Abstract
We compared the mechanical properties of bones from mice lacking either a functional cycloxygenase-1 (C57BL6/DBA COX-1−/−; n = 9) or COX-2 (C57BL6/DBA COX-2−/−; n = 9) gene and wild type mice (C57BL6/DBA; n = 10). Twenty-eight right femora from 3-month-old male mice were used to determine bulk structural and material properties of bone by three-point bending. Bone matrix properties were also measured by nanoindentation to access the changes in bulk mechanical properties due to changes in bone matrix or bone geometry. The bulk material properties (elastic modulus, P < 0.05; ultimate stress, P < 0.01) of COX-2−/− bones were lower than those of wild-type mice whereas the bulk structural properties (stiffness, P > 0.2; breaking force, P > 0.1) were similar to those of the wild-type mice. COX-2−/− mice had a longer moment of inertia but their cortical bones were thinner and contained many more intra-cortical pores compared with the bones of the other two groups. Finally, the bone matrix properties of COX-1−/− mice, COX-2−/− mice and their heterozygous littermates were similar to those of C57BL6/DBA wild-type mice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Prostaglandins (PGs) are synthesized from arachidonic acid (AA) that is converted into PGH2 by the rate-limiting enzymatic reaction carried out by cyclooxygenase (COX) [1, 2, 3, 4]. Prostaglandin H2 is then isomerized to form a number of biologically active prostanoids that include PGE2 and PGI2 [2]. The two COX isozymes, COX-1 and COX-2, are each encoded by a different gene that is subject to unique regulation in vivo. COX-1 is constitutively expressed throughout the body but COX-2 is usually not present in most tissues and its expression is induced by pro-inflammatory agents, and in case of bone, by mechanical stimulus [1, 4, 5, 6].
Prostaglandins have been shown to regulate bone metabolism in vivo and in vitro [7]. Exogeneously added PGE2 (i) stimulates periosteal bone formation to increase total tissue area; (ii) enhances endocortical bone formation that accompanies reduced area of bone marrow; (iii) stimulates trabecular bone formation; and (iv) increases cortical porosity by activating intra-cortical bone remodeling [8]. PGE2 was also reported to increase the mechanical strength of bones in rapidly growing and mature male rats and could completely restore the deficit of cancellous bone in ovariectomized rats with established osteopenia [9].
Since both COX isozymes are present in the bone, the precise contribution of COX-1 and COX-2 in the turnover and remodeling of bone is unclear [7]. It has been suggested that COX-2 plays a unique role in bone remodeling in the adult that is different from its action on de novo formation of skeleton during development. Induction of COX-2 following injury and inflammation and elaboration of PGs is thought to directly regulate bone remodeling. Consistent with this hypothesis, COX-2−/− mice were shown to have decreased bone density compared with their heterozygous littermates; COX-2 was needed for optimal differentiation of mesenchymal cells into osteoclasts and osteoblasls that contributed to both intra-membranous and endochondral bone formation during bone repair [5, 6]. Since the abnormal bone repair in COX-2−/− mice could be reversed by exogenous PGE2, the authors concluded that PGs produced via the action of COX-2 directly affected bone remodeling [5, 6].
The effects of COX-2 on the mechanical properties of bone have not been directly investigated. Based on the previous observations, we hypothesized that the bones of COX-2−/− mice may have lower mechanical properties. Therefore we compared bulk material (elastic modulus and ultimate stress) and structural (stiffness and breaking force) properties by three-point bending, bone matrix properties (elastic modulus and hardness) by nanoindentation, and bone geometries (moment of inertia, cortical thickness, cortical area, and cortical diameter) in the wild type, COX-1−/− and COX-2−/− mice. We specifically tested the bone matrix properties by nanoindentation methods with a goal to test whether the altered bulk mechanical properties of bone were due to its structure and geometry or to changes in the bone matrix.
