Abstract
Patients with type 2 diabetes mellitus (T2DM) have an increased risk of fragility fracture. However, the association between diabetes-related osteoporosis and mortality in T2DM remains unknown. This historical cohort study assessed the endpoint of all-cause mortality in patients with T2DM. According to our hospital record, bone parameters were examined in 797 patients from 1997 to 2009. We excluded 78 because of diseases affecting bone metabolism and could not follow-up 308 patients. Finally, in 411 patients, the associations of bone turnover markers, bone mineral density (BMD), and the prevalence of vertebral fractures with mortality were investigated by Cox regression analyses adjusted for confounding factors. Of 411 patients, 56 died during the follow-up period of almost 7 years. Cox regression analyses showed that reduced BMD at the lumbar spine (LS) and femoral neck (FN) (T-score ≤ −2.5) and severe vertebral fractures were associated with higher mortality (hazard ratio [HR] 3.25, 95% confidence interval [CI] 1.48–7.16, p = 0.003 for LS-T score ≤ −2.5; HR 5.19, 95% CI 1.83–14.75, p = 0.002 for FN-T score ≤ −2.5; HR 2.93, 95% CI 1.42–6.02, p = 0.004 for multiple vertebral fractures; HR 7.64, 95% CI 2.13–27.42, p = 0.002 for grade 3 vertebral fracture). Separate analysis in men and women showed that decreased serum osteocalcin was associated with mortality in women (HR 3.82, 95% CI 1.01–14.46 per SD decrease, p = 0.048). The present study is the first to show the association of reduced BMD and severe vertebral fractures with increased all-cause mortality in patients with T2DM. Moreover, higher serum osteocalcin was significantly associated with decreased mortality in women with T2DM.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Type 2 diabetes mellitus (T2DM) has become an important problem worldwide due to the rapidly increasing number of patients and its association with high mortality. Previous studies have shown that the presence of T2DM increases the risks of cardiovascular diseases [1], infection [2], and cancer [3], all of which are associated with increased mortality. Indeed, the adjusted relative risk of death was almost twice that in patients with diabetes mellitus compared to that of age-matched controls [4]. On the other hand, accumulating evidence has shown that patients with T2DM have an increased risk of osteoporotic fracture independent of bone mineral density (BMD) [5,6,7]. Because osteoporotic fractures such as hip and vertebral fractures increase mortality in the general population [8, 9], diabetes-related bone fragility may also be associated with mortality in patients with diabetes mellitus. However, no studies have investigated whether bone metabolism or the prevalence of osteoporotic fractures is involved in the mortality of patients with T2DM.
Osteoporosis is generally associated with accelerated bone turnover. Several previous studies showed bone turnover markers to be associated with mortality [10,11,12,13,14]. In patients with hip fractures, higher serum levels of carboxyterminal telopeptide of type 1 collagen (CTX), a marker of bone resorption, were associated with increased all-cause mortality, although a marker of bone formation, serum osteocalcin, was not [13]. Elderly patients with the highest quartiles of both serum CTX and aminoterminal propeptide of type 1 collagen (P1NP), another marker of bone formation, were significantly and independently more likely to die compared with other patients [10]. In contrast, several studies showed a U-shaped association of osteocalcin and CTX with mortality in elderly men aged 79–89 years [14] and patients at high cardiovascular risk referred for coronary angiography [11, 12]. However, there have been no reports on the association between bone turnover markers and mortality in T2DM patients.
Inhibited bone formation and low turnover of bone remodeling have also been suggested to be involved in diabetes-related bone fragility [15]. Several meta-analyses showed significantly lower serum levels of osteocalcin in patients with T2DM compared to those in non-diabetic subjects [16]. Osteocalcin is expressed and produced specifically in osteoblasts and is an endocrine hormone secreted by bone. Previous studies showed that osteocalcin knockout mice displayed obesity and impaired glucose tolerance due to decreased insulin secretion and sensitivity as well as inhibited adipocyte differentiation and adiponectin secretion [17]. In addition, several studies showed that the osteocalcin receptor is expressed in vascular cells [18] and that osteocalcin has beneficial anti-atherogenic effects on endothelial and vascular smooth muscle cells [19, 20]. Indeed, we previously showed that serum osteocalcin levels were associated with insulin sensitivity and secretion [21] and negatively associated with glucose levels, atherosclerosis parameters, and vascular calcification in patients with T2DM [22,23,24]. Therefore, we hypothesized that lower serum osteocalcin levels may be associated with increased mortality in patients with T2DM.
