Abstract
The measurement of lecithin: cholesterol acyltransferase (LCAT, EC 2.3.1.43) activity is important in high-density lipoprotein (HDL) metabolism study and cardiovascular disease (CVD) risk assessment. However, current methods suffer from complex design and preparation of exogenous substrate, low reproducibility, and interference of cofactors. In this study, we developed a simple and precise high performance liquid chromatography (HPLC) method for the measurement of LCAT activity. By using 7-dehydrocholesterol (7-DHC) and 1,2-didecanoyl-sn-glycero-3-phosphocholine(10:0PC) as substrates, and an LCAT activating peptide (P642) as activator and emulsifier, the substrate reagent was easily made by vortex. The substrate reagent was mixed with serum samples (50:1, v/v) and incubated at 37 °C for 1 h. After incubation, the lipid was extracted with hexane and ethanol. With a conjugated double bond and ultraviolet absorption, 7-DHC and its esterification product could be separated and analyzed by a single HPLC run without calibration. LCAT activity was a linear function of the serum sample volume and the intra- and total assay coefficients of variation (CV) less than 2.5% were obtained under the standardized conditions. The substrate reagent was stable, and assay result accurately reflected LCAT activity. LCAT activities in 120 healthy subjects were positively correlated with triglyceride (P < 0.05), fractional esterification rate of HDL cholesterol (FERHDL) (P < 0.0001), and negatively correlated with apolipoprotein AI (apoAI) (P < 0.05) and HDL cholesterol (HDL-C) (P < 0.001). These results suggest that this method is sensitive, reproducible, and not greatly influenced by serum components and added substances, and will be a useful tool in the lipid metabolism study and the risk assessment of CVD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lecithin: cholesterol acyltransferase (LCAT, EC 2.3.1.43) is a key enzyme that hydrolyzes a fatty acid from phosphatidylcholine and transfers the fatty acid to unesterified cholesterol. This reaction is responsible for the formation of most of the cholesteryl esters found in human plasma. LCAT is believed to play a critical role in high-density lipoprotein (HDL) metabolism and the reverse cholesterol transport (RCT), a process that describes the HDL-mediated removal of excess cholesterol from macrophages in the arterial wall and subsequent delivery to the liver for biliary excretion. LCAT has been a subject of great interest in cardiovascular disease (CVD) research since its identification in 1962. However, the role of LCAT in the pathogenesis of human atherosclerosis and CVD is not yet understood [1]. Although CVD had been reported in familial LCAT deficiency (FLD) [2] or fish-eye disease (FED) [3] patients, in many cases, they did not develop clinically apparent diseases despite of very low HDL-C levels [4, 5]. Relationship between LCAT activity and CVD in general populations was explored and the results of some cross-sectional and prospective studies were also controversial. Sethiet et al. [6] compared CVD patients with age-, sex-, and HDL-C matched non-CVD subjects and found that CVD patients had significantly lower LCAT activity, and LCAT activity was a potentially useful diagnostic marker for CVD. Consistent with this result, lower levels of LCAT activity were also observed in patients with acute myocardial infarction [7]. However, in various studies, it is demonstrated that an increased LCAT is associated to CVD. An increase of LCAT activity did not predict low incidence of cardiovascular events [8] and even was reported to be associated with preclinical atherosclerosis in patients with metabolic syndrome [9]. Tanaka and coworkers prospectively studied 1927 Japanese individuals and followed up for 10.9 years, and the results showed increased LCAT activity, measured as serum cholesterol esterification rate, was a risk for coronary heart disease and sudden death [10].Other studies found that LCAT was not required for an efficient RCT and that low plasma LCAT concentrations or activities were not associated with increased atherosclerosis [11, 12]. Some of these apparent differences may be related to the multiple methods used for measuring LCAT activity, and LCAT activities from different methods and conditions may have different biological significance.
