Abstract
During the last 30 years, the artificial increase of red blood cell volume (“blood doping”) has changed the level of performance in all endurance sports. Many doping scandals have shown the extent of the problem. The detection of blood doping relies on two different approaches: the direct detection of exogenous manipulating substances (erythropoietic stimulants) or red cells (homologous transfusion) and the indirect detection, where not the doping substance or technique itself, but its effect on certain biomarkers is measured. Whereas direct detection using standard laboratory procedures such as isoelectric focusing can identify erythropoietic stimulants, homologous blood transfusion is identified through mismatches in minor blood group antigens by flow cytometry. Indirect methods such as the athlete biological passport are the only means to detect autologous transfusion and may also be used for the detection of erythropoietic stimulants or homologous transfusion. New techniques to unmask blood doping include the use of high-throughput ‘omics’ technologies (proteomics/metabolomics) and the combination of different biomarkers with the help of mathematical approaches. Future strategies should aim at improving the use of the available data and resources by applying pattern recognition algorithms to recognize suspicious athletes and, on the basis of these findings, use the appropriate testing method. Different types of information should be combined in the quest for a forensic approach to anti-doping.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The oxygen carrying capacity of the organism has been addressed as performance limiting in most endurance sport disciplines. From basic physiology, it is known that the oxygen transport of the body is mediated through cardiac output and hemoglobin, both entities being key factors in the Fick principle, which defines oxygen uptake. One of the prime training targets for endurance athletes is therefore to increase their oxygen uptake and thereby increase their cardiac output and the oxygen carrying capacity of the blood. It is well known that regular endurance training leads to enlargement of the cardiac cavities and thus cardiac output and, on the other hand, induces an increase in red cell volume, which will improve the oxygen transport [1]. However, these adaptations are slow, require dedicated training over many years, and there is a high interindividual difference in the ability to adapt to training. Thus, athletes and coaches have searched for possibilities to bypass these natural adaptations. It is well known that hypoxia will accelerate red cell production and thus increase red cell volume [2] so that altitude training and different other types of hypoxic interventions are nowadays standard training strategies for most elite athletes competing in endurance events.
In light of the inventive spirit of human nature, it was clear that sooner or later athletes would seek artificial means to increase their oxygen transport capacity without having to go through the cumbersome and time-consuming process of hypoxic training. From a scientific point of view, the experiments laying the base for a beneficial effect of increased red cell mass stem from military investigations, which demonstrated that the infusion of red cells had the same physiological effects as the adaptation of the erythropoietic system to the hypoxia of altitude and that the “tolerance” of hypoxia (measured through heart rate response to exercise) was improved in the transfused subjects [3, 4]. In the following decades, this topic was further developed with additional investigations that showed a beneficial effect of increased red cell volume on endurance performance [5–7]. The positive effect of increased red cell volume depended on the amount of transfused red cells with increases in VO2max of up to 17 %.
Obviously, it was not long until these scientific findings had spread to the world of sports and Lasse Viren, a Finnish long distance runner who won gold medals at the 1972 and 1976 Olympic Games in the 5,000 m and 10,000 m, is believed to be among the first athletes to have used blood transfusions to improve performance. It should be noted that this technique was not banned at the time and although the ethical debate on the topic was in full swing [8], it was only in 1986 that the International Olympic Committee banned blood transfusions. Other than the anecdotal evidence from the Nordic distance runners, there are other reports on more systematic use of transfusions in the context of major sporting events in the 1980s. Notably, it is well established that a large part of the US cycling team was involved in a systematic blood doping program that earned them unprecedented success at the 1984 Olympic Games in Los Angeles [9]. There is also some evidence that blood transfusions were an integral part of the doping regime used for the enhancement of performance for athletes from the Eastern bloc (Soviet Union, East Germany) at that time. Nevertheless, it can be assumed that because of the logistic requirements of blood withdrawal and reinfusion, the technique was not widespread, as the technical necessities were only available to a small number of athletes, but nevertheless available to certain elite athletes.
This changed dramatically with the commercial introduction of recombinant human erythropoietin (rhEPO), the human hormone that regulates the erythropoietic system in the organism. EPO was first isolated in the 1950s and was synthesized in 1985. Commercial rhEPO was marketed throughout the world between 1987 and 1989. Studies investigating the effect of rhEPO on performance were soon published and demonstrated positive effects on maximal oxygen uptake of 6–12 % [10]. Although the authorities rapidly banned rhEPO, the easy access to the substance and the huge impact on performance resulted in widespread abuse of rhEPO during the 1990s/2000s. It is believed that this substance had a considerable impact on the development of peak performances in all endurance sports during these years and there are even scientific attempts to prove this for several sports on the basis of performance analysis [11, 12]. The abuse was facilitated by the fact that no detection method was readily available at that time. From a practical point of view, the impact of rhEPO on performance in endurance sports is best illustrated by a quote from Greg Lemond, an American cyclist who won the Tour de France in 1986 and 1989, i.e., before rhEPO became available, recalling the 1991 race: “I was the fittest I had ever been, my split times in spring training rides were the fastest of my career, and I had assembled a great team around me. But something was different in the 1991 Tour. There were riders from the previous years who couldn’t stay on my wheel who were now dropping me even on modest climbs.” These words accurately describe how rhEPO changed the entire world of endurance sport in the following decades and divided the athletes’ performance primarily between rhEPO users and non-users.
Logically, following widespread abuse from the 1990s onwards, doping scandals involving rhEPO or blood transfusions have shaken the world of sport on a regular basis, culminating recently with the investigation of Lance Armstrong, who subsequently admitted the use of both rhEPO and blood transfusions throughout his career. Although, it is therefore common belief that many recent doping cases were not unveiled by conventional anti-doping testing, but rather by police investigations or admissions from athletes or staff, thus non-analytical approaches, anti-doping laboratories were able to detect about 400 cases testing positive for rhEPO between 2003 and 2011 (World Anti-Doping Agency (WADA) statistics). Analytics have therefore come a long way in the detection of blood manipulation in sports and still outperform police investigations by 10 to 1.
The present review retraces the challenging journey of the detection of blood manipulation and the different methodical approaches that have been used over the years to unmask the abuse of blood transfusions and erythropoietic stimulating agents (ESA).
Direct detection of erythropoietic stimulating agents
Recombinant erythropoietin and derivates
Direct detection of a forbidden substance in a biological matrix such as urine or blood obtained from an athlete is the classical forensic approach to prove doping. This approach has long been the sole strategy, only fine-tuned by improving the sensitivity of the analytical detection methods and by optimizing the timing of testing. The basic principle of the direct detection of forbidden substances relies on the fact that these substances are different from the normal constituents of the human organism. With the introduction of recombinant drugs such as rhEPO, this principle was not valid anymore, as the recombinant constituent was virtually identical to the endogenous version of the substance. Thus, at first, doping tests could not differentiate between the natural, endogenous and the artificial, exogenous recombinant version of the drug. This has, for a long time, been a major difficulty for the testing laboratories. In 1995, Wide et al. described a method to separate the natural from exogenous EPO through electrophoresis, but other laboratories could never replicate their results and the described method never reached the stage of validation. Only in 2000, thus more than 10 years after the estimated beginning of rhEPO abuse in sports, the first practicable and validated test to directly detect rhEPO in urine was published by Lasne et al. [13, 14]. This test relied on a difference in glycosylation between the endogenous and the exogenous EPO molecules, which resulted in different migration characteristics during isoelectric focusing (IEF) (Fig. 1, reprinted from [15]). The recombinant EPO was industrially harvested from transfected hamster kidney or ovarian cells and, owing to the difference in cell organelles, a minor posttranslational difference in glycosylation between the rhEPO (made by the hamster cells) and the endogenous EPO (made by the human kidney cells) occurred, although the amino acid sequence is identical. The rhEPO molecules are less negative and will thus move differently from endogenous EPO in an electric field, which can be demonstrated using the IEF. Further developing the approach of Wide, IEF is then followed by double blotting, which addresses the problem of non-specific binding of the EPO molecules. Although relatively cumbersome, the method soon identified the first athletes testing positive, namely Roland Meier and Bo Hamburger, both cyclists. Ironically, Hamburger was later acquitted by the court of arbitration of sports on formal grounds (i.e., a lack of harmonization of the positivity criteria for the EPO tests between laboratories was identified). This issue has since been addressed and strict positivity criteria apply, based on acceptance, identification, and stability principles. rhEPO positive samples, for example, have to show at least three acceptable, consecutive bands (labeled 1–3 in Fig. 1) in the basic area and the two most intense bands measured by densitometry must be in the basic area. When the analysis is performed in blood (serum/plasma) the intensity of those bands must be approximately twice or more than any band in the endogenous area [15]. Many laboratories nowadays use computer-based classification algorithms to guarantee objectivity in this context (GASEpo) [16].
