Abstract
Breath analysis could offer a non-invasive means of intravenous drug monitoring if robust correlations between drug concentrations in breath and blood can be established. In this study, propofol blood and breath concentrations were determined in an animal model under varying physiological conditions. Propofol concentrations in breath were determined by means of two independently calibrated analytical methods: continuous, real-time proton transfer reaction mass spectrometry (PTR-MS) and discontinuous solid-phase micro-extraction coupled with gas chromatography mass spectrometry (SPME-GC-MS). Blood concentrations were determined by means of SPME-GC-MS. Effects of changes in pulmonary blood flow resulting in a decreased cardiac output (CO) and effects of dobutamine administration resulting in an increased CO on propofol breath concentrations and on the correlation between propofol blood and breath concentrations were investigated in seven acutely instrumented pigs. Discontinuous propofol determination in breath by means of alveolar sampling and SPME-GC-MS showed good agreement (R 2 = 0.959) with continuous alveolar real-time measurement by means of PTR-MS. In all investigated animals, increasing cardiac output led to a deterioration of the relationship between breath and blood propofol concentrations (R 2 = 0.783 for gas chromatography-mass spectrometry and R 2 = 0.795 for PTR-MS). Decreasing pulmonary blood flow and cardiac output through banding of the pulmonary artery did not significantly affect the relationship between propofol breath and blood concentrations (R 2 > 0.90). Estimation of propofol blood concentrations from exhaled alveolar concentrations seems possible by means of different analytical methods even when cardiac output is decreased. Increases in cardiac output preclude prediction of blood propofol concentration from exhaled concentrations.

Experimental setup for simultaneous real-time (PTR-MS) and discontinuous (SPME-GC-MS) drug determination in the breath of acutely instrumented pigs (A). In order to assess the influence of hemodynamic variables pulmonary artery blood flow was determined by means of Doppler-measurement (B).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Monitoring of anesthetic drug levels during anesthesia or sedation could assist in controlling anesthetic depth and may thus contribute to patient safety in terms of avoiding inadequate anesthetic depth.
Propofol (2,6-diisopropylphenol) is frequently used as part of total intravenous anesthesia and for sedation in the ICU. In contrast to volatile anesthetics, real-time monitoring of intravenous propofol concentrations is not yet available. Conventional determination of propofol blood or plasma concentrations still requires sophisticated and time-consuming techniques. Recent publications demonstrated that physicochemical properties of propofol allow the detection of propofol in expired air [1]. If propofol breath concentrations reflected propofol blood concentrations, non-invasive real-time monitoring of propofol could be possible. In pilot studies, authors reported that intravenously administered propofol could be detected in patients’ breath, and good correlations between blood and breath concentrations were found [2, 3].
Before breath analysis of drugs can be used in routine clinical practice, exhalation kinetics of the drugs has to be understood and the scope of application has to be clearly defined. During anesthesia, changes of ventilation/perfusion ratios of the lung as well as increases or decreases of cardiac output regularly occur due to mechanical ventilation and hemodynamic side effects of volatile or IV anesthetics. It is known from recent work that physiological parameters such as ventilation/perfusion ratio resulted in changes of propofol blood/breath correlation coefficients [4].
This study was intended to systematically assess the effects of cardiac output and pulmonary blood flow on propofol exhalation especially in terms of the ratio between propofol blood and breath concentrations. In an acutely instrumented animal model, effects of increased or decreased cardiac output on the correlation between propofol blood and breath concentrations were investigated. In addition, the validity of continuous proton transfer mass spectrometry (PTR-MS) and discontinuous gas chromatography mass spectrometry (GC-MS) for the determination of propofol in exhaled breath were analyzed.
Experimental
Subjects
Animal experiments were approved by the governmental ethical board for animal research in Mecklenburg-Vorpommern, Germany. Seven German Landrace pigs were investigated.
