Abstract
All presently used batteries contain reactive, corrosive or toxic components and require strong cases, usually made of steel. As a battery is miniaturized, the required case dominates its size. Hence, the smallest manufactured batteries are about 50 mm3 in size, much larger then the integrated circuits or sensors of functional analytical packages, as exemplified by implantable glucose sensors for diabetes management. The status of the miniaturization of the power sources of such implantable packages is reviewed. Three microcells, consisting only of potentially harmless subcutaneously implantable anodes and cathodes, are considered. Because their electrolyte would be the subcutaneous interstitial fluid, the cells do not have a case. One potentially implantable cell has a miniature Nafion-coated Zn anode and a biocompatible hydrogel-shielded Ag/AgCl cathode. The core innovation on which the cell is based is the growth of a hopeite-phase Zn2+ conducting solid electrolyte film on the discharging anode. The film blocks the transport of O2 to the Zn, preventing its corrosion, while allowing the necessary transport of Zn2+. The second cell, with the same anode, would have a bioinert hydrogel-shielded wired bilirubin oxidase-coated carbon cathode, on which O2 dissolved in the subcutaneous fluid would be electroreduced to water. In the third cell, the glucose of the subcutaneous interstitial would be electrooxidized to gluconolactone at an implanted wired glucose anode, similar to that tested now for continuous glucose monitoring in diabetic people, and O2 in the subcutaneous fluid would be electroreduced to water on its wired bilirubin oxidase cathode.

Similar content being viewed by others
Avoid common mistakes on your manuscript.
The need for a miniature power source
The sizes of electronic systems are defined by their displays and by their batteries. The battery and the display are also the largest components of the most widely used analytical systems, the blood glucose monitors used by diabetic people. Our recent research has been aimed at miniaturizing power sources and integrating them into disposable and implantable electronic subsystems. Potential advantages of such integration are: (a) avoidance of electrical connectors, particularly of separable but hermetic connectors, currently needed if the user of an on-the-skin medical electronic device is to shower, bathe or swim; and (b) improved reliability, as electrical contacts are particularly frequent sources of failure.
Because the energy released in the oxidation of a reductant scales with its mass, the miniaturization of power sources, even if the oxidant is O2 from air, can impact only on systems that do not consume much power or operate for long periods. An example of such a system is the subcutaneously implanted part of a continuous glucose monitor for the management of diabetes [1–3]. In its present manufacturable version [4], a disposable amperometric sensor is implanted once or twice a week by the user. The implanted part is a plastic strip small enough (about 0.5 cm long, 500 μm wide and 200 μm thick) to be implanted with little or no pain. It is connected to large, printed, contact pads on the skin. The contact pads are connected to a permanent electronic package, containing a potentiostat, an amplifier, an RF transmitter and the battery that powers these. The potentiostat, amplifier and transmitter could be integrated into a chip with a footprint of ∼ 1 mm2, mass produced for ∼ 50¢. The battery, however, is large. The smallest commercially available Zn–air battery is about 50 mm3, and its energy capacity is about 60 mWh. The integrated, disposable, miniature, subcutaneously implanted glucose monitoring sensor-transmitter would consume <1 mWh in a week. If intermittently interrogated by a transponder, the power consumed would be even less.
The small batteries manufactured at the moment, usually zinc–air, zinc–silver oxide or lithium–manganese dioxide cells, are difficult to miniaturize because they require a steel case in order to contain the caustic KOHaq of Zn batteries, or lithium (which reacts rapidly with water). The steel of the case is thick enough to prevent harm to a child biting on the battery (not an uncommon occurrence). Because the volume fraction of the case increases upon miniaturization, size reduction, though feasible, becomes impractical. The battery could be miniaturized if the anode and the cathode, as well as their reaction products, were safe enough for implantation into the subcutaneous interstitial fluid, so that the fluid would serve as the electrolyte, meaing that the need for both the electrolytic solution and case would be removed.
Progress toward an implantable caseless microbattery that uses subcutaneous fluid as electrolyte
The anode of the original version of the Zn (Hg)∣NH4Claq∣MnO2/C battery (patented by Georges Leclanchè in 1866 and widely used after about 1880 in its “dry” embodiment, where the NH4Claqu electrolyte wetted a sheet of porous paper between the anode and the cathode) corroded rapidly, in a few weeks, by reacting with dissolved O2 [5]. The shelf life of Leclanchè’s battery was short, and its zinc utilization efficiency was poor. To lower the corrosion potential and corrosion rate, the NH4Claq was replaced in 1960 by KOHaqu [6], which is now used in all Zn-anode batteries. These “alkaline” cells required a steel case, which has imposed a limit on their practical miniaturization. As the volume of the electroactive ingredients decreased, the volume fraction of the case increased.