IEF of different erythropoietins. rEPO recombinant EPO, uEPO endogenous standard. (Reprinted with permission from WADA technical document [15])
The detection window for rhEPO is known to be relatively short and depends on the dosage and the method of administration: Whereas subcutaneous administration of rhEPO in clinical dosages (e.g., 50 IU/kg body weight) might be detected over several days, it has been demonstrated that intravenous administration and microdosing (i.e., 500 IU) are virtually undetectable while still producing a measurable erythropoietic effect [17].
In order to blur the IEF picture, athletes nowadays use mixtures of different rhEPO, knowing that these will produce uncharacteristic patterns which will have difficulties in meeting the positivity criteria for positive rhEPO tests set by WADA.
To overcome this limitation and other sampling-related problems such as bacterial degradation or exercise-associated proteinuria [18, 19], which might interfere with IEF results, another method for the detection of EPO misuse, SDS/SAR-PAGE (sodium dodecyl sulfate/sarcosyl polyacrylamide gel electrophoresis) was developed [20, 21]. This method relies on the difference in molecular weight of the different types of EPO and is able to identify different rhEPO variants. With rhEPO being one of the commercially most successful drugs developed over recent decades, many biosimilars were marketed in different countries (epoietin α, δ, κ, ξ, ω etc.) [22]. As these biosimilars are also slightly different in their molecular mass (because they originate from different transfected cells), they are detectable by the same testing principles of SDS-PAGE. Even substances with modified molecular structure such as darbepoietin (Aranesp) or CERA (continuous erythropoietin receptor activator, Mircera), developed to have a longer half-life in the organism, can be detected, as they usually contain a conventional epoietin backbone paired with another component to slow its excretion and prolong its action in the organism (i.e., methoxy polyethylene glycol for CERA). It has to be acknowledged that not all rhEPO variants will be detectable, as those manufactured by underground laboratories constitute an analytical challenge, these EPO forms being slightly different and changing from batch to batch. Conversely, when applying the WADA positivity criteria, these are often not met.
The current technical document published by WADA in 2013 stipulates IEF or SAR both as the initial test and for confirmation purposes [15]. The recommended method used for confirmation depends on the type of substance found in the initial assessment.
New developments for ESA screening in urine include the use of liquid chromatography mass spectrometry (LCMS) [23, 24]. This technique, commonly used in anti-doping settings, showed promising results but still needs to be validated in the field. Another advance in the field of ESA detection is the MAIIA (membrane-assisted isoform immunoassay) method [25] for the detection of ESAs. It combines immunoassay with chromatography technology and can be used for both urine and blood samples. The first results have been promising, especially for the detection of very low doses of ESA [26, 27]. Another advantage of this new approach is the relatively easy analytical handling of the test and very little time requirements, allowing a high throughput of samples within a short time. On the other hand, the high costs of the MAIIA method may be considered a drawback. As for the LCMS method, validation is still pending.
Non-EPO-related erythropoiesis stimulating agents
With the market for anti-anemia drugs in 2012 estimated to be close to US$10 billion in the USA alone, it is clear that there is a strong research incentive for pharmaceutical companies which has led to the development of new ESAs, unrelated to the conventional EPO. Several approaches have been proposed, which are summarized in Table 1. Most of the substances are still in clinical trials, but the past has shown that black market laboratories are quick in copying drugs before even official approval has been granted to the developing pharmaceutical companies.
One drug which had US Food and Drug Administration (FDA) approval in the USA until recently is peginesatide (marketed as Omontys), a peptide structurally unrelated to EPO but with erythropoietic abilities [28]. After hypersensitivity reactions in first-time users had resulted in three deaths, the drug was withdrawn from the market in February 2013.
Fusion proteins are peptides resulting from the fusion of genes that initially coded for different proteins. The resulting peptides very often have properties from both of the genes they originated from. Fusion proteins are found in cancer cells, where they occur naturally as a result of cancer-associated mutation. In EPO research, fusion proteins showing erythropoietic capacity have been created and advanced to clinical trials. Some have been attached to immunoglobulin, which facilitates their administration (e.g., as an aerosol through a nasal spray). CNTO 530, an IgG4 fused peptide, increased erythropoietic activity after a single administration in mice [29].
Unfortunately EPO gene manipulation has for many years been recognized as a potential undetectable doping method. There are several scientific reports on the successful transfer of the EPO gene via a viral vector into muscle or dermal cells [30]. The technique demonstrated reliable increase in all erythropoietic markers.
Hypoxia inducible factor (HIF) 1α is the upstream regulator of the EPO signal in the organism. Under conditions of normoxia, this protein is usually immediately degraded by prolyl hydroxylases after its synthesis. Hypoxia, however, inhibits prolyl hydroxylases and thereby stabilizes the HIF1α protein which can then fulfill its action and induce the transcription of EPO. EPO will subsequently stimulate the erythropoietic cascade. Therapeutic anti-anemia strategies aim to inhibit the prolyl hydroxylases that induce the breakdown of HIF1α. A multitude of substances have been developed in this context and are currently at various stages of clinical experimentation [31].
Other than through prolyl hydroxylases and HIF1α, EPO gene expression is also regulated through transcription factors that will negatively affect the transcription: So-called GATA proteins bind to a certain sequence on the EPO promoter gene and inhibit its transcription, thus negatively affecting the EPO cascade. The activity of these GATA binding proteins can be altered by GATA inhibitors, which have been shown to measurably affect erythropoiesis [32, 33].
As most of the substances mentioned above are not naturally occurring in the body, their detection with conventional methods is, in theory, not problematic. Furthermore, many of the drugs are aimed at long-term action to overcome the frequent injections necessary with conventional EPO, which would improve the quality of treatment for the patient, but also the detection window for anti-doping tests. For several of the aforementioned substances, detection methods are readily available, owing to the close cooperation between WADA, anti-doping laboratories, and pharmaceutical companies [20, 28, 34].
Interestingly, the EPO gene transfer seems also to be detectable: Lasne et al. demonstrated in primates that the EPO originating from the transferred gene is different from the endogenous one, possibly because of the mild difference in cell organelles between the different types of cells. Whereas natural, endogenous EPO originates from kidney fibroblasts, the EPO genes are often transferred into muscle cells by using their cell organelles and thus creating a slight difference in glycosylation and molecular mass [35].
Detection of hemoglobin-based oxygen carriers (HBOCs)
Whereas many tissues and organs of the human body such as joints or cardiac valves can be replaced by artificial substitutes, medical science is still on the quest for a suitable blood replacement that features all qualities of the simple red blood cell to carry oxygen. So far, the greatest advances have been made in the development of HBOCs which, in contrast to other approaches such as perfluorocarbons, rely on hemoglobin molecules of animal origin or from genetic engineering [36]. A HBOC (Oxyglobin®) was approved for veterinary use in certain countries 15 years ago. Such substances are understood to have entered the world of sports already with the aim of improving oxygen delivery to tissues [37, 38] and have allegedly been used by athletes in an attempt to boost performance. However, the definite proof of the efficiency of these substances to improve performance is still lacking [39] and the few studies showing a positive effect have been criticized [40, 41]. It has been speculated that the oxygen transport effects are impaired by a significant vasoactive action of the HBOCs related to NO scavenging properties of free hemoglobin, which interferes with oxygen delivery. With the advancement of medical science it can nevertheless be anticipated that sooner or later a viable HBOC that is able to improve oxygen delivery and thereby performance in humans will be available. The detection of HBOC is straightforward and relies on electrophoresis as a screening procedure and size exclusion–high-performance liquid chromatography (SEC-HPLC) [42, 43].