Anesthesia
After overnight fasting and receiving water ad libitum, seven German Landrace pigs (five male, two female) with body weights ranging from 30–33 kg were pre-medicated intramuscularly with 4 mg/kg azaperone (Janssen-Cilag GmbH, Neuss, Germany) and 0.2 mg/kg midazolam (Dormicum®, Hoffmann La Roche AG, Grenzach-Wyhlen, Germany). After installation of standard monitoring (SpO2, ECG) and pre-oxygenation with 100% oxygen, anesthesia was induced intravenously via ear vein cannulation (Braunüle® 18 G, B. Braun Melsungen AG, Melsungen, Germany) with 6–8 μg/kg of fentanyl (Fentanyl-Janssen®; Janssen-Cilag, Neuss, Germany), 250 mg (7–8 mg/kg) thiopental (AltanaPharma, Konstanz, Germany), and 2–4 mg midazolam. Pigs were orally intubated with an endotracheal tube (ID 7.5 mm, Mallinckrodt, Hazelwood, MO, USA) after injection of 0.3 mg/kg pancuronium (DeltaSelect, Dreieich, Germany). Anesthesia was maintained by a continuous intravenous infusion of midazolam (0.25–0.3 mg⋅kg−1⋅h−1), pancuronium (0.15 mg⋅kg−1⋅h−1), and intermittent bolus application of 2–5 μg/kg fentanyl until instrumentation was finished. Volume-controlled mechanical ventilation was provided by a Servo900® ventilator (Siemens, Erlangen, Germany). Respiratory rate and tidal volume were adjusted at the beginning of the experiment to maintain an arterial partial pressure of carbon dioxide (PaCO2) at 36–42 mmHg (4.8–5.6 kPa). FiO2 was reduced to 0.4, and a positive end-expiratory pressure of 5 cm H2O was applied to maintain an arterial partial pressure of oxygen (PaO2) at 90–112 mmHg (12–15 kPa). Ventilatory settings were then kept constant during the experiment. End-tidal carbon dioxide partial pressure (PetCO2) was determined by means of mainstream capnometry. Dead space ventilation was estimated according to the formula Vd/Vt = (PaCO2 – PetCO2)/PaCO2 [5].
Instrumentation
After induction of anesthesia, animals were placed in supine position on a heating pad to keep body temperature constant at 37 °C. A triluminal central venous catheter (CVC) and a Swan-Ganz thermodilution catheter (PAC) were inserted via the right internal jugular vein.
The right femoral artery was cannulated with an arterial PiCCO-catheter (PVPK2015L20-46 N 5 F, Pulsion Medical Systems, Munich, Germany) for continuous monitoring of the arterial blood pressure and hemodynamic measurements (cardiac output, stroke volume, intra-thoracic blood volume index, extra-vascular lung water). Body temperature was monitored continuously with the PiCCO-catheter and kept at 37 ± 0.5 °C. For maintenance of normovolemia, all animals received an intravenous electrolyte solution (Jonosteril®; Fresenius, Bad Homburg, Germany) at 6–10 mg⋅kg−1⋅h−1 throughout the experiments. Additional fluid was infused according to PiCCO-catheter hemodynamic measurements.
The thorax was opened by a mid-sternotomy. The main pulmonary artery was looped with a cotton ribbon acting as a broad vessel loop. In the following experimental setting, the pulmonary artery was partially occluded by means of the vessel loop. The aim was to occlude the pulmonary artery in order to reduce the blood flow by 30% minimum and 50% maximum. The pulmonary artery blood flow was monitored by an ultrasonic perivascular flow probe (Transonic Systems Inc., Ithaca, USA) of appropriate size, which was placed around the pulmonary artery. The vessel had to fill 75–100% of the probe’s acoustic window. An improved signal quality was provided with perivascular ultrasonic gel.
All intravascular catheters were connected to pressure transducers. Signals of all catheters and the flow probe were recorded via PO-NE-MAH® (Digital Acquisition Analysis and Archive Systems, Simsbury, USA) [6]. Analyzed parameters were heart rate, arterial pressure, central venous pressure, pulmonary artery pressure and pulmonary capillary wedge pressure, cardiac output (thermodilution method via PAC), and pulmonary artery blood flow. In addition, cardiac output, intra-thoracic blood volume, and extra-vascular lung water were determined by thermodilution (mean of three injections of 20 ml ice-cold saline using the PiCCO-System. Hemoglobin, hematocrit, arterial and mixed venous blood gases, pH, base excess, bicarbonate, blood electrolytes, and glucose concentrations were determined by means of an autoanalyzer (Bayer Diagnostics 348, Bayer Vital, Fernwald, Germany).