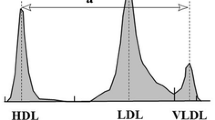
Serum LCAT activity could be measured by a variety of chemical and radiochemical methods by using either endogenous or exogenous substrates. The endogenous substrate methods were represented by cholesterol esterification rate in serum (CER) [13]or in apolipoprotein B-depleted HDL (FERHDL), which had been measured by an isotopic assay [14] or directly measure the decrease of free cholesterol [15]. Although both CER and FERHDL had been found to be associated with traditional risk factors and are predictors of CVD [10, 16], these methods were affected not only by LCAT amounts and activity but also the serum endogenous lipoprotein components; thus, they might not represent the true activity of LCAT. The most commonly used LCAT activity assay employed an artificial substrate, namely 14C-cholesterol loaded liposome made with phosphatidylcholine (PC), the LCAT activator apolipoprotein AI (apoAI) or LCAT-activating peptide P642, and many other substances such as 2-mecaptoethanol (ME), bovine serum albumin (BSA), lysophosphatidylcholine (LPC), and others [17,18,19]. These methods are sensitive and have provided important means in obtaining the majority of knowledge of LCAT mechanisms and function; however, they have several limitations. The preparations of the substrate are tedious always involving sonication or dialysis. Second, the various designs and complicated compositions of the enzymatic reaction systems do not readily distinguish influences of the enzyme from those of the substrate, cofactors, and products. Third, measurement of sterol esterification by liquid scintillation is unsafe and is not convenient in clinical laboratories. Therefore, to elucidate the role of LCAT in HDL metabolism and CVD, a manageable, accurate, and reproducible assay of LCAT enzymatic activity is required.
In this study, we select 7-dehydrocholesterol (7-DHC) as the cholesterol analogue, 1,2-didecanoyl-sn-glycero-3-phosphocholine(10:0PC) as the acyl donor for the LCAT reaction, and a synthetic peptide (P642) for the LCAT activator. With conjugated double bonds, 7-DHC allows determination of its esterification by a simple and highly precise two component normalization method without the need of calibration and internal standard. Compared to long-chain phosphatidylcholines, the 7-dehydrocholesteryl decanoate product had a relatively short retention time, thereby enabling a shorter HPLC assay time. The apoAI mimetic peptide, P642 forms stable lipid complexes that could effectively react with LCAT. In addition, the assay reagent is stable, readily available, and easily prepared. The application of this method on 120 healthy patients verified that this method is simple and precise and is essential for estimating the serum LCAT activity for clinical significance in various diseases.
Materials and methods
Equipment, chemicals, and serum sample
The HPLC analyses was performed on a 1200 HPLC system (Hewlett Packard, Waldbronn, Germany) consisting of an isocratic pump, an autosampler, and an ultraviolet detector controlled by the ChemStation. 7-DHC was obtained from Sigma (St. Louis, MO, USA). PCs containing carboxylic acid residues of 6 to14 carbon atoms (6:0PC, 8:0PC, 10:0PC, 12:0PC, and 14:0PC) were purchased from Avanti Polar Lipids (Alabaster, AL, USA). P642 was obtained from SBS Genetech Co., Ltd. (Beijing, China) as a custom synthesis of l-amino acids in the sequence PVLDLFRELLNELLEALKQKLK. HPLC-grade acetonitrile, isopropanol, and n-hexane were purchased from Fisher Scientific (Pittsburgh, PA, USA). Other chemical reagents were from Beijing Chemical Works, China.
For method development, study of LCAT activities in healthy volunteers, 120 apparently healthy subjects were recruited and individual blood samples were taken and sera were separated within 2 h of collection. Serum was aliquoted and stored in − 80 °C until analysis. This study was reviewed and approved by the Beijing Hospital Ethics Committee. All studied individuals were informed in writing of the intended use of their samples and each provided written consent.