Direct detection of blood transfusions
With the availability of direct ESA testing, it can be presumed that the ‘older technique’ for performance enhancement using blood transfusions for boosting red cell volume gained in importance among cheating athletes. Neither homologous nor autologous blood transfusions could be detected directly until 2003, when Margaret Nelson et al. presented a test for the detection of homologous transfusion that identifies mixed red blood cell (RBC) populations using antisera against minor blood group antigens [44]. In this assay, 12 blood group antigens were selected to identify donor RBC populations in patients who received between one to three units of homologous blood with a lower limit of detection around 5 % of the total red cell population [44]. The method was further validated and improved by Voss et al. who used a panel of eight primary blood groups antigens [45]. Applying the technique of signal amplification, the authors improved the separation of those antigens with weak or heterozygous expression resulting in an identification of mixed RBC populations in samples containing 0.3–2.0 % of donor blood [45].
Around the same time, Giraud et al. presented forensic standards of doping analyses for homologous blood transfusions in a single-blind and single-site study [46]. A specificity of 100 % was described as no false-positive results were observed in the analysis of 140 blood samples containing different percentages (0–5 %) of a minor RBC population. The sensitivity of the method was 78.1 % and most samples were unambiguously detected. With their approach, the ISO-17025 accreditation and validation requirements were fulfilled [46]. Examples of single and double population fluorescence intensity histograms (using anti-Jka antibody and the mix of fluorescein isothiocyanate (FITC)-coupled secondary antibodies) are presented in Fig. 2. Several athletes tested positive for homologous blood transfusion on the basis of this test.
Typical distributions of the fluorescence intensity channel responses obtained from controls. The presence of two visible peaks in these histograms is characteristic of a bimodal antigen expression, hence a mixed RBCs population. Externally phenotyped RBCs were chosen on the basis of the presence or absence of the Jka antigen. Both mixed and non-mixed samples were incubated with anti-Jka antibody and the mix of FITC-coupled secondary antibodies. a Single RBC population blood without expression, b single RBC population expressing Jka antigen, c mixed RBC population with a non-expressing main RBC population and an expressing minor RBC population, and d mixed RBC population with an expressing main RBC population and a non-expressing minor population. (Reprinted from [46] with permission from Elsevier)
Obviously, this method is inappropriate for the detection of autologous blood transfusions, which continue to be undetectable by direct means. From the time before 2000, when EPO was similarly undetectable by a direct test, indirect biomarkers have emerged as a method to deter blood doping and possibly limit the extent of manipulations.
The use of indirect biomarkers of doping has culminated in the introduction of the so-called athlete biological passport (ABP) which can be regarded as the best approach and is implemented by WADA [47]. The ABP will be described in a separate section below.
History of biomarker approach
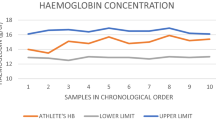
In the late 1990s, as a first step, ‘no start’ rules were introduced with the official objective to protect the health of the athletes when certain blood markers exceeded definite limits (e.g., hematocrit (Hct) above 50 % or hemoglobin (Hb) above 17 g/dL (International Cycling Union, UCI) [48] or Hb above 17.5 g/dL in men and 16.0 g/dL in women (International Ski Federation, FIS) [49, 50]. In this time, the widespread use of rhEPO can be assumed on the basis of indirect evidence; e.g., in elite cross-country skiers extreme Hb values up to 20 g/dL were common between 1994 to 1996 but disappeared after the ‘no start’ rule was introduced in 1997. Yet, mean Hb values continued to rise, suggesting the further use of artificial methods with fewer extremes [49, 51]. It became obvious, as described by Cazzola [52], that the use of upper limits of definite blood values may result in athletes who would titrate rhEPO to approach the target Hb or Hct without exceeding it.
Plasma volume fluctuations resulting from changes in posture, exercise, and training [53], altitude exposure [54, 55], season as well as storage conditions [56] influence concentration-based blood values such as Hct and Hb and thus represent a major limitation of their use with absolute limits. Additionally, cheating athletes may manipulate abnormally elevated Hb and Hct values by intravenous infusions of normal saline leading to hemodilution. On the other hand, even clean athletes may be declared unfit as Hb and Hct in a normal distribution may exceed the given limits [57].
The panel of indirect markers was extended and more evidence was gathered on the effect on blood values of rhEPO administration in training athletes [58]. Parisotto et al. suggested the use of a combination of indirect markers of altered erythropoiesis (reticulocyte Hct, serum EPO, soluble transferring receptor, Hct, %macrocytes) in a multivariate statistical model for detection of rhEPO during a possible administration phase (ON models) and after recent cessation of rhEPO use (OFF models) [59, 60]. The sensitivity of these models was improved with larger numbers of subjects and resulted in the introduction of the so-called second-generation blood tests [61] of which the OFF-hr model, a score combining Hb and %retics, is part of the current ABP according to the WADA ABP operating guidelines [47]. Although OFF-hr was originally described for the detection of rhEPO use, it is also sensitive to other forms of blood doping such as blood transfusion [62, 63].
The application of these models by sports authorities and anti-doping organizations was problematic despite their scientific impact. The OFF-hr model was used by certain sports federations as another ‘no start’ criterion [61]. Yet, infringements of the ‘no start’ rule were equal to failing a ‘health test’ but not considered a violation against WADA’s anti-doping code and therefore only yielded short mandatory interruptions of competition, e.g., 2 weeks.
As even these improved biomarkers were only compared with a population-based reference range in a cross-sectional setting (e.g., universal limit of Hct above 50 %, OFF score greater than 122), it already seemed likely in 2000 that a longitudinal, individual hematologic profile, the so-called hematologic passport, could be advantageous to prevent and perhaps detect blood doping [52]. Various attempts were made to define the natural within-subject and between-subject as well as analytical variability to use longitudinal measurements as an instrument against blood doping.
Introduction of the athlete biological passport (ABP)
The relevance of indirect biomarkers persisted even after the introduction of a direct test for rhEPO abuse [13, 64] because the time frame of direct rhEPO detection was short and other forms of blood doping such as transfusions are believed to have been revived by fraudulent athletes in that time. Even with the availability of a direct test for homologous transfusions [44, 45] biomarkers may be used to reveal manipulations induced by blood transfusions regardless of the origin. It is clear now that the biomarker approach bears another advantage. These markers are already sensitive to any future compound that elicits a similar physiological response, such as the increase of the oxygen carrying capacity. Therefore, the concept of a hematologic passport was developed further and is presented in detail in this section.
Early subject-specific reference ranges were defined by Malcovati et al. for Hb and Hct to encourage the hematologic passport in a global strategy to deter blood doping [65]. The main theory behind this concept is that each athlete provides individual reference values that allow a longitudinal analysis by applying various algorithms.
The so-called third-generation tests or the z-score were introduced by Sharpe et al. who were able to distinguish the effect of rhEPO abuse from natural biological fluctuations with longitudinal observations of Hb or OFF-hr. Assuming a universal within-subject variation only two values from one athlete could be used for the calculation of the z-score [66]. In a new approach, it was concluded that longitudinal data might not only be used to ban participation in competition but also to establish target testing of suspicious athletes [66]. This was important as only positive direct test results could be used for sanctioning of manipulating athletes.
Progress of the passport concept prevailed as Sottas et al. combined all data contained in a single blood profile of an athlete in a universal multiparametric score (abnormal blood profile score, ABPS) that was initially presented in various versions using between three and 12 different biomarkers responding to either rhEPO administration or blood transfusion [67]. In the current version of the WADA ABP operating guidelines [47], ABPS calculated from Hct, Hb, RBC count, reticulocyte percentage (RET%), mean corpuscular volume (MCV), mean corpuscular hemoglobin (MCH), and mean corpuscular hemoglobin concentration (MCHC) is recommended as a marker in addition to OFF-hr [61]. In a universal marker such as ABPS various doped states might equally lead to a high score, e.g., the donation and reinfusion of autologous blood both will elevate the score, whereas this will lead to a one-directional change only from a low to a high value for the non-universal marker OFF-hr [68].
Furthermore, it is prudent to consider that blood values may always be subject to biological variability (e.g., gender, age)—heterogeneous factors—and confounding factors such as physical activity (e.g., type of sport, competition vs. training, or exposure to altitude). Some of these factors may change over time, such as altitude or the type of instrument used, and then influence longitudinal monitoring. Yet, time-independent or fixed factors such as ethnic origin or gender are specific for a given athlete [68]. Robinson et al. considered heterogenous factors and proposed a model based on a global Bayesian inference approach for the detection of abnormal blood values over time [69]. In such a Bayesian network, the causal relationship between a doping activity and the induced alterations of blood markers is represented as probabilities where every causal relationship is itself a model represented by a conditional probability density function [68].
