Abstract
Bone disease in hemodialysis (HD) patients with type 2 diabetes mellitus (DM) is characterized by low bone turnover (Inaba M, et al. Am J Kidney Dis 2002; 39:1261-1269), although their bone quality is yet to be determined. The present study was designed to examine whether the prevalence of vertebral fracture in female HD patients with type 2 DM, age 65 years and older, might be increased, and the relation of this fracture to bone mineral density (BMD) determined by dual X-ray absorptiometry (DXA), since few data are available on the effect of DM on bone strength at lumbar spine. The prevalence of vertebral fracture in type 2 DM HD patients was 32.3%, which was greater than that of non-DM HD patients (13.3%) when adjusted for age and HD duration. Logistic regression analysis elucidated the presence of DM and age as independent risk factors for an increased prevalence of vertebral fracture in HD patients. In non-DM HD patients, those with vertebral fracture showed age significantly higher and BMD in either lumbar spine or distal one third of radius significantly lower than the respective value in those without fracture. However, in DM HD patients, neither BMD in lumbar spine nor distal one third of radius was significantly lower in those with vertebral fracture than in those without. Furthermore, age did not differ significantly between DM HD patients with and without fracture. In conclusion, female type 2 DM HD patients, age 65 years and older, showed significantly higher incidence of vertebral fracture than non-DM HD patients. Although age and low BMD emerged as independent risk factors for vertebral fracture in non-DM HD patients, those factors failed to be a risk factor in DM HD patients, suggesting that BMD determined by DXA might not be reliable in assessing bone strength in DM HD patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bone disease in diabetes mellitus (DM) is characterized by a low rate of bone formation [1-4], although its effect on the prevalence of vertebral fracture is yet to be determined. We reported that impaired bone formation in the patients with type 2 DM, including hemodialysis (HD) patients, may result mainly from impaired secretion of parathyroid hormone (PTH) [5-8]. A prospective and epidemiologic study recently reported that older female patients with type 2 DM (>65 years old) have higher incidence of nonvertebral fracture than non-DM patients, irrespective of the same BMD, although the investigators did not monitor the incidence of vertebral fracture for a study period of 9 years but only for 3 years [9]. A previous study reported that HD patients had a significantly higher prevalence of vertebral fracture [10] and that low PTH [10, 11] and low bone turnover [12] are major risk factors for vertebral fracture in those patients. Because HD patients with type 2 DM have serum PTH levels significantly lower than non-DM HD patients [5, 6], an increasing proportion of DM HD patients with lower serum PTH may contribute to the higher incidence of vertebral fracture in HD patients.
Although accumulated evidence indicates that there is a relationship between low bone mass and increased fracture risk [13, 14], the possibility that diabetes is associated with a decrease in bone strength that is not apparent from conventional bone density measurements is raised [9]. Lower PTH levels may lead to accumulation of microdamage of bone by suppressing bone turnover [15], thereby resulting in poor bone quality.
These observations prompted us to investigate (i) whether the prevalence of vertebral fracture might be increased in older female HD patients with type 2 diabetes (65 years and older) compared to non-DM counterparts, and (ii) the relationship between vertebral fracture and bone mineral density (BMD) in lumbar spine to examine the clinical utility and the appropriate role of BMD measurements in the prediction of vertebral fracture in HD patients with type 2 diabetes.
Patients and Methods
Patients
One hundred and fourteen HD patients maintained at Shirasagi Hospital were enrolled in the present study after written informed consent for joining the present study was obtained from each. Subjects were restricted to female subjects, age 65 years or older, in the present study as in the previous large epidemiologic study [9] and also to avoid the influence of the menstrual cycle on bone metabolism. The mean (± standard deviation [SD]) age was 71.8 ± 4.5 years and HD duration was 3.80 ± 3.02 years in HD patients with type 2 DM, and age 73.6 ± 6.3 years and HD duration 5.73 ± 6.03 years in non-DM HD patients, respectively. The diagnosis of type 2 DM was based on a history of diabetes or criteria according to the Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus [16].