Experimental procedures
After induction of anesthesia and insertion of CVC, PAC and PiCCO-catheter, the PTR-MS system was connected to the breathing system of the respirator. The midazolam infusion was stopped, and a bolus dose of 2 mg/kg propofol (Propofol-Lipuro®, B. Braun Melsungen AG, Melsungen, Germany) was administered, followed by a continuous propofol infusion of 6–8 mg⋅kg−1⋅h−1. Alveolar breath concentrations of propofol were measured online by means of PTR-MS.
At several preset time points, breath and blood samples were drawn simultaneously and analyzed by means of solid-phase micro-extraction coupled with gas chromatography mass spectrometry (SPME-GC-MS; as described later). A detailed sampling scheme is shown in Fig. 1. Hemodynamic and respiratory parameters, pulmonary artery blood flow, temperature, and the results of arterial and mixed venous blood gas analysis were recorded at the same time.
Schedule of the experimental procedures. Discontinuous SPME-GC-MS analyses of breath and blood (broken line) at 11 preset time points and continuous PTR-MS-measurement of breath (solid line) are shown on their respective time scales. Administration of propofol bolus and hemodynamic interventions like pulmonary banding and dobutamine dosage are illustrated by means of thick gray lines. The black dots at the time scales indicate data points used for statistical regression analyses
After 1 h of propofol infusion (with assumed steady-state 1 (StS1) of propofol blood concentrations), pulmonary blood flow was reduced by banding of the main pulmonary artery. Guided by ultrasound measurement of pulmonary blood flow, the partial occlusion of the main pulmonary artery had to be adjusted until the aim of PAF-reduction (30–50%) was achieved. The banding was removed after 60 min, and within the following 10 min, recovery was facilitated. Measurements were carried out 20, 40 and 60 min after the beginning of pulmonary artery banding and 10 min after reperfusion (steady-state 2 (StS2)).
According to the second part of the experimental protocol, the influence of dobutamine administration and increase of cardiac output (by approximately 40%) on propofol breath gas concentrations was investigated. A continuous intravenous dobutamine infusion (6 μg⋅kg−1⋅min−1) was administered for a period of 30 min. Measurements were carried out during 10, 20, and 30 min of dobutamine infusion and finally 20 min after stop of catecholamine infusion.
Propofol measurements
Propofol breath concentrations were determined by means of two independently calibrated analytical methods: continuous real-time PTR-MS and discontinuous SPME-GC-MS. In parallel to the GC-MS measurements in breath, propofol blood concentrations were analyzed by means of headspace solid-phase micro-extraction coupled with gas chromatography mass spectrometry at preset time points. A detailed sampling scheme for all breath and blood measurements is shown in Fig. 1.
-
1.
Real-time PTR-MS-measurements of propofol in breath
Continuous PTR-MS online measurements of propofol concentrations in alveolar breath using a CO2-triggered sampling device [7] were performed with a first-generation high-sensitivity PTR-MS (IONICON, Innsbruck, Austria). The transfer line was an MXT-Hydroguard column (2 m × 0.53 mm, internal diameter × 1.0 μm film thickness, BGB-Analytik, Schlossboeckelheim, Germany); it was connected to PTR using a custom-made interface. Both inlet and interface were heated by a heating hose and a heating jacket (Horst GmbH, Lorsch, Germany) up to 90 °C. Pressure in the drift tube of the PTR-MS was approximately at 2.055 mbar; drift tube voltage was set at 400 V, and drift tube temperature was held at approximately 90 °C. The quantification of exhaled propofol was performed by means of daily external calibration. Detection limit was 0.036 nmol/L, and the quantitation limit was 0.053 nmol/L. Linear range of the method was 0–2.68 nmol/L.
-
2.
Discontinuous GC-MS measurements of propofol in breath and blood
Simultaneous offline sampling of alveolar breath, arterial and mixed venous blood, and quantitative analysis of propofol breath and blood concentrations were performed as described before [4, 8] by means of SPME and GC-MS. Propofol detection limits were 0.006 nmol/L in breath and 72.20 nmol/L in blood; the quantitation limits were 0.009 nmol/L and 75.89 nmol/L (breath/blood). Intraday precision was 8–11% and recovery 97–103%. The linear range of the method was 0–1.45 nmol/L for propofol analysis in breath gas (R 2 = 0.995) and 0–120 μmol/L for the determination of propofol in blood (R 2 = 0.996).