In a step toward an implantable battery, the KOHaq electrolyte was eliminated, opening a route to eliminating the case and allow practical microbatteries. Specifically, the O2-associated corrosion of zinc anodes was reduced in a pH 7.4 physiological (0.15 M NaCl, 20 mM phosphate) buffer solution by the growth of hopeite-phase Zn3(PO4)2.4 H2O on the discharging anode [7]. The out-diffusing Zn2+, generated in the anode reaction Zn → Zn2+ + 2e−, was precipitated on the surface of Nafion-coated Zn anodes by phosphate, to form nonporous lamellae of hopeite-phase Zn3(PO4)2 4 H2O. Surprisingly, the hopeite-phase Zn3(PO4)2.4 H2O is a Zn2+ cation-conducting solid electrolyte [7]. Nonporous inorganic films are usually impermeable to gases, including O2. Hence, they block or reduce corrosion. However, because they are rarely ionic conductors, the corrosion-protected anodes cannot usually be discharged and are not useful in batteries. Because the Zn2+-conductive hopeite prevented the permeation of O2 to the electroactive metallic Zn surface, the anodes were discharged with a high zinc utilization (“current”) efficiency, even when their surface-to-volume ratios were high and their rates of discharge were slow. For example, the zinc utilization efficiency of 120 μm-diameter Zn fiber anodes, discharged over three weeks, was 86% [7]. Growth of the nonporous hopeite lamellae and high anode utilization efficiency required precoating with a polyanion, like Nafion, and addition of a halide salt like NaCl.
The anodes were discharged with little polarization, even when they were overgrown by 100 μm-thick hopeite films. At a current density of 0.13 mA cm−2, the excess polarization of the half-discharged, 100 μm hopeite-overgrown anodes was less than 50 mV. At 0.26 mA cm−1, the polarization of the half-discharged anodes exceeded their initial polarization only by about 110 mV. The ionic conductance of the hopeite lamellae was >2×10−3 S.
Hopeite is an open-framework hydrated zinc phosphate with intersecting channels. It is a known host of neutral organic molecules and cations, resembling zeolites in this aspect. The crystal consists of layers of ZnO4 tetrahedra, linked by PO4 groupings (Fig. 1). Between these two sheets, a crystallographically separate Zn atom, Zn1 (Fig. 1) is present in octahedrally coordinated units of ZnO2(H2O)4. Two oxygen atoms are shared with two separate PO4 tetrahedra. The four water molecules form a hydrogen-bonded network [8, 9]. This Zn2+ atom site is rich in the Zn2+ vacancies necessary for the diffusion of the Zn2+ cations.
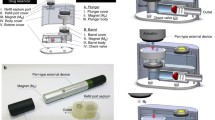
The potentially implantable Zn–AgCl cell
The zinc anodes, as well as the pH 7.3 physiological buffer electrolyte of the foreseen cells, are harmless enough to be considered for implantation. The first cathode that we explored was the implantable Ag/AgCl cathode, used in the continuous glucose monitor of Abbott Diabetes Care (Alameda, CA) and its predecessor, TheraSense [4]. The patient-replaced subcutaneously implanted sensing element of the monitor is an elongated rectangular plastic strip; glucose is electrooxidized at the anode side of this strip and AgCl was electroreduced to Ag and Cl− at its cathode side. The Ag/AgCl side is overcoated with a polymer allowing the out-diffusion of the Cl− generated in the cathode reaction [10]. Because the Ag/AgCl was used in the body, and because even the Ag(Hg) amalgam has been used for many years to fill dental cavities, we expect that the Ag/AgCl cathode should be safe to implant. Figure 2 shows a schematic drawing of the disposable subsystem of the foreseen continuous glucose monitor.
Tests of the Zn(Nafion)–Ag/AgCl cell showed that the nonporous, Zn2+-conducting, hopeite-phase Zn3(PO4)2·4 H2O also grows on the Nafion-coated zinc anode when the pH 7.4, 0.15 M NaCl, 20 mM phosphate buffer is replaced by serum, and that the zinc utilization efficiency remains near 60% when the cell is discharged at a two-week rate at 1 V [7]. Hence, it is projected that the cell will operate in the less fouling subcutaneous interstitial fluid at least as well as it operated in serum. The cell could be very simple, consisting merely of a Zn paste, screen printed on one side of the pole of a plastic flag, and overprinted with a Nafion emulsion, and a Ag/AgCl paste printed on the opposite side of the pole, overprinted with a polymer allowing the out-diffusion of the Cl− generated in the cathode reaction [10]. A schematic diagram of such a cell is shown in Fig. 2.
