Abstract
Greater body mass index (BMI) is associated with a greater risk of osteoarthritis (OA). This study sought to investigate whether the association is mediated by fat mass or lean mass. The study involved 170 men and 488 women aged between 20 and 90 (average age: 55) who were randomly recruited from Ho Chi Minh City, Vietnam. The presence of knee OA was radiographically diagnosed based on the Kellgren–Lawrence criteria. Lean mass (LM) and fat mass (FM) were obtained from the DXA whole body scan (Hologic QDR-4500). The relationship between OA, LM, and FM was analyzed by a series of multiple linear regression models which take into account the effects of gender and age. As expected, men and women with knee OA were older than those without OA (65 vs 51 year in men, and 64 vs 52 year in women). After adjusting for age, OA was associated with greater FM and percent body fat (PBF), but the association was only observed in women, not in men. There was no statistically significant difference in LM between OA and non-OA individuals. Moreover, after adjusting for age and BMI or PBF, bone density in OA patients was not significantly different from non-OA individuals. Women with OA of the knee have greater fat mass than non-OA individuals, and that there is no significant difference in bone density between OA and non-OA individuals. Thus, the association between body mass index and OA is mainly mediated by fat mass.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoarthritis (OA) is a common skeletal disorder in the general population. Approximately 10 % of men and 20 % of women of Caucasian background have symptomatic OA [1]. However, the prevalence of (asymptomatic) radiographic OA is higher, with estimates ranging between 27 and 80 % [2]. A recent analysis of data from the National Health and Nutrition Examination Survey III (NHANES III) found that approximately 35 % of women and men aged 60 years and above had radiographic OA of the knee [3]. We have undertaken a study of the Vietnamese population, and found that approximately 31 % of men and 35 % of women have evidence of radiographic OA of the knee [4]. With the rapid aging of population, it is expected that the prevalence of OA in the general community will impose a significant public health burden in the future.
The etiology of OA of the knee is complex, and several risk factors have been identified to be associated with the disease. High BMI is a well-known risk factor for both the onset [5–7] and progression of OA [8, 9]. However, BMI cannot distinguish between whole body lean mass and fat mass, and which of the two components is related to OA risk is not known. Some studies have found that high BMD is also associated with a greater risk of OA at the knee and hip [10–12]. However, BMD is associated with BMI or body fat mass, and it is not clear whether the association between BMD and OA is mediated through fat mass.
We hypothesized that individuals with OA of the knee have greater whole body fat mass, not lean mass, than individuals without OA. In this study, we sought to test the hypothesis by determining the relationship between body composition parameters, bone density, and the risk of OA of the knee in a group of well-characterized individuals.
Study Design and Methods
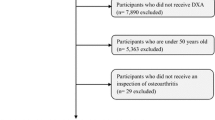
The study was designed as a cross-sectional investigation, with the setting being Ho Chi Minh City, a major city in Vietnam. The study procedure and protocol of data collection have been described previously [4]. Briefly, we approached community organizations, including church and temples, and obtained the list of members aged 18 years and above. In the next step, we used a computer program to randomly select individuals in the list. We used simple random sampling technique to identify potential participants. We sent a letter of invitation to the selected individuals. Some participants (approximately 5 %) did not respond to our letter of invitation, and we contacted them via phone. The participants did not receive any financial incentive, but they received a free health check-up and lipid analyses. Participants were excluded from the study if they had rheumatoid arthritis. In this report, we included participants aged 40 years and older because OA of the knee mainly affects people in that age range [13].
Based on the previous literature, we assumed that the prevalence of knee OA is around 30 %, and with a marginal error of 5 %, we estimated that a sample size of 323 individuals would be required to have an 80 % chance to detect the prevalence.
Data Collection
All participants underwent a detailed investigation to obtain the following baseline data: a standardized interview gathered information on demographic data, lifestyle, and nutritional status. Anthropometric parameters including age, weight, standing height were obtained. Body weight was measured on an electronic scale with indoor clothing without shoes. Height was determined without shoes on a portable stadiometer with mandible plane parallel to the floor. Body mass index (BMI) was calculated as weight in kg over height in meter squared.