Breath gas sampling
Alveolar breath samples (15 ml per sample) were withdrawn under visual control of exhaled CO2 and immediately transferred into sealed 20 ml headspace vials. End-tidal PCO2 was monitored in all pigs by a fast-responding infrared absorption mainstream CO2 monitor (Capnogard, Novametrix, USA) allowing real-time CO2 detection. A stainless steel T-piece and the CO2 measuring cuvette were introduced into the respiratory system near the endotracheal tube. Fifteen milliliters of exhaled air were withdrawn during the alveolar phase of the capnogram into a gastight glass syringe connected to the stainless T-piece and immediately transferred into an evacuated sealed 20 mL headspace vial. In order to exclude propofol accumulation within the respiratory system, inspired gas was collected during inspiration near the respirator.
All breath samples were immediately spiked with thymol as an internal standard and processed within 6 h after sampling.
Blood sampling
Arterial and mixed venous blood samples (2.7 ml per sample) were withdrawn from pigs’ arterial catheter and PAC into heparin anticoagulated tubes and transferred into 20 ml evacuated sealed headspace vials filled with 7 ml phosphate buffer [9] and thymol as an internal standard. All blood samples were processed within 6 h after sampling.
SPME-GC-MS-analysis of breath and blood
Breath and blood samples were preconcentrated by solid-phase micro-extraction (SPME fiber: CAR/PDMS/DVB, SUPELCO, Bellefonte, USA; 10 min equilibration time at 40 °C) and analyzed by GC-MS (AGILENT 7980/5975) as described before [4]. Electron Ionization (70 eV), a scan rate of 3 scans/s at a mass range 35–250 amu was applied. Ion trace of 163 m/z was used for quantitation. Calibration with internal standardization was accomplished by linear regression analysis curve fitting. Peak area ratios of target analytes and internal standards were calculated by AGILENT MSD ChemStation software (version E.02.00.493).
Statistical analysis
For statistical evaluation, correlation and linear regression analyses for propofol breath vs. propofol blood concentrations were performed. For comparison of GC-MS and PTR-MS determination of propofol breath concentrations, Bland–Altman statistics were used. Statistical calculations were performed using SigmaStat 3.5/SigmaPlot 10.0.
Results
Smirnov–Kolmogorov testing showed that data were normally distributed. Figure 2 shows mean values of exhaled propofol concentrations from all animals as continuously measured by means of PTR-MS over the whole time course of the experiment. Data were normalized to the values obtained at steady-state after end of pulmonary artery banding (StS2) to reduce interindividual variations.
Results of continuous PTR measurements from the beginning until the end of the experiments. Values are shown as means±SD. Results were normalized to StS2 (c**_ex_PTR). Zero on the time scale corresponds to steady-state 2 (StS2, recovery 10 min after end of pulmonary banding). Pulmonary artery banding was done before StS2. Dobutamine was administered after StS2
Linear regression analysis of exhaled concentrations measured by two independent analytical methods showed excellent agreement (R 2 = 0.959) between discontinuous SPME-GC-MS and continuous real-time PTR-MS (Fig. 3a). The accordance of the two (independent) methods was confirmed by Bland–Altman testing (Fig. 3b).
a Regression analysis for the relationship between exhaled propofol concentrations measured by means of PTR-MS (c_ex_PTR, [ppb]) and exhaled propofol concentrations determined by means of GC-MS (c_ex_GC, [ppb]). b Bland–Altman plot for the comparison of results from PTR-MS (c_ex_PTR) with results from GC-MS (c_ex_GC) for all seven animals and all 11 time points. Means (c_ex_PTR+c_ex_GC)/2 and differences (c_ex_PTR−c_ex_GC) were calculated for 22 measurements per animal (11 by means of PTR-MS and 11 by means of GC-MS). Reference lines represent lower and upper limit of agreement (bias ± 1.96*standard deviation)
There was good agreement between pulmonary blood flow and cardiac output determined by means of thermodilution (PAC and PiCCO; Fig. 4).
