Abstract
Purpose
We previously reported that chronic heart failure (CHF) treatments reduce the duration of hospitalisation, even in elderly patients. The present study aimed to determine whether CHF treatment also provides long-term benefits in terms of reduced mortality at 8 years.
Methods
A cohort of 281 patients who were admitted to a French teaching hospital with a main diagnosis of CHF were followed through the health insurance databases for 1 year and through the national mortality database for 8 years.
Results
Diuretics (236 patients, 84 %) and angiotensin-converting enzyme (ACE) inhibitors (193 patients, 69 %) were the most-frequently prescribed medications. The median duration of survival was 46 months. Mortality rates were significantly lower for patients administered beta-blockers (59 %) and statins (56 %) than for patients not exposed to these drugs (82 %, p < 0.001 and 78 %, p = 0.001 respectively). No significant differences in mortality were observed for spironolactone, diuretics or ACE inhibitors. After adjustment, beta-blocker treatment remained associated with a significantly lower risk of mortality (hazard ratio, HR = 0.54 [0.34–0.84]). After adjustment, the use of two or three CHF drugs was associated with longer survival (HR = 0.53 [0.36–0.77]) than the use of zero or one CHF drug. Statins were also associated with longer survival after adjustment (HR = 0.53 [0.31–0.89]). In patients 75 years of age or older (n = 73), only beta-blocker treatment was associated with a significantly lower risk of mortality (HR = 0.31 [0.16–0.63]) in multivariate analysis.
Conclusions
The use of beta-blockers was associated with better survival rates. The use of statins was also associated with better survival at 8 years. Randomised controlled trials are required to confirm these observations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic congestive heart failure (CHF) is among the most common cardiovascular disorders. Despite continued improvements in CHF therapy, mortality over 5 years is currently 60–70 % [1]. CHF can be treated with several different types of drugs, including diuretics, angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor blockers, beta-blockers and digoxin [2]. Several clinical trials have shown that ACE inhibitors, beta-blockers and spironolactone improve symptoms and cardiac function, decrease the frequency of acute heart failure episodes, decrease readmission rates and reduce mortality in CHF patients [3–8].
However, randomised controlled trials (RCTs) have strictly defined protocols (e.g., patient inclusion criteria, particular treatment prescriptions and observance characteristics and limited follow-up), which limit the applicability of their findings to patients seen in routine practice. Although up to half of patients admitted for CHF are older than 75 years, this age group usually comprises only a small minority of patients included in CHF RCTs [3, 9–12]. Additional limitations of RCTs include the use of concomitant medications, are often restricted in the trial setting and relatively short follow-up times. Furthermore, under-utilisation of CHF medications in the overall population of patients with CHF has been reported in several countries [13–15], and particularly for aldosterone antagonists [16]. Older patients are less likely to be prescribed ACE inhibitors together with beta-blockers and this was found to be associated with longer annual duration of hospitalisation in this population [17]. However, the short-term effectiveness of CHF treatment has been confirmed [17, 18].
Against this background, our study aimed to determine the effects of CHF treatment on long-term mortality in real-world conditions of use. We also studied a sub-cohort of patients over 75 years of age to determine whether patient age influenced the effectiveness of CHF treatment.
Materials and methods
Study population and databases
The study design has been described previously [17]. In brief, patients were identified from the national registry of hospitalisations (PMSI) and had been admitted to one of the departments of our teaching hospital (Henri Mondor group, Creteil, France) between 1 January and 31 December 2000. The main diagnosis was CHF, which was reported by the physician at hospital discharge. Selection criteria were:
-
1.
A history of at least one CHF episode, according to the WHO classification, before the index admission to the hospital
-
2.
The patient was living in the Val-de-Marne district, where our hospital is located
-
3.
Discharge home
Criteria 2 and 3 allowed linkage with the regional database of the main French health insurance system (CNAMTS), which covers all medical reimbursement. Some professionals, such as farmers, the self-employed and teachers and their children are covered by different insurance systems and were not included in this study. Vital status (for 8 years after the last inclusion) and cause of death information was collected from the national CepiDc-INSERM database (Epidemiological Centre for Medical Causes of Death), which is the French national death registry.