Materials and Methods
C57B6/DBA COX-1−/− (PGHS-1 null), COX-2−/− (PGHS-2 null) and their wild type littermates (C57BL6/DBA) were developed at the Department of Veteran’s Affairs Medical Center, Memphis, TN [10, 11] from mating pairs that originated at the University of North Carolina [3, 12]. Prior to experiments mice were housed in plexiglass cages at 25°C and kept on a 12-hr light/12-hr dark cycle in a virus-free environment. Food and water were available ad libitum. Due to fertility problems of the PGHS-null females, homozygous males were bred with heterozygous females to obtain homozygous COX-1 and COX-2-ablated mice used in these experiments. The progeny of heterozygous mating, containing both wild-type COX alleles, was used as control.
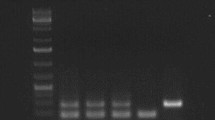
The genotypes of mice were determined by PCR [11]. DNA from tails was extracted using the Dneasy Tissue Kit from Qiagen (Valencia, CA). Tail samples were lysed overnight in a buffer containing proteinase K, and loaded onto a mini-column. After the column was washed, DNA was eluted in water and used for PCR. Three primers were used in the same PCR reactions for identification of the PGHS-1 or PGHS-2 allele. The WT allele 5′ primer (PGHS1-5′) AGGAGATGGCTGCTGAGTTGG, the mutant allele 5′ primer (PGHS1-neo) GCAGCCTCTGTTCCACATACAC, and the 3′ primer (PGHS1-3′) AATCTGACTTTCTGAGTTGCC were used to yield a fragment of 600 or 700 bp for the PGHS-1 WT or mutant allele, respectively. The WT allele 5′ primer (PGHS-2 5′-ACACATCTCACTGGCACC, the mutant allele 5′ primer (NeoPro) ACGCGTCACCTTAATATGCG, and the 3′ primer (TGC2-3) GTACGGTTCAGGGAGAA yield a fragment of 600 or 800 bp for the PGHS-2 WT or mutant allele, respectively. Three month-old mice were sacrificed by CO2 suffocation. The right femur from each mouse was excised and cleaned of soft tissue.
Femora were subjected to biomechanical testing in three-point bending (Instron 8500, Canton, MA) to measure bulk bone properties. Each femur was placed on two supports at a span length of 8.5 mm. Force was applied vertically at the mid-shaft of the bone on the anterior surface such that the anterior surface was under compression while the posterior surface was under tension. The press head as well as the two support points were rounded to avoid shear load and cutting [13, 14, 15]. Each bone was compressed at a constant rate of 3.6 mm/min until fracture [13]. Data were collected using a custom-written LabVIEW (National Instruments, Austin, TX) program and were converted into a load versus displacement curve. Stiffness (bulk structural property) was calculated as the slope of the linear (elastic) part of the load-displacement curve. Ultimate stress σ and elastic modulus E (bulk material properties) were calculated according to the previously reported formulas [14, 16, 17] as follows:


where F is the breaking force, L is the span of the support points, c is the half-diameter of the mid-shaft in the load direction, d is the displacement, and I is the principal moment of inertia.
The proximal part of each femur used in the three-point bending tests was embedded without vacuum in epoxy resin (EPO-THIN™ low viscosity epoxy, Buehler, Lake Bluff, IL) at room temperature to measure bone matrix properties by nanoindentation. Embedded samples were metallographically polished to expose the bone material to be measured and produce smooth surfaces needed for nanoindentation. Specimens were ground with silicon carbide abrasive papers of decreasing grit size (400, 600, 800, and 1200 grits) under de-ionized water, followed by micro-cloths (TEXMET, Buehler, Lake Bluff, IL) with alumina powder of 0.05 µm grit. After the polishing, the specimens were ultrasonically cleaned to remove surface debris.
All nanoindentation tests were performed using the Tribolndenter (Hysitron Inc., St. Paul, MN) in load control mode with a pyramid-shaped diamond tip. Fused silica was used prior to the measurements to calibrate the tip shape function and machine compliance. Four indents were made in each target area to reduce the effects of variations. To minimize the effects of viscoelasticity and creep on property measurements, a relatively long constant load hold period was conducted before the final unloading to diminish visco-elastic deformation to a negligible rate. The maximum load of the nanoindentation tests was 3 mN, with a loading/unloading rate of 200 µN/s, which produced impressions in bones 500 nm deep.