Optimization of enzymatic substrate and reaction conditions
7-DHC, a 3β-hydroxysterol with conjugated double bond and ultraviolet absorption, was chosen as the cholesterol mimetic substrate. P642, a commercially synthesized peptide, was used instead of apoAI as the LCAT activator. For selection of a suitable phospholipid, the reaction substrates were prepared by mixing 7-DHC and phosphatidylcholines with fatty acid chain of 6–14 carbon atoms, respectively, and incubated with a mixed serum sample for 1 h. To examine the effect of the molar ratios of the substrates on serum LCAT activity, 7-DHC and 10:0PC were mixed at a molar ratio of 1:2, 1:4, and 1:8, and incubated with a mixed serum for 0–6 h, respectively. To determine the optimal P642 concentration, 7-DHC and 10:0PC were mixed at a molar ratio of 1:8, in the presence of P642 at final concentrations of 0, 5,10, 20, 40, 60 and 80 mg/dL, and incubated with two serum samples at 37 °C for 1 h, respectively. To determine serum volume, 0.5 mL of the substrate solution was incubated with 0, 2.5, 5, 10, 15 and 20 μL serum sample, and incubated at 37 °C for 1 h. After incubation, the above reactions were stopped by placing the tubes into ice water bath, lipid was extracted by hexane and ethanol, and the esterification rates of 7-DHC in each of the experiments were analyzed by HPLC. In addition, the lipid extraction efficiencies of 7-DHC and its ester were evaluated by vortexing the reaction mixture with ethanol and hexane for 0, 2.5, 5, 10, 20, and 30 min and the recoveries of 7-DHC, 7-DHC ester as well as 7-DHC esterification rates were compared. Finally, to determine the time course of 7-DHC esterification, aliquots of serum samples were incubated with the substrate reagent at 37 °C for periods of 0 (directly put into an ice water bath), 1, 2, 4, 6, and 8 h, respectively, and esterification rates of 7-DHC were measured. Esterification of cholesterol in serum samples in the reaction system was also measured by our previously reported HPLC method [15].
Preparation of the substrate reagent
The reaction substrate was prepared by combining 6 mg of 7-DHC and 70 mg of 10:0PC, dissolved in 1 mL of ethanol. Solvents were removed by evaporation under a stream of nitrogen. After adding 40 mg of P642, the dried mixture was dispersed in 10 mL of 50 mmol/L Tris-HCl buffer (pH = 7.5), vortexed for 2 min, and a clear solution was obtained. The solution was diluted with the same buffer to the total volume of 100 mL to obtain a final 7-DHC concentration of 0.156 mmol/L and mole ratio composition of 1:8:1 for 7-DHC/10:0PC/P642. The substrate solution was aliquoted and stored at − 80 °C until use.
Measurement of LCAT activity
The LCAT substrate, serum samples, and quality control samples (QCs) were thawed. 0.5 mL substrate was aliquoted to the pre-cooled tubes in the ice water bath. Ten microliters of the serum samples and QCs were added to the tubes, mixed, and incubated at 37 °C water bath for 1 h. The tubes were then placed back into the ice water bath and 0.5 mL of ethanol and 1 mL of hexane were added. After vortexing for 20 min, an aliquot of 0.5 mL of the hexane phase was transferred to another tube and dried under a stream of nitrogen and reconstituted with 0.3 mL mobile phase (acetonitrile/isopropanol, 50:50). Twenty microliters of the reconstituted solution was injected onto a Nova-Pak C18 column (5 μm, 3.9 mm × 150 mm), eluted with the mobile phase, and detected at 280 nm. The esterification rate was represented by the percentage of 7-DHC ester peak area in those of the sum of 7-DHC and the ester. The LCAT activity was expressed as nKat/L and was calculated by the following equation.
C is concentration (nmol/L) of 7-DHC in the substrate reagent before the start of the reaction; V1 is the volume (L) of the substrate; R is the fraction of 7-DHC ester after the reaction (%); V2 is the volume of serum (L) in the reaction system; and T is the reaction time (s).
Precision and stability of the LCAT substrate reagent
To evaluate the precision of the method, LCAT activities of three serum samples were measured in three runs in triplicate. Intro- and total run imprecisions were analyzed. To evaluate the stability of the substrate reagent, LCAT activities were measured after storage of the substrate for different time period at both 4 °C and room temperature (RT). Substrate reagent was divided into 2.5 mL aliquots and stored at 4 °C for 0, 6, 12, 24, 48, and 96 h and at RT for 0, 2, 4, 8, 12 and 24 h, respectively, and then LCAT activities of two serum samples were measured in duplicate by using these substrates and the results were compared.
LCAT activity in healthy subjects
The developed LCAT assay was applied to 120 apparently healthy volunteers, 51 males and 69 females, aged from 19 to 72 years. Body weight, height, and blood pressure were measured. Serum total cholesterol (TC), triglyceride (TG), apoAI, apoB, and high sensitivity C-reactive protein (hs-CRP) were analyzed by assay kits from Sekisui Medical Technologies (Osaka, Japan) on a Hitachi 7180. LCAT mass was measured by ELISA kit from BioVender (Brno, Czech Republic) and FERHDL by our previously established HPLC method [15]. The correlations between LCAT activity and other continuous risk factors were assessed using nonparametric Spearman correlation analyses. Statistical data analysis was performed using the SPSS software, version 22 (IBM Corporation, Armonk, NY, USA). The reported P values are two-tailed, and statistical significance was defined at a P value < 0.05.