WADA and other sports federations observed the growing scientific knowledge of longitudinal subject-specific monitoring of blood values until, in 2008, UCI was the first sports organization to introduce the hematological module of the ABP to detect blood doping. WADA followed in December 2009 and approved the first version of the WADA ABPoperating guidelines which have since been revised [47]. Nowadays, the hematological module of the ABP includes the longitudinal monitoring of eight hematological markers (Hct, Hb, RBC, reticulocyte count (#retics), %retics, MCV, MCH, and MCHC) to identify abnormal patterns with a subject becoming her or his own reference. From some of the hematological markers additional models are calculated: OFF-hr [61] and ABPS (containing 7 markers) [67]. According to the WADA ABP guidelines [47] the application of the ‘adaptive model’ predicts an expected range for an individual within which a series of marker values falls assuming a normal physiological condition [47]. Outliers correspond to values out of the 99.9 % range (0.05–99.95 percentiles) and warrant further attention and review. Anti-doping organizations may select a value lower than 99.9 % to identify atypical samples and/or profiles that warrant further investigation [47]. An expert chosen by the responsible anti-doping organization shall initially review atypical values or an atypical longitudinal profile. This expert shall evaluate the anonymous passport data and respond on the basis of four hypotheses that will trigger the indicted further action [47]:
-
The measured values can be considered natural variation and thus normal: normal testing pattern is continued.
-
The measured values are suspicious: further data are required and target tests shall be performed.
-
The measured values may be the result of the use of a prohibited substance or prohibited method: two further experts review the passport.
-
The measured values are indicative of a pathological condition: information of the athlete or involvement of two further experts.
As the role of scientific experts in doping cases based on indirect evidence will considerably gain in importance, an emphasis should be made in regular scientific exchange and continuous education of the experts.
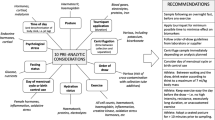
The prerequisite of valid biomarker data for objective interpretation and legal use is a strict process for sample collection, transport, and analysis that has been put into place for the ABP [47]. For instance, sample collection must not occur within 2 h after training or competition and must be carried out after the athlete has remained in a seated upright position for 10 min with feet on the floor [47] in order to allow the vascular volumes to equilibrate [70]. In addition, important minimum information should be included on the ABP control form to review blood data in an individual context such as and among others blood loss in the 3 months preceding each sample collection, use of simulated hypoxic conditions (e.g., altitude house, tents), or exposure to altitude above 1,000 m above sea level [47].
Furthermore, technical documents of the ABP guideline define the transport and storage conditions, e.g., the type of storage device, the necessity of a storage temperature data logger, and the rapid transport so that analysis can ideally be performed within 36 h of sample collection [47], although there is growing evidence that this time frame might be extended [71]. Samples should only be analyzed in WADA-accredited or WADA-approved laboratories or their satellite facilities which must all be subject to strict regular internal and external quality control procedures and follow the WADA international standard of laboratories [72].
Current ABP guidelines describe the particular importance of an athlete passport management unit (APMU) that is responsible for the administrative management of the ABP. This includes advising anti-doping organizations about intelligent, targeted testing, liaising with the expert panel, compiling an ABP documentation package, and reporting adverse analytical findings to anti-doping organizations and WADA [47].
It seems essential that APMU personnel has profound knowledge of the ABP concept and indirect doping detection methods to ensure the intelligent, targeted approach that helps to avoid a waste of organizational and financial resources. It can be postulated that a main goal is to avoid parallel passport data collected by different stakeholders such as national anti-doping organizations (NADO) or governing bodies of each sport. Therefore, harmonization of data storage with mutual sharing of results that were analyzed with strict adherence to the WADA protocol is important to use the ABP in its full capacities. The ADAMS (anti-doping administration and management system) platform could provide a system for all stakeholders for the planning, collection, and evaluation of all ABP data although the exact responsibility of each stakeholder remains to be defined. For instance, NADOs could emphasize the testing of a young and/or nationally active athlete but as the athlete moves on to a regular international competition setting, testing could be taken over by the international sporting federation.
Continuous evaluation of the ABP
Further studies evaluated the strength and possible limitations of the ABP after introduction of the hematological module by UCI and WADA which will be presented in the subsequent paragraph.
As the ABP depends on analytically flawless data, the pre-analytical conditions and the laboratory testing were put into question [73, 74]. Thus, it seemed of great importance whether the adherence to the ABP guidelines [47] will allow high quality results respecting forensic standards and thus assure their applicability in a juridical context. Robinson et al. confirmed that the rigorous adherence to WADA’s guidelines yields excellent results required in the anti-doping context [71]. According to Lombardi et al. who reviewed this and previous studies on the topic, the limit of 36 h from blood collection to analysis is reasonable to guarantee analytical quality, when the samples are transported at 4 °C which seemed to improve the stability of hematological parameters independently from the analytical methodology [75]. Further studies on the stability of blood parameters used within an anti-doping setting were available before the ABP was officially introduced [76–78]. In addition, pursuing the goal to provide a sound foundation for the interpretation of blood profiles in athletes, more data were published on various confounding factors and analytical aspects which may help to refine existing guidelines [79–82]. For instance, from a practical point of view, Schumacher at al. reported that long-haul air travel leads to normal diurnal variations of Hb without any indication that travel will affect the hematological measures in a way that might be interpreted as blood doping [83].
Despite the general appreciation of the concept, it also became clear that the ABP has some limitations. As described by Sottas and Vernec, “the sensitivity of the ABP to detect doping is limited if the physiological result of a low level of doping remains within the individual’s own reference range” [84]. It fits in this context that microdosing of rhEPO does not lead to abnormal changes in the current ABP markers during rhEPO administration [17]. Nevertheless, this study by Ashenden et al. may face certain limitations. For example, blood counts were measured only during the titration and following maintenance phase, but not longitudinally after rhEPO was discontinued for which OFF-hr was originally described [17].
In order to evaluate the best possible realistic performance of the ABP adaptive model for a blood doping technique (autologous blood doping), a longitudinal blinded study design included 21 subjects that were divided into two groups of which one was transfused with 1–2 bags of blood at 2–3 time points during a simulated time course of a professional cycling season [62]. A blinded investigator who was well trained in the use of the ABP was requested to apply an intelligent testing approach which allowed a sensitivity of 82 % at the 99 % threshold of the adaptive model as 9 of 11 subjects in the doped group had at least one value outside of the individual limits for Hb and OFF-hr or a sequence (Hb and OFF-hr) above the 99.9 % probability threshold. The specificity was 90 % for Hb (one false-positive value in 1 of 11 athletes) and 100 % for OFF-hr, sequence Hb as well as sequence OFF-hr [62]; see Fig. 3 for examples of a ’transfused’ and ‘non-transfused’ subject (modified and reprinted with permission from [62]).
Two original ABP software passport illustrations (screen shots) show the individual time course (blue line, ordinal scaling, x-axis) of the measure (Hb, OFF-hr, and ret%, each on y-axis) and the respective individual two-tailed threshold limit values (upper and lower red lines, 99 % probability). Additionally, the percentile at which the sequence falls in the distribution of sequences of the same length assuming no doping is indicated below each graph. a Case of the control group. b Case of the doped group, the time points of blood withdrawal, and reinfusion are marked by gray arrows (one arrow per unit; down arrow withdrawal of 500 mL of whole blood, up arrow reinfusion of 280 mL of RBCs). (Modified and reproduced with permission from [62])
Several aspects allude to the effectiveness of the ABP hematological module. First, individual non-physiological data from the ABP have been used to sanction athletes [85, 86] and were recognized by the Court of Arbitration in Sport (CAS) in a final hearing. Second, these precedents might have had a deterrent effect on future behavior of athletes as can be concluded from the data of Zorzoli and Rossi [87] who reported that the value of %retics has significantly changed and normalized since the introduction of the ABP in 2008, which may reflect a decreased prevalence of blood manipulations in the professional cycling peloton. From a practical and more measurable perspective, the introduction of the ABP hematological module and dedicated target testing based on the ABP data led to a 250 % increase in the number of positive rhEPO cases in 2008 and 2009. In 2011 the number of cases was still about 300 % higher than it was before the introduction of the ABP (data available from www.wada-ama.org).