At the time of the study, most of the patients had received either calcitriol or phosphate-binding therapy. Patients for whom HD duration was less than 1 year or more than 12 years, or who had a history of parathyroidectomy, oral pulse calcitriol therapy, steroid therapy, or therapy for osteoporosis such as hormone replacement therapy were excluded from the study.
Sample Collection
Patients received an HD session three times weekly, on Monday, Wednesday, and Friday. Blood sampling was performed at the Monday session, exactly 68 hours after the previous session, as previously described [6, 7]. A blood sample was withdrawn from the arteriovenous fistula and collected immediately before the start of the HD session. Blood was kept on ice for 30 minutes and then centrifuged at 1000g for 10 minutes. The resultant serum was stored in aliquots at -30?C until assayed. The frozen samples were thawed and the measurement was performed immediately.
Biochemical Parameters for Ca Metabolism and PTH Assay
Biochemical parameters in serum were determined essentially as previously described [6, 7]. Serum levels of Ca, phosphate (Pi), and albumin were measured with an autoanalyzer. Blood hemoglobin A1c (HbA1c) was determined as previously described [7]. Serum PTH was measured by immunoradiometric assay (Allegro Intact PTH, Nichol’s Institute, San Juan, Capistrano, CA, U.S.A.) [6, 7]. The intra- and interassay CVs for PTH were 4.8% and 9.3%, respectively [17]. The normal range for healthy people determined in our laboratory was 15.4 to 60.0 pg/mL.
Assessment of Vertebral Fractures
All patients underwent radiographic examinations of the thoracic and lumber spine. Vertebral fractures were assessed with lateral radiographs. The vertebral bodies from the fourth thoracic to the fifth lumbar were measured by using a digitizer. Ratios of the anterior or midpoint height of the vertebra to the posterior height were obtained. The assessment of vertebral fracture was based on the criteria created by the research group on osteoporosis of the Ministry of Health and Welfare of Japan; a fracture was considered present if the anterior height of the vertebra was 25% less than the posterior height or if the middle or posterior was 20% less than the posterior height within a vertebra or adjacent vertebra [10].
BMD Measurement
BMD was measured by dual X-ray absorptiometry (DXA) (QDR-4500A; Hologic Inc., Waltham, MA, U.S.A), with both measurements performed 21 to 24 hours after completion of a dialysis session. BMD measurement was performed at least 1 year after HD initiation to avoid the influence of acute metabolic change on BMD in the induction period of hemodialysis [18]. BMD was measured in the distal one third of the radius and the third of the lumbar spine (L3). L3 BMD measurement was performed in the lateral position to avoid the influence of the calcification of the descending aorta on lumbar spine BMD that is often seen in HD patients [19]. Any patient enrolled in the present study was confirmed not to have a fracture at L3 in lateral radiographs to avoid the apparent increase of BMD by fracture.
Statistical Analysis
Data were analyzed by using the StatView 5.0 J program (Abacus Concepts, Inc,. Berkeley, CA, U.S.A.). Values are means ± SD unless otherwise indicated. The differences in the means between DM and non-DM patients were analyzed by the Student t test. Correlation coefficients were calculated by using simple regression analysis. The χ 2 test was used for comparisons of proportions. The risk of vertebral fracture was estimated by using logistic regression models. Findings of P < 0.05 were considered significant.
Results
Clinical and Biochemical Profiles of HD Patients with and without Type 2 DM
Clinical and biochemical profiles of the patients enrolled in the present study are shown in Table 1. There was no significant difference in age; body weight; HD duration; or serum levels of albumin, Ca, Pi, and PTH between older DM HD patients (n = 31) and non-DM HD patients (n = 83). Mean serum PTH level in the DM group was 106.1 ± 97.1 pg/mL, which was not significantly lower than that in the non-DM HD patients (139.5 ± 135.8 pg/mL), probably because of the small number of subjects. L3 BMD did not differ between DM HD patients and non-DM HD patients, whereas BMD in the distal one third radius was higher in DM HD patients than in non-DM HD patients. The numbers of patients having vertebral fracture were 10 (32.3%) of 31 DM HD patients and 11 (13.2%) of 83 non-DM HD patients. The difference in the proportions having fracture was statistically significant between DM HD and non-DM HD patients (P < 0.05 by χ2 test), indicating higher prevalence of vertebral fracture in DM HD patients.
