Abstract
Objectives
Previous studies have investigated the occupancy of the serotonin reuptake transporter (SERT) after clinical doses of citalopram and other selective serotonin reuptake inhibitors. In the present study, the occupancies of SERT after multiple doses of escitalopram and citalopram were compared using the radioligand [123I]ADAM and single photon emission computed tomography (SPECT).
Methods
Fifteen healthy subjects received escitalopram 10 mg/day (n = 6) or citalopram 20 mg/day (n = 9) for a total of 10 days. SERT occupancies in midbrain were determined with SPECT and [123I]ADAM at three different time points: at baseline (no medication) and at 6 and 54 h after last drug intake.
Results
At 6 h after the last dose, mean SERT occupancies were 81.5 ± 5.4% (mean±SD) for escitalopram and 64.0 ± 12.7% for citalopram (p < 0.01). At 54 h after the last dose, mean SERT occupancies were 63.3 ± 12.1% for escitalopram and 49.0 ± 11.7% for citalopram (p < 0.05). The plasma concentrations of the S-enantiomer were of the same magnitude in both substances. For both drugs, the elimination rate of the S-enantiomer in plasma was markedly higher than the occupancy decline rate in the midbrain.
Conclusion
The significantly higher occupancy of SERT after multiple doses of escitalopram compared to citalopram indicates an increased inhibition of SERT by escitalopram. The results can also be explained by an attenuating effect of R-citalopram on the occupancy of S-citalopram at the SERT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The serotonin reuptake transporter (SERT, 5-HTT) is the primary target for selective serotonin reuptake inhibitors (SSRI), which are commonly used for treatment of psychiatric disorders and as first-line treatment for major depression and anxiety disorders (Bauer et al. 2002). Among the group of SSRIs, citalopram represents a widely prescribed SSRI (Noble and Benfield 1997). It is a racemic mixture of S(+)- and R(−)-citalopram. Escitalopram is the therapeutically active S-enantiomer of citalopram, which modulates the serotonin reuptake activity and is therefore thought to be responsible for the pharmacological effects (Kasper 2004; Murdoch and Keam 2005). Escitalopram binds to both the primary site of the SERT and on an allosteric site (Sanchez et al. 2004). It is approved for the treatment of depression and anxiety disorders.
Meyer et al. (2004) reported SSRI occupancy rates for various SSRIs with the positron-emission tomography (PET) ligand [11C] DASB. They found a SERT occupancy of 76% for 10 mg citalopram, 79% for 20 mg citalopram, and 85% for 40 mg citalopram, and that the in vitro median effective concentration (EC50) does not correlate with affinity. This demonstrated that although target-specific affinity is obviously a very important feature of a drug, it does not predict the occupancy value in vivo, even when plasma levels are known (Meyer et al. 2004).
On the other hand, Herold et al. (2006) reported a mean occupancy of SERT of 61% (single photon emission computed tomography [SPECT] methodology, ADAM ligand) in depressed patients after treatment for 7 days with 10 mg/day of citalopram. A recent SPECT study using the radioligand [123I]ADAM performed by Klein et al. (2006) found a dose-dependent, statistically significant increase from 60 to 75% in occupancies of SERT after single doses of escitalopram (5, 10, and 20 mg), while the occupancies after citalopram (10 and 20 mg) did not demonstrate statistically significant differences (65–70%). Furthermore, no statistically significant difference in the occupancy was found when comparing equimolar doses of escitalopram and citalopram (i.e., 10 mg escitalopram with 20 mg citalopram; Klein et al. 2006).
In the present study, the occupancy of SERT after multiple doses of escitalopram and citalopram was compared using the radioligand [123I]ADAM and single photon emission computed tomography (SPECT). The doses investigated were equal with respect to the amount of the S-enantiomer, i.e., 10 mg escitalopram and 20 mg citalopram. We hypothesized that SERT occupancy rates would be higher for escitalopram than for citalopram at steady state after multiple dose-intake 6 h after last dose.
Materials and methods
Subjects
The study protocol and all procedures were approved by the research ethics committee of the Medical University of Vienna, Austria. Twenty healthy male subjects (mean age 27 ± 6 years) without past or current neuropsychiatric history, as established by a structured clinical interview for DSM-IV (Mini International Neuropsychiatric Interview, German version 5.0.0), were included into the study. The subjects that fulfilled the inclusion criteria and did not meet any exclusion criteria were enrolled into the study after they signed the informed consent form.
All 20 subjects received treatment with escitalopram or citalopram. Five subjects were excluded from the SPECT data analysis due to software error during the SPECT scan (n = 2), troubles with the shipment of the radioligand (n = 2), or unavailability of the magnetic resonance imaging (MRI) scanner (n = 1). The 15 subjects included in the further data analysis had a mean age (±SD) of 28 ± 7 years (range 20–47 years).
Drug treatment
After the screening visit, each subject was randomly assigned to one of two medication groups (10 mg/day escitalopram or 20 mg/day citalopram, treatment period of 10 days) by an unblinded study coordinator, who was not involved in the procedures of the SPECT data acquisition or data analysis. Of the 15 subjects available for the SPECT data analysis, 6 received 10 mg escitalopram and 9 were treated with 20 mg citalopram. Adverse events were assessed by the UKU side effects scale at the end of the study (Lingjaerde et al. 1987).
