Abstract
Objective
The substantial weight loss in Parkinson’s patients may be related to direct influences of levodopa treatment on fat mobilization/oxidation. We assessed systemic and local metabolic responses to levodopa/benserazide in patients with idiopathic Parkinson’s disease.
Methods
We studied 10 Parkinson’s disease patients and examined adipose tissue and skeletal muscle metabolism directly with microdialysis. We monitored dialysate concentrations of ethanol, glucose, lactate, pyruvate, and glycerol to assess tissue blood flow and metabolism before and after levodopa/benserazide intake. We also conducted in vitro studies on adipocytes from healthy women.
Results
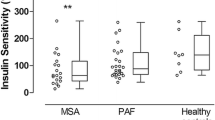
Levodopa/benserazide increased serum levodopa, 3,4-dihydroxyphenylacetic acid (DOPAC), and norepinephrine (P < 0.01). Serum adipose tissue and skeletal muscle glycerol did not change or decreased. Adipose tissue glycerol was inversely correlated with serum levodopa concentrations (P < 0.05). In isolated adipocytes, levodopa attenuated isoproterenol-induced glycerol release (P < 0.05).
Conclusion
Levodopa/benserazide elicits pronounced metabolic changes in both adipose tissue and skeletal muscle with a switch from lipid to carbohydrate metabolism. In adipose tissue, levodopa/benserazide failed to activate lipolysis. Therefore, we suggest that levodopa/benserazide does not induce fat wasting through direct and acute influences on adipose tissue metabolism.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Weight loss due to body-fat wasting is a poorly understood phenomenon in Parkinson’s disease patients. Whether or not therapy contributes to wasting is unknown [1–3]. Weight loss cannot be solely attributed to severity of motor symptoms [3–7]. In contrast to patients undergoing drug therapy, Parkinson’s disease patients who are treated with deep brain electrical stimulation often experience substantial weight gain [8]. The observation challenges the concept that weight loss in drug-treated patients is explained by augmented energy expenditure through improved motor function [3, 4]. Instead, Parkinson’s medications may directly affect adipose tissue mobilization [4]. Levodopa in combination with peripheral aromatic l-amino acid decarboxylase inhibitors is still the most common and effective treatment [9]. In the absence of a decarboxylase inhibitor, levodopa increases circulating free fatty acid concentrations [10, 11]. However, the observation is of limited clinical significance because levodopa is usually prescribed in combination with a decarboxylase inhibitor.
Levodopa and its metabolites accumulate in adipose tissue after levodopa/carbidopa intake [12] where they might elicit metabolic responses locally through interaction with amine oxidases. Monoaminoxidases (MAO A and B) and semicarbazide-sensitive amine oxidase (SSAO) are highly expressed in human adipose tissue [13, 14]. These enzymes produce superoxide during amine degradation, which in turn inhibits lipolysis in human adipocytes [14–16]. Yet, direct influences of levodopa on adipose tissue metabolism have not been studied. We assessed systemic and local metabolic responses to levodopa/benserazide in patients with idiopathic Parkinson’s disease. We applied in-situ microdialysis to study both subcutaneous adipose tissue and skeletal muscle metabolism [17, 18]. Furthermore, we followed changes in lipolysis with direct application of levodopa and levodopa metabolites to isolated human adipocytes.
Methods
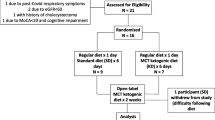
Patients and study design
We studied 10 patients (58–75 years, BMI 18–28 kg/m2) with idiopathic Parkinson syndrome (5 men and 5 women; duration of disease upon diagnosis: 3–13 years), who were stage 2 according to the Hoehn-Yahr rating scale in the on-state [19]. All patients had been on dopamine agonists, including 9 on levodopa/benserazide or levodopa/carbidopa, and 2 on NMDA or COMT inhibitor treatment. Patients were recruited from the Department of Neurology, Charité Campus Virchow, Berlin. All studies were approved by the institutional review board. We obtained written informed consent before study entry. Diagnosis was based on clinical symptoms according to the criteria of the UK Parkinson’s Disease Brain Bank and on an improvement of motor symptoms >30% following exposure to dopaminergic drugs [20].