Future perspectives
Apart from the application of the ABP hematological passport, other strategies were pursued to narrow the incidence of blood doping and offer a broader spectrum of detection methods. This is especially true for the detection of otherwise untraceable autologous blood transfusions.
Phthalates
One idea was to identify markers that indirectly allude to the autologous transfusion. After withdrawal, freshly donated blood requires an initial processing and storage for a certain amount of time, which mostly occurs in plastic bags. The softening substances of these plastic blood bags or so-called plasticizers are phthalates (di-(2-ethylhexyl)phthalate (DEHP)) and their derivates. A considerable amount of the phthalates will diffuse from the plastic bag into the stored blood during long-term storage and will be transfused with the blood. Monfort et al. demonstrated that phthalates are metabolized in the human body to distinct molecules (mono-(2-ethylhexyl)phthalate (MEHP), mono-(2-ethyl-5-hydroxyhexyl)phthalate (MEHHP), and mono-(2-ethyl-5-oxohexyl)phthalate (MEOHP)) and can be detected in urine for a short time after transfusion using LCMS methods [88]. The measurement of phthalates is the first approach using urine as a matrix, which is collected commonly at anti-doping controls. This may also include using phthalate analyses for homologous blood transfusion for which the direct test requires the collection of blood samples [44, 45]. Blood samples are now collected in a much higher percentage than in the past but not in all subjects.
On the other hand, as phthalates are ubiquitous and present in many products of daily use, testing for phthalates will very likely not be a suitable stand-alone detection method for blood transfusion. Therefore, several validation studies [89–91] have been conducted in order to identify threshold values for the different metabolites in athletes, taking into account the normal daily exposure to plasticizers. Recently, two further metabolites were described as possible markers (mono-(2-ethyl-5-carboxypentyl)phthalate (5cx-MEPP) and mono-(2-carboxymethylhexyl)phthalate (2cx-MMHP)) for blood transfusions measured by ultraperformance liquid chromatography tandem mass spectrometry together with the molecules MEHP, MEHHP, and MEOHP [92]. The use of urine for the detection of blood transfusions with phthalates seems promising as all urine samples submitted to doping analysis in any accredited laboratory could provide corroborating evidence in subjects potentially using blood transfusion, e.g., based on ABP data. Phthalate data could also be applied together with other indirect markers in a multifactor approach.
Hemoglobin mass
Coinciding with the agreement on the ABP, Morkeberg et al. [63] evaluated three passport approaches for their sensitivity and specificity for the detection of autologous blood transfusion. The best possible marker for lower dosages of transfused blood (e.g., one bag) was OFF-hr [87]. Interestingly, a new score (Hbmr) was introduced and showed the best performance for larger amounts (e.g., three bags), but requires the determination of total hemoglobin mass (Hb mass) as a further measure. Hb mass determined by the optimized CO rebreathing method [93] was first suggested as a potential biomarker in the context of blood doping in 2007 [94], mainly because it is independent of plasma volume fluctuations. The usefulness and applicability in several circumstances were evaluated in several studies thereafter [95–101]. Hb mass was also evaluated as a marker in the adaptive model of the ABP in a longitudinal blinded study [102], in which a new score (OFFmass including %retics) was likewise published and yielded a sensitivity of 73 % without false-positives at the 99.9 % specificity level. Hb mass was also evaluated for the potential to detect rhEPO misuse [103]. Various efforts have been made [104, 105] to improve the problems associated with the CO rebreathing method such as the administration of a potentially toxic substance and lack of a quality control system. Nevertheless, it seems that these problems limit the applicability of the method in anti-doping [104, 105]. Therefore, the search is on for an alternative to Hb mass determination which is compatible with today’s standards of testing because of its potential to improve the detection rate of autologous blood transfusion. On such approach could be the indirect modeling of Hb mass from indirect markers. Research on this topic is currently being conducted.
MicroRNAs
Further biomarkers could be derived from ‘circulating miRNAs' as shown by Leuenberger et al. for the abuse of ESAs [106]. On the basis of microarray results, a significant difference in the levels of miRNAs was measured in plasma after CERA injection, even for a longer period of time as the increase of the specific miR-144 l lasted 27 days after CERA administration. Similarly, the same group described that autologous blood transfusion leads to an increase of selected circulating miRNAs in plasma of pulmonary and liver tissue origin compared to a non-transfused control group (personal communication).
Response to foreign erythrocytes
Another interesting approach arises from the analysis of erythrocytes. In a pilot project, Nikolovski et al. analyzed proteomic data (e.g., from 2-DE gels) from two volunteers and showed that RBC membrane proteome changes during storage could provide biomarkers for the detection of autologous transfusion in the future [107]. In a similar small study, Marrocco et al. showed that the marker ‘oxidative stress-related protein peroxiredoxin 2’ and the RBC population characterized by density separation significantly changed after mixture of stored RBCs with freshly withdrawn RBCs in vitro [108]. In a current project supported by WADA (11B16TP), our group hypothesized that a systemic response towards a ‘supra-physiological’ red cell volume induced by autologous transfusion might be assessable in vivo by measuring the differences in red cell distribution by continuous density gradients and flow cytometry characterization of erythrocytes.
Furthermore, as several molecular changes occur in stored RBCs, commonly referred to as the ‘storage lesion’, we hypothesized that autologous transfusion will lead to a sudden exposure of cell detritus to the immune system causing a cellular and molecular immune response. A distinct immune reaction was found on a transcriptional level in T lymphocytes using whole genome microarrays and qRT-PCR confirmation [109]. This concept was reassessed by evaluation of the immune response of peripheral blood mononuclear cells using cellular fluorescence markers in vitro and in vivo by our group (BISP IIA1-070303/10-11); these results will be published elsewhere.
Other serum markers
Several authors have highlighted the impact of blood manipulation on iron metabolism [110, 111]. With iron being the major substrate for Hb synthesis, it is evident that iron-related variables will be affected by any manipulations of erythropoiesis. Ferritin, the iron storage protein, was addressed as a potential marker as early as the 1980s [111]. However, the association to inflammation and its susceptibility to be influenced by external iron administration limits its specificity. Hepcidin was recently investigated as another potential marker in this context. This molecule regulates the iron absorption by the body and was found in several studies to be a potential marker for blood manipulation [112]. However, more data on the natural variation and the impact of exercise and other confounding factors are necessary.
Combination of biomarkers
As the evidence from above illustrates, the main scientific focus has been on finding single biomarkers that will detect certain doping techniques with acceptable sensitivity and good specificity. Future research should explore complementary paths using mathematical methods for the combination of the multitude of markers that often display a good sensitivity but may lack specificity. Approaches such as support vector machines and other classification techniques that are in use in many other domains of science might be helpful. In this context, information from different sources (e.g., urine tests, blood tests) should be combined, as also for urine test information, a longitudinal monitoring has been proposed [27]. By these means, specificity could be increased and distinct patterns for certain doping interventions or the identification of suspicious and potentially doping athletes could be warranted, which would then trigger follow-up testing with more specific methods. This would help to save resources and make the fight against doping more efficient.
In this context, the application of newer diagnostic tools relating to the ‘omics’ technologies such as transcriptomics, proteomics, and metabolomics will nurture this area in the years to come [113, 114]. Thus, it may be possible to identify the biological fingerprint of many potential doping substances which would allow athletes to present themselves to a competition with physiological values and profiles that fall within their own personal limits [84]. Additionally, the scope of analyses could be expanded to performance profiling for targeting and intelligent testing procedures [11].
Conclusions
Nowadays, several blood doping techniques can be directly detected such as the misuse of many types of ESAs and homologous blood transfusion. A new era was initiated with the introduction of the hematological module of the ABP by WADA in 2009 which may allow one to overcome certain limitations of direct testing (e.g., ESAs similar to endogenous compounds, limited detection window) and may provide an instrument for the detection of autologous blood transfusion. The main advantage of this new approach is that it remains applicable regardless of the doping technique and will remain sensitive even with upcoming new substances that cause a similar physiological phenotype. Figure 4 displays a synopsis of the available methods for blood doping detection. In the future, a multitude of markers provided by the ‘omics’ technologies could be used in an individual subject-based model to identify non-physiological patterns and use the individual ABP to its full capacity.