Results
Selection of the LCAT substrate
7-DHC is cholesterol like sterol with a conjugated double bond and has maximum ultraviolet absorption at 280 nm. HPLC chromatograms of 7-DHC and the esterification product with 10:0PC before and after enzymatic reactions are presented in Fig. 1, and those with other phosphatidylcholines are shown in the Electronic Supplementary Material (ESM), Fig. S1. The results showed that before incubation, no esterified 7-DHC was observed (Fig. 1a). After incubation, 7-DHC and the respective esters could be separated and detected. The retention times of 6:0PC, 8:0PC, 12:0PC, and 14:0PC esters were approximately 3.8, 4.8, 12.0, and 13.5 min, respectively. Compared to 10:0PC, the esterification rates of 8:0PC and 6:0PC were lower, and the retention times of 12:0PC and 14:0PC esters were longer; thus, 10:0PC was selected as the PC substrate. UV spectra for 7-DHC and 7-DHC ester complex as well as the LC/MS identification of 7-DHC ester are shown in ESM Figs. S2 and S3, respectively. As shown in Fig. 2, the 7-DHC esterification rate increased with increased molar ratio of 10:0PC to 7-DHC. The relationship between P642 and LCAT activity is presented in Fig. 3, the result indicated that LCAT activities were increased by P642 in the concentration range of 0–20 mg/dL, but kept nearly unchanged at 20–80 mg/dL. Therefore, the molar ratio of 7-DHC to 10:0PC of 1:8 and P642 concentration of 40 mg/dL were chosen in our study. The final concentrations of 7-DHC, 10:0PC, and P642 in the substrate reagent were 6, 70, and 40 mg/dL (0.156, 1.238, and 0.152 mmol/L), respectively, with molar ratios of 1:8:1.
HPLC chromatogram of 7-dehydrocholesterol and its esterification products with phosphatidylcholines 10:0. 0.5 mL of LCAT substrate was mixed with 10 μL serum sample and incubated at 37 °C for 0 (a) and 1 h (b), respectively. After incubation, lipid was extracted with hexane and ethanol, evaporated, reconstituted with mobile phase, and analyzed by HPLC, and both 7-DHC (1) and its ester (2) can be analyzed in one run without the need of calibrators and internal standard. Chromatographic conditions were as follows: column, Nova-Pak C18 (5 nm, 3.9 mm × 150 mm); mobile phase, acetonitrile/isopropanol (50:50); flow-rate, 1 mL/min; detection, ultraviolet absorbance at 280 nm
Effect of different 7-DHC and phosphatidylcholine molar ratios on LCAT activity. 7-DHC and 10:0PC were mixed at a molar ratio of 1:2, 1:4, and 1:8, respectively, in the presence of P642. 0.5 mL of the substrates were mixed with 10 μL serum sample and incubated at 37 °C for 0 (in iced water bath), 1, 2, 4, and 6 h. After incubation, lipid was extracted by hexane and ethanol, evaporated and reconstituted with acetonitrile/isopropanol (50:50), and analyzed by HPLC. Means and error bars (SD) of triplicate measurements are shown
Effects of P642 concentrations on serum LCAT activity. Ten microliters of two serum samples was mixed with the reaction substrate at a ratio of 1:50 (v/v), in the presence of P642 at final concentration of 0, 5, 10, 20, 40, 60, and 80 mg/dL, respectively, and incubated at 37 °C for 1 h. The reaction mixture was extracted with hexane and ethanol, evaporated, reconstituted with acetonitrile/isopropanol (50:50), and analyzed by HPLC. Means and error bars (SD) of two runs each in duplicate measurements are shown
Serum volume, lipid extraction, and the enzymatic reaction
The relationship between serum volumes and the esterification rates of 7-DHC is shown in Fig. 4. Linear dose-response curve was derived in the range of 0–20 μL serum samples. In this method, the serum volume of 10 μL was chosen and the ratio of the substrate to serum was 50:1. The efficiency of lipid extraction was shown by ESM Fig. S4. The recoveries of 7-DHC and 7-DHC ester as well as ratios were increased from 0 to 10 min vortex and then stabilized from 10 to 30 min vortex. Therefore, 20 min vortex was sufficient for extraction of the lipid and for the calculation of 7-DHC esterification. By using the procedures described in this study, the time courses of two individual serum samples was examined and the results were presented in ESM Fig. S5. Moreover, the esterification of 7-DHC and serum cholesterol was almost linearly correlated (EMS Fig. S6), suggesting that 7-DHC esterification could accurately reflect LCAT enzyme activity and was not significantly affected by the endogenous serum lipids (ESM Fig. S7).
