Abstract
Romosozumab can increase bone mineral density (BMD) in patients with osteoporosis, but some patients do not respond to it. This study aimed to identify risk factors for being a nonresponder to romosozumab treatment. This retrospective observational study included 92 patients. Romosozumab (210 mg) was subcutaneously administered to the participants every 4 weeks over 12 months. We excluded patients who previously underwent treatment for osteoporosis to assess the impact of romosozumab alone. We evaluated the proportion of patients who did not respond to romosozumab treatment to the lumbar spine and hip with increased BMD. Nonresponders were defined as those with a bone density change of < 3% after 12 months of treatment. We compared demographics and biochemical markers between responders and nonresponders. We found that 11.5% of patients were nonresponders at the lumbar spine, and 56.8% were nonresponders at the hip. A risk factor for nonresponse at the spine was low type I procollagen N-terminal propeptide (P1NP) values at 1 month. The cutoff value for P1NP at month 1 was 50 ng/ml. We found that 11.5% and 56.8% of patients experienced no significant improvement in the lumbar spine and hip BMD, respectively. Clinicians should use nonresponse risk factors to inform decisions about romosozumab treatment for patients with osteoporosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
As the populations of developed countries continue to age, the number of patients affected by osteoporosis has increased [1]. Globally, > 200 million women have osteoporosis [2]. Patients with osteoporosis are at an increased risk for fragility fractures, which are associated with high 1-year mortality rates. For example, between 5.9% and 28% of vertebral fractures and 15.1% and 23.3% of proximal hip fractures result in mortality within one year [3, 4]. Additionally, patients with fragility fractures have a lower quality of life; simultaneously, their caregivers’ quality of life is also reduced [5]. Recent reports indicate that therapeutic intervention with appropriate drugs can reduce mortality after spine and hip fractures in patients with osteoporosis [6, 7]. This evidence suggests that therapeutics are an essential intervention for osteoporotic fractures.
Romosozumab is an effective monoclonal antibody that binds to and inhibits sclerostin, thereby increasing bone mineral density (BMD) [8]. A lack of sclerostin is a cause of van Buchem disease, an autosomal recessive inherited form of sclerosteosis characterized by progressive bone thickening [8]. Romosozumab’s efficacy was demonstrated in a large phase III clinical trial in postmenopausal females, which reported that one year of romosozumab treatment led to a 13.3% increase in lumbar spine BMD and a 6.8% increase in total hip BMD [9]. Romosozumab increases bone formation markers and decreases bone resorption markers, thereby rapidly increasing BMD via its dual effects on bone formation and breakdown [9]. When used clinically, romosozumab can rapidly increase BMD, particularly in the lumbar spine [10,11,12]. However, there are few reports on which patients respond favorably to romosozumab treatment [10, 11], and some patients do not experience a meaningful increase in BMD. This study aimed to identify variables that can be used as early predictors of nonresponse to romosozumab treatment. Clinicians could use these predictors to determine a patient’s likelihood of nonresponse to romosozumab, improving osteoporosis treatment outcomes.
Method
Study Design and Subjects
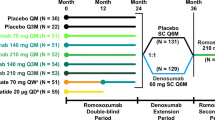
This retrospective observational study included patients treated with romosozumab at our hospital and affiliated hospitals from March 2019 to December 2021. All patient information and outcome data were extracted from patients’ medical records. All of the patients were Asian. Patients were included in the study if they had multiple low-energy fractures (including vertebral fractures, proximal femur fractures, proximal humerus fractures, and distal radius fractures) or low BMD values at the spine or total hip (≤ 2.5 standard deviations) before starting romosozumab treatment. The use of other antiosteoporosis treatments before treatment with romosozumab affects romosozumab efficacy [10, 11, 13, 14]. Therefore, we only included patients who had started osteoporosis treatment with romosozumab and had no previous exposure to other osteoporosis medications. Patients diagnosed with cerebrovascular disease within 1 year of starting romosozumab and those who did not complete ≥ 12 months of romosozumab treatment were excluded from the study. We excluded the patients with high parathyroid hormone (PTH) levels (> 70 pg/ml) and vitamin D deficiency (25OH VitD < 20 ng/ml) [15, 16]. Patients included in the study received subcutaneous injections of romosozumab (210 mg) once every 4 weeks. In our hospital, a nurse always injects patients with romosozumab.