In the present study, we examined the association of bone turnover markers including osteocalcin, BMD, and the presence of vertebral fracture with all-cause mortality in patients with T2DM.
Subjects and Methods
Subjects
This is a historical cohort study investigating the association between bone parameters and the endpoint of all-cause mortality in patients with T2DM. Patients admitted to Shimane University Hospital for T2DM education and treatment from 1997 to 2009 were screened. According to the hospital records, 843 men and 667 women were admitted. We consecutively examined bone parameters in patients with T2DM who admitted to our hospital for the treatment of T2DM except for having malignant diseases, infection, necessity of operation, and other special purposes. Among them, the bone parameters of 441 men and 356 postmenopausal women were evaluated by measurements of bone turnover markers and BMD as well as lateral X-ray examination of the thoracic and lumbar spine (LS) to assess for the presence of vertebral fracture on admission. We excluded 58 men and 20 women with diseases including hyperthyroidism, hyperparathyroidism, hepatic dysfunction, growth hormone deficiency, and acromegaly because these diseases influence bone metabolism. We investigated patient survival or mortality by medical records and telephone surveys from 2013 to 2014, a median follow-up period of 80 and 83 months in men and women, respectively. Unfortunately, we were unable to contact 161 men and 147 women. Finally, 222 men and 189 postmenopausal women with T2DM were included in this study.
Biochemical Measurements
After overnight fasting, blood and urine samples were collected on the second day after admission. Hemoglobin A1c (HbA1c) and serum creatinine levels were measured by standard biochemical methods as previously reported [21,22,23,24,25,26]. HbA1c was determined by high-performance liquid chromatography. HbA1c values were estimated as NGSP (National Glycohemoglobin Standardization Program) equivalent values calculated by the formula: HbA1c (%) = HbA1c (JDS) (Japan Diabetes Society) (%) + 0.4%. Serum total osteocalcin and bone-specific alkaline phosphatase (BAP) levels were measured by radioimmunoassay and enzyme immune assay, respectively. The coefficients of variation (CV) of osteocalcin and BAP measurements were 5.5 and 6.9%, respectively. Urinary N-terminal cross-linked telopeptide of type-I collagen (uNTX) was measured by enzyme-linked immunosorbent assay with CV of 5.7%.
Radiography
Lateral X-ray films of the thoracic and LS were taken at the time of admission. The anterior, central, and posterior heights of each of the 13 vertebral bodies from Th4-L4 were measured. A patient was diagnosed with a vertebral fracture when at least one of the three vertebral height measurements decreased by >20% when compared to the height of the nearest uncompressed vertebral body. Grading of vertebral fracture was performed using Genant semiquantitative criteria [27]. VFs were classified as follows; grade 1, a reduction of 20–25%; grade 2, 25–40%; and grade 3, more than 40%.
BMD values of the LS 2–4, femoral neck (FN), and one-third of the radius (1/3R) were measured by dual-energy X-ray absorptiometry (QDR-4500; Hologic, Waltham, MA, USA). The CV (precision) of measurements of LS-, FN-, and 1/3R-BMD by our methods were 0.9, 1.7, and 1.9%, respectively. T-scores indicate a deviation from the averaged BMD in sex-matched young Japanese normal reference mean, and Z-scores indicate a deviation from the averaged BMD in normal age- and sex-matched Japanese subjects in the standardized normal distribution.
Statistical Analysis
Data were expressed as mean ± standard deviation (SD). When bone turnover markers were examined, we omitted the patients with treatments for osteoporosis. The statistical significance between two groups was determined using Student’s t and χ 2 tests. Kaplan–Meier curves, log-rank tests, and Cox proportional hazard regression analyses were used to estimate the association between bone parameters and the risk of mortality after adjusting for confounding factors. All analyses were performed using StatView (Abacus Concepts, Berkeley, CA, USA). A p < 0.05 was considered statistically significant.