Logistic Regression Analysis of Risk Factors for Vertebral Fracture
We next determined the risk factors for vertebral fractures in HD patients. As shown in Table 2, logistic regression analysis between the vertebral fracture and nonfracture groups elucidated age and the presence of type 2 DM as independent risk factors for vertebral fractures in HD patients. HD duration, L3 BMD, and serum PTH level did not emerge as a risk factor for vertebral fracture.
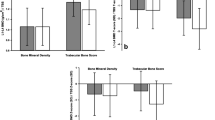
Comparison of Clinical Profiles of DM and non-DM HD Patients with and without Vertebral Fracture
In non-DM HD patients, those with fracture had age significantly older than those without fracture (Table 3). Furthermore, BMD either in lumbar spine or in the distal one third of the radius was significantly lower in those with fractures than in those without. In contrast, between DM HD patients with and without fracture there was no significant difference in BMD in either site or with respect to age. Serum PTH did not differ significantly between those with and without fracture in either the DM or non-DM group of patients.
Discussion
The present study clearly demonstrated that the prevalence of vertebral fracture in female DM HD patients, age 65 years and older, was higher than that of non-DM HD patients when adjusted for age, HD duration, and biochemical parameters including serum PTH, Ca, and Pi levels (Table 1). Logistic regression analysis elucidated the presence of DM, in addition to age, as an independent risk factor for increased prevalence of vertebral fracture in HD patients (Table 2). In non-DM HD patients, those with vertebral fracture showed age significantly older and BMD in either lumbar spine or distal one third of radius significantly lower than the respective value in those without fracture (Table 3). However, of great interest, BMD in either lumbar spine or distal one third of the radius was not significantly lower in DM HD patients with vertebral fracture than in those without. Furthermore, age did not differ significantly between DM HD patients with and without fracture (Table 3), andincreased incidence of vertebral fracture is not explained by lower BMD in DM HD patient in contrast to non-DM HD patients. It is possible that BMD did not differ between DM HD patients with and without fracture because of the small number of patients. However, the mean BMD value was essentially the same for those with and without fracture. Therefore, even if the number of DM HD patients increases, the difference should not become statistically significant; this contrasts with the situation of significantly lower BMD in non-DM HD patients with fracture.
It was previously reported that HD patients show a higher prevalence of vertebral fracture and that a reduction of lumbar spine BMD and aging increased the odds ratio of vertebral fracture [10]. These findings are in agreement our data in terms of non-DM HD patients. However, neither BMD in the lumbar spine and distal one third of radius nor age of DM HD patients differed significantly between those with and without vertebral fracture (Table 3). BMD of a given region is the best predictor of fractures in that region [20], but BMD at another site is a second best predictor. Therefore, the present study was designed to measure BMD in the lumbar spine to assess risk for vertebral fracture. The lack of a significant reduction in lumbar spine BMD in DM HD patients with vertebral fracture strongly suggests that bone strength might not be determined principally by BMD in DM HD patients. A previous study reported that, irrespective of having the same BMD, DM patients have a higher incidence of nonvertebral fracture than non-DM patients, although no data were available from the study on the incidence of vertebral fracture during the study period of 9 years [9]. Therefore, it is possible that bone quality of the vertebrae might be deteriorated, irrespective of a high BMD level at lumbar spine in DM HD patients. Although little is known about bone quality in DM patients, it is suggested that the low bone turnover state in DM patients resulting from low PTH [5, 6] and the occurrence of osteoblast refractoriness to PTH [7, 21-24] may cause an accumulation of microdamage of bone, thereby leading to increasing bone fragility [15]. It was reported previously that low PTH [10, 11] and low-turnover osteodystrophy [12] are risk factors for vertebral osteoporosis in HD patients. Although a significant difference did not exist in serum PTH levels between DM and non-DM HD patients, probably because of the small number of patients in the present study (Table 1), the data supported the notion of lower serum PTH levels in DM HD patients compared to non-DM HD patients as we described previously [5, 6]. Supportive of lower bone turnover in DM HD patients DM HD patients exhibited a significantly higher BMD in the distal one third of the radius than non-DM HD patients and a tendency toward higher BMD in L3. This may be a consequence of a low bone turnover state, whereby there is attenuation of age-related/postmenopausal bone loss in DM HD patients [3, 4].