Data Collection and Preparation
BMD tests were performed using dual-energy X-ray absorptiometry. Spinal BMD was evaluated at L1–L4, and hip BMD was measured using the entire hip. BMD measurements were taken at months 0, 6, and 12 after starting romosozumab treatment. Discovery (Hologic, Marlborough, MA, USA) and Lunar iDXA (GE Healthcare, Chicago, IL, USA) units were used for bone densitometry, but each patient was measured with the same device throughout their assessments. Although we used different DEXA instruments for our multicenter study, a previous study concluded that the accuracy of Hologic and Lunar DEXA machines is consistent, and they can be used with confidence in multicenter clinical trials [17]. Patient characteristics extracted from medical records include age, sex, body mass index (BMI), primary or secondary osteoporosis diagnosis, and concomitant use of vitamin D (yes/no). Blood tests to assess renal function (estimated glomerular filtration rate; eGFR), PTH, 25OH Vitamin D (25OH VitD), and bone metabolism markers were performed at 0, 1, 3, 6, 9, and 12 months after starting romosozumab treatment. Intact type I procollagen N-terminal propeptide (iP1NP) was measured as a bone formation marker, whereas tartrate-resistant acid phosphatase 5b (TRACP-5b) was measured as a bone resorption marker [18,19,20,21]. Both P1NP and TRACP-5b are insensitive to renal function and daily fluctuations [22,23,24]. The iP1NP was quantified using the Elecsys reagent (Roche Diagnostics, Minato-ku, Tokyo, Japan) and the enzyme-linked immunoassay (ECLIA) principle. The Osteolinx kit (Nittobo Medical, Koriyama, Fukushima, Japan) was used to measure TRACP-5b using an enzyme-linked immunosorbent assay principle.
We used the least significant change (LSC) for BMD to judge the treatment efficacy [25]. Based on previous studies, we set the LSC for the spinal BMD change from baseline to month 12 at 3% [25,26,27,28,29]. We also examined the use of a significant change of 6% for spinal BMD because previous reports indicated large effects of romosozumab in the spine [9,10,11,12, 14, 27]. We used a 3% LSC change from baseline to assess efficacy at the hip [10, 25]. The main objective was to calculate the percentage of patients who did not achieve the LSC value for BMD increase at each assessment site (nonresponders). We also compared patient characteristics (including bone formation markers) between nonresponders and responders and examined risk factors for being a nonresponder. All study procedures complied with the 1964 Helsinki declaration and its later amendments and were approved by our University Ethics Committee. The study followed the ethical standards of the 1964 Declaration of Helsinki and its later human and animal rights amendments. Informed consent was obtained from all participants included in the study.
Statistical Analysis
Easy R (EZR), an R interface (Saitama Medical Center, Jichi Medical University, Saitama, Japan), was used for all statistical analyses [30]. Data distributions were tested for normality using the Kolmogorov–Smirnov test; subsequently, nonparametric tests were used for all comparisons. We used the Mann–Whitney U and Fisher’s exact tests to compare demographics and laboratory results between nonresponders and responders. We recognize the possibility of type 1 errors when performing multiple statistical tests. However, we chose to perform these tests in our Tables, which were summary statistics for the background factors, to evaluate the examinee’s identification of possible risk factors using logistic regression analysis. Nonresponse-related risk factors were examined using logistic regression analysis, with trend scores for sex and age. All tests with α = 0.05 were considered significant. Specific cutoff values were calculated for identified risk factors using receiver operating characteristic curves.