Synopsis of major blood doping detection methods. Established methods are printed in black (solid line), future or experimental methods are printed in gray (dashed line). The sensitivity of the ABP may be limited if the physiological result of a low level of doping remains within the individual’s own reference range. See text for abbreviations
References
Sawka MN, Convertino VA, Eichner ER, Schnieder SM, Young AJ (2000) Blood volume: importance and adaptations to exercise training, environmental stresses, and trauma/sickness. Med Sci Sports Exerc 32:332–348
Bonetti DL, Hopkins WG (2009) Sea-level exercise performance following adaptation to hypoxia: a meta-analysis. Sports Med 39:107–127
Pace N, Consolazio WV, Lozner EL (1945) The effect of transfusions of red blood cells on the hypoxia tolerance of normal men. Science 102:589–591
Pace N, Lozner EL (1947) The increase in hypoxia tolerance of normal men accompanying the polycythemia induced by transfusion of erythrocytes. Am J Physiol 148:152–163
Gullbring B, Holmgren A, Sjostrand T, Strandell T (1960) The effect of blood volume variations on the pulse rate in supine and upright positions and during exercise. Acta Physiol Scand 50:62–71
Ekblom B, Goldbarg AN, Gullbring B (1972) Response to exercise after blood loss and reinfusion. J Appl Physiol 33:175–180
Robinson BF, Epstein SE, Kahler RL, Braunwald E (1966) Circulatory effects of acute expansion of blood volume: studies during maximal exercise and at rest. Circ Res 19:26–32
Sawka MN, Joyner MJ, Miles DS, Robertson RJ, Spriet LL, Young AJ (1996) American College of Sports Medicine position stand. The use of blood doping as an ergogenic aid. Med Sci Sports Exerc 28:i–viii
Cramer RB (1985) Olympic cheating: the inside story of illicit doping and the U.S. cycling team. Rolling Stone 14:25–30
Ekblom B, Berglund B (1991) Effect of erythropoietin administration on maximal aerobic power in man. Scand J Med Sci Sport 1:88–93
Schumacher YO, Pottgiesser T (2009) Performance profiling: a role for sport science in the fight against doping? Int J Sports Physiol Perform 4:129–133
El Helou N, Berthelot G, Thibault V, Tafflet M, Nassif H, Campion F, Hermine O, Toussaint J-F (2010) Tour de France, Giro, Vuelta, and classic European races show a unique progression of road cycling speed in the last 20 years. J Sports Sci 28:789–796
Lasne F, de Ceaurriz J (2000) Recombinant erythropoietin in urine. Nature 405:635
Lasne F, Martin L, Crepin N, de Ceaurriz J (2002) Detection of isoelectric profiles of erythropoietin in urine: differentiation of natural and administered recombinant hormones. Anal Biochem 311:119–126
WADA (2013) WADA technical document EPO detection 2013. http://www.wada-ama.org/documents/world_anti-doping_program/wadp-is-laboratories/technical_documents/wada-td2013epo-harmonization-analysis-of-recombinant-erythropoietins-en.pdf. Accessed 23 Apr 2013
Bajla I, Holländer I, Minichmayr M, Gmeiner G, Reichel C (2005) GASepo–a software solution for quantitative analysis of digital images in Epo doping control. Comput Methods Prog Biomed 80:246–270
Ashenden M, Gough CE, Garnham A, Gore CJ, Sharpe K (2011) Current markers of the athlete blood passport do not flag microdose EPO doping. Eur J Appl Physiol 111(9):2307–2314
Lamon S, Robinson N, Sottas PE, Henry H, Kamber M, Mangin P, Saugy M (2007) Possible origins of undetectable EPO in urine samples. Clin Chim Acta 385:61–66
Lamon S, Martin L, Robinson N, Saugy M, Ceaurriz J, Lasne F (2009) Effects of exercise on the isoelectric patterns of erythropoietin. Clin J Sport Med 19:311
Reichel C, Abzieher F, Geisendorfer T (2009) SARCOSYL-PAGE: a new method for the detection of MIRCERA- and EPO-doping in blood. Drug Test Anal 1:494–504
Reichel C, Kulovics R, Jordan V, Watzinger M, Geisendorfer T (2009) SDS-PAGE of recombinant and endogenous erythropoietins: benefits and limitations of the method for application in doping control. Drug Test Anal 1:43–50
Macdougall IC, Ashenden M (2009) Current and upcoming erythropoiesis-stimulating agents, iron products, and other novel anemia medications. Adv Chronic Kidney Dis 16:117–130
Möller I, Thomas A, Geyer H, Schänzer W, Thevis M (2011) Synthesis, characterisation, and mass spectrometric detection of a pegylated EPO-mimetic peptide for sports drug testing purposes. Rapid Commun Mass Spectrom 25:2115–2123
Chang Y, Maylin GM, Matsumoto G, Neades SM, Catlin DH (2011) Screen and confirmation of PEG-epoetin β in equine plasma. Drug Test Anal 3:68–73
Lönnberg M, Carlsson J (2000) Membrane assisted isoform immunoassay. A rapid method for the separation and determination of protein isoforms in an integrated immunoassay. J Immunol Methods 246:25–36
Ashenden M, Sharpe K, Garnham A, Gore CJ (2012) Evaluation of the MAIIA dipstick test to detect recombinant human erythropoietin in plasma. J Pharm Biomed Anal 67–68:123–128
Mørkeberg J, Sharpe K, Karstoft K, Ashenden MJ (2013) Detection of microdoses of rhEPO with the MAIIA test. Scand J Med Sci Sports. doi:10.1111/sms.12049
Leuenberger N, Saugy J, Mortensen RB, Schatz PJ, Giraud S, Saugy M (2011) Methods for detection and confirmation of Hematide™/peginesatide in anti-doping samples. Forensic Sci Int 213:15–19
Sathyanarayana P, Houde E, Marshall D, Volk A, Makropoulos D, Emerson C, Pradeep A, Bugelski PJ, Wojchowski DM (2009) CNTO 530 functions as a potent EPO mimetic via unique sustained effects on bone marrow proerythroblast pools. Blood 113:4955–4962
Lippin Y, Dranitzki-Elhalel M, Brill-Almon E, Mei-Zahav C, Mizrachi S, Liberman Y, Iaina A, Kaplan E, Podjarny E, Zeira E et al (2005) Human erythropoietin gene therapy for patients with chronic renal failure. Blood 106:2280
Yan L, Colandrea VJ, Hale JJ (2010) Prolyl hydroxylase domain-containing protein inhibitors as stabilizers of hypoxia-inducible factor: small molecule-based therapeutics for anemia. Expert Opin Ther Pat 20:1219–1245
Imagawa S, Matsumoto K, Horie M, Ohkoshi N, Nagasawa T, Doi T, Suzuki N, Yamamoto M (2007) Does K-11706 enhance performance and why? Int J Sports Med 28:928–933
Suzuki N, Ohneda O, Takahashi S, Higuchi M, Mukai HY, Nakahata T, Imagawa S, Yamamoto M (2002) Erythroid-specific expression of the erythropoietin receptor rescued its null mutant mice from lethality. Blood 100:2279–2288
Beuck S, Schänzer W, Thevis M (2012) Hypoxia-inducible factor stabilizers and other small-molecule erythropoiesis-stimulating agents in current and preventive doping analysis. Drug Test Anal 4:830–845
Lasne F, Martin L, de Ceaurriz J, Larcher T, Moullier P, Chenuaud P (2004) Genetic doping with erythropoietin cDNA in primate muscle is detectable. Mol Ther 10:409
Riess JG (2001) Oxygen carriers (“blood substitutes”)—raison d’etre, chemistry, and some physiology. Chem Rev 101:2797–2920
Schumacher YO, Schmid A, Dinkelmann S, Berg A, Northoff H (2001) Artificial oxygen carriers–the new doping threat in endurance sport? Int J Sports Med 22:566–571
Schumacher YO, Ashenden M (2004) Doping with artificial oxygen carriers: an update. Sports Med 34:141–150
Ashenden MJ, Schumacher YO, Sharpe K, Varlet-Marie E, Audran M (2007) Effects of Hemopure on maximal oxygen uptake and endurance performance in healthy humans. Int J Sports Med 28:381–385
