Abstract
Objective
Therapeutic drug monitoring (TDM) is a procedure in which the levels of drugs are assayed in various body fluids with the aim of individualizing the dose of critical drugs, such as cyclosporine A. Cyclosporine A assays are performed in blood.
Methods
We proposed the use of the Takagi and Sugeno-type “adaptive-network-based fuzzy inference system” (ANFIS) to predict the concentration of cyclosporine A in blood samples taken from renal transplantation patients. We implemented the ANFIS model using TDM data collected from 138 patients and 20 input parameters. Input parameters for the model consisted of concurrent use of drugs, blood levels, sampling time, age, gender, and dosing intervals.
Results
Fuzzy modeling produced eight rules. The developed ANFIS model exhibited a root mean square error (RMSE) of 0.045 with respect to the training data and an error of 0.057 with respect to the checking data in the MATLAB environment.
Conclusion
ANFIS can effectively assist physicians in choosing best therapeutic drug dose in the clinical setting.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Therapeutic Drug Monitoring (TDM) is a useful procedure that helps physicians estimate effective plasma concentrations of the prescribed drugs [1, 2]. To determine critical doses of drugs, the physicians use the quantitative TDM assay results in their clinical reasoning to diagnose drug toxicity, ineffective dosing or poor patient compliance [1–3]. As such, TDM offers the opportunity to control pharmacokinetic variability during the drug therapy based on the analyses of drug concentrations in body fluids rather than using the dose alone. However, TDM is not only a costly procedure, which restricts its use, but fast and easy analytical methods are not available for most agents in many medical centers.
Cyclosporine A, an immunosuppressant agent, is of critical value in terms of immunosuppressive therapy for the prevention of graft rejection and autoimmune diseases [4, 5]. The striking importance of cyclosporine A TDM assays becomes apparent when the outcomes of ineffective cyclosporine A treatment begin to manifest. Many factors affect the blood levels of cyclosporine A [6].
There has been limited use of TDM in planning a treatment regimen for cyclosporine A since what we measure is simply what we had administered. In fact, the basic requirement of most physicians is to know what to prescribe rather than to learn how effective the prescribed drug was. In other words, TDM should be used for checking whether the administered dose is effective.
The use of simple pharmacokinetic relationships is not easy and practical at outpatient clinics, and most of the mathematical algorithms currently available do not reflect patient characteristics, such as concurrent use of drugs, presence of various disease states, race, sex, among others. In addition, data from pharmacokinetic studies performed on large patient populations are scarce. The necessity of population pharmacokinetic studies performed using TDM data is important, as demonstrated in one study using Bayesian estimators [7].
Data mining, also known as knowledge-discovery in databases, is the process of automatically searching large volumes of data for patterns [7–14]. It is a fairly recent development and a contemporary topic in the field of computer sciences. However, current data mining procedures used many older computational techniques from statistics, information retrieval, machine learning and pattern recognition. One common approach to evaluate the fitness of a model generated via data mining techniques is called cross validation, which is a technique that produces an estimate of generalization error based on re-sampling. In simple terms, the general idea behind cross validation is that dividing the data into two or more separate data subsets allows one subset to be used to evaluate the generalizeability of the model learned from the other data subset(s). A data subset used to build a model is called a training set; the evaluation data subset is called the checking set.
In this study, we propose the use of adaptive-network-based fuzzy inference system (ANFIS) to predict the level of cyclosporine A in blood of renal transplantation patients.
Methods
Data
Cyclosporine A assays carried out in 2005 on renal transplant patients who had been admitted to the TDM Unit of Marmara University Hospital were included in this study. The use of this retrospective data set was accepted by the Local Research Ethics Committee of Marmara University, School of Medicine (Protocol and approval number: 2007-70/813).