Each participant was asked to provide information on current and past smoking habits. Smoking was quantified in terms of the number of pack-years consumed in each ten-year interval age group. Alcohol intake in average numbers of standard drinks per day, at present as well as within the last 5 years, was obtained. Clinical data including blood pressure, pulse, and reproductive history (i.e., parity, age of menarche, and age of menopause), medical history (i.e., previous fracture, previous and current use of pharmacological therapies) were also obtained. The interview was conducted by the research team which included doctors and nurses who were completely blind to radiographs.
Assessment of OA
Knee radiographs were taken using semi-flexed with the participant standing, using the General Electric radiographic equipment (General Electric Medical Systems, Milwaukee, WI) and Kodak film. The ascertainment of OA was based on radiographic assessment using the Kellgren–Lawrence scoring system which is recommended by the WHO as a standard method for studying OA in epidemiologic studies [14]. Anterior-posterior radiographs of both knees were taken from all participants. Radiographs were read by a single rheumatologist (LHP) who was completely unaware of the clinical conditions of participants. In each knee, the presence or absence of osteophytes, joint space narrowing, sclerosis, and cysts was examined for each hand joint using the Kellgren–Lawrence system of scoring: 0 = none, 1 = possible osteophytes only, 2 = definite osteophytes and possible joint space narrowing, and 4 = large osteophytes, severe joint space narrowing, and/or bony sclerosis. The presence of radiographic OA was defined if the grade was 2 or more in at least one joint.
Measurement of Body Composition and Bone Density
Body composition, including lean mass, fat mass, and bone mineral density, was measured by the dual energy X-ray absorptiometry densitometer (Hologic QDR 4500, Hologic, Inc., Waltham, Massachusetts). BMD was measured at the lumbar spine, femoral neck, and whole body. The densitometer was standardized by a standard phantom before each measurement was undertaken. Fat mass was expressed as percentage of body weight to derive the “traditional” PBF. In addition, we derived the lean mass index (LMI) as the ratio of lean mass (in kg) over the squared body height (in m2).
Data Analysis
We conducted both descriptive and inferential analyses according to a pre-conceived plan. In the descriptive analysis, we computed mean and standard deviation for each continuous variable by OA status. The difference between OA patients and non-OA participants was tested by the unpaired t test for normally distributed data or Chi-square test for categorical data. In addition, we used the analysis of covariance (ANCOVA) model to test the hypothesis of equivalence in body composition between OA and non-OA participants. In this ANCOVA model, body composition parameters were considered outcomes, and age was considered the covariate.
In the logistic regression analysis, the presence or absence of OA was considered the outcome variable, while age, fat mass, and lean mass were independent predictors. We considered three alternative models: model I includes age, fat mass, and lean mass; model II includes age, percent body fat, and lean mass index; and model III includes age and body mass index. The strength of association between each predictor and OA risk was estimated by the odds ratio (OR) with 95 % confidence interval per unit increase in each variable. The statistical significance of each predictor was assessed by the standard likelihood-ratio test, which compares the deviance of the predictor with that of the null model on a Chi-squared distribution. In addition, we assessed the model discrimination by computing the c-statistic which is can be interpreted as area under of the receiver operating characteristic curve. All analyses were done with the R statistical environment [15].
Results
As reported previously, the prevalence of radiographic OA of the knee in this population was 32 % (n = 53/170) in men and 36 % (n = 176/488) in women [4]. Basic clinical and demographic characteristics of participants classified by OA status are shown in Table 1. As expected, men and women with OA were older than those without OA. In men, there was no statistically significant difference in BMI and fat mass between OA and non-OA group. However, in women, the OA group had statistically greater BMI, fat mass, and percent body fat than the non-OA group. There was no statistically significant difference in lean mass between OA and non-OA group.
Bone Mineral Density and Osteoarthritis
In univariate analysis, individuals with OA had significantly lower lumbar spine and femoral neck BMD than non-OA individuals, and the difference was around 0.06 g/cm2 (Table 1). However, after adjusting for age, the difference in BMD between OA and non-OA individuals was no longer statistically significant for both men and women. The result remained virtually unchanged after adjustment for fat mass or percent body fat.