Forty-eight hours before the experiment, volunteers were asked to abstain from smoking, alcohol ingestion, caffeine-containing beverages, and exercise. All vasoactive medications, including levodopa, were discontinued at least five half-lives before the study. We were concerned that some patients may not tolerate levodopa withdrawal. Therefore, patients were advised that they could take one or two tablets of soluble levodopa preparation as rescue medication. However, all patients tolerated levodopa withdrawal well. The experiment took place after an overnight fast in the morning in a quiet room. After a 60-min resting phase, patients ingested 200 mg levodopa/50 mg benserazide (Madopar, Hoffmann-La Roche, Basel, Switzerland). Venous blood and microdialysis samples were collected in 30-min intervals during baseline and over 120 min after levodopa intake.
Microdialysis
After an overnight fast, microdialysis probes were inserted into abdominal subcutaneous adipose tissue at the level of the umbilicus and into skeletal muscle (vastus lateralis muscle) [17, 18, 21]. We started the tissue perfusion with lactate-free Ringer’s solution (E156, Serumwerk Bernburg, Bernburg, Germany) at a flow rate of 2 μl/min. The solution was supplemented with 50 mmol/l ethanol (Alkohol-Konzentrat 95%, B. Braun Melsungen, Melsungen, Germany) for blood-flow determinations. CMA/60 microdialysis catheters and CMA/102 microdialysis pumps (both from CMA Microdialysis, Solna, Sweden) were used. A 60-min period was allowed for tissue recovery and for baseline calibration before levodopa intake.
Analytical methods
Heart rate and blood pressure were determined by standard techniques. Catecholamines were collected in EGTA tubes (Kabevette; Kabe Labortechnik, Nümbrecht-Elsenroth, Germany) and processed immediately in a refrigerated centrifuge. Serum was stored at –80°C until analysis. Serum levodopa, DOPAC (3,4-dihydroxy-phenylacetic acid), dopamine, DHPG, and norepinephrine were assayed by HPLC with electrochemical (amperometric) detection. Serum-free fatty acids were assayed with an enzymatic method (Wako NEFA C-Test; Wako Chemicals, Neuss, Germany). Serum insulin and glucose concentrations were measured by the hexokinase method and by an enzyme immunoassay, respectively (Roche Diagnostics, Boehringer Mannheim, Germany). Serum human growth hormone was assayed using the IMMULITE 2500 Kit (Siemens Medical, Bad Nauheim, Germany). Ethanol concentrations in perfusate (inflow) and dialysate (outflow) were determined with a standard enzymatic assay [17]. Dialysate glucose, lactate, pyruvate, and glycerol as well as serum glycerol and lactate were measured with a CMA/600 analyzer (CMA Microdialysis).
In vitro studies
We isolated human adipocytes from subcutaneous adipose tissue obtained during liposuction on healthy women (20–50 years, BMI 22–35 kg/m2) by collagenase digestion as described previously [22]. Briefly, adipocytes (85,000–170,000 cells/assay) were incubated in vials containing 500 μl Krebs Ringer Hepes buffer (25 mM HEPES, pH 7.4; 120 mM NaCl, 4.8 mM KCl, 1.2 mM KH2PO4, 1.2 mM MgSO4) supplemented with BSA (1%, w/v), glucose (5 mM), and ascorbate (5 μM) to prevent autooxidation [23]. Then adipocytes were incubated for 120 min in the absence (control) and presence of increasing concentrations of levodopa (1, 10, 100 nM, 1 μM); in the absence and presence of isoproterenol (1 μM); and increasing concentrations of the metabolites dopamine (0.1, 1, 10, 100 nM), DOPAC (1, 10, 100 nM, 1 μM), and HVA (homovanillic acid; 0.1, 1, 10, 100 nM) at 37°C under gentle shaking in a water bath. We terminated incubations by putting the vials on ice and measured glycerol concentration in medium with a CMA/600 analyzer. We expressed lipolytic activity as percentage changes in glycerol release.
Calculations and statistical analysis
Changes in blood flow were determined by using the ethanol dilution technique, which is based on Fick’s principle [24]. Accordingly, a decrease in the outflow-to-inflow ratio is equivalent to an increase in blood flow and vice versa. For simplicity, the term “ethanol ratio” is substituted for the term “ethanol outflow-to-inflow ratio.” Changes in glycerol were used to assess changes in lipolysis/lipid mobilization, and changes in glucose, lactate, and pyruvate were used to assess changes in carbohydrate metabolism. All data are expressed as mean ± SEM. Kolmogorov-Smirnov test was applied to test for a normal distribution of the data. Repeated-measures ANOVA followed by Dunnett’s multiple comparison test was used for multiple comparisons. Linear regression analysis was conducted and the Pearson correlation coefficient was determined. A value of P < 0.05 was considered significant.