Another possible candidate to induce low bone turnover in patients with DM is the abnormal vascular function caused by the microvascular complications associated with diabetes [25, 26], which may impair osteoblast function by decreasing blood supply to bone cells. Furthermore, there are many factors that could predispose DM patients to bone fractures. These include altered proprioception, balance, postural hypotension, and gait caused by neuropathy and visual impairment from diabetic retinopathy and cataracts, which may increase the risk for fractures by causing frequent falls [27]. Although osteoporosis traditionally has not been listed as a complication of DM, particularly those with type 2 DM, recent large-scale epidemiologic data demonstrated higher incidence of bone fracture in type 2 DM patients [9, 28, 29]. Although DXA, which is available in clinical practice, is the best predictor and evaluator of osteoporosis, it is not a perfect diagnostic tool because there are many microarchitectural bone qualities and bone geometries that are not detectable via DXA. This is particularly true when assessing patients with type 2 DM [30]. The limitation of the present study is the small number of patients. Because the present study was performed in only one hospital, the finding should be further confirmed by a larger scale multicenter study.
In summary, female DM HD patients, age 65 years and older, showed a higher incidence of vertebral fracture than non-DM HD patients. Although age and low BMD emerged as an independent risk factors for vertebral fracture in non-DM HD patients, those factors failed to be a risk factor in DM HD patients, suggesting that BMD determined by DXA might not be reliable in assessing bone strength in DM HD patients.
References
Inaba, M, Ishimura, E (2002) “Secondary osteoporosis” In: Moril, H, Nishizawa, Y, Masry, SG, (editors), Calcium in Internal Medicine, Springer-Verlag, London, pp 347–360
H Rico ER Hernandez JA Cabranes F Gomez-Castresana (1989) ArticleTitleSuggestion of a deficient osteoblastic function in diabetes mellitus. The possible cause of osteopenia in diabetics Calcif Tissue Int 45 71–73 Occurrence Handle1:STN:280:DyaL1Mzns1WgtA%3D%3D Occurrence Handle10.1007/BF02561404
R Bouillon M Bex EV Herck J Laureys L Dooms E Lesaffre Ravussin (1995) ArticleTitleInfluence of age, sex, and insulin on osteoblast function: Osteoblast dysfunction in diabetes mellitus J Clin Endocrinol Metab 80 1194–1202 Occurrence Handle1:CAS:528:DyaK2MXkvFaqu7Y%3D Occurrence Handle7714089
JC Krakauer MJ McKenna NF Buderer DS Rao FW Whitehouse AM Parfitt (1995) ArticleTitleBone loss and bone turnover in diabetes Diabetes 44 775–782 Occurrence Handle1:CAS:528:DyaK2MXms1Cmsrw%3D Occurrence Handle10.2337/diab.44.7.775
M Inaba K Nagasue S Okuno M Ueda Y Kumeda Y Imanishi T Shoji E Ishimura T Ohta T Nakatani M Kim Y Nishizawa (2002) ArticleTitleImpaired secretion of parathyroid hormone, but not refractoriness of osteoblast, is a major mechanism of low bone turnover in hemodialyzed patients with diabetes mellitus Am J Kidney Dis 39 1261–1269 Occurrence Handle1:CAS:528:DC%2BD38XkvFGgtrk%3D Occurrence Handle10.1053/ajkd.2002.33400