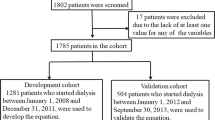
Whole blood samples were analyzed using the TDx assay [based on fluorescence polarization immunoassay (FPIA; Abbott Laboratories, Abbot Park, IL). Data on a total of 654 TDM assays were collected from 138 patients (78 male, 60 female). The concentration of cyclosporine A in the blood was monitored in each patient at different post-dose sampling times. The data collected for each assay were age of the patient (years), morning/evening doses of cyclosporine A (mg), post-dose sampling time (h), concentration of cyclosporine A in the blood (ng/ml), and gender. In the checking data set, 69 of the TDM assays were from female patients and 112 from male patients. In the training data set, 166 TDM assays were from female patients and 307 from male patients. The mean and ranges of the TDM parameters are given in Table 1.
The cyclosporine A assays were randomly assigned into two sets: 473 assays were used for training the data mining models, and the other 181 assays were used for checking the models. Some basic population statistics for the training and checking sets are shown in Tables 2 and 3.
Fuzzy modeling
Fuzzy modeling or fuzzy identification, first explored by Takagi and Sugeno, has found numerous practical applications in control, prediction and inference [13]. Fuzzy if–then rules or fuzzy conditional statements are expressions of the form IF A, THEN B, where A and B are linguistic labels of fuzzy sets characterized by the appropriate membership functions [13]. Fuzzy if-then rules are often employed to capture the imprecise modes of reasoning that play an essential role in the human ability to make decisions in an environment of uncertainty and imprecision. The ANFIS is a fuzzy inference system (FIS) implemented in the framework of adaptive networks [8]. By applying Jang’s hybrid learning procedure, an input–output mapping is constructed based on both fuzzy if–then rules (human knowledge) and stipulated input–output pairs [8]. Basically, a FIS is composed of five functional blocks:
-
1.
a rule base which contains a number of fuzzy if–then rules;
-
2.
a database which defines membership functions of the fuzzy sets used in the fuzzy rules;
-
3.
a decision-making unit which handles the inference operations of the rules;
-
4.
a fuzzification interface which converts the crisp inputs into degrees-of-match with linguistic values;
-
5.
a defuzzification interface which converts the fuzzy results of the inference into a crisp output.
In this study, Takagi and Sugeno’s fuzzy if–then rules are used such that the output of each rule is a linear combination of input variables plus a constant term, and the final output is the weighted average of each rule’s output. The rules’ premise membership functions are optimized by gradient descent, while the consequent equations are optimized by linear least squares estimation. The optimization process stops when the improvement in root mean square error (RMSE) after a pass through the data becomes less than 0.1% of the previous RMSE. The ANFIS constructs a consequent parameter matrix C based on the linguistic labels defined by the bell-shaped membership functions. As the values of these parameters change, the bell-shaped functions vary accordingly. The bell-shaped function is defined as:
A Takagi and Sugeno-type ANFIS is illustrated in Fig. 1. For simplicity, the fuzzy inference system shown in Fig. 1 has two inputs x and y and one output z, and the rule base contains two rules:
-
Rule 1:
If x is A 1 and y is B 1, then \(f_1 = p_1 x + q_1 y + r_1 .\)
-
Rule 2:
If x is A 2 and y is B 2, then \(f_2 = p_2 x + q_2 y + r_2 .\)
Schematic representation of Takagi and Sugeno’s type adaptive-network-based fuzzy inference system (ANFIS) for two rules (redrawn from [8])
In layer 1 of Fig. 1, every node i in this layer is a square node with a node function, \(\mu _{A_i } \left( x \right)\) where x is the input to node i, and A i is the linguistic label associated with this node. The parameter set {a i , b i , c i } of \(\mu _{A_i } \left( x \right)\) is referred to as premise parameters [8]. In layer 2 of Fig. 1, every node is a circle node labeled π, which multiplies the incoming signals and sends the product out. For instance:
Every node in layer 3 shown in Fig. 1 is a circle node labeled N. The ith node calculates the ratio of the ith rule’s firing strength to the sum of all rules’ firing strengths:
Every node in layer 4 shown in Fig. 1 is a square node with a node function:
Finally, the single node in fifth layer shown in Fig. 1 is a circle node labeled ∑ that computes the overall output as the summation of all incoming signals:
We developed the ANFIS model in the MATLAB environment, a numerical environment and programming language created by The MathWorks Inc. [15]. which allows easy matrix manipulation, plotting of functions and data, implementation of algorithms, creation of user interfaces and interfacing with programs in other languages. Although it specializes in numerical computing, an optional toolbox interfaces with the Maple symbolic engine, allowing it to be a part of a full computer algebra system.