Results
In vivo studies
Clinical characteristics of subjects are summarized in Table 1. The five men and five women were older and of normal body habitus. None had diabetes mellitus. Blood pressure and heart rate at baseline were 126 ± 6/74 ± 6 mm Hg and 64 ± 1 beats/min, respectively, and did not change with levodopa/benserazide intake.
Venous levodopa increased from 0.06 ± 0.02 μM at baseline to a maximum of 21 ± 4.2 μM 60 min after levodopa/benserazide intake (P < 0.01; Fig. 1a). Venous dopamine concentration was 2.5 ± 2.1 nM at baseline and 3.8 ± 0.9 nM towards the end of the test (n.s.; Fig. 1b). Dihydroxyphenylglycol (DHPG) was 6.83 ± 0.60 and 5.97 ± 0.72 nM after levodopa/benserazide ingestion (n.s.). Within 30 min after levodopa/benserazide intake, venous DOPAC concentration increased to 92 ± 19 from 15 ± 1.6 nM (P < 0.01; Fig. 1c) and remained elevated for the remainder of the experiment. Venous norepinephrine concentration increased to a maximum of 3.06 ± 0.50 from 0.96 ± 0.19 nM at 60 min (P < 0.01; Fig. 1d). Insulin (baseline: 4.4 ± 0.7 μU/ml) and growth hormone concentration (baseline: 2.9 ± 1.2 ng/ml) did not change significantly with levodopa/benserazide.
Within 60 min after levodopa/benserazide intake, venous lactate decreased from 1.26 ± 0.18 mM to a minimum of 0.86 ± 0.11 mM (P < 0.01; Fig. 2a) and remained stable thereafter. Venous glycerol was 55 ± 10 μM at baseline and 41 ± 7 μM 60 min after levodopa/benserazide intake (n.s.; Fig. 2b). Venous free fatty acid (baseline: 499 ± 43 μM) and glucose concentrations (4.9 ± 0.1 mM) did not change.
In subcutaneous adipose tissue, ethanol ratio and dialysate glucose did not change with levodopa/benserazide (Fig. 3a and b). Within 60 min after levodopa/benserazide intake, dialysate glycerol tended to decrease from 57 ± 11 μM at baseline to 51 ± 10 μM after drug intake (n.s.; Fig. 3c). Dialysate lactate increased from 0.40 ± 0.09 mM at baseline to a maximum of 0.61 ± 0.16 mM (P < 0.01; Fig. 3d).
In skeletal muscle, ethanol ratio increased from 0.21 ± 0.03 at baseline to 0.32 ± 0.04 with levodopa/benserazide (P < 0.01; Fig. 4a). Dialysate glucose was 2.1 ± 0.15 mM at baseline and did not change (Fig. 4b). Dialysate glycerol decreased from 46 ± 4 μM at baseline to 37 ± 3 μM 60 min after levodopa/benserazide intake (P < 0.05; Fig. 4c). Dialysate lactate and pyruvate increased moderately with levodopa/benserazide (Fig. 4d and e; P < 0.01). The lactate-to-pyruvate ratio decreased from 49 ± 5 at baseline to 31 ± 2 with levodopa/benserazide (Fig. 4f; P < 0.01).
Sixty minutes after levodopa/benserazide intake, we observed an inverse correlation between serum levodopa concentration and dialysate glycerol in subcutaneous adipose tissue (P < 0.05; Fig. 5a). Dialysate glycerol in skeletal muscle correlated positively with venous glycerol concentration 60 min after levodopa/benserazide intake (P < 0.01; Fig. 5b).
In vitro studies
We tested the effects of levodopa, levodopa + 1 μM isoproterenol, dopamine, and DOPAC on glycerol production in vitro. Baseline glycerol was 45 ± 5 μM per 100 μl of cells per 2 h. Levodopa did not affect basal glycerol release (Fig. 6a). With 1 μM isoproterenol, glycerol release was three times higher than the control level (P < 0.001). Levodopa at 100 nM attenuated isoproterenol-stimulated glycerol release down to 86 ± 2% (P < 0.05; Fig. 6b). With dopamine, glycerol release in adipocytes decreased below baseline values (n.s.; Fig. 6c). Glycerol release was elevated to 130 ± 6% with 100 nM DOPAC (P < 0.01; Fig. 6d). HVA did not affect glycerol release (data not shown).