Results
In total, 92 patients completed 12 months of romosozumab treatment (see Table 1 for patient demographics). Of them, 67 patients were diagnosed with primary osteoporosis, and 25 were diagnosed with secondary osteoporosis. The documented causes of secondary osteoporosis included cases of diabetes mellitus (14 cases), rheumatoid arthritis (2 cases), glucocorticoid-induced osteoporosis (4 cases), neurological disease (3 cases), renal failure (3 cases), myelodysplastic syndrome (2 cases), multiple myeloma (1 cases), and malignant lymphoma (1 case). Secondary pathologies in secondary osteoporosis cases occasionally overlapped. A total of 17 patients used concomitant vitamin D (0.75 µm eldecalcitol) preparations. At baseline, 67 patients presented with fragility fractures, including 60 vertebral fractures, affecting a mean of 2.12 vertebrae per patient. As for other fragility fractures, 12 cases of proximal femoral fracture, 3 cases of proximal humerus fracture, and 2 cases of distal radius fracture were observed (some occurred at multiple sites in the same patient). Before the start of treatment, the mean T-score was − 2.90 [− 4.1 to 3.7] for the spine and 2.65 [− 4.10 to − 0.10] for the total hip. Of the 92 patients included in this study, 78 underwent spinal BMD testing, and 81 underwent hip BMD testing. We could not perform all tests in some cases due to postoperative restrictions. We assessed the PTH of 62 patients, iP1NP for 79 patients, and TRACP-5b for 66 patients. The median iP1NP at the start of treatment was 60.70 ng/ml [Interquartile range (IR) 15.90–142.00 ng/ml, average 64.17 ng/ml, and standard error (SE) 3.28 ng/ml], and the median TRACP-5b was 632.5 mU/dL [IR 134.00–1500 mU/dL, average 657.30 mU/dL, and SE 39.45 mU/dL]. The mean BMD change from baseline to month 12 was 14.24% [− 6.50%–44.88%, average 15.55%, and SE 1.16%] at the spine and 2.49% [− 16.01%–19.88%, average 2.43%, and SE 0.74%] at the hip.
Nonresponders with Spinal BMD at a 3% Cutoff
Sixty-nine patients experienced an improvement of at least 3% in spinal BMD (responders), whereas nine patients did not (nonresponders). A comparison between responder and nonresponder characteristics is shown in Table 2. Nonresponders had a significantly lower change in spine and total hip BMD at month 6 (spine: responders 11.71% vs nonresponders 1.12%, p = 0.02, total hip: responders 1.08% vs − x2.98%, p = 0.008.), and lower iP1NP values at months 1 and 3 (Month 1: responders 116.50 ng/ml vs nonresponders 40.20 ng/ml, p = 0.023, month 3; responders 81.70 ng/ml vs 57.05 ng/ml, p = 0.038.) Moreover, nonresponders demonstrated a significantly greater TRACP-5b change at months 1 and 9 (Month 1: responder − 41.05% vs nonresponder 1.99%, p = 0.014, month 9: responder − 43.58% vs nonresponder − 7.05%, p = 0.043.)
We also performed logistic regression analysis to examine the risk for nonresponse to romosozumab treatment at the spine with a 3% LSC value (Table 3). We found that less of a change in spinal and total hip BMD at month 6 was associated with greater odds of nonresponse (spine: OR = 0.743, p = 0.006; total hip: OR = 0.79, p = 0.028). The calculated cutoff values for nonresponders were a spinal BMD change of ≤ 1.95% (AUC 0.88, 95% 0.73–1.00) and a hip BMD change of ≤ − 1.55% at month 6 (AUC 0.79, 95% 0.64–0.94). Additionally, we found that lower iP1NP values at month 1 was associated with greater odds for nonresponse (OR = 0.927, p = 0.042). The cutoff values for month 1 for iP1NP were ≤ 50.30 ng/ml (AUC 0.86, 95% 0.63–1). Also, we found that a greater TRACP-5b change at month 9 was a risk factor for nonresponse (OR = 1.11, p = 0.048). The cutoff values for the TRACP-5b change in month 9 was ≥ − 20.07% (AUC 0.83, 95% 0.62–1.00).
Nonresponders with Spinal BMD at a 6% Cutoff
We found that 66 patients were responders, and 12 were nonresponders. Comparisons between responder and nonresponder characteristics are shown in Supplementary Table 1. Nonresponders demonstrated significantly lower changes in the spine and total hip BMD at month 6 (spine: responder 12.28% vs nonresponder 1.79%, p < 0.001, total hip: responder 1.11% vs − 2.81%, p = 0.008.) and lower iP1NP values at months 1 and 3 (Month 1: responder 118.5 ng/ml vs nonresponder 59.15 ng/ml, p = 0.004, month 3: responder 85 ng/ml vs nonresponder 59.25 ng/ml, p = 0.014.) In contrast, a significantly greater TRACP-5b change at months 1 and 9 was observed in nonresponders (Month 1: responder − 41.05% vs nonresponder 1.99%, p = 0.014, month 9: responder − 43.58 vs nonresponder − 7.05%, p = 0.043.)