Mean cardiac output values±SD for the 11 time points of the experiment determined by means of thermodilution via pulmonary artery catheter (CO_PAC, green line, [l/min]) and by means of transpulmonary thermodilution via PiCCO (CO_PiCCO, red line, [l/min]) in relation to pulmonary blood flow (PBF, blue line, [l/min])
Dead space ventilation at base status was 12%, increased up to 22% during pulmonary artery banding, and decreased to 7% during dobutamine administration.
Propofol concentrations in arterial and mixed venous blood were almost identical (R 2 = 0.989, p < 0.001). Mean propofol breath concentrations (as measured by GC-MS and PTR-MS), mean arterial and venous blood concentrations, as well as corresponding mean pulmonary blood flow for all animals and all preset time points of the experiment are shown in Fig. 5.
Breath propofol concentrations (c_ex_GC and c_ex_PTR, [ppb]), arterial (c_art, [μg/ml]), and mixed venous (c_ven, [μg/ml]) concentrations of propofol in relation to pulmonary blood flow (PBF, [l/min]). Breath and blood concentrations are shown as mean±SEM calculated from quantitative data for 11 time points of all seven animals
The results of linear regression analysis for the relation between propofol breath and blood concentrations are shown in Table 1 (n = 7 pigs, calculations carried out for all 11 stages of the experiment and separately for stages with decreased and increased cardiac output).
Linear regression analysis for the relation between propofol blood concentrations (arterial and mixed venous) and propofol breath concentrations yielded regression coefficients (R 2) between 0.621 and 0.685 for GC-MS and 0.597 and 0.669 for PTR-MS (n = 7 pigs, calculations carried out for all 11 stages of the experiment).
When calculations were carried out for stages 1 (base status) and 3–7 (StS1, pulmonary banding) of the experiment, linear regression analysis for the relation between propofol blood and breath concentrations yielded regression coefficients (R 2) between 0.906 and 0.935 for GC-MS and 0.925 and 0.952 for PTR-MS.
When calculations were carried out for stages 1 (base line) and 8–11 (dobutamine infusion) of the experiment, linear regression analysis for the relation between propofol breath and blood concentrations yielded regression coefficients (R 2) between 0.783 and 0.815 for GC-MS and 0.795 and 0.838 for PTR-MS.
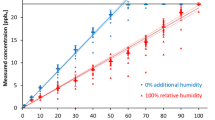
Figure 6 shows relations between mean arterial blood and breath concentrations during pulmonary artery banding and during dobutamine administration as measured by means of SPME-GC-MS.
Relationship between mean arterial (c_art, [μg/ml]) and mean exhaled (c_ex_GC, [ppb]) propofol concentrations. Red dots represent concentrations determined during base line, steady-state, and pulmonary artery banding. Blue crosses represent concentrations determined during baseline and dobutamine infusion. The points red dot over blue cross represent propofol concentrations at baseline and those determined after the end of dobutamine infusion
Discussion
As conventional analysis of propofol from blood is invasive and time-consuming, this method cannot be used for onsite monitoring or tailoring of propofol application during anesthesia or sedation. Non-invasive breath analysis may be used for therapeutic drug monitoring whenever drugs or their metabolites are volatile enough to be determined in exhaled breath. Authors of several studies [1, 2, 10] concluded that propofol breath monitoring during anesthesia could be possible.
If propofol breath concentrations are to be used to estimate propofol blood concentrations during anesthesia or sedation, propofol determination in breath has to be reliable and reproducible, and a robust and reliable correlation between propofol breath and blood concentrations has to be established. Ninety-eight percent of injected propofol is bound to plasma protein and erythrocytes. The free and pharmacologically active fraction in blood was determined as 1.2–1.7% [11]. In order to derive therapeutic decisions, e.g., increasing or decreasing the amount of infused propofol, blood concentrations estimated from breath concentrations have to be reproducibly close to actual free blood levels.