Discussion
Our study is the first to systematically assess the effect of levodopa combined with the peripheral aromatic l-amino acid decarboxylase inhibitor, benserazide, on tissue metabolism in idiopathic Parkinson’s disease patients. Levodopa/benserazide intake caused a sharp increase in venous levodopa, DOPAC, and norepinephrine concentrations. Mean venous dopamine concentration increased nonsignificantly.
Although plasma norepinephrine concentration increased more than threefold, we observed no related changes in lipolytic activity [25, 26]. Indeed, levodopa/benserazide intake caused a switch from lipid to carbohydrate metabolism at the tissue level. Our in vitro adipocyte studies actually showed that levodopa attenuated isoproterenol-induced lipid mobilization.
Levodopa/benserazide influenced metabolism in a tissue-specific manner. With levodopa/benserazide, adipose tissue blood flow did not change. Thus, changes in local metabolite concentrations cannot be explained by changes in supply from, or clearance into, the systemic circulation. Venous and adipose microdialysate glucose remained stable with levodopa/benserazide throughout the experiment. This observation suggests that glucose uptake did not change in adipose tissue. However, a larger proportion of the glucose taken up by adipose tissue undergoes glycolysis, as evidenced by the increased dialysate lactate concentration. The slight decrease in adipose tissue dialysate glycerol indicates no change or even reduction in adipose tissue lipolysis with levodopa/benserazide.
In skeletal muscle, levodopa/benserazide intake resulted in a marked decrease in skeletal muscle blood flow. Even though blood flow and, therefore, glucose supply decreased, dialysate glucose concentrations remained unchanged. This observation suggests reduction in skeletal muscle glucose uptake under levodopa/benserazide. Similarly, levodopa even with carbidopa attenuates insulin-stimulated glucose transport in rat skeletal muscle [27, 28]. Lactate and pyruvate accumulation in skeletal muscle with levodopa/benserazide suggests that a larger proportion of the glucose taken up by skeletal muscle undergoes glycolysis. Reduction in lactate-to-pyruvate ratio with levodopa/benserazide is consistent with improved aerobic glycolysis. In rat myocytes, levodopa/carbidopa treatment attenuated glycogen synthase and tended to induce phosphorylase activity [27]. We speculate that levodopa may divert glucose from muscle glycogen synthesis to aerobic glycolysis.
Skeletal muscle dialysate glycerol concentration decreased under levodopa/benserazide. The measurement was not correlated with serum concentrations of levodopa or its metabolites [29]. However, skeletal muscle dialysate glycerol was positively correlated with serum glycerol 1 h after levodopa/benserazide intake. We suggest that the reduction in skeletal muscle dialysate glycerol resulted from diminished supply from the circulation [30]. One possible mechanism that could contribute to the effect of levodopa/benserazide on lipolysis is an altered availability of lipolysis-regulating hormones. Insulin attenuates while growth hormone and catecholamines stimulate lipolysis [31, 32]. Insulin and growth hormone concentrations did not change significantly with levodopa/benserazide. However, plasma norepinephrine increased more than threefold. DHPG, which is norepinephrine’s main intraneuronal metabolite, did not change with levodopa/benserazide. We speculate that the plasma norepinephrine increase may have been secondary to conversion from levodopa rather than reflex sympathetic activation [25]. Norepinephrine infusion that increases plasma concentrations from approximately 1 to 13 nM elicits a threefold increase in glycerol release from adipose tissue [26]. However, lipolysis increases only moderately when isolated human adipocytes are exposed to 1–10 nM norepinephrine [33]. Since we did not measure norepinephrine directly in adipose tissue, we cannot completely exclude that the levodopa-induced norepinephrine release was insufficient to activate adipose tissue lipolysis. Nevertheless, we speculate that absence of a change or, perhaps, reduction in lipolysis in the setting of raised plasma norepinephrine may be suggestive of an inhibitory effect of levodopa/benserazide on lipolysis.
In the event, adipose tissue glycerol correlated inversely with serum levodopa concentrations. Moreover, levodopa attenuated isoproterenol-induced lipolysis in isolated human adipocytes. Local levodopa concentrations in subcutaneous adipose tissue appear to increase in a similar manner as in serum after levodopa/benserazide intake [12, 34]. Thus, levodopa acutely attenuates catecholamine-induced adipose tissue lipolysis. The response may be explained by enzymatic degradation of levodopa by monoamine-oxidases (MAO A and B), which are highly expressed in the plasma membrane of adipocytes [13, 14]. Oxidation of the monoamines tyramine and benzylamine by these enzymes generates H2O2, which inhibits catecholamine-induced lipolysis in adipocytes [16, 35]. DOPAC at therapeutic concentrations [36] increased glycerol release from isolated adipocytes, which may have attenuated levodopa’s antilipolytic actions. DOPAC’s lack of an amino group rules out binding to lipolytic beta-adrenoreceptors. The more delayed increase in adipose tissue dialysate lactate with levodopa/benserazide may be secondary to norepinephrine release [16, 37].