Results
In our ANFIS model, we used 473 assays for training and the remainder (181 assays) for checking the model. The number of linear and nonlinear parameters were 168 (consequent parameters) and 69 (premise parameters), respectively. Eight fuzzy rules were found.
Table 4 presents the premise parameters of the bell-shaped membership functions for the linguistic labels of the linguistic variables, such as post-dose sampling time, morning dose and evening dose. The input vector,
consists of six age variables (A 1,A 2,A 3,A 4,A 5,A 6), one gender variable (G), one post-dose sampling time (ST), ten concurrent drug usage variables (C 1,C 2,C 3,C 4,C 5,C 6,C 7,C 8,C 9,C 10), one morning dose (M) and one evening dose (E). We choose one fuzzy set with the corresponding bell-shaped membership function for each age, gender and drug class input. For each post-dose sampling time, morning dose and evening dose inputs, we choose two fuzzy sets with two bell-shaped membership functions.
For example, suppose we want to predict the C2 level of a 23-year-old female patient that has a history of concurrent Class I and Class VIII drug usage with 100 mg of cyclosporine A morning and evening doses. The corresponding input vector should be given as \(\vec X = \left[ {0,0,1,0,0,0,0,0.081,1,0,0,0,0,0,0,1,0,0,0.500,0.500,1} \right]\) in normalized form. The output vector \(\vec O\) is computed from the matrix product \(\vec O = \vec X \times C.\)The consequent parameter matrix C constructed by ANFIS is presented in the Appendix. The overall output (predicted cyclosporine A level) is calculated by taking the weighed average of each rule’s output. Thus, the ANFIS model has a total of eight rules and one output, CyA level :
where \(\vec c_i \) corresponds to the ith column of the consequent matrix. The weight of each rule’s output is set to one. The fuzzy if–then rules after training can be expressed as follows:
-
Rule 1:
If ST is in ST morning and M is in Dose morning_low and E is in Dose evening_low , then \(Cyclosporine\,A\,level = \vec c_1 .\vec X.\)
-
Rule 2:
If ST is in ST morning and M is in Dose mornig_low and E is in Dose evening_high , then \(Cyclosporine\,A\,level = \vec c_2 .\vec X.\)
-
Rule 3:
If ST is in ST morning and M is in Dose mornig_high and E is in Dose evening_low , then \(Cyclosporine\,A\,level = \vec c_3 .\vec X.\)
-
Rule 4:
If ST is in ST morning and M is in Dose mornig_high and E is in Dose evening_high , then \(Cyclosporine\,A\,level = \vec c_4 .\vec X.\)
-
Rule 5:
If ST is in ST evening and M is in Dose mornig_low and E is in Dose evening_low , then \(Cyclosporine\,A\,level = \vec c_5 .\vec X.\)
-
Rule 6:
If ST is in ST evening and M is in Dose mornig_low and E is in Dose evening_high , then \(Cyclosporine\,A\,level = \vec c_6 .\vec X.\)
-
Rule 7:
If ST is in ST evening and M is in Dose mornig_high and E is in Dose evening_low , then \(Cyclosporine\,A\,level = \vec c_7 .\vec X.\)
-
Rule 8:
If ST is in ST evening and M is in Dose mornig_high and E is in Dose evening_high , then \(Cyclosporine\,A\,level = \vec c_8 .\vec X.\)
The ANFIS performances in the checking and training data sets for the prediction of cyclosporine A level are shown in Figs. 2 and 3, respectively. The developed ANFIS model exhibited a RMSE of 0.045 with respect to the training data and an error of 0.057.