Results
Subject Baseline Characteristics
The patient background characteristics are shown in Table 1; these parameters were compared between male and female subjects. Age, body mass index (BMI), Z-score at FN and 1/3R, and bone turnover markers were significantly lower in men than in women. Serum creatinine levels, absolute BMD, and T-score at all sites, as well as the ratio of the presence of grades 1 and 2 vertebral fractures, were significantly higher in men than in women. We observed 37 and 19 deaths in men and women (cumulative mortality; 16.7 and 10.0%, respectively). The numbers of patients who had been taking insulin, sulfonylurea, metformin, and thiazolidines, respectively, were 41, 83, 32, and 24 men, and 59, 65, 37, and 17 women. A man took bisphosphonate, and 13 and 5 women took bisphosphonate and selective estrogen receptor modulator, respectively.
We then compared various parameters between dead and surviving patients (Table 2). In total, male, and female subjects, the dead patients were significantly older; the BMD, and LS and FN-T scores were significantly lower in dead patients compared with survivors. In the overall subject population, the duration of diabetes, serum creatinine level, and the ratio of multiple and grade 3 vertebral fractures were significantly higher in dead patients than in survivors, while BMI, FN-Z score, and osteocalcin levels were significantly lower in dead patients than in survivors. Among male subjects, serum creatinine levels were significantly higher in dead patients than in survivors, while 1/3R-T score was significantly lower in dead patients than in survivors. Among female subjects, the duration of diabetes, HbA1c level, and the ratio of multiple and grade 3 vertebral fractures were significantly higher in dead patients than in survivors, while 1/3R-BMD and 1/3R-T scores and serum osteocalcin level were significantly lower in dead patients than in survivors.
Association Between Bone Turnover Markers and All-Cause Mortality
We examined the association between bone turnover markers and mortality risk only in those patients who were not treated for osteoporosis (221 men and 171 women). High and low levels of bone turnover markers were established according to the median levels of each marker. The median levels of osteocalcin were 5.3 ng/mL for all subjects, 4.7 ng/mL for men, and 6.5 ng/mL for women. Unadjusted survival analyses indicated that female patients with lower osteocalcin levels had higher mortality than those with higher levels of osteocalcin (p = 0.011) (Fig. 1c), but the association was not significant in the overall population and male subjects (Fig. 1a and b). In contrast, neither BAP nor uNTX was associated with mortality in the total subject population, male, or female subjects (data not shown).
In the Cox regression analysis adjusted for age, HbA1c level, BMI, duration of diabetes, and serum creatinine level, systolic blood pressure, and LDL-cholesterol, serum osteocalcin levels were significantly associated with mortality in female subjects (hazard ratio [HR] 3.82, 95% confidence interval [CI] 1.01–14.46 per SD decrease, p = 0.048), but not the total population or male subjects (Table 3). The association remained significant even after adjusting for LS-BMD (HR 5.84, 95% CI 1.04–32.78, p = 0.045). In contrast, neither BAP nor uNTX were associated with mortality in the total population, male, or female subjects.
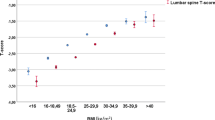
Association Between BMD and All-Cause Mortality
In the total subject population, Cox regression analysis adjusted for age, gender, HbA1c level, BMI, duration of diabetes, serum creatinine level, systolic blood pressure, LDL-cholesterol, and treatment for osteoporosis showed that absolute LS-BMD and FN-BMD were significantly associated with mortality (HR 1.72, 95% CI 1.21–2.45 per SD decrease, p = 0.002 and HR 1.53, 95% CI 1.03–2.27 per SD decrease, p = 0.040) (Table 4). Then, we divided the subjects into three categories, normal (1.0 ≤ T-score), osteopenia (−2.5 < T-score < −1.0), and osteoporosis (T-score ≤ −2.5), according to World Health Organization (WHO) osteoporosis categorization [28]. Unadjusted survival analyses indicated that the total population and female subjects with LS-T scores ≤ −2.5 had higher mortality compared with those with normal LS-T scores (p < 0.001 and p < 0.001), and that the total population, male, and female subjects with FN-T scores ≤ −2.5 had higher mortality compared with those with normal FN-T scores (p < 0.001, p < 0.001, and p = 0.033, respectively) (Fig. 2). Moreover, Cox regression analysis adjusted for age, gender, HbA1c level, BMI, duration of diabetes, and serum creatinine level, systolic blood pressure, LDL-cholesterol, and treatment for osteoporosis revealed that LS-T score ≤ −2.5 or FN-T score ≤ −2.5 were significantly and positively associated with mortality in the total subjects (HR 3.25, 95% CI 1.48–7.16, p = 0.003 and HR 5.19, 95% CI 1.83–14.75, p = 0.002, respectively). In contrast, 1/3R-BMD was not associated with mortality in the unadjusted survival analyses (data not shown) and adjusted Cox regression.