Time courses of propofol plasma concentrations after IV application can be described in a three-compartment model [12, 13]. Initially, plasma concentrations quickly drop due to the short half-life (2–4 min, α-phase) of distribution into well-perfused compartments. Elimination half-life during the ß-phase is about 30–60 min. After the ß-phase, a γ-elimination phase is described. During γ-elimination phase, plasma concentrations slowly decrease (t1/2 180–320 min up to 475 min [12]), as propofol is redistributed from less perfused compartments (“deep compartments”, such as lipid tissues). As nearly 100% of cardiac output passes through the lungs, exhalation of propofol starts immediately after injection. The amount of drug that comes into the alveoli mainly depends on blood-gas partitioning. In terms of non-invasive propofol monitoring by means of breath analysis, crucial issues are steady-state of (plasma) concentrations and how closely breath and blood concentrations are correlated. There is strong evidence that, after bolus injection and during initial phases of drug infusion, there is neither steady-state nor is there a reliable correlation between breath and blood concentration of the drug.
Results from a previous study in patients after thoracotomy and lung resection led to the conclusion that physiological parameters may have a significant impact on the correlation between propofol blood and breath concentrations [4].
In agreement with recently published studies [4, 14], we found a correlation between arterial, mixed venous, and alveolar propofol concentrations. However, the strength of this correlation, i.e., the reliability of the estimation of propofol blood concentrations from propofol breath concentrations, depended on variations of cardiac output.
If cardiac output was increased during dobutamine infusion, the arterial and mixed venous propofol concentrations and expired concentrations diverged. From literature, there is some information on changes of propofol blood concentrations under increasing cardiac output: An inverse relation between cardiac output and propofol blood concentrations has already been observed by Kurita et al. [15] who attributed these effects to cardiac output-dependent distribution of the drug between different compartments [16]. Myburgh et al. [17] explained a significant reduction in arterial propofol concentrations induced by increased cardiac output after catecholamine infusion in a sheep model with a mechanism based on increased first-pass dilution and clearance of propofol secondary to the increased cardiac output. Takizawa et al. [18] suggested from results of a patient study that the resulting decrease of propofol blood levels could be of clinical relevance.
Up to now, no study has investigated the effect of catecholamine application on the propofol exhalation and propofol blood/breath correlations. Surprisingly, propofol breath concentrations decreased in a less pronounced way than propofol blood concentrations when cardiac output was increased. Two effects may possibly have contributed to this phenomenon:
-
The lung represents one of the compartments into which propofol is redistributed when cardiac output is increased, i.e., the effects of decreasing arterial concentrations on the drug exhalation might be partially compensated by increasing propofol concentrations in the lung.
-
As dead space ventilation decreased considerably when cardiac output was increased, propofol exhalation might have been facilitated through an improved ventilation perfusion ratio. However, this hypothesis is in contrast to multiple inert gas elimination theory. [19, 20] As water solubility of propofol (0.124 mg/ml) falls between solubility of ethane (0.057 mg/ml) and solubility of cyclopropane (0.502 mg/ml), propofol exhalation through the lung should not significantly be affected by dead space ventilation.
Due to intraoperative stress, liberation of endogenous catecholamines or administration of these drugs for hemodynamic stabilization increases of cardiac output may frequently occur during anesthesia and sedation. In these cases, reliability of estimation of propofol blood concentrations from exhaled concentrations may be seriously impaired. Erroneously high or low concentrations may thus be deduced resulting in inadequate depth of anesthesia.
In order to investigate the effects of decreasing pulmonary blood flow and consecutive impairment of the ventilation perfusion ratio on propofol exhalation, pulmonary blood flow was reduced by means of banding of the main pulmonary artery. Previous animal studies described pulmonary artery banding as a model for pulmonary hypertension with consecutive right ventricular pressure load [21–23]. In this study, ultrasound-guided reduction of pulmonary blood flow by pulmonary artery banding under constant mechanical ventilation additionally allowed the investigation of propofol exhalation changes caused by dead space ventilation.
Banding of the pulmonary artery until 30–50% reduction of the pulmonary artery blood flow was achieved resulted in a reproducible reduction of cardiac output accompanied by hypotension and tachycardia in all pigs. As minute ventilation was kept constant, dead space ventilation increased. In contrast to the conditions under dobutamine infusion, propofol concentrations in blood and breath increased in the same way when cardiac output decreased, and dead space ventilation increased. This may be explained by the following reasons:
-
Inversely to the conditions when cardiac output increased, propofol was redistributed to a less extent into the body compartments when cardiac output and pulmonary blood flow decreased. This consequently resulted in an increase of propofol blood concentrations and in an increase of propofol exhalation. As pulmonary blood flow was decreased, there was no extra distribution of propofol into the lung as in the case of increasing cardiac output under dobutamine infusion and, as a consequence, increasing propofol blood concentrations resulted in proportionally increasing breath concentrations.
