence of self-reported cancer in the CH and no CH groups, suggesting that opioids were likely being taken for non-cancer pain.
In this cross-sectional study, we cannot determine which came first: headache, other chronic pain, or opioid use. A US-based study described that 17.7 % of people with CH used opioids for headache or any other pain [23]. Longitudinal studies have demonstrated the link between opioid use and headache chronification [24, 25].
It is unclear why the number of prescriptions for tramadol was second only to paracetamol. There is weak evidence for tramadol efficacy in migraine, and even in emergency settings, risks may outweigh benefits [26, 27]. Tramadol is not indicated for tension-type headache: limited data show declining efficacy over time and the common occurrence of adverse events [28].
Plain codeine was not initially included in an earlier analysis of MOH prevalence because of its primary indication as a cough suppressant [5]. Studies on prescription patterns of codeine for non-malignant pain both include [29] and exclude [30] plain codeine. The current analysis shows that 10 % of people with MOH purchased plain codeine. None of them overused plain codeine exclusively, but rather used this in combination with other medications. Including plain codeine as a drug of interest yielded additional cases of MOH but did not change the overall MOH prevalence estimate of 1.8 %. Excluding this drug would have underestimated opioid exposure. The large difference in the average DDDs of codeine purchased by the MOH and CHnoO groups is unlikely to be due simply to a higher prevalence of chronic cough in the MOH group.
Triptans and ergotamines
There were 1277 persons from the study population who purchased a triptan at least once. Utilization can be estimated as 18.6 per 1000 people, a threefold increase from 6.6 per 1000 in 1994 [18]. Coverage of migraineurs can be estimated as 15.2 % assuming a 1-year migraine prevalence of 12.3 % [31]. This level of triptan use is within the range (3 to 19 %) reported by other countries [19, 32, 33]. However, the proportion using triptans among those with CH is on the low end at 5.1 %.
There were cases of overuse among the triptan users. The MOH group showed a wide range of DDDs per person for triptans. While there were cases of exclusive triptan overuse, for the most part, people with MOH who used triptans were classified as having MOH due to overuse of other pain medications.
The proportion of triptan users among those with MOH was very low considering that migraineurs account for 37.0 % of MOH cases in Norway [13] and 58.5 % of cases in Sweden [10]. Population-based studies report co-occurrence of migraine in 50–70 %, while co-occurrence is 80–100 % in tertiary headache centres [4].
It is possible that migraine was under-recognized and under-treated in our study population. The underutilization of an effective migraine treatment might in part explain the overuse of other pain medications. Migraineurs who discontinue triptans tend to shift to using OTC analgesics or opioids during migraine attacks [34]. A recent longitudinal study found that poor treatment efficacy carries a twofold to threefold increased risk of new-onset chronic migraine among those with episodic migraine. Those who used NSAIDs and simple analgesics were less likely to have high treatment efficacy compared to those who used triptans [35].
Ergotamine use has declined in Europe because of changes in migraine treatment guidelines [36]. There were no cases of ergotamine overuse identified in this study.
Simple and combination analgesics
Paracetamol and ibuprofen ranked highest in terms of amount dispensed. These medications do not necessarily present the highest risk for developing MOH; the results may simply reflect how these are the most commonly purchased analgesics. Their use appeared to be within the therapeutic range based on the amount of medications dispensed as well as intervals between purchases.
Nonetheless, there were differences in the average amounts of paracetamol and ibuprofen dispensed to the MOH and CHnoO groups. These medications are also available without prescription, and differences in actual intake could be even higher.
Chronic headache and comorbid pain
Our findings on the association between CH and other chronic pain are consistent with previous studies. Hagen et al. showed that chronic musculoskeletal or gastrointestinal complaints at baseline increased the risk of MOH and CHnoO [10]. Bahra et al. found that CH could develop de novo among patients treated for arthritis, but only among those predisposed to headache [37]. Yoon et al. found strong associations between CH and back pain [38]. Johnson et al. described how prolonged opioid use for different pain conditions could cause opioid-induced hyperalgesia which might have pathophysiological features common to MOH [39].
Methodological considerations
We cannot interpret the direction of causality. Medication intake could be a consequence or cause of worsening headache [24]. It is not possible to determine a causal relationship between MOH and specific prescription medications.
The 59.5 % nationwide participation rate was expected for the DNHS. Non-response trends have been previously analysed and found to be lowest for young men, those with an ethnic background other than Danish, and also in specific neighbourhoods [14]. Prevalence proportions were adjusted for non-response and were generally slightly higher than crude prevalences [5]. A non-responder analysis was not done with respect to headache. This was performed in Norway in a study that showed small differences in headache reporting among respondents and non-respondents [39].