In men, the adjusted Cox regression analyses showed that FN-T score ≤ −2.5 was significantly associated with mortality (HR 7.15, 95% CI 1.95–26.18, p = 0.003), and absolute FN-BMD was tended to be associated with mortality (HR 1.50, 95% CI 0.97–2.32 per SD decrease, p = 0.069). In contrast, neither BMD nor T-score at LS, FN, and 1/3R categories were associated with mortality in women in adjusted Cox regression analyses.
Association Between Vertebral Fractures and All-Cause Mortality
Finally, we examined the association between the severity of vertebral fracture and mortality. Unadjusted survival analyses indicated that patients with multiple vertebral fractures had higher mortality compared with those without vertebral fractures in the total population and female subjects (p < 0.001 and p < 0.001, respectively) (Fig. 3a, c), but not male subjects (Fig. 3b). Moreover, patients with grade 3 vertebral fracture had higher mortality compared with those without vertebral fractures in the total population and female subjects (p = 0.002 and p < 0.001, respectively) (Fig. 3d, f). In Cox regression analysis adjusted for age, gender, HbA1c level, BMI, duration of diabetes, serum creatinine level, systolic blood pressure, LDL-cholesterol, and treatment for osteoporosis, multiple vertebral fractures were significantly and positively associated with mortality in the total population (HR 2.93, 95% CI 1.42–6.02, p = 0.004) (Table 5). Cox regression analysis adjusted for the confounding factors described above revealed grade 3 vertebral fracture to be significantly and positively associated with mortality in the total subjects (HR 7.64, 95% CI 2.13–27.42, p = 0.002) (Table 5). Furthermore, the association remained significant even after adjusting for LS-BMD, FN-BMD, and 1/3R-BMD (HR 6.89, 95% CI 1.93–24.54, p = 0.003, HR 5.39, 95% CI 1.43–20.33, p = 0.013, and HR 6.87, 95% CI 1.82–26.01, p = 0.005, respectively).
Discussion
Several studies have examined the association of serum osteocalcin levels with mortality. Gulin et al. showed that serum osteocalcin levels were not associated with one-year all-cause mortality in 236 patients (59 males) with hip fracture, although high levels of a bone resorption marker were significantly associated with mortality [13]. However, Lerchbaum et al. showed a U-shaped association of serum osteocalcin with all-cause mortality in men and women referred for coronary angiography [11, 12]. Yeap et al. also reported that the highest and lowest quintiles of serum osteocalcin levels showed a significant increase in all-cause mortality in older men aged 70–89 years [14]. These findings suggest that higher and lower levels of serum osteocalcin may be associated with mortality in elderly subjects at high cardiovascular risk. Although the underlying mechanism of the association between osteocalcin and mortality risk is unclear, the association appears to depend on the background characteristics. However, no studies have examined the effects of serum osteocalcin level on mortality risk in patients with T2DM. To our knowledge, the present study is the first to show that lower serum osteocalcin levels were associated with higher risk of all-cause mortality in postmenopausal women with T2DM. Moreover, the association between osteocalcin level and the mortality rate was significant even after adjusting for BMD, suggesting that the effects of osteocalcin on mortality risk are independent of bone mass.
Although we tested the association of osteocalcin tertile with mortality in female subjects, we did not observe a U-shaped association of serum osteocalcin with mortality (data not shown). As previous studies have shown lower serum osteocalcin levels in T2DM than in persons without T2DM [16], the serum osteocalcin levels of the participants in the current study were lower compared with those in previous studies [11, 12, 14]. This may explain the differences in association curves between previous studies and ours. Furthermore, the previous studies did not examine bone formation markers other than serum osteocalcin. The present study observed no association between BAP or uNTX and mortality; therefore, osteocalcin may play important roles in T2DM independently of bone formation and turnover.