Status of the subcutaneously implantable Zn–O2 microcell
The energy density of the implantable cell would be increased about tenfold if an air cathode was used instead of AgCl/Ag. At physiological pH, the cathode could be wired bilirubin oxidase O2 [11], overcoated with a bioinert O2-permeable, proton-transporting polymer or hydrogel [12]. Current glucose-O2 biofuel cells operate for about a week in pH 7.3 physiological buffer [11, 13–16] containing 0.14 M NaCl and 20 mM phosphate; for about a day in the living grape [17], the sap of which is particularly rich in glucose; but only for hours in serum [18, 19]. The concentrations of proteins and many other constituents in the subcutaneous interstitial fluid is considerably lower than in serum, so stability testing of the wired bilirubin oxidase O2 cathode in serum is excessively, and possibly unnecessarily, harsh.
Status of the implantable glucose–O2 miniature biofuel cell
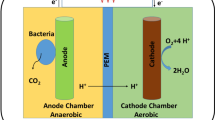
Energy capacity would not be limiting in a cell utilizing glucose and O2 of the subcutaneous interstitial (intercellular) fluid, which is blood-supplied. In the glucose–O2 biofuel cell, neither the cathodic reactant, O2, nor the anodic reactant, glucose, is cell-contained; instead they diffuse to the electrodes from the subcutaneous fluid. Consequently, this type of cell would be the smallest. Its present laboratory version consists merely of two 7 μm-diameter, 2 cm-long carbon fibers [20], one being the wired glucose oxidase-coated anode, and the other the wired bilirubin oxidase-coated cathode [15]. The cell operates optimally at 0.6 V [15], where its power density is about 4.8 μW mm−2 of carbon fiber area. The best enzyme wires are electron-conducting redox hydrogels. These are permeable to glucose and O2; to gluconolactone, the glucose oxidation product; and to ions. For the best wires, the apparent electron diffusion coefficient reaches 5.8×10−6cm2 s −1 [14, 16].
The wired bilirubin oxidase is a faster electrocatalyst (by nearly an order of magnitude) than the wired glucose oxidase and, if the transport of glucose and O2 were rapid, for example under fast flow conditions, the power output of the cell would be anode-limited. In the absence of forced flow (stirring), the power is cathode-limited because the concentration of O2 in the subcutaneous interstitial fluid is only about 0.2 mM, and its flux to the cathode limits the current. In the present design, this problem is alleviated by using long and small-diameter (high surface/volume ratio) carbon fibers. In weeklong operation at 37 °C, the cell generates ∼1 J of electrical energy while a 2 C of charge is passed. This 2 C charge exceeds about a hundredfold the 0.016 C charge that would have been passed in the discharge of a zinc fiber anode of similar dimensions (7 μm diameter, 2 cm long) at 100% utilization efficiency.
Unlike other fuel and biofuel cells, the enzyme wiring-based glucose–O2 cell is simple and potentially inexpensive, because its anode and cathode compartments need not be separated by a membrane. If a sophisticated ion-transporting, reactant-transport-blocking membrane were needed, as it is in other fuel cells (to prevent access of H2 or methanol to the O2 or air cathode and access of O2 to the H2 or methanol oxidizing anode), it would be difficult to miniaturize. The need for the membrane is avoided in biofuel cells because the anodic and cathodic electrocatalysts are wired enzymes. Unlike the platinum alloy electrocatalysts of other fuel cells, the wired enzyme electrocatalysts are so selective for the substrates of their enzymes that neither the crossover of glucose to the cathode compartment nor the crossover of O2 to the anode compartment prevents the operation of the cell. Furthermore, unlike the platinum alloy-utilizing cathodes, which are rapidly poisoned by carbon-containing oxidation intermediates, the wired bilirubin oxidase cathode is not poisoned by glucose or by its oxidation product, gluconolactone. Because the cell does not have diffusional anodic or cathodic redox mediators that would short it (due to the mediator that is reduced at the anode diffusing to and being oxidized at the cathode; or the mediator that is oxidized at the cathode diffusing to and being reduced at the anode), there is no need for the compartments to be separated. In the absence of a membrane, the biofuel cell merely consists of the two wired enzyme-coated electrodes, which would be overcoated in the actually implantable version with bioinert hydrogels, permeable to glucose, O2 and ions [12].
Summary and conclusion
Recent research indicates that electrochemical power sources far smaller than the smallest presently manufactured batteries could be formed by subcutaneously implanting an anode and a cathode. These are listed, along with the smallest presently commercially available batteries, in Table 1. The first of these, which is ready for in vivo studies, is the Zn–AgCl cell, where a corrosion-preventing, yet Zn2+ ion-conducting, film of hopeite-phase Zn3 (PO4)2.4 H2O precipitates during the discharge on the Zn anode [7].