The Oliver-Pharr method [18] for determining the indentation modulus and hardness has been well documented and will not be discussed at length. Measurements of load and displacement were used to determine the contact stiffness. The reduced modulus E r was determined from the contact stiffness. The equations used to calculate the hardness (H) and the reduced modulus (E r) were:

and

where P max is the maximum force, A c is the contact area, and S the contact stiffness. The elastic modulus of specimen was derived from:

where ν is Poisson’s ratio. The Poisson’s ratio and elastic modulus of the diamond indenter tip, νtip and E tip, were 0.07 and 1140 GPa, respectively.
Bone cross-sectional geometry was evaluated at one femoral site adjacent to the fracture site. A transverse section about 1 mm thick was cut from each femur using Isomet 1000 (Bulhler, Lake Bluff, IL). Cross-sectional pictures were obtained using a digitizing optical microscope. A custom-written Visual C++ program was used to measure the geometric parameters by digitizing the periosteal and endocortical boundary [19].
The bone cross-sectional area was further examined by histological sections that were stained with hematoxylin and eosin (H&E). Specimens were demineralized and embedded in paraffin. Sections 5 µm thick were cut and mounted on slides to be assessed by light microscopy.
To compare the bulk mechanical properties, bone matrix properties, and geometric properties for different groups, one-way analysis of variance (ANOVA) was used (P < 0.05 for significance). Schéffe test (significance level: 5%) was employed to determine if specific pair-wise values were significantly different. All statistical analyses were performed with StatView 5.0.1 (SAS Institute Inc., USA).
Results
There were statistically significant differences in bulk material properties of C57BL6/DBA COX-2−/− mice when compared with either C57BL6/DBA COX-1−/− or wild-type mice (P < 0.05). Bulk material properties of COX-2−/− mice were 29% lower than those of the wild-type mice and 21% lower than those of the C57BL6/DBA COX-1−/− mice. In contrast, there were no significant differences in bulk material properties between COX-1−/− and their heterozygous littermates. The bulk structural properties (i.e., stiffness and breaking force) of bone among the three groups of mice, regardless of their COX genotype, were also similar (Table 1). Finally, as judged by the nanoindenation tests, no significant differences in bone matrix properties could be demonstrated among the wild type COX-1−/− and COX-2−/− mice (Table 2).
As shown in Table 3, no significant differences in cortical thickness and cortical cross-sectional area could be measured among the three groups of mice. This is in contrast to the measurements of the moment of inertia that was 11% higher in COX-2−/− mice compared with either COX-1−/− or wild-type mice (P < 0.001). There was slightly larger pericortical diameter of bone in COX-2−/− mice (7%) compared with either wild-type or COX-1−/− mice but this apparent difference in pericortical diameter was not statistically significant. In contrast, the endocortical diameter of the femora of COX-2−/− mice was larger than that of either COX-1−/− or wild-type mice (P < 0.001). In general, COX-1−/− mice had the smallest bones accompanied by the thickest cortical bone. The bones of COX-2−/− mice had significantly larger cortical diameter. As depicted in the representative cross-section of H&E-stained bone (Fig. 1), the cortices of COX2−/− were thinner and contained 2–3 times more intracortical pores compared with COX-1−/− or wild-type mice. The histological appearances of bones from heterozygous C57BL6/DBA COX-2−/+ mice were similar to those of COX1−/−, COX1−/+ or WT (unpublished data).
Histological sections stained with hematoxylin and eosin of femoral cortical bones from (A) COX-1−/−, (B) COX-2−/−, and (C) wild-type (heterozygous littermates) mice. Cortical bones of COX-2−/− mice were thinner and contained many more intra-cortical pores compared with the bones of the other two groups. Scale bar indicates 500 µm.
Discussion
We report that the bulk material properties of C57BL6/DBA COX-2−/− bones are lower than those of the wild-type or COX-1−/− mice. The mechanical tests, combined with the results of geometry, histology, and nanoindentation tests, indicate that the decreased bulk material properties of the COX-2−/− mice are mainly due to the decreased thickness of cortical bone containing larger numbers of small intracortical pores (Fig. 1). It appears therefore that the material properties of bones were compensated for by differences in the geometries of bones from COX-1−/− and COX-2−/− mice and their heterozygous littermates. The cellular and molecular mechanisms by which numbers of intracortical pores are increased in the COX-2−/− mice needs to be investigated. How the lack of a functional COX-2 causes the observed changes in the bones of these mice remains unclear.