Discussion
The concentration of a drug in the blood is the ratio of the absorbed dose to the volume of distribution, and many factors can affect the drug level since the drug is subject to eliminatory processes immediately following its absorption. All factors that affect the pharmacokinetics (absorption, distribution, metabolism and excretion) of the drug in question would determine the blood level of that drug. There is also a great variability among patients, and drug levels will sometimes change in the same individual during the course of treatment [1–3]. In TDM, the standard and acceptable approach is to use the measurement of the trough concentrations (C0) after the onset of the steady state to interprete the TDM data [1–3]. Cyclosporine A therapeutic trough values are considered to be within the range of 100 to 350 ng/ml [4]. Recent studies have shown that the first 2-hour post-dose concentration (C2) is a better index than the C0 measurement in improving the clinical outcomes for kidney transplant patients [16, 17].
Camps-Valls et al. developed three kinds of networks (multilayer perceptron [10], finite impulse response and the Elman recurrent network) for predicting cyclosporine A levels as a means to facilitate physicians in making informed clinical decisions in terms of drug therapy. They showed that the application of neural networks was clinically useful for the prediction of dose and blood concentrations of cyclosporine A in the steady-state condition [7, 10, 14]. Camps-Valls et al. also addressed that the need for the additional studies to explore statistical differences between data mining techniques [7].
The ANFIS was employed recently for detecting epilepsy entropies in electroencephalography, and a 90% classification accuracy was achieved [9]. The ANFIS can serve as a basis for constructing an input–output mapping based on both human knowledge (in the form of fuzzy if–then rules) and stipulated input–output data pairs. Due to their concise form, fuzzy if–then rules can easily capture the local description of the system under consideration.
We have developed here an ANFIS model with Takagi and Sugeno-type reasoning mechanism for predicting cyclosporine A levels. One of the advantages of using this approach for prediction is that the membership functions can be easily tuned to minimize the output error measure. By employing a hybrid learning procedure, ANFIS can refine fuzzy if–then rules obtained from experts to describe the input–output behavior of a complex TDM system. However, to make this approach more complete, structure identification, such as the selection of the number of membership functions on each input and, most importantly, an appropriate input–space partition style, is very important for achieving less RMSE. In this study, the input–space is partitioned according to age, dose administration time and concurrent drug use.
The impact of obesity, a frequent problem in patients after renal transplantation, has been attributed to poor graft and patient survival and worsening kidney functions [7]. In one study, smaller cyclosporine A doses were shown to be sufficient to maintain the C0 and C2 levels at levels similar those of the lean patients, results that were parallel to those of adult renal recipients [18]. The data processed in ours did not contain any information on body weights of the patients, but all other variables were applied successfully. We assume that the addition of age groups helps restore the missing parameter.
It has also been shown that morning or evening administration of cyclosporine A produces different pharmacokinetic differences [19]. In our method, we also included morning or evening doses, and the system predicts the concentration accordingly.