Body Composition and Osteoarthritis
The relationship between body composition and OA of the knee was gender dependent. In women, for any given age, those with OA of the knee had greater fat mass (Fig. 1), greater percent body fat, and greater lean mass or lean mass index than those without OA. The age-adjusted difference in fat mass was 1.8 kg (95 % CI 0.8–2.7 kg), slightly higher than the age-adjusted difference in lean mass (1.1 kg; 95 % CI 0.2–1.8 kg) (Table 2). In men, although individuals with OA of the knee also had greater fat mass and lean mass than those without OA, the difference did not reach a statistical significance.
In the logistic regression model (Table 3), increased odds of OA in women was significantly associated with greater fat mass and advancing age. However, when fat mass was replaced with the percent body fat, and lean mass was replaced with the lean mass index (model II), both percent body fat and lean mass index were significant associated with OA. Moreover, in model III, both age and body mass index were significantly associated with OA. The c-index of the three models was approximately 0.80 (Fig. 2).
When the three logistic regression models were applied in men, only age was a significant predictor of OA. Fat mass, percent body fat, lean mass, lean mass index, and body mass index were not statistically associated with OA.
Discussion
While it has been well established that OA patients have a greater body weight or body mass index than non-OA individuals, it has not been clear whether this difference is due to lean mass and fat mass. In this study, we have demonstrated that in women, the risk of knee OA was associated with greater whole body fat mass, but not lean mass; interestingly, in men neither fat mass or lean mass was associated with OA of the knee. Moreover, OA and non-OA individuals have similar age-adjusted BMD. These findings deserve further elaboration.
Few studies have examined the association between body composition and OA of the knee [16–19]. However, our finding of association between fat mass and OA of the knee confirms a previous observation that knee OA patients had greater fat mass than non-OA people [20]. In our study, the magnitude of association between fat mass or height-adjusted lean mass and OA is higher than the magnitude of association between BMI and OA. It is interesting to note that all three models, with different ways to express fat mass and lean mass, showed virtually the same index of discrimination (~0.80). This suggests that in terms of prediction, body composition parameters and body mass index yield similar predictive value. However, BMI has more practical value than fat mass or lean mass, since the former is an easy and inexpensive way to measure obesity.
In this study, we found that the effect of fat mass on knee OA was more apparent in women than in men, and this is consistent with previous observation for BMI [21]. The mechanism of association between fat mass and OA is not clear, but it appears that the association may be explained by metabolic factors [22, 23]. Another hypothesis related to mechanical factor can also be put forward to explain the association. Greater body fat results in an increased in force and stress that joints are subjected to which could cause cartilage breakdown and osteoarthritis [24].
The relationship between BMD and OA has been controversial. The Framingham Study found that among women, femoral neck BMD in knee OA patients was greater than those without OA [25]; however, the association was not adjusted for fat mass. Greater BMD was also a risk factor for incidence of knee OA [26]. A study in Japanese population found that in women osteoporosis (e.g., low BMD) was associated with reduced risk of OA [27]. However, in our study, after adjusting for age and fat mass, there was no significant association between BMD and knee OA. This non-significant association can be seen by the substantial overlap in the distribution of BMD between OA and non-OA group. The main difference between our finding and previous findings are that we have adjusted for fat mass, whereas previous studies did not adjust for fat mass or BMI.
The present results have to be interpreted within the context of strengths and potential limitations. The study was based on a reasonably large sample size, and the participants were randomly selected using a rigorous random sampling technique to ensure the representativeness of the general population. The study population is highly homogeneous, which reduces the effects of potential confounders that could compromise the estimates. Nevertheless, the participants in this study were sampled from an urban population; as a result, the study’s finding may not be generalizable to the rural populations. Because we excluded individuals with diseases deemed to interfere with bone metabolism, the prevalence of knee OA reported here could be an underestimate of the true prevalence in the general population. Moreover, the Kellgren–Lawrence method may not be as sensitive and accurate as the MRI technique in the diagnosis of knee OA. Finally, the study was observational, and no causal inference could be made from the association between BMD or fat mass and OA.