Since previous studies have reported different effects of osteocalcin on sex hormones [29, 30], analysis of the results of clinical studies on osteocalcin and mortality should separately consider men and women in order to avoid such sex-related differences. The findings of the current study suggest that serum osteocalcin may play important roles in the prognosis of women with T2DM. In contrast, serum osteocalcin was not associated with mortality risk in men with T2DM. Thus, there may be sex differences in the association in patients with T2DM. There are no clear reasons why serum osteocalcin was not associated with the risk of mortality in men with T2DM in this study. Other researchers and we previously showed serum osteocalcin to be positively associated with serum adiponectin in women, but not men [26, 31, 32]. As adiponectin has anti-diabetic, anti-atherogenic, and anti-tumor effects [31,32,33,34,35], the effects of osteocalcin on adiponectin expression may be more significant in female patients with T2DM. Moreover, previous studies have shown that osteocalcin enhances testosterone secretion from Leydig cells in men [29]. Indeed, we previously reported a significant positive association between serum osteocalcin and free testosterone levels in men with T2DM [36]. However, it has no effect on estrogen expression because ovaries lack its receptor. Differences in the effects of osteocalcin on sex hormones may be another possible explanation. However, to determine the association between osteocalcin and mortality in patients with T2DM, it is necessary to perform further large-scale studies.
On the other hand, we found that the reduction in BMD was a significant predictor of the risk of mortality in patients with T2DM, especially in men. Although patients with T2DM show no BMD reduction, there is an increased risk of hip fracture [6, 7]. These findings suggest that deterioration of bone quality is an important factor in the etiology of diabetes-related bone fragility. Therefore, T2DM patients with both impaired bone quality as well as decreased BMD may be at extremely high risk of fracture. FN-BMD may be more accurate, especially in elderly patients compared to LS-BMD because of the lack of accuracy in systematic measurements due to irregularities in the spinal elements. In addition, a higher frequency of arterial calcification in the aorta could directly interfere with BMD acquisition in the LS, especially in patients at high risk of cardiovascular diseases such as those with T2DM. Indeed, atherosclerosis parameters are negatively associated with FN-BMD, but not LS-BMD, in men with T2DM [37]. Therefore, the WHO did not recommend the measurement of LS-BMD when developing the absolute risk score for osteoporotic fractures [38]. The results of the present study suggest that measurement of FN-BMD may be more accurate than that of LS-BMD for assessing mortality risk in patients with T2DM. Although it is unknown why the association between FN-BMD and mortality is more pronounced in men, there may exist sex differences. Because previous studies have shown that the increased mortality after hip fractures is more prominent in men than in women [39, 40], lower FN-BMD was significantly associated with mortality in men in this study. However, further studies are needed to clarify the sex differences.
Previous studies have shown that vertebral fracture increases mortality [39]. We previously demonstrated an increased risk of vertebral fracture in patients with T2DM [7]. The present study revealed that the presence of severe vertebral fractures such as multiple and grade 3 fractures is associated with increased mortality in patients with T2DM independent of age, duration of diabetes, HbA1c levels, BMI, and renal function. In addition, the association between grade 3 vertebral fracture and mortality remained significant after additional adjustment for BMD. Therefore, vertebral fracture independent of diabetic status and associated with impaired bone quality may be involved in the increased mortality observed in patients with T2DM.