We also performed logistic regression to evaluate the risk of nonresponse to romosozumab treatment at the spine with a 6% change (Supplementary Table 2). We found that less change in spinal and total hip BMD at month 6 was associated with a greater odd of nonresponse (spine: OR = 0.703, p = 0.001; total hip: OR = 0.789, p = 0.012). The cutoff values for nonresponders were a spinal BMD change of ≤ 3.77% (AUC 0.91, 95% 0.81–1.00) and a hip BMD change of ≤ − 1.55% at month 6 (AUC 0.77, 95% 0.61–0.92). We also found that smaller iP1NP values at months 1 and 3 were associated with a greater odds for nonresponse (month 1: OR = 0.951, p = 0.025; month 3: OR = 0.956, p = 0.03). The cutoff values for iP1NP at months 1 and 3 were ≤ 69.30 ng/ml (AUC 0.88, 95% 0.73–1.00) and ≤ 62.40 ng/ml (AUC 0.78, 95% 0.62–0.93), respectively. In addition, we found that a greater TRACP-5b change at month 9 was a risk factor for nonresponse (OR = 1.11, p = 0.048). The cutoff values for the TRACP-5b change in month 9 was ≥ ˗20.07% (AUC 0.83, 95% 0.62–1.00).
Nonresponders with Total Hip BMD
We found that 35 patients experienced an improvement of at least 3% BMD at the total hip (responders), whereas 46 did not (nonresponders). A comparison between responder and nonresponder characteristics is shown in Table 4. Nonresponders had a smaller change in total hip BMD at month 6 (responder 2.74% vs nonresponder − 0.86%, p = 0.005), lower BMI (responder 22.71 kg/m2 vs nonresponder 20.20 kg/m2, p = 0.019), and lower iP1NP at month 1 (responder 124 ng/ml vs nonresponder 82.65 ng/ml, p = 0.046). A greater change in iP1NP at month 12 was significantly associated with being a nonresponder (responder − 34.57% vs nonresponder − 28.99%, p = 0.049).
We also performed logistic regression analysis to examine the risk of nonresponse to romosozumab treatment at the hip (Table 5). We found that a lower change in total hip BMD at month 6 was associated with a greater odds of nonresponse (BMD: OR = 0.846, p = 0.007). The cutoff value for nonresponders was a hip BMD change of ≤ 1.08% at month 6 (AUC 0.70, 95% 0.57–0.83).
Discussion
In this study, we examined the percentage of patients with osteoporosis who did not experience a significant increase in BMD with a 12-month course of romosozumab treatment (nonresponders). The importance of this study is that we investigated the effects of romosozumab in isolation; all previously treated patients were excluded, and only patients who started osteoporosis treatment with romosozumab were included. Only ~ 12% of patients were spine nonresponders with a cutoff of a 3% increase in BMD, whereas ~ 57% of patients were total hip nonresponders with a cutoff of a 3% increase in BMD. Cases with low iP1NP values in the first month were found to be at risk for spinal nonresponders. The results of this study can be used to estimate a patient’s odds of responding to romosozumab treatment, which can be used to make a clinically informed decision about osteoporosis treatment. We believe that presenting specific cutoff values will make clinical applications more feasible.
Recently, many papers have reported a high efficacy of romosozumab in preventing new bone fractures and increasing BMD [9,10,11,12,13, 31, 32]. Romosozumab and teriparatide appear to stimulate bone formation, but their mechanisms differ [13]. Romosozumab has a modeling effect, whereas teriparatide has a remodeling effect [33, 34]. Previous papers have reported that this difference in effects causes differences in cortical and trabecular bone growth and changes in bone strength [13]. However, there are still relatively few reports on patients who do or do not benefit from romosozumab. Some evidence was reported that prior osteoporosis treatment before starting romosozumab confounds the observed effects of romosozumab treatment [10, 11, 13, 14]. However, while some studies reported that BMD, iP1NP, and TRACP-5b values before the start of romosozumab treatment were correlated with an improvement in spinal BMD after 12 months of treatment [10], others described the percentage change in iP1NP and TRACP-5b as potential predictors of both spine and total hip BMD improvement [11, 32]. However, these studies combined patients newly started on osteoporosis treatment with romosozumab and those previously using antiosteoporosis treatments. Additionally, they did not focus on nonresponders but rather on patients who exhibited a higher percent change in BMD. Importantly, some patients do not respond to treatment with romosozumab, despite its effectiveness in improving BMD in the total population. Our study aimed to examine the proportion of patients who are nonresponders to romosozumab treatment and identify early predictors of nonresponse.