Data
On admission, the following variables were recorded on a standardised form for each patient by the physician: age, gender, aetiology of CHF, NYHA class, left ventricular ejection fraction, alcohol use, smoking history, comorbidities and drugs prescribed at discharge. History of diabetes or dyslipidaemia was assessed from records of laboratory tests or medication use in the database.
The following data were collected from the CNAMTS database for each patient for the 12 months following hospital discharge: the data from office-based physician follow-ups, such as all prescriptions by general practitioners and/or specialists for CHF treatment and for concomitant cardiovascular treatment, and all hospital readmissions (whether or not related to CHF). This provided us with a reliable source of data, as this database contains all information about the reimbursement claims for CHF drugs (including the date, ATC code of the drug and speciality of the prescribing physician). Claims for reimbursement are filed by the pharmacists who deliver the drugs. Thus, the database information reflects the drugs purchased, but not necessarily those taken by the patient. Claims for reimbursement of in-patient care are filed by the hospital. We collected data on the following CHF drugs: diuretics, ACE inhibitors, beta-blockers, spironolactone, digitalis and nitrates [3]. We also recorded concomitant prescription information, classified according to the ATC codes. Exposure to CHF therapy was defined as follows: prescription of the drug at hospital discharge and at least one purchase during the year following discharge.
The main outcome was vital status at 8 years. Date of death was obtained from the death certificate through the national CepiDc-INSERM mortality database; 117 patients were lost from the study (99 for birth date error, 15 for civil status error and 3 for place of death error between databases).
Statistics
Results are expressed as arithmetic means and standard deviations (SD) for continuous variables, and as percentages for categorical variables. Means were compared using Student’s t test and percentages were compared using the Chi-squared test. For each class of CHF treatment patients exposed to the class were compared with those not exposed. Log-rank statistics were used to compare unadjusted survival rates. The Kaplan–Meier method was used to plot survival curves. Cox proportional hazard analyses were used to estimate mortality risk ratios. A retroactive elimination procedure was used to adjust for age and for any factors that were significant predictors of mortality in the univariate analyses or were significantly different between the treatment groups. In the regression models, age, gender, NYHA class, ischaemic aetiology, ejection fraction, smoking status, coronary heart disease, type 2 diabetes, dyslipidemia, hypertension, cardiac dysrhythmia, chronic obstructive pulmonary disease, renal failure and cardiovascular medication were considered dependent variables of mortality. To evaluate the effects of combined CHF medication use on mortality, we weighted the model on the propensity to receive a combined CHF treatment. Multiple propensity scores [19] can be used to control for selection bias related to the non-random assignment of treatment. For each patient, a propensity score was calculated by logistic regression adjusted for significant potential confounders. The cohort was then subdivided into quintiles based on these propensity scores so that patients with similar probabilities of receiving a combined CHF treatment could be compared. All interactions were tested and adjusted. P values from a multivariate regression model are presented. P values less than 0.05 were considered to indicate statistical significance. All statistical analyses were conducted using the SAS 9.0 (SAS, Chicago, IL, USA) package for Windows.
Results
Baseline data
Among the 654 patients admitted for CHF during the 12-month inclusion period, 281 patients who were covered by the national health insurance and who lived in Val de Marne were included in this study. The mean age of these patients was 73 ± 14 years and 57 % were men (Table 1). The recommended CHF drugs prescribed at hospital discharge and 1 year later are listed in Table 1. Diuretics (84 %, n = 236) and ACE inhibitors (69 %, n = 193) were the most frequently prescribed drugs. In contrast, fewer patients were prescribed beta-blockers (36 %, n = 101), spironolactone (32 %, n = 90) and angiotensin receptor blockers (13 %, n = 37). Eleven percent of the patients (n = 30) were treated with a tri-therapy consisting of spironolactone, ACE inhibitors and beta-blockers and 25 % (n = 69) were treated with ACE inhibitors, beta-blockers and a diuretic other than spironolactone. At 1 year, 23 patients (8 %) remained without CHF treatment. An ischaemic aetiology was reported for 54 % of the 235 patients whose aetiologies were assessed and statins were prescribed for 21 % of all patients (n = 60).