The present study had several limitations. First, the sample size was not large enough to make definite conclusions. Second, we analyzed only those subjects who visited Shimane University Hospital, a tertiary center for evaluation or treatment of T2DM. Therefore, the patients enrolled in this study might have relatively severe disease. Third, we could not follow up several patients. Some patients lost to follow-up may have died. Fourth, non-diabetic control subjects were not examined in this study. Thus, we cannot compare the contribution of BMD reduction, low osteocalcin level, and the presence of vertebral fracture to the mortality between T2DM and non-diabetics. Fifth, the information regarding the treatments for osteoporosis and diabetes was not available in this study. Sixth, we diagnosed vertebral fracture according to height-based criteria [27] in this study. Therefore, grade 1 deformities might be non-fractural in their etiology. We performed subgroup analysis about the association between the number of grade 1 fractures and mortality after excluding the patients with grade 2 and 3. Cox proportional hazard regression analyses adjusting for confounding factors (model 5) showed a significant association of multiple grade 1 fractures with all-cause mortality in total subjects (HR 5.65, 95% CI 1.51–21.19, p = 0.010). Finally, we could not analyze the causes of death such as cardiovascular, infection, and malignant diseases. In conclusion, we found for the first time that lower serum osteocalcin levels, reduced BMD, and severe vertebral fractures were associated with increased all-cause mortality in patients with T2DM. Moreover, higher serum osteocalcin was significantly associated with decreased mortality in women with T2DM. Because this is a historical cohort study, there are several limitations such as limited sample size and loss to follow-up. Thus, further large-scale longitudinal studies are necessary.
Abbreviations
- T2DM:
-
Type 2 diabetes mellitus
- BMD:
-
Bone mineral density
- CTX:
-
Carboxyterminal telopeptide of type 1 collagen
- P1NP:
-
Aminoterminal propeptide of type 1 collagen
- BAP:
-
Bone-specific alkaline phosphatase
- uNTX:
-
Urinary N-terminal cross-linked telopeptide of type-I collagen
- CV:
-
Coefficients of variation
- HbA1c:
-
Hemoglobin A1c
- LS:
-
Lumbar spine
- FN:
-
Femoral neck
- 1/3R:
-
One-third of the radius
- SD:
-
Standard deviation
- HR:
-
Hazard ratio
- 95% CI:
-
95% confidence interval
- BMI:
-
Body mass index
References
Matheus AS, Tannus LR, Cobas RA, Palma CC, Negrato CA, Gomes MB (2013) Impact of diabetes on cardiovascular disease: an update. Int J Hypertens 2013:653789
Fisher-Hoch SP, Mathews CE, McCormick JB (2013) Obesity, diabetes and pneumonia: the menacing interface of non-communicable and infectious diseases. Trop Med Int Health 18:1510–1519
Gallagher EJ, LeRoith D (2015) Obesity and diabetes: the increased risk of cancer and cancer-related mortality. Physiol Rev 95:727–748
Almdal T, Scharling H, Jensen JS, Vestergaad H (2004) The independent effect of type 2 diabetes mellitus on ischemic heart disease, stroke, and death: a population-based study of 13,000 men and women with 20 years of follow-up. Arch Intern Med 164:1422–1426
Barret-Connor E, Holbrook TL (1992) Sex differences in osteoporosis in older adults with non-insulin-dependent diabetes mellitus. JAMA 268:3333–3337
Vestergaard P (2007) Discrepancies in bone mineral density and fracture risk in patients with type 1 and type 2 diabetes-a meta-analysis. Osteoporos Int 18:427–444
Yamamoto M, Yamaguchi T, Yamauchi M, Kaji H, Sugimoto T (2009) Diabetic patients have an increased risk of vertebral fractures independent of bone mineral density or diabetic complications. J Bone Miner Res 24:702–709
Haentjens P, Magaziner J, Colon-Emeric CS, Vanderschueren D, Milisen K, Velkeniers B, Boonen S (2010) Meta-analysis: excess mortality after hip fracture among older women and men. Ann Intern Med 152:380–390