Factors such as the concurrent use of drugs may interfere with various pharmacokinetic factors and thus affect the target concentration. The effect of the use of other agents, such as diltiazem, was also studied, and the results showed that the concurrent use of diltiazem with cyclosporine A produced a better correlation with the area under curve fitting of the first 4 h following the cyclosporine A administration [20]. Similarly, the effect of ketoconazole use on the correlation of high cyclosporine A level and liver toxicity was also reported [21]. The use of concurrent drugs is included in our method to predict cyclosporine A level and may help physicians in prescribing drugs that require TDM. It is well documented that steroids and calcium channel blockers reduce cyclosporine A levels; consequently, the use of these agents should also be considered in choosing the best cyclosporine A dose to attain the target level. It has been demonstrated that under physiological conditions, the oral bioavailability of cyclosporine A is mainly controlled by cytochrome P4503A enzyme (CYP3A) in the upper intestine, rather than in the liver, but when P-glycoprotein is induced by dexamethasone, the intestinal absorption of cyclosporine A may be inhibited [22]. A microdialysis study demonstrated that the bioavailability of cyclosporine A was reduced markedly by methyl prednisolone succinate pulse treatment. The mechanism of this interaction was confirmed to involve an enhancement of small intestinal P-glycoprotein function and a decrease in bile secretion [23]. The orphan nuclear receptor, steroid and xenobiotic receptor [SXR; also called the pregnane X receptor (PXR)] is highly expressed in the liver and small intestine and regulates the CYP3A4 gene [24–26]. The SXR forms a heterodimer with retinoid X receptor (RXR) on xenobiotic-response elements (XREs), which are located in the promoter region of the CYP3A4 gene. A variety of known CYP3A4 inducers bind to SXR as ligands and stimulate transcription of the CYP3A4 [24–26]. It is also apparent that steroids induce CYP3A4 and P-glycoprotein via the SXR receptor and thus reduce the level of cyclosporine A in the blood. Age-related differences in the body’s capacity to metabolize steroids and xenobiotic compounds have also been demonstrated, suggesting an important role for SXR and its target genes, CYP3A4 and the multidrug resistance gene 1 (MDR1) in this process [27]. In our model, age groups were involved in the prediction of cyclosporine A blood levels. In our study, the drugs categorized into ten different pharmacological classes were included in the model for prediction the level of cyclosporine A in the blood. We are able to calculate the level of cyclosporine A at any time by entering the patient information prior to prescribing.
Genetic polymorphism of the CYP3A5 enzyme plays a critical role in cyclosporine dose requirements in terms of maintaining blood concentrations within the therapeutic target range [28]. It goes without saying that our model will be more valuable as a TDM tool if the type of isoenzyme is used as an addition input parameter. However, although we did not have the data on the genetic polymorphisms of enzymes in our patient cohort, we were still able to accurately predict cyclosporine A dose or blood levels.
We suggest that new studies should be planned that use the same approach for testing other critical dose drugs, such as antiepileptics, cardiac glycosides, and aminoglycosides. Various other pharmacological and pharmaceutical factors may be included in developing the model.
In conclusion, the results of our study demonstrate that ANFIS modeling can be used in clinical pharmacology for estimating the dose and facilitating safe prescribing. Based on our results, the application of ANFIS in the context of TDM is a clinically useful tool. We do not yet suggest that TDM assays are not required, but this approach may assist clinicians to determine the best dose with the aim of individualizing the drug therapy.
References
Karaalp A, Demir D, Gören MZ et al (2004) Therapeutic drug monitoring of immunosuppressant drugs in Marmara University Hospital. Ther Drug Monit 26:263–266
Aronson JK, Hardman M (1992) Why monitor drug therapy? Br Med J 305:947–948
Gross AS (1998) Best practice in therapeutic drug monitoring. Br J Clin Pharmacol 46:95–99
Jensen SA, Dalhoff KP (2001) Cyclosporin therapeutic drug monitoring. Transplant Proc 33:3003–3005