Patients taking a beta-blocker or spironolactone or a statin at discharge (baseline, Table 1) were younger than patients not receiving a beta-blocker or spironolactone or a statin respectively. Patients taking a beta-blocker or diuretics were more frequently prescribed ACE inhibitors. More of the patients prescribed than not prescribed beta-blockers were also prescribed nonspironolactone diuretics or statins. More patients on statin therapy than not on statin therapy were prescribed aspirin, thienopyridines or an oral anticoagulant (70 % vs. 41 %, p < 0.001).
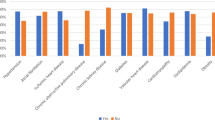
Mortality
Among the patients followed through the national CepiDc-INSERM mortality database during the 8-year follow-up (n = 164), there were 120 deaths (73 %), with only 55 having a cardiac cause. The median duration of survival was 46 months. Mortality rates were significantly lower (Fig. 1) among patients taking beta-blockers than those not taking beta-blockers (59 % vs 82 %, 36 out of 61 patients; p < 0.001) and among patients taking statins than those not taking statins (56 % vs 78 %, 22 out of 39 patients; p < 0.001). No significant difference in mortality was observed between patients treated or not treated with spironolactone (63 %, 34 out of 54 patients vs 78 %, 86 out of 110 patients), diuretics (73 %, 102 out of 140 patients vs 75 %, 18 out of 24 patients) and ACE inhibitors (71 %, 84 out of 118 patients vs 78 %, 36 out of 46 patients; Fig. 1). Whether or not digoxin was used did not significantly affect mortality (83 %, 35 out of 42 patients vs 70 %, 85 out of 122 patients). After stratifying for age and adjusting for chronic obstructive pulmonary disease, beta-blockers, statins, digoxin, dyslipidemia and cardiac dysrhythmia, only beta-blockers and statins remained associated with significantly lower risks of mortality (HR = 0.59 [0.38–0.93] and HR = 0.52 [0.30–0.90] respectively). When propensity scores were used to adjust the Cox model, the risks associated with beta-blockers and statins were similar (HR = 0.54 [0.34–0.84] and HR = 0.53 [0.31–0.89] respectively).
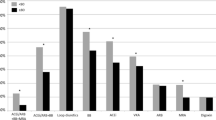
Kaplan–Meier survival curves plotted according to the number of associated CHF therapies revealed differences in survival (Fig. 2). Patients on two or three CHF drugs survived longer than those on other treatments (log rank, p < 0.001). After adjusting for propensity scores, which included age, cardiac history, cardiac dysrhythmia and dyslipidaemia, treatment including two or three CHF drugs, compared with zero or one CHF drug remained a predictor of increased survival (HR = 0.53 [0.36–0.77]). Treatment with three CHF medications was not associated with better survival than treatment with two CHF drugs (HR = 0.82 [0.40–1.71]) after adjustment using adequate propensity scores, which included age, gender, renal failure and smoking. Combined beta-blocker and ACE inhibitor therapies and combined beta-blocker and spironolactone therapies both had similar effects on mortality (HR = 1.06 [0.33–3.42]) after adjustment for propensity scores determined by age and cardiac history. For patients treated with an ACE inhibitor and/or beta-blockers, Kaplan–Meier curves indicated that the survival of those taking spironolactone was no better than that of those taking other diuretics (P = 0.2).
We performed a subgroup analysis of patients 75 years old or older (n = 73). The mortality rate was significantly lower among patients taking beta-blockers (86 %, P = 0.005), statins (82 %, P = 0.007) or other diuretics (94 %, P = 0.01) than among patients not taking these drugs (97 %, 97 % and 100 % respectively; Table 2). There were no significant differences in mortality between patients taking and those not taking spironolactone, an ACE inhibitor, or digoxin. After adjusting for gender, hypertension, chronic obstructive pulmonary disease and co-prescriptions, only beta-blocker treatment was associated with a significantly lower risk of mortality (HR = 0.31 [0.16–0.63]) in this population.