A potential limitation of our study is that we used an open design without a control intervention. However, local blood flow and metabolism have been shown to remain constant in adipose tissue and skeletal muscle for at least 2 h [38]. Therefore, we conclude that levodopa/benserazide elicits pronounced metabolic changes in both adipose tissue and skeletal muscle with a switch from lipid to carbohydrate metabolism. In adipose tissue, levodopa/benserazide appears to attenuate lipolysis through direct antilipolytic actions. Therefore, we do not believe that levodopa/benserazide per se contributes to body fat loss in patients with Parkinson’s disease [1–3]. However, reduction in skeletal muscle glucose uptake could promote glucose intolerance in Parkinson’s disease [39].
References
Markus HS, Tomkins AM, Stern GM (1993) Increased prevalence of undernutrition in Parkinson’s disease and its relationship to clinical disease parameters. J Neural Transm Parkinson’s Dis Dement Sect 5:117–125
Davies KN, King D, Davies H (1994) A study of the nutritional status of elderly patients with Parkinson’s disease. Age Ageing 23:142–145
Bachmann CG, Trenkwalder C (2006) Body weight in patients with Parkinson’s disease. Mov Disord 21:1824–1830
Palhagen S, Lorefalt B, Carlsson M et al (2005) Does L-dopa treatment contribute to reduction in body weight in elderly patients with Parkinson’s disease? Acta Neurol Scand 111:12–20
Toth MJ, Fishman PS, Poehlman ET (1997) Free-living daily energy expenditure in patients with Parkinson’s disease. Neurology 48:88–91
Abbott RA, Cox M, Markus H et al (1992) Diet, body size and micronutrient status in Parkinson’s disease. Eur J Clin Nutr 46:879–884
Lorefalt B, Ganowiak W, Palhagen S et al (2004) Factors of importance for weight loss in elderly patients with Parkinson’s disease. Acta Neurol Scand 110:180–187
Macia F, Perlemoine C, Coman I et al (2004) Parkinson’s disease patients with bilateral subthalamic deep brain stimulation gain weight. Mov Disord 19:206–212
Giroux ML (2007) Parkinson disease: managing a complex, progressive disease at all stages. Cleve Clin J Med 74:313–320
Boyd AE III, Lebovitz HE, Pfeiffer JB (1970) Stimulation of human-growth-hormone secretion by L-dopa. N Engl J Med 283:1425–1429
Sirtori CR, Bolme P, Azarnoff DL (1972) Metabolic responses to acute and chronic L-dopa administration in patients with parkinsonism. N Engl J Med 287:729–733
Deleu D, Sarre S, Ebinger G et al (1993) Simultaneous monitoring of levodopa, dopamine and their metabolites in skeletal muscle and subcutaneous tissue in different pharmacological conditions using microdialysis. J Pharm Biomed Anal 11:577–585
Pizzinat N, Marti L, Remaury A et al (1999) High expression of monoamine oxidases in human white adipose tissue: evidence for their involvement in noradrenaline clearance. Biochem Pharmacol 58:1735–1742
Morin N, Lizcano JM, Fontana E et al (2001) Semicarbazide-sensitive amine oxidase substrates stimulate glucose transport and inhibit lipolysis in human adipocytes. J Pharmacol Exp Ther 297:563–572
Adams F, Boschmann M, Schaller K et al (2006) Tyramine in the assessment of regional adrenergic function. Biochem Pharmacol 72:1724–1729
Bairras C, Ferrand C, Atgie C (2003) Effect of tyramine, a dietary amine, on glycerol and lactate release by isolated adipocytes from old rats. J Physiol Biochem 59:161–167
Boschmann M, Krupp G, Luft FC et al (2002) In vivo response to alpha(1)-adrenoreceptor stimulation in human white adipose tissue. Obes Res 10:555–558
Jordan J, Tank J, Stoffels M et al (2001) Interaction between beta-adrenergic receptor stimulation and nitric oxide release on tissue perfusion and metabolism. J Clin Endocrinol Metab 86:2803–2810
Hoehn MM, Yahr MD (1967) Parkinsonism: onset, progression and mortality. Neurology 17:427–442