In our study, 88.46% of patients were responders at the spine with a cutoff value of a 3% improvement in BMD. Our results are comparable to the previous studies examining teriparatide treatment, where 91% of patients experienced a 3% increase in spinal BMD at month 18, and 88% experienced a 3% increase at month 24 [26, 28]. The similarity between studies supports romosozumab’s favorable treatment effects [26, 28].
Early iP1NP values, particularly a low iP1NP level at month 1, were a significant risk factor for spine BMD. We consider iP1NP to be the most convenient prognostic indicator of romosozumab efficacy. The same is true for teriparatide agents, where increases in P1NP during early treatment have previously been correlated with increased BMD [35]. Early iP1NP may have predictive value for osteogenic agents. Transient and rapid increases in iP1NP from week 2 to month 1 of treatment are characteristics of romosozumab, and the importance of these increases is well recognized [11, 13, 31]. Regarding the specific value of iP1NP during treatment with romosozumab, it may be difficult to achieve a 3% increase in spinal BMD if iP1NP is < 50 ng/ml in the first month. Conversely, if the iP1NP at month 1 exceeds 70 ng/ml, the percent change of spine BMD at month 12 is likely to exceed 6%. We believe that specific numbers will be more useful in clinical practice.
In terms of bone resorption markers, a greater change in TRACP-5b at month 9 was a risk factor for spinal BMD nonresponse. However, since the results were obtained in month 9, we considered these results to be of limited utility in predicting the efficacy of romosozumab. In the BMD of the spine, the logistic regression analysis indicated a change in TRACP-5b in the first month with a p-value of 0.065 (both, at Spine 3% and 6%). If the sample size is increased, TRACP-5b in the first month may potentially serve as a significant risk factor. Nonetheless, further investigation is necessary to augment the number of cases. A previous study reported that the rate of change in TRACP-5b at month 3 is related to the rate of change in spine BMD [36]. Similarly, our study found that a change in TRACP-5b, rather than the absolute value of TRACP-5b, is an important bone resorption marker for predicting romosozumab response. Similar results have been reported in previous studies, but the reasons for these results require further investigation [11, 36, 37].
However, failure to meet the cutoff values for these risk factors does not mean that immediate discontinuation of romosozumab therapy is recommended. Reports on teriparatide suggest that patients with significantly elevated bone metabolism markers can be encouraged to continue treatment [35]. Additionally, favorable results may motivate patients to continue independently [35]. Conversely, patients who do not have a significant early increase in iP1NP during treatment may need to be evaluated for compliance, injection site, and method, which should be confirmed with the healthcare provider responsible for injections, or for conditions that impair response, such as vitamin D deficiency [35].
Limitations
Our study has some limitations, including the small sample size, retrospective design, and uneven distribution of age and sex. This study that included Asian participants may have an impact on the results. Smoking, a risk factor for osteoporosis, could not be evaluated in this study because it was not documented in the medical charts. We did not measure thyroid hormone levels in this study. Furthermore, there were only four cases of glucocorticoid use and one case of proton pump inhibitor use. Due to the small number of cases, we could not evaluate the association between the use of these concomitant medications. Finally, due to the small number of patients who received active vitamin D preparations concurrently, more research into the relationship between vitamin D and romosozumab is required. Future research should be conducted with larger sample sizes and prospective research designs.
Conclusion
Based on our results, a month-1 iP1NP value was a risk factor for nonresponse in the spine BMD. In contrast, the percentage of hip nonresponders was higher than that for the spine, with a cutoff of a 3% increase in BMD. Regarding the specific value of iP1NP during the first month, it may be difficult to achieve a 3% increase in spine BMD with an iP1NP value < 50 ng/ml. Accordingly, these risk factors can be used to make informed decisions about romosozumab treatment for osteoporosis patients.