Discussion
Our observational study suggests that CHF treatment was associated with improved survival rates of patients with chronic heart failure disease. Survival was better among patients taking two or three CHF drugs than among patients taking no or only one CHF drug. In particular, we confirmed the beneficial effects of beta-blocker treatment in the long term in a population-based setting after adjustment. Statins were also associated with a decrease in mortality in these patients. Moreover, our results also suggested that beta-blockers were associated with improved survival of older CHF patients.
The lower mortality among the patients treated with two or three CHF drugs may result from a beneficial synergistic effect of beta-blockers and ACE inhibitors and/or spironolactone on survival. The effect of a beta-blocker plus spironolactone combination was not different from that of a beta-blocker plus ACE inhibitor combination.
European guidelines emphasise the importance of using ACE inhibitors in all patients with symptomatic CHF and a LVEF ≤40 %, but ACE inhibitors should only be used in patients with adequate renal function and normal serum potassium concentrations [2]. A review of observational studies revealed that ACE inhibitor use in elderly CHF patients was associated with significantly lower rates of mortality for up to 4 years in one study, but in most studies follow-up was limited to only 1 year [18]. In the short term, most studies report that ACE inhibitor use leads to relative reductions in mortality of between 15 % and 30 % [4, 5, 20]; ACE inhibitor therapies have been associated with a 12 % reduction in adjusted mortality at 1 year and a 7 % reduction in mortality at 3 years [21]. By contrast, no significant difference in all-cause mortality in the long term was observed in an observational study with a mean follow-up of 5 years [22]. In our observational study, we also found that ACE inhibitor use had no significant effect on the survival of patients >75 years old or on the survival of the overall CHF patient population at 8 years. However, our study was limited by its sample size.
Randomised controlled trials (RCTs) and observational studies have shown that beta-blockers reduce mortality in CHF patients by about 30–40 % [6, 7, 23]. The inclusion of younger patients in RCTs limits the strength of the evidence for older CHF patients, but SENIORS (Study of the Effects of Nebivolol Intervention on Outcomes and Rehospitalisation in Seniors with Heart Failure) and a subgroup analysis in MERIT (Metoprolol CR/XL Randomised Intervention Trial) showed that beta-blockers also reduced mortality among elderly patients with heart failure [24, 25]. Here, we report a positive association between beta-blocker use and global mortality at 8 years in both an unselected population and an elderly population.
Renal sodium and water retention are characteristic of congestive heart failure. Thus, diuretic treatment is a standard component of CHF therapy. However, there is no clear evidence that the use of diuretics has beneficial effects on the most important outcomes, notably survival after discharge. However, the Randomized Aldactone Evaluation Study (RALES) indicated a potential benefit of aldosterone in patients with systolic heart failure [8] as patients in the spironolactone group had a 30 % lower risk of death. In contrast, we observed a non-significant reduction of 9 % associated with spironolactone treatment in the long term for CHF patients in real-life conditions.
In a previous study with this population [17], we reported that ACE inhibitors, beta-blockers and spironolactone are underused in patients >75 years old despite being effective CHF treatments: older patients who were treated according to current guidelines spent less time hospitalised during the 1-year follow-up period [17]. Here, we present results confirming the worst mortality among elderly patients who did not receive a recommended CHF treatment, particularly beta-blockers.
The significant benefit of statins on CHF patient survival (a 47 % reduction in mortality) we describe here is consistent with several observational studies showing that statins are associated with reduced mortality of about 35–50 % [26]. In contrast, two prospective randomised studies investigated the efficacy of daily rosuvastatin (10 mg) versus placebo in patients with symptomatic HF, and found no significant differences in mortality between the two groups [27, 28]. The discrepancy between this result and our findings may be a consequence of differences in study design, the drugs used and patient selection criteria [29].