Nevertheless, our findings have important implication in clinical practice and public health relevance. The fact that higher body fat mass is a risk factor for OA of the knee underlines that obesity imposes healthcare burden beyond metabolic disorders but also skeletal disorders. Obesity is increasingly becoming a public health problem, not just in industrialized countries, but also in developing countries in Asia. Thus, given the fat–OA association, it is expected that the prevalence of OA in Asian populations will also be increased in the near future.
In summary, these data suggest that in women, elevated whole body fat mass, not lean mass, is a risk factor for OA of the knee, and that there is no difference in BMD between individuals with radiographic knee OA and those without OA.
References
March LM, Schwarz JM, Carfrae BH, Bagge E (1998) Clinical validation of self-reported osteoarthritis. Osteoarthr Cartil 6:87–93
Lawrence RC, Felson DT, Helmick CG, Arnold LM, Choi H et al (2008) Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum 58:26–35
Nguyen US, Zhang Y, Zhu Y, Niu J, Zhang B et al (2011) Increasing prevalence of knee pain and symptomatic knee osteoarthritis: survey and cohort data. Ann Intern Med 155:725–732
Ho-Pham LT, Lai TQ, Mai LD, Doan MC, Pham HN et al (2014) Prevalence of radiographic osteoarthritis of the knee and its relationship to self-reported pain. PLoS One 9:e94563
Felson DT, Zhang Y (1998) An update on the epidemiology of knee and hip osteoarthritis with a view to prevention. Arthritis Rheum 41:1343–1355
Felson DT, Zhang Y, Hannan MT, Naimark A, Weissman B et al (1997) Risk factors for incident radiographic knee osteoarthritis in the elderly: the Framingham Study. Arthritis Rheum 40:728–733
Manninen P, Riihimaki H, Heliovaara M, Makela P (1996) Overweight, gender and knee osteoarthritis. Int J Obes Relat Metab Disord 20:595–597
Felson DT, Goggins J, Niu J, Zhang Y, Hunter DJ (2004) The effect of body weight on progression of knee osteoarthritis is dependent on alignment. Arthritis Rheum 50:3904–3909
Spector TD, Hart DJ, Doyle DV (1994) Incidence and progression of osteoarthritis in women with unilateral knee disease in the general population: the effect of obesity. Ann Rheum Dis 53:565–568
Nevitt MC, Zhang Y, Javaid MK, Neogi T, Curtis JR et al (2010) High systemic bone mineral density increases the risk of incident knee OA and joint space narrowing, but not radiographic progression of existing knee OA: the MOST study. Ann Rheum Dis 69:163–168
Hart DJ, Cronin C, Daniels M, Worthy T, Doyle DV et al (2002) The relationship of bone density and fracture to incident and progressive radiographic osteoarthritis of the knee: the Chingford Study. Arthritis Rheum 46:92–99
Nevitt MC, Lane NE, Scott JC, Hochberg MC, Pressman AR et al (1995) Radiographic osteoarthritis of the hip and bone mineral density. The Study of Osteoporotic Fractures Research Group. Arthritis Rheum 38:907–916
Thiem U, Lamsfuß R, Gunther S, Schumacher J, Baker C et al (2013) Prevalence of self-reported pain, joint complaints and knee or hip complaints in adults aged ≥40 years: a cross-sectional survey in Herne, Germany. PLoS One 8:e60753
Litwic A, Edwards MH, Dennison EM, Cooper C (2013) Epidemiology and burden of osteoarthritis. Br Med Bull 105:185–199
R Development Core Team (2008) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna. http://www.R-project.org
Segal NA, Findlay C, Wang K, Torner JC, Nevitt MC (2012) The longitudinal relationship between thigh muscle mass and the development of knee osteoarthritis. Osteoarthr Cartil 20:1534–1540
Blumenfeld O, Williams FM, Hart DJ, Arden NK, Spector TD et al (2013) Lower limbs composition and radiographic knee osteoarthritis (RKOA) in Chingford sample—a longitudinal study. Arch Gerontol Geriatr 56:148–154