Since the regulation of bone metabolism and remodeling by PGs has been established both in vivo and in vitro, we hypothesize that lack of a functional COX-2 may potentially lead to the altered metabolism of prostaglandins in the bone. Exogenous PGE2 stimulated bone formation at the periosteal, endocortical, and marrow trabecular surfaces; PGs have also been reported to inhibit endocortical bone resorption with a consequent increase in the cortical bone mass [7, 8, 9, 20, 21, 22]. Although bone is capable of expressing COX-1 and COX-2, experiments with selective inhibitors of COX isozymes implicate COX-2 as the main regulator of bone remodeling. These experiments are largely corroborated by observations of COX-ablated mice, COX-1 and COX-2 knockout mice have revealed unique as well as overlapping roles of the two COX isozymes in various patho-physiological processes, including bone remodeling [23, 24, 25]. Since COX-2−/− mice are born with renal abnormalities [26, 27], it may be argued that the abnormalities in their bones may indirectly emanate from renal dysfunction. We believe that such a scenario is unlikely. The severity of renal pathology and lifespan of COX-2−/− mice appears to be strain-dependent; COX-2−/− mice with a mixed genetic background (DBA/B6) used in our study do not die of renal failure, unlike their B6/COX-2 counterparts [27, 29].
Furthermore, two recent studies provided direct evidence for the involvement of COX-2 in bone remodeling [5, 6]. Bone marrow cells from COX-2−/− mice cultured in vitro elicited decreased osteoclastogenesis and osteoblastogenesis and bone nodule formation. Both of these deficits in osteoclast and osteoblast formation in vitro could be overcome by exogenous PGE2 [5, 6]. Okada et al. [5] also showed that bone marrow cultures from COX-2 heterozygous mice had an intermediate deficit in osteoclastogenesis. In contrast, our COX2 heterozygous mice were similar to wild type with respect to bulk material properties, perhaps reflecting a different genetic background of our strain [10]. These differences not withstanding, we believe that the lower bulk material properties of COX-2−/− mice are not caused by renal complications but are a direct result of a lack of congenital COX-2.
We can only speculate if slightly larger cortical bones of COX-2−/− mice reflect a compensatory mechanical function (i.e., greater moment of inertia) in these animals. Both COX-1 and COX-2 catalyze the same reaction in the synthesis of PGs and it is conceivable that the lack of one type of COX may induce a compensatory change in the remaining isozyme. We have shown earlier that compensatory changes in the metabolism of PGs in fact occur in a number of tissues of COX-2−/− mice both in vivo and in vitro [10, 28, 30].
Nanoindentation is a widely used tool for measuring bone matrix properties [31, 32]. It allows us to probe a surface and map its properties with high resolution [31] and therefore it is a suitable method for assessing whether changes in bulk material properties of bone are due to changes in the bone matrix or geometry [33]. Our nanoindentation data showed that absence of either COX-1 or COX-2 gene had a significant effect on the bone matrix property. We are aware that bulk material properties may not represent true material properties because of a number of assumptions in the interpretation of nanoindentation data that may be too simplistic. For example, the cross-sectional geometry of a long bone varies along its length and is also poorly represented by a hollow circular cross-section, although the bulk material properties derived from whole bone tests assume both geometric and bone matrix properties to be constant [34, 35].
A number of COX-2-selectivc nonsteroidal antiinflammatory drugs (NSAIDs) have been developed in recent years [7, 36]. Although it is well appreciated that non-COX selective NSAIDs inhibit healing of bone-factures, the effects of COX-2 selective NSAIDs on bone remodeling and mechanical properties have not been investigated in detail. The long-term administration of COX-2 selective NSAIDs may decrease the bulk material properties in patients because of increased intracortical porosity and altered bone remodeling. We should point out, however, that the treatment with COX-2-selective NSAIDs in the adults and congenital ablation of COX-2 may not have similar consequences in the bone.