M Inaba S Okuno K Nagasue T Otoshi Y Kurioka K Maekawa Y Kumeda Y Imanishi E Ishimura T Ohta H Morii M Kim Y Nishizawa (2001) ArticleTitleImpaired secretion of parathyroid hormone is coherent to diabetic hemodialyzed patients Am J Kidney Dis 38 IssueID4 suppl 1 S139–142 Occurrence Handle1:CAS:528:DC%2BD3MXnslKgtrk%3D Occurrence Handle10.1053/ajkd.2001.27423
M Inaba Y Nishizawa K Mita Y Kumeda M Emoto T Kawagishi E Ishimura K Nakatsuka A Shioi H Morii (1999) ArticleTitlePoor glycemic control impairs the response of biochemical parameters of bone formation and resorption to exogenous 1,25-dihydroxyvitamin D3 in patients with type 2 diabetes Osteoporos Int 9 525–531 Occurrence Handle1:CAS:528:DyaK1MXlslSlt74%3D Occurrence Handle10.1007/s001980050180
T Kawagishi H Morii K Nakatsuka K Sasao K Kawasaki T Miki Y Nishizawa (1991) ArticleTitleParathyroid hormone secretion in diabetes mellitus Contrib Nephrol 90 217–22 Occurrence Handle1:STN:280:DyaK38%2FntVWjug%3D%3D Occurrence Handle10.1159/000420146
AV Schwartz DE Sellmeyer KE Ensrud JA Cauley HK Tabor PJ Schreiner SA Jamal DM Black SR Cummings (2001) ArticleTitleOlder women with diabetes have an increased risk of fracture: a prospective study J Clin Endocrinol Metab 86 32–38 Occurrence Handle1:CAS:528:DC%2BD3MXhtVGgu74%3D Occurrence Handle10.1210/jcem.86.1.7139
K Atsumi K Kushida K Yamazaki S Shimizu A Ohmura T Inoue (1999) ArticleTitleRisk factors for vertebral fractures in renal osteodystrophy Am J Kidney Dis 33 287–293 Occurrence Handle1:STN:280:DyaK1M7ks1antw%3D%3D Occurrence Handle10.1016/S0272-6386(99)70302-1
M Coco H Rush (2000) ArticleTitleIncreased incidence of hip fractures in dialysis patients with low serum parathyroid hormone Am J Kidney Dis 36: 1115–1121 Occurrence Handle10.1053/ajkd.2000.19812
B Piraino T Chen L Cooperstein G Segre J Puschett (1988) ArticleTitleFractures and vertebral bone mineral density in patients with renal osteodystrophy Clin Nephrol 30 57–62 Occurrence Handle1:STN:280:DyaL1M%2FivFaksw%3D%3D Occurrence Handle3180516
DA Nelson SJ Jacober (2001) ArticleTitleEditorial: Why do older women with diabetes have an increased fracture risk? J Clin Endocrinol Metab 86 29–31 Occurrence Handle1:CAS:528:DC%2BD3MXhtVGgurc%3D Occurrence Handle10.1210/jcem.86.1.7248
WHO Study Group (1994) Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. WHO Technical Report Series 843. Geneva, WHO
MR Schaffler (2003) ArticleTitleRole of bone turnover in microdamage Osteoporos Int 14 IssueIDsuppl 5 S73–S80 Occurrence Handle10.1007/s00198-003-1477-1
InstitutionalAuthorNameAmerican Diabetes Association (1998) ArticleTitleMellitus TECotDacoD. Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus Diabetes Care 21 IssueIDsuppl 1 S5–S22
Y Kumeda M Inaba H Tahara Y Kurioka T Ishikawa H Morii Y Nishizawa (2000) ArticleTitlePersistent increase in bone turnover in Graves’ patients with subclinical hyperthyroidism J Clin Endocrinol Metab 85 4157–4161 Occurrence Handle1:CAS:528:DC%2BD3cXotlWnurY%3D Occurrence Handle11095447
E Ishimura S Okuno M Kim T Yamamoto T Izumotani T Otoshi T Shoji M Inaba Y Nishizawa (2001) ArticleTitleIncreasing body fat mass in the first tear of hemodialysis J Am Soc Nephrol 12 1921–1926 Occurrence Handle1:STN:280:DC%2BD3MvnsFertQ%3D%3D Occurrence Handle11518786
M Ueda M Inaba S Okuno K Nagasue K Kitatani E Ishimura M Shimizu T Miki M Kim Y Nishizawa (2002) ArticleTitleClinical usefulness of the serum N-terminal propeptide of type I collagen as a marker of bone formation in hemodialysis patients Am J Kidney Dis 40 802–809 Occurrence Handle1:CAS:528:DC%2BD38Xotl2hs70%3D Occurrence Handle10.1053/ajkd.2002.35692