In the second cell likely to be implemented, which has a tenfold greater energy density and a higher power density, the AgCl cathode would be replaced with a wired bilirubin oxidase cathode, on which O2 is electroreduced to water at an overpotential considerably smaller than that for platinum-based alloys [21, 22]. This cathode works well for about two weeks in a pH 7.4 physiological saline buffer solution at 37 °C, but not yet in serum [18, 19]. The third power source, the glucose–O2 biofuel cell, would be by far the smallest of the cells, because it would draw its reactants from the subcutaneous interstitial fluid. The cell utilizes a wired glucose oxidase anode [14–16, 23, 24] and a wired bilirubin oxidase cathode [11, 22, 25]. It works for a week in pH 7.4 physiological saline buffer solution at 37 °C and for a day in a grape [17, 26]. The implanted glucose electrooxidizing anode has been successfully used in diabetic volunteers for monitoring glucose in the subcutaneous interstitial fluid [4, 27]. However, its wired bilirubin oxidase cathode is as yet unstable in serum [18, 19]. The stabilization of the cathode operating in the subcutaneous interstitial fluid, which is currently being investigated, would open the way to implanting the Zn–O2 microcell and the glucose–O2 miniature biofuel cell.
References
Csöregi E, Schmidtke DW, Heller A (1995) Anal Chem 67:1240–1244
Heller A (1999) Annu Rev Biomed Eng 1:153–175
Wagner JG, Schmidtke DW, Quinn CP, Fleming TF, Bernacky B, Heller A (1998) Proc Natl Acad Sci USA 95:6379–6382
Feldman B, Brazg R, Schwartz S, Weinstein R (2003) Diabetes Technol Ther 5:769–779
Boto KG, Williams LFG (1977) J Electroanal Chem 77:1–20
Kordesch K (1962) US Patent 3,042,732, issued on July 3, 1962
Shin W, Lee J, Kim Y, Steinfink H, Heller A (2005) J Am Chem Soc 127:14590–14591
Whitaker A (1975) Acta Crystallogr B31:2026–2035
Whitaker A (1978) Acta Crystallogr B34:2385–2386
Feldman B, Liu Z, Mao F, Heller A (2005) US Patent Application 20050173245, published on August 11, 2005
Mano N, Kim H-H, Zhang Y, Heller A (2002) J Am Chem Soc 124:6480–6486
Hubbell JA, Kornfield JA, Tae G (2005) US Patent Application 2000559984, published on April 26, 2000
Mano N, Mao F, Heller A (2002) J Am Chem Soc 124:12962–12963
Mao F, Mano N, Heller A (2003) J Am Chem Soc 125:4951–4957
Mano N, Mao F, Heller A (2004) ChemBioChem 5:1703–1705
Mano N, Mao F, Heller A (2005) J Electroanal Chem 574:347–357
Mano N, Mao F, Heller A (2003) J Am Chem Soc 125:6588–6594
Kang C, Shin H, Zhang Y-C, Heller A (2004) Bioelectrochemistry 65:83–88
Kang C, Shin H, Heller A (2006) Bioelectrochemistry 68:22–26
Chen T, Barton SC, Binyamin G, Gao Z, Zhang Y, Kim H-H, Heller A (2001) J Am Chem Soc 123:8630–8631
Mano N, Fernandez Jose L, Kim Y, Shin W, Bard Allen J, Heller A (2003) J Am Chem Soc 125:15290–15291
Fernandez JL, Mano N, Heller A, Bard AJ (2004) Angew Chem Int Edit 43:6355–6357
Binyamin G, Chen T, Heller A (2001) J Electroanal Chem 500:604–611
Mano N, Mao F, Heller A (2004) Chem Commun 2116–2117
Mano N, Kim H-H, Heller A (2002) J Phys Chem B 106:8842–8848
Heller A (2004) Phys Chem Chem Phys 6:209–216
Heller A (2005) AIChE J 51:1054–1066
Acknowledgements
The writing of this review was supported in part by the Welch Foundation and the U.S. Office of Naval Research.
Author information
Authors and Affiliations
Corresponding author
Additional information
Part of the material reviewed was included in the authors lecture on the occasion of his receipt of the Fransenius Gold Medal and Prize of the Gesellschaft Deutscher Chemiker at ANAKON in Regensburg, Germany, on February 17, 2005.
Rights and permissions
About this article
Cite this article
Heller, A. Potentially implantable miniature batteries. Anal Bioanal Chem 385, 469–473 (2006). https://doi.org/10.1007/s00216-006-0326-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00216-006-0326-4