Drug utilization was not calculated for non-respondents. Data on paracetamol, tramadol, ibuprofen, and codeine from our sample were slightly lower than the national data, suggesting that non-response might have contributed to an underestimation of total drug utilization.
It was beyond the scope of the study to validate chronic pain self-reports with patient records.
Large differences in access to health care according to socioeconomic position were not expected because health services are largely free in Denmark. Low income could certainly affect medication purchase patterns but not necessarily in terms of less access to medication. In this population, low income groups had a significantly higher prevalence of MOH [5].
Avenues for future research
Which cutoff level is indicative of overuse? Cutoff levels should consider likely differences between amounts purchased and amounts actually consumed. Hagen et al. [13] used the same cutoff level of ≥20 DDDs per month for triptans and opioids. Our cutoff level of ≥30 DDDs per month for simple analgesics is equivalent to daily intake of the full dose of these medications and is lower than the level used by Hagen et al. (≥70 DDDs per month). Studies to assess the sensitivity and specificity of these levels have yet to be performed.
MOH can arise in susceptible individuals even if the main indication for pain treatment is not headache [11, 13, 37–39]. There is a need for studies on headache comorbidity. Studies that analyse comorbidity among non-communicable diseases should include CH.
Conclusions and recommendations
The four prescription pain medications most commonly dispensed to people with CH were paracetamol, tramadol, ibuprofen, and codeine. These were likely taken not just for CH but also other chronic pain conditions prevalent among those with CH. About half of those with CH overused pain medications purchased with or without prescription and were classified as having MOH. There were cases of triptan overuse; however, the proportion of triptan users was low relative to the expected prevalence of migraine among those with CH or MOH. This suggests that migraine may be under-recognized and inappropriately treated, which might lead to overuse of other medications. Opioid use among people with CH needs urgent attention since this represents inappropriate opioid use for headache or the development of MOH in people treated with opioids for other pain.
Increasing universal awareness about rational use of analgesics is important for MOH prevention efforts. Physicians must be aware of MOH risk in patients who are prescribed analgesics for any chronic pain. Education of physicians on appropriate headache management is essential for prevention of MOH.
References
Paulose-Ram R, Hirsch R, Dillon C, Losonczy K, Cooper M, Ostchega Y (2003) Prescription and non-prescription analgesic use among the US adult population: results from the third National Health and Nutrition Examination Survey (NHANES III). Pharmacoepidemiol Drug Saf 12:315–326. doi:10.1002/pds.755
Saper JR, Sa Silva AN (2013) Medication overuse headache: history, features, prevention and management strategies. CNS Drugs 27:867–877. doi:10.1007/s40263-013-0081-y
Munksgaard SB, Jensen RH (2014) Medication overuse headache. Headache 54:1251–1257. doi:10.1111/head.12408
Kristoffersen ES, Lundqvist C (2014) Medication-overuse headache: a review. J Pain Res 7:367–368. doi:10.2147/JPR.S46071
Westergaard ML, Glumer C, Hansen EH, Jensen RH (2014) Prevalence of chronic headache with and without medication overuse: associations with socioeconomic position, and physical and mental health status. Pain 155:2005–2013. doi:10.1177/0333102413512033
Lanteri-Minet M, Duru G, Mudge M, Cottrell S (2011) Quality of life impairment, disability and economic burden associated with chronic daily headache, focusing on chronic migraine with or without medication overuse: a systematic review. Cephalalgia 31:837–850. doi:10.1177/0333102411398400
Steiner TJ, Stovner LJ, Katsarava Z, Lainez JM, Lampl C, Lantéri-Minet M, Rastenyte D, de la Torre ER, Tassorelli C, Barré J, Andrée C (2014) The impact of headache in Europe: principal results of the Eurolight project. J Headache Pain 15:31. doi:10.1186/1129-2377-15-31