-
The fact that propofol exhalation apparently was not affected by increasing dead space ventilation is in agreement with multiple inert gas elimination theory [19, 20] (see above).
The different impact of increasing and decreasing cardiac outputs on the relationship of propofol breath and blood concentrations is most probably due to the particular distribution of the drug. The lack of effect of dead space ventilation on propofol exhalation can be explained by multiple inert gas elimination theory. Dead space ventilation seems to have no relevant effect on breath/blood ratios of propofol.
Apart from these physiological considerations, important methodological issues were addressed in this study. Drugs and their metabolites represent typical blood-borne substances which are ingested or injected, distributed into the different compartments of the body, and which are then transported to the lungs via the bloodstream. When passing through the lung capillaries, substances cross the alveolar–capillary membrane and substance concentrations corresponding to the blood-gas partition coefficients are built up in the alveoli [8, 9, 24, 25]. Thus, only substance concentrations in the alveolar portion of breath correlate well with concentrations in blood [24, 26]. Therefore, we used CO2 controlled alveolar sampling [8, 24, 27] for all measurements of exhaled propofol concentrations. An automatic CO2 controlled sampling device [7] was applied to provide the PTR-MS instrument continuously with alveolar air. Rapid changes of exhaled drug concentrations and development of drug concentrations over the time course could easily be monitored by means of the adapted PTR-MS technique. The excellent correlation between discontinuous GC-MS data and continuous PTR-MS measurements proved efficacy and reliability of this technique.
Conclusions
In conclusion, estimation of propofol blood concentration from exhaled concentrations is not affected when cardiac output is decreased. Increases in cardiac output preclude prediction of blood propofol concentration from exhaled concentrations.
References
Harrison GR, Critchley AD, Mayhew CA, Thompson JM (2003) Real-time breath monitoring of propofol and its volatile metabolites during surgery using a novel mass spectrometric technique: a feasibility study. Br J Anaesth 91(6):797–799
Takita A, Masui K, Kazama T (2007) On-line monitoring of end-tidal propofol concentration in anesthetized patients. Anesthesiology 106(4):659–664
Hornuss C, Praun S, Villinger J, Dornauer A, Moehnle P, Dolch M, Weninger E, Chouker A, Feil C, Briegel J, Thiel M, Schelling G (2007) Real-time monitoring of propofol in expired air in humans undergoing total intravenous anesthesia. Anesthesiology 106(4):665–674
Miekisch W, Fuchs P, Kamysek S, Neumann C, Schubert JK (2008) Assessment of propofol concentrations in human breath and blood by means of HS-SPME-GC-MS. Clin Chim Acta 395(1–2):32–37
Hardman JG, Aitkenhead AR (2003) Estimating alveolar dead space from the arterial to end-tidal CO(2) gradient: a modeling analysis. Anesth Analg 97(6):1846–1851
Roesner JP, Petzelbauer P, Koch A, Tran N, Iber T, Mutz C, Vollmar B, Noldge-Schomburg GE, Zacharowski K (2009) A double blind, single centre, sub-chronic reperfusion trial evaluating FX06 following haemorrhagic shock in pigs. Resuscitation 80(2):264–271
Miekisch W, Hengstenberg A, Kischkel S, Beckmann U, Mieth M, Schubert JK (2010) Construction and evaluation of a versatile CO2 controlled breath collection device. IEEE Sens J 10(1):211–215. doi:10.1109/Jsen.2009.2035757
Birken T, Schubert J, Miekisch W, Noldge-Schomburg G (2006) A novel visually CO2 controlled alveolar breath sampling technique. Technol Health Care 14(6):499–506
Miekisch W, Schubert JK, Vagts DA, Geiger K (2001) Analysis of volatile disease markers in blood. Clin Chem 47(6):1053–1060