Serum LCAT activity as a function of serum volume. Various volumes of fresh serum were used as specimen and incubated with 0.5 mL of LCAT reaction substrate at 37 °C for 1 h. The reaction mixture was extracted with hexane and ethanol, evaporated, reconstituted with acetonitrile/isopropanol (50:50), and analyzed by HPLC. Means and error bars (SD) of triplicate measurements are shown
Assay imprecision and substrate stabilities
Intra-run and total assay imprecisions of three individual serum samples and two control samples are shown in Table 1. For the individual samples, LCAT activity was measured in three runs with triplicate measurements in each run. For the control samples, LCAT was analyzed in 10 runs. The intra- and total analytical imprecisions were less than 2.5%, demonstrating an excellent precision. As shown in ESM Fig. S8, LCAT activities of the serum samples did not change significantly after the storage of the substrate reagent at RT for 24 h and at 4 °C for 96 h (4 days), indicating good stability of the substrate reagent.
Determination of LCAT activity in healthy volunteers
LCAT activities in 120 healthy subjects were normally distributed with mean (± SD) values of 25.13 ± 7.44 nKat/L. No significant difference was found between males (25.03 ± 7.35 nKat/L) and females (25.20 ± 7.55 nKat/L). As shown in Table 2, LCAT activity was positively correlated with body mass index (BMI, r = 0.284, P < 0.001), TG (r = 0.259, P < 0.05), hs-CRP (r = 0.273, P < 0.05), while negatively correlated with HDL-C (r = − 0.320, P < 0.001) and apoAI (r = − 0.225, P < 0.05). In addition, significant positive associations were observed between LCAT activity and FERHDL (r = 0.521, P < 0.0001), measured by endogenous substrate method in apoB depleted HDL fractions, and LCAT mass (r = 0.503, P < 0.0001) measured by a commercial ELISA kit (ESM Fig. S9).
Discussion
Substrate components and the preparation process are important for LCAT activity measured by exogenous substrates. The substrates of LCAT, cholesterol and phosphatidylcholine, are both water insoluble, so a liposome needs to be prepared for LCAT reaction. These hydrophobic substrates will form phospholipid bilayer vesicles in the aqueous phase with sterol intercalated throughout the bilayer. LCAT reacts relatively slowly with such vesicular substrate; therefore, the natural LCAT activator apoAI is traditionally included in the mixture. Other substances such as ME, BSA, and LPC, which have been confirmed to have effects on LCAT activity [17,18,19,20], are also used in most of the assays to further activate LCAT or stabilize the substrate solution. In this study, the substrate solution contained only a sterol, a PC, and P642, an inexpensive and commercially reproducible substitute of apoAI. P642 has been demonstrated to form stable lipid complexes and react with LCAT as efficient as reconstituted HDL preparations formed from apoAI, PC, and cholesterol [19,20,21]. Preparation of the substrate reagent was simple and clear solution could be easily obtained by a brief vortex for 2 min.