Crago MS, West SD, McKenzie JE (1999) Effects of diaspirin crosslinked hemoglobin infusion in treadmill-exercised swine. Heart Vessels 14:1–8
Hughes GS Jr, Yancey EP, Albrecht R, Locker PK, Francom SF, Orringer EP, Antal EJ, Jacobs EE Jr (1995) Hemoglobin-based oxygen carrier preserves submaximal exercise capacity in humans. Clin Pharmacol Ther 58:434–443
Lasne F, Crepin N, Ashenden M, Audran M, de Ceaurriz J (2004) Detection of hemoglobin-based oxygen carriers in human serum for doping analysis: screening by electrophoresis. Clin Chem 50:410–415
Varlet-Marie E, Ashenden M, Lasne F, Sicart M-T, Marion B, de Ceaurriz J, Audran M (2004) Detection of hemoglobin-based oxygen carriers in human serum for doping analysis: confirmation by size-exclusion HPLC. Clin Chem 50:723–731
Nelson M, Popp H, Sharpe K, Ashenden M (2003) Proof of homologous blood transfusion through quantification of blood group antigens. Haematologica 88:1284–1295
Voss SC, Thevis M, Schinkothe T, Schanzer W (2007) Detection of homologous blood transfusion. Int J Sports Med 28:633–637
Giraud S, Robinson N, Mangin P, Saugy M (2008) Scientific and forensic standards for homologous blood transfusion anti-doping analyses. Forensic Sci Int 179:23–33
WADA (2012) WADA world anti-doping code. Athlete biological passport operating guidelines and compilation of required elements. V3.1, 2012. http://www.wada-ama.org
UCI (1997) UCI sporting safety and condition regulations. UCI, Lausanne, Chapt XIII:13.01.023
Morkeberg J, Saltin B, Belhage B, Damsgaard R (2009) Blood profiles in elite cross-country skiers: a 6-year follow-up. Scand J Med Sci Sports 19:198–205
FIS Medical Committee (2000) Medical guide 2000/2001. International Ski Federation, Oberhofen am Thunersee, p 13–14
Videman T, Lereim I, Hemmingsson P, Turner MS, Rousseau-Bianchi MP, Jenoure P, Raas E, Schönhuber H, Rusko H, Stray-Gundersen J (2000) Changes in hemoglobin values in elite cross-country skiers from 1987-1999. Scand J Med Sci Sports 10:98–102
Cazzola M (2000) A global strategy for prevention and detection of blood doping with erythropoietin and related drugs. Haematologica 85:561–563
Sharpe K, Hopkins W, Emslie KR, Howe C, Trout GJ, Kazlauskas R, Ashenden MJ, Gore CJ, Parisotto R, Hahn AG (2002) Development of reference ranges in elite athletes for markers of altered erythropoiesis. Haematologica 87:1248–1257
Ashenden MJ, Sharpe K, Schoch C, Schumacher YO (2004) Effect of pre-competition and altitude training on blood models used to detect erythropoietin abuse by athletes. Haematologica 89:1019–1020
Ashenden MJ, Gore CJ, Parisotto R, Sharpe K, Hopkins WG, Hahn AG (2003) Effect of altitude on second-generation blood tests to detect erythropoietin abuse by athletes. Haematologica 88:1053–1062
Felding P, Petersen PH, Hørder M (1981) The stability of blood, plasma and serum constituents during simulated transport. Scand J Clin Lab Invest 41:35–40
Johansson PI, Ullum H, Jensen K, Secher NH (2009) A retrospective cohort study of blood hemoglobin levels in blood donors and competitive rowers. Scand J Med Sci Sports 19:92–95
Audran M, Gareau R, Matecki S, Durand F, Chenard C, Sicart MT, Marion B, Bressolle F (1999) Effects of erythropoietin administration in training athletes and possible indirect detection in doping control. Med Sci Sports Exerc 31:639–645
Parisotto R, Wu M, Ashenden MJ, Emslie KR, Gore CJ, Howe C, Kazlauskas R, Sharpe K, Trout GJ, Xie M (2001) Detection of recombinant human erythropoietin abuse in athletes utilizing markers of altered erythropoiesis. Haematologica 86:128–137
Parisotto R, Gore CJ, Emslie KR, Ashenden MJ, Brugnara C, Howe C, Martin DT, Trout GJ, Hahn AG (2000) A novel method utilising markers of altered erythropoiesis for the detection of recombinant human erythropoietin abuse in athletes. Haematologica 85:564–572
Gore CJ, Parisotto R, Ashenden MJ, Stray-Gundersen J, Sharpe K, Hopkins W, Emslie KR, Howe C, Trout GJ, Kazlauskas R, Hahn AG (2003) Second-generation blood tests to detect erythropoietin abuse by athletes. Haematologica 88:333–344
Pottgiesser T, Sottas P-E, Echteler T, Robinson N, Umhau M, Schumacher YO (2011) Detection of autologous blood doping with adaptively evaluated biomarkers of doping: a longitudinal blinded study. Transfusion 51:1707–1715
Morkeberg J, Sharpe K, Belhage B, Damsgaard R, Schmidt W, Prommer N, Gore CJ, Ashenden MJ (2011) Detecting autologous blood transfusions: a comparison of three passport approaches and four blood markers. Scand J Med Sci Sports 21:235–243
Breidbach A, Catlin DH, Green GA, Tregub I, Truong H, Gorzek J (2003) Detection of recombinant human erythropoietin in urine by isoelectric focusing. Clin Chem 49:901–907
Malcovati L, Pascutto C, Cazzola M (2003) Hematologic passport for athletes competing in endurance sports: a feasibility study. Haematologica 88:570–581
Sharpe K, Ashenden MJ, Schumacher YO (2006) A third generation approach to detect erythropoietin abuse in athletes. Haematologica 91:356–63
Sottas PE, Robinson N, Giraud S, Taroni F, Kamber M, Mangin P, Saugy M (2006) Statistical classification of abnormal blood profiles in athletes. International J Biostat 2:1–21
Sottas PE, Robinson N, Saugy M (2010) The athlete’s biological passport and indirect markers of blood doping. Handb Exp Pharmacol 305–26
Robinson N, Sottas PE, Mangin P, Saugy M (2007) Bayesian detection of abnormal hematological values to introduce a no-start rule for heterogeneous populations of athletes. Haematologica 92:1143–1144
Ahlgrim C, Pottgiesser T, Robinson N, Sottas PE, Ruecker G, Schumacher YO (2010) Are 10 min of seating enough to guarantee stable haemoglobin and haematocrit readings for the athlete’s biological passport? Int J Lab Hematol 32:506–511
Robinson N, Sottas PE, Pottgiesser T, Schumacher YO, Saugy M (2011) Stability and robustness of blood variables in an antidoping context. Int J Lab Hematol 33:146–153
WADA (2012) World anti-doping code international standard for laboratories, version 7.0. WADA, Lausanne
Lippi G, Banfi G, Maffulli N (2010) Preanalytical variability: the dark side of the moon in blood doping screening. Eur J Appl Physiol 109:1003–1005
Banfi G, Lombardi G, Colombini A, Lippi G (2010) A world apart: inaccuracies of laboratory methodologies in antidoping testing. Clin Chim Acta 411:1003–1008
Lombardi G, Lanteri P, Colombini A, Lippi G, Banfi G (2011) Stability of haematological parameters and its relevance on the athlete’s biological passport model. Sports Med 41:1033–1042
Robinson N, Mangin P, Saugy M (2004) Time and temperature dependant changes in red blood cell analytes used for testing recombinant erythropoietin abuse in sports. Clin Lab 50:317–323
Voss SC, Flenker U, Majer B, Schänzer W (2008) Stability tests for hematological parameters in antidoping analyses. Lab Hematol 14:24–29
Imeri F, Herklotz R, Risch L, Arbetsleitner C, Zerlauth M, Risch GM, Huber AR (2008) Stability of hematological analytes depends on the hematology analyser used: a stability study with Bayer Advia 120, Beckman Coulter LH 750 and Sysmex XE 2100. Clin Chim Acta 397:68–71
Voss SC, Alsayrafi M, Alsowaidi N, Elzain Elgingo M, Bourdon P, Robinson N, Sottas PE, Klodt F, Nonis D, Schumacher YO (2011) The influence of exercise and circadian rhythm of haemoglobin concentration associated changes in plasma volume on the biological passport. Br J Sports Med 45:A7