SR Cummings DM Black MC Nevitt W Browner J Cauley K Ensrud HK Genant L Palermo J Scott TM Vogt (1993) ArticleTitleBone density at various sites for prediction of hip fractures. The Study of Osteoporotic Fractures Research Group Lancet. 341 IssueID8837 72–75 Occurrence Handle1:STN:280:DyaK3s7hs1GisA%3D%3D Occurrence Handle10.1016/0140-6736(93)92555-8
M Inaba M Terada H Koyama O Yoshida E Ishimura T Kawagishi Y Okuno Y Nishizawa S Otani H Morii (1995) ArticleTitleInfluence of high glucose on 1,25-dihydroxyvitamin D3-induced effect on human osteoblast-like MG-63 cells J Bone Miner Res 10 1050–1060 Occurrence Handle1:CAS:528:DyaK2MXntVakt78%3D Occurrence Handle10.1002/jbmr.5650100709
M Terada M Inaba Y Yano T Hasuma Y Nishizawa H Morii S Otani (1998) ArticleTitleGrowth-inhibitory effect of a high glucose concentration on osteoblast-like cells Bone 22 17–23 Occurrence Handle1:CAS:528:DyaK1cXjvFKhsA%3D%3D Occurrence Handle10.1016/S8756-3282(97)00220-2
M Inaba M Terada Y Nishizawa A Shioi E Ishimura S Otani H Morii (1999) ArticleTitleProtective effect of aldose reductase inhibitor against bone loss in galactose-fed rats: possible involvement of polyol pathway in bone metabolism Metabolism 48 904–909 Occurrence Handle1:CAS:528:DyaK1MXksFOru70%3D Occurrence Handle10.1016/S0026-0495(99)90227-5
M Inaba Y Nishizawa A Shioi H Morii (1997) ArticleTitleImportance of sustained high glucose condition in the development of diabetic osteopenia: possible involvement of the polyol pathway Osteoporos Int 7 . IssueIDsuppl 3 S209–S212 Occurrence Handle10.1007/BF03194374
MT Vogt JA Cauley LH Kuller MC Nevitt (1977) ArticleTitleBone mineral density and blood flow to the lower extremities: The Study of Osteoporotic Fractures J Bone Miner Res 12 283–289 Occurrence Handle10.1359/jbmr.1997.12.2.283
B Piepkorn P Kann T Forst J Andreas A Pfutzner J Beyer (1997) ArticleTitleBone mineral density and bone metabolism in diabetes mellitus Horm Metab Res 29 584–591 Occurrence Handle1:CAS:528:DyaK1cXhs1WrtQ%3D%3D Occurrence Handle10.1055/s-2007-979106
RQ Ivers RG Cumming P Mitchell AJ Peduto (2001) ArticleTitleDiabetes and risk of fracture Diabetes Care 24 1198–1203 Occurrence Handle1:STN:280:DC%2BD3MzmtF2qtA%3D%3D Occurrence Handle10.2337/diacare.24.7.1198
RQ Ivers RG Cumming P Mitchell AJ Peduto (2000) ArticleTitleDiabetes and risk of fracture: the Blue Mountains Eye Study Diabetes Care 24 1198–2003 Occurrence Handle10.2337/diacare.24.7.1198
K Nicodemus AR Folsom (2001) ArticleTitleType 1 and type 2 diabetes and incident hip fracture in postmenopausal women Diabetes Care 24 1192–1197 Occurrence Handle1:STN:280:DC%2BD3MzmtF2qtw%3D%3D Occurrence Handle10.2337/diacare.24.7.1192
DL Chau SV Edelman (2002) ArticleTitleOsteoporosis and Diabetes Clin Diabetes 20 153–157 Occurrence Handle10.2337/diaclin.20.3.153
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Inaba, M., Okuno, S., Kumeda, Y. et al. Increased Incidence of Vertebral Fracture in Older Female Hemodialyzed Patients with Type 2 Diabetes Mellitus. Calcif Tissue Int 76, 256–260 (2005). https://doi.org/10.1007/s00223-004-0094-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-004-0094-0