Both the reaction and detection of sterol esterification are dependent on the forms of the sterol and PC used in the substrates. Sterols of a wide range of structures and composition are accepted as substrates for LCAT esterification, with a critical requirement of β conformation of the 3-hydroxyl group [22]. The most commonly used assays employ substrate composed of isotopic 14C-labeled cholesterol as the LCAT substrate, and the reaction are detected by the liquid scintillation counting [17, 19], which is unsafe and not suitable for clinical applications. Other methods use fluorescent sterol and sterol esterification is detected by fluorescence reader [21]. Both liquid scintillation counting and fluorescent measurement are not as precise as chromatography measurement. In another variant, LCAT is estimated by enzymatically or chromatographically measuring the decrease in unesterified cholesterol after incubation of serum with liposomes [18, 23]; however, large variations might occur because cholesterol measurement needs to be performed twice and the changes of cholesterol are too small. In our study, 7-DHC was selected for the assay because of its ultraviolet absorption properties with the expectation that as a 3β-hydroxy sterol it was suitable for LCAT reaction [22]. By using 7-DHC as the sterol substrate, it was possible to analyze both 7-DHC and its ester by HPLC in one run without the need of calibrators and internal standard. Although7-DHC and 10:0PC might not be the physiological substrate for LCAT, and LCAT had different ability to esterify 7-DHC and cholesterol, our results showed that the esterification rate of 7-DHC was almost linearly correlated with that of serum cholesterol (r = 0.99) in the reaction system. The HPLC run time was only 6 min, when 10:0PC was used as the phosphatidylcholine substrate. Using this artificial substrate LCAT activity could be accurately reflected. The esterification rate was calculated by comparing 7-DHC peak area to the sum of 7-DHC and its ester, and LCAT activity was presented by the unit nKat/L, nanomolar of esterified 7-DHC by 1 L of serum in 1 s incubation at 37 °C. Under the defined conditions, the extent of 7-DHC esterification was about 1%, which was much lower compared to the previous methods (10–30%) [17,18,19]. The low esterification rate helped to minimize the effect of substrate consumption and product inhibition.
Validation of the method demonstrated that, although the reaction was not linear, the velocity did not change significantly during the incubation period within 8 h. LCAT activity was linearly correlated with serum volume and LCAT amount. The intra- and total analytical imprecisions were less than 2.5%, which were much lower than the previous reports by isotopic, enzymatic, and fluorescence measurements [15, 17,18,19, 23]. The satisfactory precision was achieved by the highly reproducible ultraviolet (UV) detector and the direct comparison of the peak area of 7-DHC and ester within one chromatogram without the need of calibration. Moreover, the prepared substrate reagent was stable at RT for 24 h and at 4 °C for 96 h (4 days). We observed the two quality control materials to be stable at − 80 °C for at least 1 year. The homogeneity and stability of the substrate reagent also contributed to the high precision of the method.
Serum LCAT has been represented by LCAT activity (as measured by the exogenous substrates), LCAT mass (which strongly correlate with LCAT activity), and cholesterol esterification rate (CER or FERHDL). CER and FERHDL have been proved to be significantly correlated with atherosclerotic dyslipidemia [24] and are predictors of coronary heart disease [16, 25]and sudden death [10], while the relationships between LCAT activity/mass and CVD are controversial. In many of the previous studies, LCAT activity/mass were reported to be significantly positively correlated with BMI [26], TC [7, 8, 26], low-density lipoprotein cholesterol (LDL-C) [7], and triglycerides [8, 9] and negatively correlated with HDL-C [9, 26] or no correlations existed [7, 12]. However, opposite associations between LCAT mass/activity and HDL-C were also reported [11, 27]. In the results of 120 healthy volunteers, LCAT activity was positively correlated with BMI, TG, hs-CRP, and negatively correlated with HDL-C and apoAI. This finding, along with some of the previous data, did not support the presumed concept that LCAT was the driving force in HDL metabolism and RCT. In fact, several recent studies in CVD patients indicated that LCAT might be proatherogenic [8, 9, 12, 27,28,29], especially in women. Therefore, further investigation is required to establish the exact role of LCAT in the development of atherosclerosis. In addition, in agreement with the previous studies [26, 30], we found LCAT activity was significantly positively associated with both LCAT mass and FERHDL.
In conclusion, by using 7-DHC, 10:0PC and P642 as the LCAT substrate components, an HPLC method for the measurement of LCAT activity has been developed. This method is simple, precise, and reliable and may provide an important role in clarifying the exact role of LCAT in lipoprotein metabolism as well as risk assessment of CVD.
Abbreviations
- CER:
-
Cholesterol esterification rate
- CVD:
-
Cardiovascular diseases
- FC:
-
Free cholesterol
- FERHDL :
-
Fractional esterification rate of HDL cholesterol
- HDL:
-
High-density lipoprotein
- HDL-C:
-
HDL cholesterol
- LCAT:
-
Lecithin/cholesterol acyltransferase
- PC:
-
Phosphatidylcholine
- P642:
-
LCAT-activating peptide
- RCT:
-
Reverse cholesterol transport
- 7-DHC:
-
7-Dehydrocholesterol
References
Toth PP, Barter PJ, Rosenson RS, Boden WE, Chapman MJ, Cuchel M, et al. High-density lipoproteins: a consensus statement from the National Lipid Association. J Clin Lipidol. 2013;7(5):484–525.