Russell MB, Lundqvist C (2012) Prevention and management of medication overuse headache. Curr Opin Neurol 25:290–295. doi:10.1097/WCO.0b013e328352c431
Headache Classification Committee of the International Headache Society (2013) The international classification of headache disorders, 3rd edition (beta version). Cephalalgia 33:629–808. doi:10.1177/0333102413485658
Jonsson P, Hedenrud T, Linde M (2011) Epidemiology of medication overuse headache in the general Swedish population. Cephalalgia 31:1015–1022. doi:10.1177/0333102411410082
Da Silva AN, Lake AE III (2014) Clinical aspects of medication overuse headaches. Headache 54:211–217. doi:10.1111/head.12223
Nielsen MW, Søndergaard B, Kjøller M, Hansen EH (2008) Agreement between self-reported data on medicine use and prescription records vary according to method of analysis and therapeutic group. J Clin Epidemiol 61:919–924. doi:10.1016/j.jclinepi.2007.10.021
Hagen K, Lind M, Steiner TJ, Stovner LJ, Zart J-A (2012) Risk factors for medication-overuse headache: an 11-year follow-up study. The Nord-Trøndelag health studies. Pain 153:56–61. doi:10.1016/j.pain.2011.08.018
Christensen AI, Ekholm O, Glümer C, Andreasen AH, Hvidberg MF, Kristensen PL, Larsen FB, Ortiz B, Juel K (2012) The Danish National Health Survey 2010. Study design and respondent characteristics. Scand J Public Health 40:391–397. doi:10.1177/1403494812451412
Kildemoes HW, Sørensen HT, Hallas J (2011) The Danish national prescription registry. Scand J Public Healt 39(Suppl 7):38–41. doi:10.1177/1403494810394717
WHO Collaborating Centre for Drug Statistics Methodology (2011) Use of ATC/DDD, www.whocc.no/use_of_atc_ddd (accessed 11 February 2015)
Pedersen CB (2011) The Danish civil registration system. Scand J Public Health 39(Suppl 7):22–25. doi:10.1177/1403494810387965
Gaist D (1999) Use and overuse of sumatriptan. Pharmacoepidemiological studies based on prescription register and interview data. Cephalalgia 19:735–761
Von Euler M, Keshani S, Baatz K, Wettermark B (2014) Utilization of triptans in Sweden; analyses of over the counter and prescription sales. Pharmacoepidemiol Drug Saf 23:1288–1293. doi:10.1002/pds.3681
20 Bendtsen L, Birk S, Kasch H, Aegidius K, Sørensen PS, Thomsen LL, Poulsen L, Rasmussen MJ, Kruuse C, Jensen R (2012) Danish Headache Society. Reference programme: diagnosis and treatment of headache disorders and facial pain. Danish Headache Society, 2nd Edition. J Headache Pain 13 Suppl 1: S1–29. doi: 10.1007/s10194-011-0402-9
Franklin GM (2014) Opioids for chronic noncancer pain: a position paper of the American Academy of Neurology. Neurology 83:1277–1284. doi:10.1212/WNL.0000000000000839
Marmura MJ, Silberstein SD, Schwedt TJ (2015) The acute treatment of migraine in adults: the american headache society evidence assessment of migraine pharmacotherapies. Headache 55(1):3–20. doi:10.1111/head.12499
Scher AI, Lipton RB, Stewart WF, Bigal M (2010) Patterns of medication use by chronic and episodic headache sufferers in the general population: results from the frequent headache epidemiology study. Cephalalgia 30:321–328. doi:10.1111/j.1468-2982.2009.01913.x
Bigal ME, Lipton RB (2008) Excessive acute migraine medication use and migraine progression. Neurology 71:1821–1828. doi:10.1212/01.wnl.0000335946.53860.1d
Limmroth V, Katsarava Z, Fritsche G, Przywara S, Diener HC (2002) Features of medication overuse headache following overuse of different acute headache drugs. Neurology 59:1011–1014
Orr SL, Aubé M, Becker WJ, Davenport WJ, Dilli E, Dodick D, Giammarco R, Gladstone J, Leroux E, Pim H, Dickinson G, Christie SN (2015) Canadian Headache Society systematic review and recommendations on the treatment of migraine pain in emergency settings. Cephalalgia 35:271–284. doi:10.1177/0333102414535997
Kelley NE, Tepper DE (2012) Rescue therapy for acute migraine, part 3: opioids, NSAIDs, steroids, and post-discharge medications. Headache 52:467–482. doi:10.1111/j.1526-4610.2012.02097.x
Robbins L (2004) Tramadol for tension-type headache. Headache 44(2):192–193
Ekholm O, Kurita GP, Højsted J, Juel K, Sjøgren P (2014) Chronic pain, opioid prescriptions, and mortality in Denmark: a population-based cohort study. Pain 155(12):2486–2490. doi:10.1016/j.pain.2014.07.006