Our study has limitations inherent to its observational design. Many patients were lost after linkage of the different databases. This lost population was not substantially different from that included in terms of drugs used or most of the other patient characteristics except gender (data not shown): most of the lost patients were women. Changes in their marital status or changes in their insurance system affiliations, often related to their husband, may explain many of these losses. How well this particular population represents CHF patients in general is not known, as populations may differ from one area to another. However, the characteristics of our patient population were similar to those found in far larger surveys of CHF patients in Europe [14, 30–32]. Treatments may be influenced by physician habits or local recommendations. The treatments prescribed for our population at hospital discharge were also similar to those reported previously suggesting that the influences of local particularities were small [17]. CHF diagnosis in our study relied solely on the physician’s report, so some patients may have been misclassified. However, several factors limited the risk of misclassification: only patients with at least one prior acute CHF episode were included; most patients met criteria for NYHA class III or IV; and most had markedly decreased ejection fraction values. The ejection fraction is assessed in only a small proportion of patients in routine practice (44 % in our study), and this could be improved. Although we have fewer missing data on ejection fraction (EF) than in other cohorts (63 % and 80 % missing in [33, 34]), this information was not included in our analysis so as to ensure sufficient statistical power. The characteristics that were different in patients with and those without EF data (age, gender, COPD and ischaemic aetiology, all P < 0.05), but analyses were adjusted for age, gender, comorbidities (hypertension and COPD) and other treatments; these factors were similarly used to adjust in other studies. Our results were confirmed with the addition of other potential confounders, recorded in our study, both in the whole population and in patients over 75. We did not record medication doses and therefore were unable to determine whether this factor affected survival. Our assessment of the benefit of cardiovascular drugs was based on treatment defined by drug prescription at the time of hospital discharge and during the year following discharge. This does not necessarily accurately reflect therapy continuation over the 8 years of follow-up. Nevertheless, as previously published, discharge orders have a major influence on the drugs prescribed over the following year [17].
Observational studies of CHF patients allow the effectiveness of treatment in routine practice to be confirmed, in the long term and in populations under-represented or excluded from RCTs [18]. They also provide relevant additional information on the comparative effectiveness of different therapeutic strategies.
References
McMurray JJV, Pfeffer MA (2005) Heart failure. Lancet 365:1877–1889
Dickstein K, Cohen-Solal A, Filippatos G, McMurray JJV, Ponikowski P, Poole-Wilson PA, Strömberg A, van Veldhuisen DJ, Atar D, Hoes AW, Keren A, Mebazaa A, Nieminen M, Priori SG, Swedberg K (2008) ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: the Task Force for the diagnosis and treatment of acute and chronic heart failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM). Eur J Heart Fail 10:933–989
Cohen-Solal A, Desnos M, Delahaye F, Emeriau JP, Hanania G (2000) A national survey of heart failure in French hospitals. The Myocardiopathy and Heart Failure Working Group of the French Society of Cardiology, the National College of General Hospital Cardiologists and the French Geriatrics Society. Eur Heart J 21:763–769
The SOLVD Investigators (1991) Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. The SOLVD Investigators. N Engl J Med 325:293–302