Schumacher YO, Sahm D, Baumstark MW, Pottgiesser T (2010) Reticulocytes in athletes: longitudinal aspects and the influence of long- and short-term exercise. Drug Test Anal 2:469–474
Schumacher YO, Wenning M, Robinson N, Sottas P-E, Ruecker G, Pottgiesser T (2010) Diurnal and exercise-related variability of haemoglobin and reticulocytes in athletes. Int J Sports Med 31:225–230
Schumacher YO, Pottgiesser T (2011) The impact of acute gastroenteritis on haematological markers used for the athletes biological passport - report of 5 cases. Int J Sports Med 32:147–150
Schumacher YO, Klodt F, Nonis D, Pottgiesser T, Alsayrafi M, Bourdon PC, Voss SC (2012) The impact of long-haul air travel on variables of the athlete’s biological passport. Int J Lab Hematol. doi:10.1111/j.1751-553X.2012.01450.x
Sottas P-E, Vernec A (2012) Current implementation and future of the athlete biological passport. Bioanalysis 4:1645–1652
CAS (2010) http://www.tas-cas.org; TAS 2010/A/2235 UCI v. Tadej Valjavec & Olympic Committee of Slovenia
CAS (2010) http://www.tas-cas.org: TAS 2010/A/2178 Pietro Caucchioli. CONI & UCI
Zorzoli M, Rossi F (2010) Implementation of the biological passport: the experience of the International Cycling Union. Drug Test Anal 2:542–547
Monfort N, Ventura R, Latorre A, Belalcazar V, López M, Segura J (2010) Urinary di-(2-ethylhexyl)phthalate metabolites in athletes as screening measure for illicit blood doping: a comparison study with patients receiving blood transfusion. Transfusion 50:145–149
Monfort N, Ventura R, Platen P, Hinrichs T, Brixius K, Schänzer W, Thevis M, Geyer H, Segura J (2012) Plasticizers excreted in urine: indication of autologous blood transfusion in sports. Transfusion 52:647–657
Solymos E, Guddat S, Geyer H, Thomas A, Thevis M, Schänzer W (2011) Di(2-ethylhexyl) phthalate metabolites as markers for blood transfusion in doping control: intra-individual variability of urinary concentrations. Drug Test Anal 3:892–895
Solymos E, Guddat S, Geyer H, Flenker U, Thomas A, Segura J, Ventura R, Platen P, Schulte-Mattler M, Thevis M, Schänzer W (2011) Rapid determination of urinary di(2-ethylhexyl) phthalate metabolites based on liquid chromatography/tandem mass spectrometry as a marker for blood transfusion in sports drug testing. Anal Bioanal Chem 401:517–528
Monfort N, Ventura R, Balcells G, Segura J (2012) Determination of five di-(2-ethylhexyl)phthalate metabolites in urine by UPLC-MS/MS, markers of blood transfusion misuse in sports. J Chromatogr B Anal Technol Biomed Life Sci 908:113–121
Schmidt W, Prommer N (2005) The optimised CO-rebreathing method: a new tool to determine total haemoglobin mass routinely. Eur J Appl Physiol 95:486–495
Pottgiesser T, Umhau M, Ahlgrim C, Ruthardt S, Roecker K, Schumacher YO (2007) Hb mass measurement suitable to screen for illicit autologous blood transfusions. Med Sci Sports Exerc 39:1748–1756
Prommer N, Sottas PE, Schoch C, Schumacher YO, Schmidt W (2008) Total hemoglobin mass–a new parameter to detect blood doping? Med Sci Sports Exerc 40:2112–2118
Pottgiesser T, Specker W, Umhau M, Roecker K, Schumacher YO (2009) Post-transfusion stability of haemoglobin mass. Vox Sang 96:119–127
Pottgiesser T, Specker W, Umhau M, Dickhuth HH, Roecker K, Schumacher YO (2008) Recovery of hemoglobin mass after blood donation. Transfusion 48:1390–1397
Eastwood A, Hopkins WG, Bourdon PC, Withers RT, Gore CJ (2008) Stability of hemoglobin mass over 100 days in active men. J Appl Physiol 104:982–985
Eastwood A, Sharpe K, Bourdon PC, Woolford SM, Saunders PU, Robertson EY, Clark SA, Gore CJ (2012) Within-subject variation in hemoglobin mass in elite athletes. Med Sci Sports Exerc 44:725–732
Garvican LA, Eastwood A, Martin DT, Ross ML, Gripper A, Gore CJ (2010) Stability of hemoglobin mass during a 6-day UCI ProTour cycling race. Clin J Sport Med 20:200–204
Schumacher YO, Pottgiesser T, Ahlgrim C, Ruthardt S, Dickhuth HH, Roecker K (2008) Haemoglobin mass in cyclists during stage racing. Int J Sports Med 29:372–378
Pottgiesser T, Echteler T, Sottas P-E, Umhau M, Schumacher YO (2012) Hemoglobin mass and biological passport for the detection of autologous blood doping. Med Sci Sports Exerc 44:835–843
Lundby C, Robach P (2010) Assessment of total haemoglobin mass: can it detect erythropoietin-induced blood manipulations? Eur J Appl Physiol 108:197–200
Gough CE, Sharpe K, Ashenden MJ, Anson JM, Saunders PU, Garvican LA, Bonetti DL, Gore CJ, Prommer N (2011) Quality control technique to reduce the variability of longitudinal measurement of hemoglobin mass. Scand J Med Sci Sports 21:e365–371
Alexander AC, Garvican LA, Burge CM, Clark SA, Plowman JS, Gore CJ (2011) Standardising analysis of carbon monoxide rebreathing for application in anti-doping. J Sci Med Sport 14:100–105
Leuenberger N, Jan N, Pradervand S, Robinson N, Saugy M (2011) Circulating microRNAs as long-term biomarkers for the detection of erythropoiesis-stimulating agent abuse. Drug Test Anal 3:771–776
Nikolovski Z, De La Torre C, Chiva C, Borràs E, Andreu D, Ventura R, Segura J (2012) Alterations of the erythrocyte membrane proteome and cytoskeleton network during storage–a possible tool to identify autologous blood transfusion. Drug Test Anal 4:882–890
Marrocco C, Pallotta V, D’alessandro A, Alves G, Zolla L (2012) Red blood cell populations and membrane levels of peroxiredoxin 2 as candidate biomarkers to reveal blood doping. Blood Transfus 10(Suppl 2):s71–77
Pottgiesser T, Schumacher YO, Funke H, Rennert K, Baumstark MW, Neunuebel K, Mosig S (2009) Gene expression in the detection of autologous blood transfusion in sports–a pilot study. Vox Sang 96:333–336
Christensen B, Sackmann-Sala L, Cruz-Topete D, Jørgensen JOL, Jessen N, Lundby C, Kopchick JJ (2011) Novel serum biomarkers for erythropoietin use in humans: a proteomic approach. J Appl Physiol 110:149–156
Berglund B, Birgegård G, Wide L, Pihlstedt P (1989) Effects of blood transfusions on some hematological variables in endurance athletes. Med Sci Sports Exerc 21:637–642
Lainé F, Laviolle B, Ropert M, Bouguen G, Morcet J, Hamon C, Massart C, Westermann M, Deugnier Y, Loréal O (2012) Early effects of erythropoietin on serum hepcidin and serum iron bioavailability in healthy volunteers. Eur J Appl Physiol 112:1391–1397
Teale P, Barton C, Driver PM, Kay RG (2009) Biomarkers: unrealized potential in sports doping analysis. Bioanalysis 1:1103–1118
Reichel C (2011) OMICS-strategies and methods in the fight against doping. Forensic Sci Int 213:20–34
Acknowledgments
The authors declare that they have no conflict of interest relevant to the manuscript submitted. T.P. received a WADA grant for 2012 (11B16TP). Y.O.S. acted as an independent expert for different anti-doping stakeholders in several doping cases.
Author information
Authors and Affiliations
Corresponding author
Additional information
Published in the topical collection Anti-doping Analysis with guest editor Christopher Harrison.
Rights and permissions
About this article
Cite this article
Pottgiesser, T., Schumacher, Y.O. Current strategies of blood doping detection. Anal Bioanal Chem 405, 9625–9639 (2013). https://doi.org/10.1007/s00216-013-7270-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00216-013-7270-x