Perl T, Carstens E, Hirn A, Quintel M, Vautz W, Nolte J, Junger M (2009) Determination of serum propofol concentrations by breath analysis using ion mobility spectrometry. Br J Anaesth 103(6):822–827
Mazoit JX, Samii K (1999) Binding of propofol to blood components: implications for pharmacokinetics and for pharmacodynamics. Br J Clin Pharmacol 47(1):35–42
Langley MS, Heel RC (1988) Propofol. A review of its pharmacodynamic and pharmacokinetic properties and use as an intravenous anaesthetic. Drugs 35(4):334–372
Gepts E, Camu F, Cockshott ID, Douglas EJ (1987) Disposition of propofol administered as constant rate intravenous infusions in humans. Anesth Analg 66(12):1256–1263
Grossherr M, Hengstenberg A, Meier T, Dibbelt L, Gerlach K, Gehring H (2006) Discontinuous monitoring of propofol concentrations in expired alveolar gas and in arterial and venous plasma during artificial ventilation. Anesthesiology 104(4):786–790
Kurita T, Morita K, Kazama T, Sato S (2002) Influence of cardiac output on plasma propofol concentrations during constant infusion in swine. Anesthesiology 96(6):1498–1503
Upton RN (2000) Relationships between steady state blood concentrations and cardiac output during intravenous infusions. Biopharm Drug Dispos 21(2):69–76
Myburgh JA, Upton RN, Grant C, Martinez A (2001) Epinephrine, norepinephrine and dopamine infusions decrease propofol concentrations during continuous propofol infusion in an ovine model. Intensive Care Med 27(1):276–282
Takizawa D, Nishikawa K, Sato E, Hiraoka H, Yamamoto K, Saito S, Horiuchi R, Goto F (2005) A dopamine infusion decreases propofol concentration during epidural blockade under general anesthesia. Can J Anaesth 52(5):463–466
Rodriguez-Roisin R, Wagner PD (1990) Clinical relevance of ventilation–perfusion inequality determined by inert gas elimination. Eur Respir J 3(4):469–482
Wagner PD (2008) The multiple inert gas elimination technique (MIGET). Intensive Care Med 34(6):994–1001
Bauer EP, Kuki S, Zimmermann R, Schaper W (1998) Upregulated and downregulated transcription of myocardial genes after pulmonary artery banding in pigs. Ann Thorac Surg 66(2):527–531
Cusimano RJ, Ashe KA, Abel JG, Lichtenstein SV, Salerno TA (1988) A simple model of right ventricular hypertrophy. J Invest Surg 1(1):45–53
Muhlfeld C, Coulibaly M, Dorge H, Sellin C, Liakopoulos O, Ballat C, Richter J, Schoendube F (2004) Ultrastructure of right ventricular myocardium subjected to acute pressure load. Thorac Cardiovasc Surg 52(6):328–333
Schubert JK, Spittler KH, Braun G, Geiger K, Guttmann J (2001) CO(2)-controlled sampling of alveolar gas in mechanically ventilated patients. J Appl Physiol 90(2):486–492
Cope KA, Watson MT, Foster WM, Sehnert SS, Risby TH (2004) Effects of ventilation on the collection of exhaled breath in humans. J Appl Physiol 96(4):1371–1379
Schubert JK, Miekisch W, Birken T, Geiger K, Noldge-Schomburg GF (2005) Impact of inspired substance concentrations on the results of breath analysis in mechanically ventilated patients. Biomarkers 10(2–3):138–152
Miekisch W, Kischkel S, Sawacki A, Liebau T, Mieth M, Schubert JK (2008) Impact of sampling procedures onto results of breath analysis. J Breath Res 2:026007
Acknowledgments
The authors thank all members of the anesthesia research group from the Department of Anesthesia and Intensive Care for their precious support during realization of the animal study and data acquisition.
Author information
Authors and Affiliations
Corresponding author
Additional information
Published in the special issue Biomarkers with Guest Editors Boguslaw Buszewski and Jochen Schubert.
Rights and permissions
About this article
Cite this article
Kamysek, S., Fuchs, P., Schwoebel, H. et al. Drug detection in breath: effects of pulmonary blood flow and cardiac output on propofol exhalation. Anal Bioanal Chem 401, 2093–2102 (2011). https://doi.org/10.1007/s00216-011-5099-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00216-011-5099-8