The CONSENSUS Trial Study Group (1987) Effects of enalapril on mortality in severe congestive heart failure. Results of the Cooperative North Scandinavian Enalapril Survival Study (CONSENSUS). The CONSENSUS Trial Study Group. N Engl J Med 316:1429–1435
The CIBIS Investigators and Committees (1999) The Cardiac Insufficiency Bisoprolol Study II (CIBIS-II): a randomised trial. Lancet 353:9–13
The MERIT-HF Study Group (1999) Effect of metoprolol CR/XL in chronic heart failure: Metoprolol CR/XL Randomised Intervention Trial in Congestive Heart Failure (MERIT-HF). Lancet 353:2001–2007
Pitt B, Zannad F, Remme WJ, Cody R, Castaigne A, Perez A, Palensky J, Wittes J (1999) The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized Aldactone Evaluation Study Investigators. N Engl J Med 341:709–717
Cowie MR (1999) Annotated references in epidemiology. Eur J Heart Fail 1:101–107
Cowie MR, Fox KF, Wood DA, Metcalfe C, Thompson SG, Coats AJS, Poole-Wilson PA, Sutton GC (2002) Hospitalization of patients with heart failure: a population-based study. Eur Heart J 23:877–885
Davis RC, Hobbs FDR, Kenkre JE, Roalfe AK, Hare R, Lancashire RJ, Davies MK (2002) Prevalence of left ventricular systolic dysfunction and heart failure in high risk patients: community based epidemiological study. BMJ 325:1156
Gottdiener JS, Arnold AM, Aurigemma GP, Polak JF, Tracy RP, Kitzman DW, Gardin JM, Rutledge JE, Boineau RC (2000) Predictors of congestive heart failure in the elderly: the Cardiovascular Health Study. J Am Coll Cardiol 35:1628–1637
Havranek EP, Masoudi FA, Westfall KA, Wolfe P, Ordin DL, Krumholz HM (2002) Spectrum of heart failure in older patients: results from the National Heart Failure project. Am Heart J 143:412–417
Higashi T, Shekelle PG, Solomon DH, Knight EL, Roth C, Chang JT, Kamberg CJ, MacLean CH, Young RT, Adams J, Reuben DB, Avorn J, Wenger NS (2004) The quality of pharmacologic care for vulnerable older patients. Ann Intern Med 140:714–720
Horwich TB, MacLellan WR, Fonarow GC (2004) Statin therapy is associated with improved survival in ischemic and non-ischemic heart failure. J Am Coll Cardiol 43:642–648
Krantz MJ, Ambardekar AV, Kaltenbach L, Hernandez AF, Heidenreich PA, Fonarow GC (2011) Patterns and predictors of evidence-based medication continuation among hospitalized heart failure patients (from Get With the Guidelines-Heart Failure). Am J Cardiol 107:1818–1823
Maison P, Cunin P, Hemery F, Fric F, Elie N, Del’volgo A, Dubois-Randé JL, Hittinger L, Macquin-Mavier I (2005) Utilisation of medications recommended for chronic heart failure and the relationship with annual hospitalisation duration in patients over 75 years of age. A pharmacoepidemiological study. Eur J Clin Pharmacol 61:445–451
Dobre D, van Veldhuisen DJ, DeJongste MJL, van Sonderen E, Klungel OH, Sanderman R, Ranchor AV, Haaijer-Ruskamp FM (2007) The contribution of observational studies to the knowledge of drug effectiveness in heart failure. Br J Clin Pharmacol 64:406–414
Spreeuwenberg MD, Bartak A, Croon MA, Hagenaars JA, Busschbach JJV, Andrea H, Twisk J, Stijnen T (2010) The multiple propensity score as control for bias in the comparison of more than two treatment arms: an introduction from a case study in mental health. Med Care 48:166–174
Packer M, Poole-Wilson PA, Armstrong PW, Cleland JG, Horowitz JD, Massie BM, Rydén L, Thygesen K, Uretsky BF (1999) Comparative effects of low and high doses of the angiotensin-converting enzyme inhibitor, lisinopril, on morbidity and mortality in chronic heart failure. ATLAS Study Group. Circulation 100:2312–2318
Shah R, Wang Y, Foody JM (2008) Effect of statins, angiotensin-converting enzyme inhibitors, and beta blockers on survival in patients > or = 65 years of age with heart failure and preserved left ventricular systolic function. Am J Cardiol 101:217–222
Allen LaPointe NM, Zhou Y, Stafford JA, Hernandez AF, Kramer JM, Anstrom KJ (2009) Association between mortality and persistent use of beta blockers and angiotensin-converting enzyme inhibitors in patients with left ventricular systolic dysfunction and coronary artery disease. Am J Cardiol 103:1518–1524