Fredheim OMS, Skurtveit S, Moroz A, Breivik H, Borchgrevink PC (2009) Prescription pattern of codeine for non-malignant pain: a pharmacoepidemiological study from the Norwegian Prescription Database. Acta Anaesthesiol Scand 53:627–633
Le H, Tfelt-Hansen P, Skytthe A, Kyvik KO, Olesen J (2012) Increase in self-reported migraine prevalence in the Danish adult population: a prospective longitudinal population-based study. BMJ Open 2. doi:10.1136/bmjopen-2012-000962
Antonaci F, Dumitrache C, De Cillis I et al (2010) A review of current European treatment guidelines for migraine. J Headache Pain 11:13–19. doi:10.1007/s10194-009-0179-2
Bigal ME, Borucho S, Serrano D, Lipton RB (2009) The acute treatment of episodic and chronic migraine in the USA. Cephalalgia 29:891–897. doi:10.1111/j.1468-2982.2008.01819.x
Wells RE, Markowitz SY, Barton EP, Hentz JG, Kalidas K, Mathew PG, Halker R, Dodick DW, Schwedt TJ (2014) Identifying the factors underlying discontinuation of triptans. Headache 54:278–289. doi:10.1111/head.12198
Lipton RB, Fanning KM, Serrano D, Reed ML, Cady R, Buse DC (2015) Ineffective acute treatment of episodic migraine is associated with new-onset chronic migraine. Neurology 84:688–695. doi:10.1212/WNL.0000000000001256
Tfelt-Hansen PC, Koehler PJ (2008) History of the use of ergotamine and dihydroergotamine in migraine from 1906 onward. Cephalalgia 28:877–886. doi:10.1111/j.1468-2982.2008.01578.x
Bahra A, Walsh M, Menon S, Goadsby PJ (2003) Does chronic headache arise de novo in association with regular use of analgesics? Headache 43:179–190. doi:10.1046/j.1526-4610.2003.03041.x
Yoon MS, Manack A, Schramm S, Fritsche G, Obermann M, Diener HC, Moebus S, Katsarava Z (2013) Chronic migraine and chronic tension-type headache are associated with concomitant low back pain: results of the German Headache Consortium Study. Pain 154(3):484–492. doi:10.1016/j.pain.2012.12.010
Johnson JL, Hutchinson MR, Williams DB, Rolan P (2013) Medication-overuse headache and opioid-induced hyperalgesia: a review of mechanisms, a neuroimmune hypothesis and a novel approach to treatment. Cephalalgia 33(1):52–64. doi:10.1177/0333102412467512
Langhammer A, Krokstad S, Romundstad P, Heggland J, Holmen J (2012) The HUNT study: participation is associated with survival and depends on socioeconomic status, diseases and symptoms. BMC Med Res Methodol 12:143. doi:10.1186/1471-2288-12-143
Acknowledgments
The authors thank the Research Centre for Prevention and Health, especially data manager Carsten Agger, and the team responsible for the Danish National Health Survey; Inger Helt Poulsen for facilitating use of data from Region Zealand; and Statistics Denmark for management of the raw data. Furthermore, we thank everyone who responded to the surveys.
Funding
This study did not receive corporate sponsorship. The Region Zealand Health Profile 2010 and The Capital Region Health Profile 2010 were funded by The Region Zealand and The Capital Region of Denmark. MW received research grants from IMK Almene Fond and the patient organization Migræne og Hovedpineforeningen in connection with this study.
Conflict of interest statement
MW received travel grants from Pfizer, Lundbeck Fund, and Allergan to attend international conferences. RJ has given lectures for Pfizer, Berlin-Chemie, Allergan, Merck, and Autonomic Technologies; is a member of the advisory boards of Autonomic Technologies, Medotech, and Neurocore; and is co-director of Lifting The Burden and EHMTIC. EHH and CG declare that they have no conflict of interest.
Author’s contributions
MLW preformed the drafting and revising the manuscript, study concept, statistical analysis, and interpretation of data; EHH for revising the manuscript, study concept, interpretation of data, and study supervision; CG for revising the manuscript, study design, acquisition and interpretation of data, obtaining funding, study supervision, and coordination; and RHJ for revising the manuscript, study concept and design, interpretation of data, obtaining funding, study supervision, and coordination.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Westergaard, M.L., Hansen, E.H., Glümer, C. et al. Prescription pain medications and chronic headache in Denmark: implications for preventing medication overuse. Eur J Clin Pharmacol 71, 851–860 (2015). https://doi.org/10.1007/s00228-015-1858-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-015-1858-3