References
Lems WF, Raterman HG (2017) Critical issues and current challenges in osteoporosis and fracture prevention. An overview of unmet needs. Ther Adv Musculoskelet Dis 9:299–316. https://doi.org/10.1177/1759720X17732562
Anam AK, Insogna K, Anam A, Insogna K (2021) Update on osteoporosis screening and management. Medical Clin N 105:1117–1134. https://doi.org/10.1016/j.mcna.2021.05.016
Johnell O, Kanis JA, Odén A, Sernbo I, Redlund-Johnell I, Petterson C, De Laet C, Jönsson B (2004) Mortality after osteoporotic fractures. Osteoporos Int 15:38–42. https://doi.org/10.1007/s00198-003-1490-4
Morin S, Lix LM, Azimaee M, Metge C, Caetano P, Leslie WD (2011) Mortality rates after incident non-traumatic fractures in older men and women. Osteoporos Int 22:2439–2448. https://doi.org/10.1007/s00198-010-1480-2
Soen S, Usuba K, Crawford B, Adachi K (2021) Family caregiver burden of patients with osteoporotic fracture in Japan. J Bone Miner Metab 39:612–622. https://doi.org/10.1007/s00774-020-01197-9
Sambrook PN, Cameron ID, Chen JS, March LM, Simpson JM, Cumming RG, Seibel MJ (2011) Oral bisphosphonates are associated with reduced mortality in frail older people: a prospective five-year study. Osteoporos Int 22:2551–2556. https://doi.org/10.1007/s00198-010-1444-6
Iida H, Sakai Y, Seki T, Watanabe T, Wakao N, Matsui H, Imagama S (2022) Bisphosphonate treatment is associated with decreased mortality rates in patients after osteoporotic vertebral fracture. Osteoporos Int. https://doi.org/10.1007/s00198-021-06264-z
Balemans W (2001) Increased bone density in sclerosteosis is due to the deficiency of a novel secreted protein (SOST). Hum Mol Genet 10:537–543. https://doi.org/10.1093/hmg/10.5.537
Cosman F, Crittenden DB, Adachi JD, Binkley N, Czerwinski E, Ferrari S, Hofbauer LC, Lau E, Lewiecki EM, Miyauchi A, Zerbini CAF, Milmont CE, Chen L, Maddox J, Meisner PD, Libanati C, Grauer A (2016) Romosozumab treatment in postmenopausal women with osteoporosis. N Engl J Med 375:1532–1543. https://doi.org/10.1056/NEJMoa1607948
Tominaga A, Wada K, Okazaki K, Nishi H, Terayama Y, Kato Y (2021) Early clinical effects, safety, and predictors of the effects of romosozumab treatment in osteoporosis patients: one-year study. Osteoporos Int 32:1999–2009. https://doi.org/10.1007/s00198-021-05925-3
Ebina K, Tsuboi H, Nagayama Y, Kashii M, Kaneshiro S, Miyama A, Nakaya H, Kunugiza Y, Hirao M, Okamura G, Etani Y, Takami K, Goshima A, Miura T, Nakata K, Okada S (2021) Effects of prior osteoporosis treatment on 12-month treatment response of romosozumab in patients with postmenopausal osteoporosis. Joint Bone Spine 88:105219. https://doi.org/10.1016/j.jbspin.2021.105219
Kobayakawa T, Suzuki T, Nakano M, Saito M, Miyazaki A, Takahashi J, Nakamura Y (2021) Real-world effects and adverse events of romosozumab in Japanese osteoporotic patients: a prospective cohort study. Bone Rep 14:101068. https://doi.org/10.1016/j.bonr.2021.101068
Langdahl BL, Libanati C, Crittenden DB, Bolognese MA, Brown JP, Daizadeh NS, Dokoupilova E, Engelke K, Finkelstein JS, Genant HK, Goemaere S, Hyldstrup L, Jodar-Gimeno E, Keaveny TM, Kendler D, Lakatos P, Maddox J, Malouf J, Massari FE, Molina JF, Ulla MR, Grauer A (2017) Romosozumab (sclerostin monoclonal antibody) versus teriparatide in postmenopausal women with osteoporosis transitioning from oral bisphosphonate therapy: a randomised, open-label, phase 3 trial. Lancet 390:1585–1594. https://doi.org/10.1016/S0140-6736(17)31613-6