Abbate LM, Stevens J, Schwartz TA, Renner JB, Helmick CG et al (2006) Anthropometric measures, body composition, body fat distribution, and knee osteoarthritis in women. Obesity (Silver Spring) 14:1274–1281
Madsen OR, Brot C, Petersen MM, Sorensen OH (1997) Body composition and muscle strength in women scheduled for a knee or hip replacement. A comparative study of two groups of osteoarthritic women. Clin Rheumatol 16:39–44
Hochberg MC, Lethbridge-Cejku M, Scott WW Jr, Reichle R, Plato CC et al (1995) The association of body weight, body fatness and body fat distribution with osteoarthritis of the knee: data from the Baltimore Longitudinal Study of Aging. J Rheumatol 22:488–493
Reijman M, Pols HA, Bergink AP, Hazes JM, Belo JN et al (2007) Body mass index associated with onset and progression of osteoarthritis of the knee but not of the hip: the Rotterdam Study. Ann Rheum Dis 66:158–162
Hart DJ, Doyle DV, Spector TD (1995) Association between metabolic factors and knee osteoarthritis in women: the Chingford Study. J Rheumatol 22:1118–1123
Davis MA, Ettinger WH, Neuhaus JM (1988) The role of metabolic factors and blood pressure in the association of obesity with osteoarthritis of the knee. J Rheumatol 15:1827–1832
Felson DT (1996) Weight and osteoarthritis. Am J Clin Nutr 63:430S–432S
Hannan MT, Anderson JJ, Zhang Y, Levy D, Felson DT (1993) Bone mineral density and knee osteoarthritis in elderly men and women. The Framingham Study. Arthritis Rheum 36:1671–1680
Hochberg MC, Lethbridge-Cejku M, Tobin JD (2004) Bone mineral density and osteoarthritis: data from the Baltimore Longitudinal Study of Aging. Osteoarthr Cartil 12(Suppl A):S45–S48
Yoshimura N, Muraki S, Oka H, Mabuchi A, Kinoshita H et al (2009) Epidemiology of lumbar osteoporosis and osteoarthritis and their causal relationship—is osteoarthritis a predictor for osteoporosis or vice versa?: the Miyama study. Osteoporos Int 20:999–1008
Acknowledgments
The study was partially supported by a Grant from the Department of Science and Technology, Ho Chi Minh City, and a grant from the University Commission for Development (CUD) program, Belgium. We thank the following friends and colleagues for their support and help in the recruitment and providing logistic support for the study: Fr. Pham Ba Lam, Fr. Vu Minh Danh, Mr. Pham Doan Phong, Mr. Luong Thanh Phat, Mr. Nguyen Cong Phu, and Mr. Tien Ngoc Tuan. We thank Dr. Le Thi Ngoc Linh and Dr. Pham Ngoc Khanh of the People’s Hospital 115, and our medical students Nguyen Hai Dang, Vo Thi Thuy An, Nguyen Thi Thanh Thao, Mai Duy Linh, Nguyen Vu Dat, Diem Dang Khoa, and Tran Hong Bao for their assistance in the interview of participants.
Author Contribution
The conception and design of the study: Lan T. Ho-Pham and Tuan V. Nguyen; Acquisition of data: Lan T. Ho-Pham, Thai Q Lai, Linh D. Mai, and Minh C Doan. Analysis and interpretation of data: Lan T. Ho-Pham and Tuan V. Nguyen; Drafting the manuscript: Lan T. Ho-Pham and Tuan V. Nguyen; Statistical analysis: Thai Q. Lai, Tuan V. Nguyen; Critical revision of the manuscript: Lan Ho-Pham and Tuan V. Nguyen. All authors read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors (Dr. Lan T. Ho-Pham, Dr. Thai Q. Lai, Dr. Linh D. Mai, Dr. Minh C. Doan, Prof. Tuan V. Nguyen) declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
The research protocol and procedures were approved by the Scientific Committee of the People’s Hospital 115 and Pham Ngoc Thach University of Medicine. All participants were provided with full information about the study’s purposes, and gave written informed consent to participate in the study.
Rights and permissions
About this article
Cite this article
Ho-Pham, L.T., Lai, T.Q., Mai, L.D. et al. Body Composition in Individuals with Asymptomatic Osteoarthritis of the Knee. Calcif Tissue Int 98, 165–171 (2016). https://doi.org/10.1007/s00223-015-0080-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-015-0080-8