Ensrund KE, Thompson DE, Cauley JA, Nevitt MC, Kado DM, Hochberg MC, Santora AC 2nd, Black DM (2009) Prevalent vertebral deformities predict mortality and hospitalization in older women with low bone mass. J Am Geriatr Soc 48:241–249
Sambrook PN, Chen CJ, March L, Cameron ID, Cumming RG, Lord SR, Simpson JM, Seibel MJ (2006) High bone turnover is an independent predictor of mortality in the frail elderly. J Bone Miner Res 21:549–555
Lerchbaum E, Schwetx V, Pilz S, Grammer TB, Look M, Boehm BO, Obermayer-Pietsch B, März W (2012) Association of bone turnover markers with mortality in men referred to coronary angiography. Osteoporos Int 24:1321–1332
Lerchbaum E, Schwetz V, Pilz S, Boehm BO, März W (2014) Association of bone turnover markers with mortality in women referred to coronary angiography: the Ludwigshafen Risk and Cardiovascular Health (LURIC) study. Osteoporos Int 25:455–465
Gulin T, Kruljac I, Kirigin L, Merc M, Pavic M, Trcin MT, Bokulic A, Megla ZB, Kastelan D (2016) Advanced age, high & #x03B2;-CTX levels, and impaired renal function are independent risk factors for all-cause one-year mortality in hip fracture patients. Calcif Tissue Int 98:67–75
Yeap BB, Chubb SA, Flicker L, McCaul KA, Ebeling PR, Hankey GJ, Beilby JP, Norman PE (2012) Associations of total osteocalcin with all-cause and cardiovascular mortality in older men: the Health In Men Study. Osteoporos Int 23:599–606
Saito M, Fujii K, Mori Y, Marumo K (2006) Role of collagen enzymatic and glycation induced cross-links as a determinant of bone quality in spontaneously diabetic WBN/Kob rats. Osteoporos Int 17:1514–1523
Liu C, Wo J, Zhao Q, Wang Y, Wang B, Zhao W (2015) Association between serum total osteocalcin level and type 2 diabetes mellitus: a systematic review and meta-analysis. Horm Metab Res 47:813–819
Lee NK, Sowa H, Hinoi E, Ferron M, Ahn JD, Confavreux C, Dacquin R, Mee PJ, McKee MD, Jung DY, Zhang Z, Kim JK, Mauvais-Jarvis F, Ducy P, Karsenty G (2007) Endocrine regulation of energy metabolism by the skeleton. Cell 130:456–469
Pi M, Quarles LD (2012) Multiligand specificity and wide tissue expression of GPRC6A reveals new endocrine networks. Endocrinology 153:2062–2069
Jung CH, Lee WJ, Hwang JY, Lee MJ, Seol SM, Kim YM, Lee YL, Park JY (2013) The preventive effect of uncarboxylated osteocalcin against free fatty acid-induced endothelial apoptosis through the activation of phosphatidylinositol 3-kinase/Akt signaling pathway. Metabolism 62:1250–1257
Zhou B, Li H, Liu J, Xu L, Zang W, Wu S, Sun H (2013) Intermittent injections of osteocalcin reverse autophagic dysfunction and endoplasmic reticulum stress resulting from diet-induced obesity in the vascular tissue via the NFκB-p65-dependent mechanism. Cell Cycle 12:1901–1903
Kanazawa I, Yamaguchi T, Tada Y, Yamauchi M, Yano S, Sugimoto T (2011) Serum osteocalcin level is positively associated with insulin sensitivity and secretion in patients with type 2 diabetes. Bone 48:720–725
Kanazawa I, Yamaguchi T, Yamamoto M, Yamauchi M, Kurioka S, Yano S, Sugimoto T (2009) Serum osteocalcin level is associated with glucose metabolism and atherosclerosis parameters in type 2 diabetes mellitus. J Clin Endocrinol Metab 94:45–49
Ogawa-Furuya N, Yamaguchi T, Yamamoto M, Kanazawa I, Sugimoto T (2013) Serum osteocalcin levels are inversely associated with abdominal aortic calcification in men with type 2 diabetes mellitus. Osteoporos Int 24:2223–2230
Kanazawa I, Yamaguchi T, Yamauchi M, Yamamoto M, Kurioka S, Yano S, Sugimoto T (2011) Serum undercarboxylated osteocalcin was inversely associated with plasma glucose level and fat mass in type 2 diabetes mellitus. Osteoporos Int 22:187–194
Kanazawa I, Yamaguchi T, Yamamoto M, Yamauchi M, Yano S, Sugimoto T (2009) Adiponectin is associated with changes in bone markers during glycemic control in type 2 diabetes mellitus. J Clin Endocrinol Metab 94:3031–3037
Kanazawa I, Yamaguchi T, Yamamoto M, Yamauchi M, Yano S, Sugimoto T (2009) Relationships between serum adiponectin levels versus bone mineral density, bone metabolic markers, and vertebral fractures in type 2 diabetes mellitus. Eur J Endocrinol 160:265–273