References
MR Forwood (1996) ArticleTitleInducible cyclo-oxygenase (COX-2) mediates the induction of bone formation by mechanical loading in vivo. J Bone Miner Res 11 1688–1693 Occurrence Handle1:CAS:528:DyaK28XnsV2js7w%3D Occurrence Handle8915776
M Joldersma EH Burger CM Semeins JK Nulend (2000) ArticleTitleMechanical stress induces COX-2 mRNA expression in bone cells from elderly women. J Biomech 33 53–61 Occurrence Handle10.1016/S0021-9290(99)00172-4 Occurrence Handle1:STN:280:DC%2BD3c%2FnsFKjuw%3D%3D Occurrence Handle10609518
R Langenbach SG Morham HF Tiano et al. (1995) ArticleTitleProstaglandin synthase 1 gene disruption in mice reduces arachidonic acid-induced inflammation and indomethacin-induced gastric ulceration. Cell 83 483–492 Occurrence Handle1:CAS:528:DyaK2MXpt1Olt78%3D Occurrence Handle8521478
N Shimizu Y Ozawa M Yamaguchi T Goseki K Ohzeki Y Abiko (1998) ArticleTitleInduction of COX-2 expression by mechanical tension force in human periodontal ligament cells. J Periodon 69 670–677 Occurrence Handle1:CAS:528:DyaK1cXkt1Kjuro%3D
Y Okada JA Lorenzo AM Freeman M Tomita SG Morham LG Raisz CC Pilbeam (2000) ArticleTitleProstaglandin G/H synthase-z is required for maximal formation of osteoclast-like cells in culture. J Clin Invest 105 823–832 Occurrence Handle1:CAS:528:DC%2BD3cXhvFehsbY%3D Occurrence Handle10727451
X Zhang EM Schwarz DA Young JE Puzas RN Rosier RJ O’Keefe (2002) ArticleTitleCyclooxygenase-2 regulates mesenchymal cell differentiation into the osteoblast lineage and is critically involved in bone repair. J Clin Invest 109 1405–1415 Occurrence Handle10.1172/JCI200215681 Occurrence Handle1:CAS:528:DC%2BD38XktlWlu74%3D Occurrence Handle12045254
LG Raisz (1999) ArticleTitleProstaglandins and bone: physiology and pathophysiology. Osteoarthritis Cartilage 7 419–421 Occurrence Handle10.1053/joca.1998.0230 Occurrence Handle1:STN:280:DyaK1MzltVyisA%3D%3D Occurrence Handle10419786
HZ Ke WS Jee QQ Zeng M Li BY Lin (1993) ArticleTitleProstaglandin E2 increases rat cortical bone mass when administered immediately following ovariectomy. J Bone Miner Res 21 189–201 Occurrence Handle1:CAS:528:DyaK2cXps12gsw%3D%3D
HZ Ke VW Shen H Qi et al. (1998) ArticleTitleProstaglandin E2 increases bone strength in intact rats and in ovariectomized rats with established osteopenia. Bone 23 249–255 Occurrence Handle10.1016/S8756-3282(98)00102-1 Occurrence Handle1:CAS:528:DyaK1cXlvF2hurg%3D Occurrence Handle9737347
LR Ballou RM Botting S Goorha J Zhang JR Vane (2000) ArticleTitleNociception in cyclooxygenase isozyme-deficient mice. Proc National Acad Sci USA 97 10272–10276 Occurrence Handle10.1073/pnas.180319297 Occurrence Handle1:CAS:528:DC%2BD3cXmtlehtLo%3D
SJF Laulederkind S Thompson-Jaeger Q Chen A Fu JY Rho R Raghow (2002) ArticleTitleBoth constitutive and inducible prostaglandin H synthase affect dermal wound healing in mice. Lab Invest 82 919–927 Occurrence Handle1:CAS:528:DC%2BD38Xmt1Wlsbs%3D Occurrence Handle12118094
SGH Morham R Langenbach CD Loftin et al. (1995) ArticleTitleProstaglandin synthase 2 gene disruption causes severe renal pathology in the mouse. Cell 83 473–482 Occurrence Handle1:CAS:528:DyaK2MXpt1Olt74%3D Occurrence Handle8521477