Cook TLJ (1998) Fever associated with cyclosporine for treating atopic dermatitis. Br Med J 317:1291
Wacke R, Rohde B, Engel G (2000) Comparison of several approaches of therapeutic drug monitoring of cyclosporine A based on individual pharmacokinetics. Eur J Clin Pharmacol 56:43–48
Camps-Valls G, Oltra BP, Olivas ES et al (2003) Prediction of cyclosporine dosage in patients after kidney transplantation using neural networks. IEEE Trans Biomed Eng 50:442–448
Jang JSR (1993) ANFIS: Adaptive-Network-based Fuzzy Inference Systems. IEEE Trans Syst Man Cybern 23:665–685
Kannathal N, Choo ML, Rajendra Acharya U et al (2005) Entropies for detection of epilepsy in EEG. Comput Methods Programs Biomed 80:187–194
Haykin S (1999) Neural networks: a comprehensive foundation. Prentice Hall, New Jersey
Dunham MH (2003) Data mining. Prentice Hall, New Jersey
Takagi T, Sugeno M (1985) Fuzzy identification of systems and its applications to modeling and control. IEEE Trans Syst Man Cybern 15:116–132
Zadeh LA (1965) Fuzzy sets. Inf Control 8:338–353
Elman JL (1988) Finding structure in time. Cogn Sci 14:179–211
MATLAB. Available via http://www.mathworks.com/products/matlab
Oellerich M, Armstrong VW (2002) Two-hour cyclosporine determination: an appropriate tool to monitor Neoral therapy? Ther Drug Monit 24:40–46
Morris RG, Russ GR, Cervelli MJ (2002) Comparison of trough, 2-hour and limited AUC blood sampling for monitoring cyclosporin (Neoral) at day 7 post-renal transplantation and incidence of rejection in the first month. Ther Drug Monit 24:479–486
Kasap B, Soylu A, Turkmen M et al (2006) Effect of obesity and overweight on cyclosporine blood levels and renal functions in renal adolescent recipients. Transplant Proc 38:463–465
Iwahori T, Takeuchi H, Matsuno N et al (2005) Pharmacokinetic differences between morning and evening administration of cyclosporine and tacrolimus therapy. Transplant Proc 37:1739–1740
Aros CA, Schneider HO, Flores CA et al (2005) Correlation between C2 and AUC(0–4) in renal transplant patients treated with diltiazem. Transplant Proc 37:1580–1582
Videla C, Vega J, Borja H (2005) Hepatotoxicity associated with cyclosporine monitoring using C2 recommendations in adults renal recipients receiving ketoconazole. Transplant Proc 37:1574–1576
Jin M, Shimada T, Yokogawa K et al (2006) Site-dependent contributions of P-glycoprotein and CYP3A to cyclosporin A absorption, and effect of dexamethasone in small intestine of mice. Biochem Pharmacol 72:1042–1050
Konishi H, Sumi M, Shibata N et al (2004) Decrease in oral bioavailability of cyclosporin by intravenous pulse of methylprednisolone succinate in rats. J Pharm Pharmacol 56:1259–1266
Lehmann JM, Mckee DD, Watson MA et al (1998) The human orphan nuclear receptor PXR is activated by compounds that regulate CYP3A4 gene expression and cause drug interactions. J Clin Invest 102:1016–1023
Blumberg B, Sabbagh W Jr, Juguilon H et al (1998) SXR, a novel steroid and xenobiotic-sensing nuclear receptor. Genes Dev 12:3195–3205
Bertilsson G, Heidrich J, Svensson K et al (1998) Identification of a human nuclear receptor defines a new signaling pathway for CYP3A induction. Proc Natl Acad Sci USA 95:12208–12213
Akira T, Manabu T, Noriyuki K et al (2002) Putative role of the orphan nuclear receptor SXR (Steroid and Xenobiotic Receptor) in the mechanism of CYP3A4 inhibition by xenobiotics. J Biol Chem 277:32453–32458
Haufroid V, Mourad M, Van Kerckhove V et al (2004) The effect of CYP3A5 and MDR1 (ABCB1) polymorphisms on cyclosporine and tacrolimus dose requirements and trough blood levels in stable renal transplant patients. Pharmacogenetics 14:147–154
Acknowledgements
We appreciate the generous work of the “Marmara University, School of Medicine, Therapeutic Drug Monitoring Unit” staff, who carried out the analyses and all the physicians who referred the patients to the unit.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
The consequent parameter matrix C of the developed ANFIS model:
Rights and permissions
About this article
Cite this article
Gören, S., Karahoca, A., Onat, F.Y. et al. Prediction of cyclosporine A blood levels: an application of the adaptive-network-based fuzzy inference system (ANFIS) in assisting drug therapy. Eur J Clin Pharmacol 64, 807–814 (2008). https://doi.org/10.1007/s00228-008-0490-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-008-0490-x