Genant HK, Wu CY, van Kuijk C, Nevitt MC (1993) Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 8:1137–1148
Report of a WHO Study Group (1994) Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. World Health Organ Tech Rep Ser 843:1–129
Oury F, Sumara G, Sumara O, Ferron M, Chang H, Smith CE, Hermo L, Suarez S, Roth BL, Ducy P, Karsenty G (2011) Endocrine regulation of male fertility by the skeleton. Cell 144:796–809
Karsenty G, Oury F (2014) Regulation of male fertility by the bone-derived hormone osteocalcin. Mol Cell Endocrinol 382:521–526
Richards JB, Valdes AM, Burling K, Perks UC, Spector TD (2007) Serum adiponectin and bone mineral density in women. J Clin Endocrinol Metab 92:1517–1523
Oh KW, Lee WY, Rhee EJ, Baek KH, Yoon KH, Kang MI, Yun EJ, Park CY, Ihm SH, Choi MG, Yoo HJ, Park SW (2005) The relationship between serum resistin, leptin, adiponectin, ghrelin levels and bone mineral density in middle-aged men. Clin Endocrinol 63:131–138
Kadowaki T, Yamauchi T (2005) Adiponectin and adiponectin receptors. Endocr Rev 26:439–451
Yamauchi T, Hara K, Kubota N, Terauchi Y, Tobe K, Froguel P, Nagai R, Kadowaki T (2003) Dual roles of adiponectin/Acrp30 in vivo as an anti-diabetic and anti-atherogenic adipokine. Curr Drug Targets Immune Endocr Metabol Disord 3:243–254
Dalamaga M, Diakopoulos KN, Mantzoros CS (2012) The role of adiponectin in cancer: a review of current evidence. Endocr Rev 33:547–594
Kanazawa I, Tanaka K, Ogawa N, Yamauchi M, Yamaguchi T, Sugimoto T (2013) Undercarboxylated osteocalcin is positively associated with free testosterone in male patients with type 2 diabetes mellitus. Osteoporos Int 24:1115–1119
De Almeida Pereira Coutinho M, Bandeira E, de Almeida JM, Godoi ET, Vasconcelos G, Bandeira F (2013) Low bone mass is associated with increased carotid intima media thickness in men with type 2 diabetes mellitus. Clin Med Insights Endocrinol Diabetes 6:1–6
Kanis JA, McCloskey EV, Johansson H, Strom O, Borqstrom F, Oden A, National Osteoporosis Guideline Group (2008) Case finding for the management of osteoporosis with FRAX–assessment and intervention thresholds for the UK. Osteoporos Int 19:1395–1408
Center JR, Nguyen TV, Schneider D, Sambrook PN, Eisman JA (1999) Mortality after all major types of osteoporotic fracture in men and women an observational study. Lancet 353:878–882
Klop C, van Staa TP, Cooper C, Harvey NC, de Vries F (2017) The epidemiology of mortality after fracture in England: variation by age, sex, time, geographic location, and ethnicity. Osteoporos Int 28:161–168
Acknowledgements
The authors thank the patients and staff of Shimane University Faculty of Medicine who participated in this study. This study had no funding support. All authors participated in the development and writing of the article and approved the final manuscript for publication. IK takes full responsibility for the content of the article.
Author information
Authors and Affiliations
Contributions
HM researched data and wrote manuscript. IK researched data and wrote/reviewed/edited manuscript. TS contributed to discussion and reviewed/edited manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
Hitomi Miyake, Ippei Kanazawa, and Toshitsugu Sugimoto declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This study was approved by the institutional review board of Shimane University Faculty of Medicine; the requirement for informed patient consent was waived because no intervention and further examinations were performed.
Additional information
This manuscript has not been published and is not under consideration for publication elsewhere.
Rights and permissions
About this article
Cite this article
Miyake, H., Kanazawa, I. & Sugimoto, T. Association of Bone Mineral Density, Bone Turnover Markers, and Vertebral Fractures with All-Cause Mortality in Type 2 Diabetes Mellitus. Calcif Tissue Int 102, 1–13 (2018). https://doi.org/10.1007/s00223-017-0324-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-017-0324-x