Hughes AJ, Ben-Shlomo Y, Daniel SE et al (1992) What features improve the accuracy of clinical diagnosis in Parkinson’s disease: a clinicopathologic study. Neurology 42:1142–1146
Arner P, Bolinder J, Eliasson A et al (1988) Microdialysis of adipose tissue and blood for in vivo lipolysis studies. Am J Physiol 255:E737–E742
Janke J, Engeli S, Gorzelniak K et al (2002) Mature adipocytes inhibit in vitro differentiation of human preadipocytes via angiotensin type 1 receptors. Diabetes 51:1699–1707
Han SK, Mytilineou C, Cohen G (1996) L-DOPA up-regulates glutathione and protects mesencephalic cultures against oxidative stress. J Neurochem 66:501–510
Fellander G, Linde B, Bolinder J (1996) Evaluation of the microdialysis ethanol technique for monitoring of subcutaneous adipose tissue blood flow in humans. Int J Obes Relat Metab Disord 20:220–226
Stallknecht B, Lorentsen J, Enevoldsen LH et al (2001) Role of the sympathoadrenergic system in adipose tissue metabolism during exercise in humans. J Physiol 536:283–294
Kurpad A, Khan K, Calder AG et al (1994) Effect of noradrenaline on glycerol turnover and lipolysis in the whole body and subcutaneous adipose tissue in humans in vivo. Clin Sci 86:177–184
Smith JL, Ju JS, Saha BM et al (2004) Levodopa with carbidopa diminishes glycogen concentration, glycogen synthase activity, and insulin-stimulated glucose transport in rat skeletal muscle. J Appl Physiol 97:2339–2346
Smith JL, Patil PB, Minteer SD et al (2005) Possibility of autocrine beta-adrenergic signaling in C2C12 myotubes. Exp Biol Med 230:845–852
Rose S, Jenner P, Marsden CD (1988) The effect of carbidopa on plasma and muscle levels of L-dopa, dopamine, and their metabolites following L-dopa administration to rats. Mov Disord 3:117–125
Coppack SW, Persson M, Judd RL et al (1999) Glycerol and nonesterified fatty acid metabolism in human muscle and adipose tissue in vivo. Am J Physiol 276:E233–E240
Duncan RE, Ahmadian M, Jaworski K et al (2007) Regulation of lipolysis in adipocytes. Annu Rev Nutr 27:79–101
Mauras N, Haymond MW (2005) Are the metabolic effects of GH and IGF-I separable? Growth Horm IGF Res 15:19–27
Hellström L, Wahrenberg H, Reynisdottir S et al (1997) Catecholamine-induced adipocyte lipolysis in human hyperthyroidism. J Clin Endocrinol Metab 82:159–166
Dizdar N, Kullman A, Norlander B et al (1999) Human pharmacokinetics of L-3,4-dihydroxyphenylalanine studied with microdialysis. Clin Chem 45:1813–1820
Visentin V, Prevot D, Marti L et al (2003) Inhibition of rat fat cell lipolysis by monoamine oxidase and semicarbazide-sensitive amine oxidase substrates. Eur J Pharmacol 466:235–243
Lyytinen J, Kaakkola S, Ahtila S et al (1997) Simultaneous MAO-B and COMT inhibition in L-dopa-treated patients with Parkinson’s disease. Mov Disord 12:497–505
Flechtner-Mors M, Jenkinson CP, Alt A et al (2005) Studies of phosphodiesterase effects on adipose tissue metabolism in obese subjects by the microdialysis technique. J Physiol Pharmacol 56:355–368
Goossens GH, Blaak EE, Saris WH et al (2004) Angiotensin II-induced effects on adipose and skeletal muscle tissue blood flow and lipolysis in normal-weight and obese subjects. J Clin Endocrinol Metab 89:2690–2696
Sandyk R (1993) The relationship between diabetes mellitus and Parkinson’s disease. Int J Neurosci 69:125–130
Acknowledgements
The authors thank Henning Damm, Katrin Sprengel, and Janin Andres for expert technical assistance and the Department of Surgery at the Vivantes Klinikum Prenzlauer Berg in Berlin for providing us with adipose tissue samples.
Conflict of Interest
The authors declared no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Adams, F., Boschmann, M., Lobsien, E. et al. Influences of levodopa on adipose tissue and skeletal muscle metabolism in patients with idiopathic Parkinson’s disease. Eur J Clin Pharmacol 64, 863–870 (2008). https://doi.org/10.1007/s00228-008-0532-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-008-0532-4