Packer M, Bristow MR, Cohn JN, Colucci WS, Fowler MB, Gilbert EM, Shusterman NH (1996) The effect of carvedilol on morbidity and mortality in patients with chronic heart failure. U.S. Carvedilol Heart Failure Study Group. N Engl J Med 334:1349–1355
Deedwania PC, Gottlieb S, Ghali JK, Waagstein F, Wikstrand JCM (2004) Efficacy, safety and tolerability of beta-adrenergic blockade with metoprolol CR/XL in elderly patients with heart failure. Eur Heart J 25:1300–1309
Flather MD, Shibata MC, Coats AJS, Van Veldhuisen DJ, Parkhomenko A, Borbola J, Cohen-Solal A, Dumitrascu D, Ferrari R, Lechat P, Soler-Soler J, Tavazzi L, Spinarova L, Toman J, Böhm M, Anker SD, Thompson SG, Poole-Wilson PA (2005) Randomized trial to determine the effect of nebivolol on mortality and cardiovascular hospital admission in elderly patients with heart failure (SENIORS). Eur Heart J 26:215–225
Van der Harst P, Böhm M, van Gilst WH, van Veldhuisen DJ (2008) The case for statin therapy in chronic heart failure. Clin Res Cardiol 97:139–146
Kjekshus J, Apetrei E, Barrios V, Böhm M, Cleland JGF, Cornel JH, Dunselman P, Fonseca C, Goudev A, Grande P, Gullestad L, Hjalmarson A, Hradec J, Jánosi A, Kamenský G, Komajda M, Korewicki J, Kuusi T, Mach F, Mareev V, McMurray JJV, Ranjith N, Schaufelberger M, Vanhaecke J, van Veldhuisen DJ, Waagstein F, Wedel H, Wikstrand J (2007) Rosuvastatin in older patients with systolic heart failure. N Engl J Med 357:2248–2261
Tavazzi L, Maggioni AP, Marchioli R, Barlera S, Franzosi MG, Latini R, Lucci D, Nicolosi GL, Porcu M, Tognoni G (2008) Effect of rosuvastatin in patients with chronic heart failure (the GISSI-HF trial): a randomised, double-blind, placebo-controlled trial. Lancet 372:1231–1239
Tang WHW, Francis GS (2010) Statin treatment for patients with heart failure. Nat Rev Cardiol 7:249–255
Hunt SA, Baker DW, Chin MH, Cinquegrani MP, Feldman AM, Francis GS, Ganiats TG, Goldstein S, Gregoratos G, Jessup ML, Noble RJ, Packer M, Silver MA, Stevenson LW, Gibbons RJ, Antman EM, Alpert JS, Faxon DP, Fuster V, Gregoratos G, Jacobs AK, Hiratzka LF, Russell RO, Smith SC Jr (2001) ACC/AHA Guidelines for the Evaluation and Management of Chronic Heart Failure in the Adult: Executive Summary A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1995 Guidelines for the Evaluation and Management of Heart Failure): Developed in Collaboration With the International Society for Heart and Lung Transplantation; Endorsed by the Heart Failure Society of America. Circulation 104:2996–3007
Johnson D, Jin Y, Quan H, Cujec B (2003) Beta-blockers and angiotensin-converting enzyme inhibitors/receptor blockers prescriptions after hospital discharge for heart failure are associated with decreased mortality in Alberta, Canada. J Am Coll Cardiol 42:1438–1445
Nicol ED, Fittall B, Roughton M, Cleland JGF, Dargie H, Cowie MR (2008) NHS heart failure survey: a survey of acute heart failure admissions in England, Wales and Northern Ireland. Heart 94:172–177
Saczynski JS, Darling CE, Spencer FA, Lessard D, Gore JM, Goldberg RJ (2009) Clinical features, treatment practices, and hospital and long-term outcomes of older patients hospitalized with decompensated heart failure: The Worcester Heart Failure Study. J Am Geriatr Soc 57:1587–1594
Teng T-HK, Hung J, Finn J (2010) The effect of evidence-based medication use on long-term survival in patients hospitalised for heart failure in Western Australia. Med J Aust 192:306–310
Acknowledgements
We thank F. Fric and P. Cunin for their help in starting this study.
Conflict of interest
The authors declare that they have no conflict of interest
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Maison, P., Desamericq, G., Hemery, F. et al. Relationship between recommended chronic heart failure treatments and mortality over 8 years in real-world conditions: a pharmacoepidemiological study. Eur J Clin Pharmacol 69, 901–908 (2013). https://doi.org/10.1007/s00228-012-1400-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-012-1400-9