Scarpioni R, Paties C, Bergonzi G. Dramatic atherosclerotic vascular burden in a patient with familial lecithin-cholesterol acyltransferase (LCAT) deficiency. Nephrol Dial Transplant. 2008;23(3):1074. author reply 1074-1075
Kuivenhoven JA, van Voorst tot Voorst EJ, Wiebusch H, Marcovina SM, Funke H, Assmann G, et al. A unique genetic and biochemical presentation of fish-eye disease. J Clin Invest. 1995;96(6):2783–91.
Schwartz GG, Olsson AG, Abt M, Ballantyne CM, Barter PJ, Brumm J, et al. Effects of dalcetrapib in patients with a recent acute coronary syndrome. N Engl J Med. 2012;367(22):2089–99.
Boden WE, Probstfield JL, Anderson T, Chaitman BR, Desvignes-Nickens P, Koprowicz K, et al. Niacin in patients with low HDL cholesterol levels receiving intensive statin therapy. N Engl J Med. 2011;365(24):2255–67.
Sethi AA, Sampson M, Warnick R, Muniz N, Vaisman B, Nordestgaard BG, et al. High pre-beta1 HDL concentrations and low lecithin:cholesterol acyltransferase activities are strong positive risk markers for ischemic heart disease and independent of HDL-cholesterol. Clin Chem. 2010;56(7):1128–37.
Dullaart RP, Tietge UJ, Kwakernaak AJ, Dikkeschei BD, Perton F, Tio RA. Alterations in plasma lecithin:cholesterol acyltransferase and myeloperoxidase in acute myocardial infarction: implications for cardiac outcome. Atherosclerosis. 2014;234(1):185–92.
Dullaart RP, Perton F, van der Klauw MM, Hillege HL, Sluiter WJ. High plasma lecithin:cholesterol acyltransferase activity does not predict low incidence of cardiovascular events: possible attenuation of cardioprotection associated with high HDL cholesterol. Atherosclerosis. 2010;208(2):537–42.
Dullaart RP, Perton F, Sluiter WJ, de Vries R, van Tol A. Plasma lecithin:cholesterol acyltransferase activity is elevated in metabolic syndrome and is an independent marker of increased carotid artery intima media thickness. J Clin Endocrinol Metab. 2008;93(12):4860–6.
Tanaka S, Yasuda T, Ishida T, Fujioka Y, Tsujino T, Miki T, et al. Increased serum cholesterol esterification rates predict coronary heart disease and sudden death in a general population. Arterioscler Thromb Vasc Biol. 2013;33(5):1098–104.
Calabresi L, Baldassarre D, Simonelli S, Gomaraschi M, Amato M, Castelnuovo S, et al. Plasma lecithin:cholesterol acyltransferase and carotid intima-media thickness in European individuals at high cardiovascular risk. J Lipid Res. 2011;52(8):1569–74.
Holleboom AG, Kuivenhoven JA, Vergeer M, Hovingh GK, van Miert JN, Wareham NJ, et al. Plasma levels of lecithin:cholesterol acyltransferase and risk of future coronary artery disease in apparently healthy men and women: a prospective case-control analysis nested in the EPIC-Norfolk population study. J Lipid Res. 2010;51(2):416–21.
Marcel YL, Vezina C. A method for the determination of the initial rate of reaction of lecithin:cholesterol acyltransferase in human plasma. Biochim Biophys Acta. 1973;306(3):497–504.
Dobiasova M, Adler L, Ohta T, Frohlich J. Effect of labeling of plasma lipoproteins with [(3)H]cholesterol on values of esterification rate of cholesterol in apolipoprotein B-depleted plasma. J Lipid Res. 2000;41(8):1356–7.
Dong J, Yu S, Yang R, Li H, Guo H, Zhao H, et al. A simple and precise method for direct measurement of fractional esterification rate of high density lipoprotein cholesterol by high performance liquid chromatography. Clin Chem Lab Med. 2014;52(4):557–64.