MP Akhter UT Iwaniec MA Covey DM Cullen DB Kimmel RR Recker (2000) ArticleTitleGenetic variation in bone density, histomorphometry, and strength in mice. Calcif Tissue Int 67 337–344 Occurrence Handle10.1007/s002230001144 Occurrence Handle1:CAS:528:DC%2BD3cXntlOlu7c%3D Occurrence Handle11000349
T Jamasa P Jalovaara Z Peng HK Vaananen J Tuukknen (1998) ArticleTitleComparison of three-point bending test and peripheral quantitative computed tomography analysis in the evaluation of the strength of mouse femur and tibia. Bone 23 155–161 Occurrence Handle10.1016/S8756-3282(98)00076-3 Occurrence Handle9701475
M Martens RV Audekereke PD Meester JC Mulier (1986) ArticleTitleMechanical behaviour of femoral bones in bending loading. J Biomech 19 443–454 Occurrence Handle1:STN:280:BimA3cvkvVw%3D Occurrence Handle3745220
MP Akhter DM Cullen G Gong RR Recker (2001) ArticleTitleBone biomechanical properties in prostaglandin EP1 and EP2 knockout mice. Bone 29 121–125 Occurrence Handle10.1016/S8756-3282(01)00486-0 Occurrence Handle1:CAS:528:DC%2BD3MXlvFWkur8%3D Occurrence Handle11502472
H Oxlund NB Andersen G Qrtoft H Qrskov TT Anderassen (1998) ArticleTitleGrowth hormone and mild exercise in combination markedly enhance cortical bone formation and strength in old rats. Endocrinology 139 1899–1904 Occurrence Handle1:CAS:528:DyaK1cXitVKltrY%3D Occurrence Handle9528976
WC Oliver GM Pharr (1992) ArticleTitleAn improved technique for determining hardness and elastic modulus using load and displacement sensing indentation experiments. J Mater Res 7 1564–1583 Occurrence Handle1:CAS:528:DyaK38XktlWqtb4%3D
ML Nagurka WC Hayes (1979) ArticleTitleAn interactive graphics package for calculating cross-sectional properties of complex shapes. J Biomech 13 59–64
H Kawaguchi CC Pilbeam JR Harrison LG Raisz (1995) ArticleTitleThe role of prostaglandins in the regulation of bone metabolism. Clin Orthop 313 36–46 Occurrence Handle7641496
CH Lin WS Jee YF Ma RB Setterberg (1995) ArticleTitleEarly effects of prostaglandin E2 on bone formation and resorption in different bone sites of rats. Bone 17 IssueID4 suppl 255S–259S Occurrence Handle10.1016/8756-3282(95)98406-D Occurrence Handle1:CAS:528:DyaK2MXptlKjsbk%3D Occurrence Handle8579925
I Suponitzky M Weinreb (1998) ArticleTitleDifferent effects of systemic prostaglandin E2 on bone mass in rat long bones and calvariae. J Endocrinol 156 51–57 Occurrence Handle1:CAS:528:DyaK1cXnslaitA%3D%3D Occurrence Handle9496233
LR Ballou CM Blatteis R Raghow (2001) Elucidation of the patho-physiological roles of prostaglandins using cyclooxygenase gene-deficient mice. JR Vane RM Botting (Eds) Therapeutic role of COX-2 inhibitors. William Harvey Press . 128–167
W Smith D DeWitt R Garavito (2000) ArticleTitleCyclooxygenases: structure, cellular and molecular biology. Ann Rev Biochem 69 145–182
WL Smith R Langenbach (2001) ArticleTitleWhy are there two cyclooxygenase isozymes? J Clin Invest 107 1491–1495 Occurrence Handle1:CAS:528:DC%2BD3MXksFeqsL4%3D Occurrence Handle11413152
SJF Laulederkind BM Wall LR Ballou R Raghow (2002) ArticleTitleRenal pathology resulting from PGHS-2 gene ablation in DBA/B6 mice. Protaglandins & Other Lipid Mediators 67 1–8