Cosman F, Kendler DL, Langdahl BL, Leder BZ, Lewiecki EM, Miyauchi A, Rojeski M, McDermott M, Oates MK, Milmont CE, Libanati C, Ferrari S (2022) Romosozumab and antiresorptive treatment: the importance of treatment sequence. Osteoporos Int 33:1243–1256. https://doi.org/10.1007/s00198-021-06174-0
Roman SA, Roman S, Sosa J, Pietrzak R, Snyder P, Thomas D, Udelsman R, Mayes L et al (2011) The effects of serum calcium and parathyroid hormone changes on psychological and cognitive function in patients undergoing parathyroidectomy for primary hyperparathyroidism. Ann Surg 253:131–137. https://doi.org/10.1097/SLA.0b013e3181f66720
Holick MF (2017) The vitamin D deficiency pandemic: Approaches for diagnosis, treatment and prevention. Rev Endocr Metab Disord 18:153–165. https://doi.org/10.1007/s11154-017-9424-1
Tothill P, Fenner JAK, Reid DM, Tothill P, Fenner JAK, Reid DM (1995) Comparisons between three dual-energy X-ray absorptiometers used for measuring spine and femur. Br J Radiol 68:621–629. https://doi.org/10.1259/0007-1285-68-810-621
Cavalier E, Souberbielle JC, Gadisseur R, Dubois B, Krzesinski JM, Delanaye P (2014) Inter-method variability in bone alkaline phosphatase measurement: clinical impact on the management of dialysis patients. Clin Biochem 47:1227–1230. https://doi.org/10.1016/j.clinbiochem.2014.04.007
Eastell R, Krege JH, Chen P, Glass EV, Reginster JY (2006) Development of an algorithm for using PINP to monitor treatment of patients with teriparatide. Curr Med Res Opin 22:61–66. https://doi.org/10.1185/030079905X75096
Igarashi Y, Lee MY, Matsuzaki S (2002) Acid phosphatases as markers of bone metabolism. J Chromatogr B Analyt Technol Biomed Life Sci 781:345–358. https://doi.org/10.1016/s1570-0232(02)00431-2
Gertz BJ, Clemens JD, Holland SD, Yuan W, Greenspan S (1998) Application of a new serum assay for type I collagen cross-linked n-telopeptides: assessment of diurnal changes in bone turnover with and without alendronate treatment. Calcif Tissue Int 63:102–106. https://doi.org/10.1007/s002239900497
Garnero P, Vergnaud P, Hoyle N, Garnero P, Vergnaud P, Hoyle N (2008) Evaluation of a fully automated serum assay for total N-terminal propeptide of type I collagen in postmenopausal osteoporosis. Clin Chem 54:188–196. https://doi.org/10.1373/clinchem.2007.094953
Szulc P, Naylor K, Hoyle NR, Eastell R, Leary ET (2017) Use of CTX-I and PINP as bone turnover markers: National Bone Health Alliance recommendations to standardize sample handling and patient preparation to reduce pre-analytical variability. Osteoporos Int 28:2541–2556. https://doi.org/10.1007/s00198-017-4082-4
Yamada S, Inaba M, Kurajoh M, Shidara K, Imanishi Y, Ishimura E, Nishizawa Y (2008) Utility of serum tartrate-resistant acid phosphatase (TRACP5b) as a bone resorption marker in patients with chronic kidney disease: independence from renal dysfunction. Clin Endocrinol (Oxf) 69:189–196. https://doi.org/10.1111/j.1365-2265.2008.03187.x
Fogelman I, Blake GM (2000) Different approaches to bone densitometry. J Nucl Med 41:2015–2025
Gallagher JC, Rosen CJ, Chen P, Misurski DA, Marcus R (2006) Response rate of bone mineral density to teriparatide in postmenopausal women with osteoporosis. Bone 39:1268–1275. https://doi.org/10.1016/j.bone.2006.06.007
Miller PD, Hattersley G, Lau E, Fitzpatrick LA, Harris AG, Williams GC, Hu MY, Riis BJ, Russo L, Christiansen C (2019) Bone mineral density response rates are greater in patients treated with abaloparatide compared with those treated with placebo or teriparatide: Results from the ACTIVE phase 3 trial. Bone 120:137–140. https://doi.org/10.1016/j.bone.2018.10.015
Niimi R, Kono T, Nishihara A, Hasegawa M, Kono T, Sudo A (2016) A retrospective analysis of nonresponse to daily teriparatide treatment. Osteoporos Int 27:2845–2853. https://doi.org/10.1007/s00198-016-3581-z