Frohlich J, Dobiasova M. Fractional esterification rate of cholesterol and ratio of triglycerides to HDL-cholesterol are powerful predictors of positive findings on coronary angiography. Clin Chem. 2003;49(11):1873–80.
Chen CH, Albers JJ. Characterization of proteoliposomes containing apoprotein A-I: a new substrate for the measurement of lecithin:cholesterol acyltransferase activity. J Lipid Res. 1982;23(5):680–91.
Manabe M, Abe T, Nozawa M, Maki A, Hirata M, Itakura H. New substrate for determination of serum lecithin:cholesterol acyltransferase. J Lipid Res. 1987;28(10):1206–15.
Vaisman BL, Remaley AT. Measurement of lecithin-cholesterol acyltransferase activity with the use of a peptide-proteoliposome substrate. Methods Mol Biol. 2013;1027:343–52.
Fielding CJ, Shore VG, Fielding PE. Lecithin:cholesterol acyltransferase: effects of substrate composition upon enzyme activity. Biochim Biophys Acta. 1972;270(4):513–8.
Homan R, Esmaeil N, Mendelsohn L, Kato GJ. A fluorescence method to detect and quantitate sterol esterification by lecithin:cholesterol acyltransferase. Anal Biochem. 2013;441(1):80–6.
Piran U, Nishida T. Utilization of various sterols by lecithin-cholesterol acyltransferase as acyl acceptors. Lipids. 1979;14(5):478–82.
Bartholome M, Niedmann D, Wieland H, Seidel D. An optimized method for measuring lecithin:cholesterol acyltransferase activity, independent of the concentration and quality of the physiological substrate. Biochim Biophys Acta. 1981;664(2):327–34.
Dobiasova M, Frohlich J, Sedova M, Cheung MC, Brown BG. Cholesterol esterification and atherogenic index of plasma correlate with lipoprotein size and findings on coronary angiography. J Lipid Res. 2011;52(3):566–71.
Liu J, Yang R, Zhou M, Mao W, Li H, Zhao H, et al. Fractional esterification rate of cholesterol in high-density lipoprotein associates with risk of coronary heart disease. Lipids Health Dis. 2017;16(1):162.
Albers JJ, Chen CH, Adolphson JL. Lecithin:cholesterol acyltransferase (LCAT) mass; its relationship to LCAT activity and cholesterol esterification rate. J Lipid Res. 1981;22(8):1206–13.
Tani S, Takahashi A, Nagao K, Hirayama A. Association of lecithin–cholesterol acyltransferase activity measured as a serum cholesterol esterification rate and low-density lipoprotein heterogeneity with cardiovascular risk: a cross-sectional study. Heart Vessel. 2015;31(6):831–40.
Hovig T, Gjone E. Familial plasma lecithin:cholesterol acyltransferase (LCAT) deficiency. Ultrastructural aspects of a new syndrome with particular reference to lesions in the kidneys and the spleen. Acta Pathol Microbiol Scand A Pathol. 1973;81(5):681–97.
Wells IC, Peitzmeier G, Vincent JK. Lecithin:cholesterol acyltransferase and lysolecithin in coronary atherosclerosis. Exp Mol Pathol. 1986;45(3):303–10.
Kobori K, Saito K, Ito S, Kotani K, Manabe M, Kanno T. A new enzyme-linked immunosorbent assay with two monoclonal antibodies to specific epitopes measures human lecithin-cholesterol acyltransferase. J Lipid Res. 2002;43(2):325–34.
Acknowledgments
This study was supported by research grants from the National Natural Science Foundation of China (81472035, 81171647, 81501842).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was reviewed and approved by the Beijing Hospital Ethics Committee. All studied individuals were informed in writing of the intended use of their samples and each provided written consent.
Conflict of interest
No authors declared any potential conflicts of interest. The funding organizations played no role in the design of the study, review and interpretation of data, or preparation or approval of the manuscript.
Electronic supplementary material
ESM 1
(PDF 506 kb).
Rights and permissions
About this article
Cite this article
Wang, Y., Wang, S., Zhang, L. et al. A simple and precise method to detect sterol esterification activity of lecithin/cholesterol acyltransferase by high-performance liquid chromatography. Anal Bioanal Chem 410, 1785–1792 (2018). https://doi.org/10.1007/s00216-017-0834-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00216-017-0834-4