JE Dinchuk BD Car RJ Focht et al. (1995) ArticleTitleRenal abnormalilites and an altered inflammatory response in mice lacking cyclooxygenase II. Nature 378 IssueID6555 406–409 Occurrence Handle1:CAS:528:DyaK2MXps1ams7c%3D Occurrence Handle7477380
K Kirtikara SG Morham R Raghow SJF Laulederkind T Kanekura S Goorha LR Ballou (1998) ArticleTitleCompensatory prostaglandin E2 biosynthesis in cyclooxygenase 1 and 2 null cells. J Exp Med 187 517–523 Occurrence Handle10.1084/jem.187.4.517 Occurrence Handle1:CAS:528:DyaK1cXhtFCqtL8%3D Occurrence Handle9463402
VF Norwood SG Morham O Smithies (2000) ArticleTitlePostnatal development and progression of renal dysplasia in cyclooxygenase-2 null mice. Kidney Int 58 2291–3000 Occurrence Handle10.1046/j.1523-1755.2000.00413.x Occurrence Handle1:CAS:528:DC%2BD3MXitFShsg%3D%3D Occurrence Handle11115063
J Zhang S Goorha R Raghow LR Ballou (2002) ArticleTitleThe tissue-specific, compensatory expression of cyclooxygenase-1 and -2 in transgenic mice. Prostaglandins 67 121–135 Occurrence Handle10.1016/S0090-6980(01)00177-0 Occurrence Handle1:CAS:528:DC%2BD38Xjt1Khu7c%3D
JY Rho YT Ting GM Pharr (1997) ArticleTitleElastic properties of human cortical and trabecular lamellar bone measured by nanoindentation. Biomaterials 18 1325–1330 Occurrence Handle10.1016/S0142-9612(97)00073-2 Occurrence Handle1:CAS:528:DyaK2sXntVSlurc%3D Occurrence Handle9363331
PK Zysset XE Guo CE Hoffler KE Moore SA Goldstein (1999) ArticleTitleElastic modulus and hardness of cortical and trabecular bone lamellae measured by nanoindentation in the human femur. J Biomech 32 1005–1012 Occurrence Handle10.1016/S0021-9290(99)00111-6 Occurrence Handle1:STN:280:DyaK1MvgsVCrug%3D%3D Occurrence Handle10476838
CH Turner DB Burr (1993) ArticleTitleBasic biomechanical measurements of bone: a tutorial. Bone 14 595–608 Occurrence Handle1:STN:280:ByuC3c%2FgtVw%3D Occurrence Handle8274302
ME Levenston GS Beaupre MCH van der Meulen (1994) ArticleTitleImproved method for analysis of whole bone torsion tests. J Bone Miner Res 9 1459–1465 Occurrence Handle1:STN:280:ByqC3MjlvV0%3D Occurrence Handle7817831
MCH van der Meulen KJ Jepsen B Mikic (2001) ArticleTitleUnderstanding bone strength: size isn’t everything. Bone 29 101–104 Occurrence Handle10.1016/S8756-3282(01)00491-4 Occurrence Handle1:STN:280:DC%2BD3Mvls1yjsg%3D%3D Occurrence Handle11502469
RD Altman LL Latta R Keer K Renfree FJ Hornicek L Banovac (1995) ArticleTitleEffect of nonsteroidal anti-inflammatory drugs on fracture healing: a laboratory study in rats. J Orthop Trauma 9 392–400 Occurrence Handle1:STN:280:BymC3c%2FjtVU%3D Occurrence Handle8537842
Acknowledgements
These studies were supported by grants from the Department of Veterans Affairs (DVA) and the National Institutes of Health (RR), and the Arthritis Foundation (JR). Rajendra Raghow is a Senior Research Career Scientist of DVA.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chen, Q., Rho, J., Fan, Z. et al. Congenital Lack of COX-2 Affects Mechanical and Geometric Properties of Bone in Mice . Calcif Tissue Int 73, 387–392 (2003). https://doi.org/10.1007/s00223-002-0009-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-002-0009-x