Cosman F, Crittenden DB, Ferrari S, Khan A, Lane NE, Lippuner K, Matsumoto T, Milmont CE, Libanati C, Grauer A (2018) FRAME study: the foundation effect of building bone with 1 year of romosozumab leads to continued lower fracture risk after transition to denosumab. J Bone Miner Res 33:1219–1226. https://doi.org/10.1002/jbmr.3427
Kanda Y (2013) Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant 48:452–458. https://doi.org/10.1038/bmt.2012.244
Ishibashi H, Ishibashi H, Crittenden D, Miyauchi A, Libanati C, Maddox J, Fan M, Chen L, Grauer A et al (2017) Romosozumab increases bone mineral density in postmenopausal Japanese women with osteoporosis: a phase 2 study. Bone (New York, NY) 103:209–215. https://doi.org/10.1016/j.bone.2017.07.005
Takada J, Dinavahi R, Miyauchi A, Hamaya E, Hirama T, Libanati C, Nakamura Y, Milmont CE, Grauer A (2020) Relationship between P1NP, a biochemical marker of bone turnover, and bone mineral density in patients transitioned from alendronate to romosozumab or teriparatide: a post hoc analysis of the STRUCTURE trial. J Bone Miner Metab 38:310–315. https://doi.org/10.1007/s00774-019-01057-1
Ominsky MS, Niu Q-T, Li C, Li X, Ke HZ (2014) Tissue-level mechanisms responsible for the increase in bone formation and bone volume by sclerostin antibody. J Bone Miner Res 29:1424–1430. https://doi.org/10.1002/jbmr.2152
Macdonald HM, Nishiyama KK, Hanley DA, Boyd SK (2011) Changes in trabecular and cortical bone microarchitecture at peripheral sites associated with 18 months of teriparatide therapy in postmenopausal women with osteoporosis. Osteoporos Int 22:357–362. https://doi.org/10.1007/s00198-010-1226-1
Tsujimoto M, Chen P, Miyauchi A, Sowa H, Krege JH (2011) PINP as an aid for monitoring patients treated with teriparatide. Bone 48:798–803. https://doi.org/10.1016/j.bone.2010.12.006
Shimizu T, Arita K, Murota E, Hiratsuka S, Fujita R, Ishizu H, Asano T, Takahashi D, Takahata M, Iwasaki N (2021) Effects after starting or switching from bisphosphonate to romosozumab or denosumab in Japanese postmenopausal patients. J Bone Miner Metab 39:868–875. https://doi.org/10.1007/s00774-021-01226-1
Tominaga A, Wada K, Kato Y, Nishi H, Terayama Y, Okazaki K (2021) Early clinical effects, safety, and appropriate selection of bone markers in romosozumab treatment for osteoporosis patients: a 6-month study. Osteoporos Int 32:653–661. https://doi.org/10.1007/s00198-020-05639-y
Acknowledgements
The authors would like to thank Enago (www.enago.com) for the manuscript review and editing support.
Funding
This work was partly supported by a research grant from Tokyo Women’s Medical University Career Development Center for Medical Professionals.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Ayako Tominaga, Ken Okazaki, Hideharu Nishi, Yasushi Terayama, Shuji Shimamoto, Yasuteru Kodama, and Yoshiharu Kato declare that they have no conflicts of interest. Keiji Wada received a speaking fee from Amgen Inc.
Ethical approval
The procedures complied with the 1964 Helsinki declaration and its later amendments and were approved by Tokyo Women’s Medical University Ethics Committee, number 5596.
Informed consent
Informed consent was obtained from all participants in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tominaga, A., Wada, K., Okazaki, K. et al. Nonresponder Considerations for Romosozumab Treatment. Calcif Tissue Int 113, 157–165 (2023). https://doi.org/10.1007/s00223-023-01087-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-023-01087-y