Radioligand
[123I]ADAM (2-((2-((dimethylamino)methyl)phenyl)thio)-5-iodophenylamine) was used as a highly specific SPECT radioligand for the SERT. [123I]ADAM was synthesized at MAP Medical Technologies Oy, Tikkakoski, Finland, as previously described (Oya et al. 2000) and purified with a high-performance liquid chromatography (HPLC) system as described by Klein et al. (2006).
SPECT and MRI scan
All subjects underwent a magnetic resonance scan (T1-weighted, matrix 256 × 256, GE Sigma 1.5 Tesla scanner) to improve the regions of interest (ROIs) definition on coregistered images.
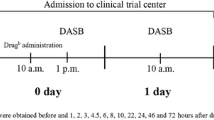
In total, three SPECT scans were performed: (1) a baseline scan without medication, (2) a scan 6 h, and (3) a scan 54 h after last study drug administration. The radioligand was administered intravenously as bolus injection. In the citalopram treatment group, the mean±SD amount of injected activity of [123I]ADAM was 165 ± 18, 158 ± 17, and 173 ± 2 MBq for the first, second, and third measurement sessions, respectively. In the escitalopram group, subjects received 175 ± 20, 162 ± 17, and 146 ± 41 MBq for scans one, two, and three, respectively. SPECT scans were performed with a three-headed rotating scintillation camera (Siemens MultiSPECT 3), equipped with medium energy collimators after blockade of thyroid uptake with 600 mg sodium perchlorate 30 min before tracer application. SPECT investigations were performed about 275 min after tracer application (Sacher et al. 2006), and the data were collected as described by Klein et al. (2006). A total of 180 frames (60/camera head) was collected using a step and shoot mode. A 128 × 128 matrix was used and the slice thickness of cross-sections was 3.5 mm. Reconstruction was performed with filtered back projection and a Butterworth filter (cutoff frequency 0.7, order 7). Finally, attenuation correction with an attenuation coefficient of 0.12/cm was done after drawing an ellipse around the head contour. Characteristics on the SPECT scan and administration of the radiotracer for both groups are shown in Table 1.
Data analysis
In each subject the structural magnetic resonance image was coregistered to the corresponding SPECT image using a neuroimaging software package (RView®). The ROIs including the midbrain/hypothalamus and the cerebellum were drawn on each coregistered MRI/SPECT data volume by a single examiner blind to the treatment details using a manually defined template. These ROIs were transferred to the corresponding SPECT images. Data were analyzed as the mean count rate within the ROIs. Counts in midbrain/hypothalamic regions were calculated in three consecutive axial slices using the highest mean values to avoid tilting errors. The three midbrain/hypothalamic ROIs (three slices) and the six cerebellar ROIs (three slices, left + right) were each pooled together, then the average counts per pixel were calculated. Because of the very low density of SERT in the cerebellum, the activity measured in the cerebellar ROI represents mainly unspecific binding, whereas the midbrain/hypothalamic ROI represents specific and unspecific binding (Backstrom et al. 1989; Kish et al. 2005). The occupancy in midbrain/hypothalamus was expressed as percentage and calculated for each subject according to the following equation:
where binding potential (BP)1 is binding potential without medication and BP2 with medication (for more details see Klein et al. 2006).
Pharmacokinetic analysis
The term “S-citalopram” will be used for plasma concentration of the S-enantiomer, whereas “escitalopram” will be used when referring to the study medication. Blood samples for pharmacokinetic analysis were obtained at predose on day 10, before and after the 6 h SPECT scan, at 8, 10, and 24 h postdose, and before and after the 54 h SPECT scan. Nominal sampling times were used, and the time points before and after the two postdose SPECT scans were set to 5.5 and 6.5 h and 53.5 and 54.5 h, respectively. Plasma samples were analyzed for S- and R-citalopram using an enantiomer-selective HPLC mass spectrometry (MS)/MS, as described by Gutierrez et al. (2003). The pharmacokinetic parameters t max, C max, AUCss, and t 1/2 on day 10 of dosing were estimated for S-citalopram and R-citalopram with standard noncompartmental analysis using WinNonlin Professional (version 4.1, Pharsight). Differences in the pharmacokinetic parameters t max, C max, AUCss, and t 1/2 of S-citalopram after administration of citalopram and escitalopram were analyzed with a t test, with the significance level set to 0.05.
Pharmacodynamic analysis
Differences in mean SERT occupancy values between escitalopram and citalopram 6 and 54 h postdose were tested using a t test. The rate of decline in occupancy for escitalopram and citalopram was estimated by linear regression of the logarithmic mean occupancy values at 6 and 54 h for each compound.
An E max model was used to describe the relationship between the S-citalopram plasma concentrations and the SERT occupancy values by means of non-linear regression analysis (NLMIXED). The following model was used:
where C is the S-citalopram plasma concentration immediately before the SPECT scan, E max is the maximum occupancy, and EC50 is the S-citalopram concentration giving rise to half the maximum occupancy (i.e., apparent equilibrium association constant). All pharmacodynamic analyses were performed with the statistical software SAS®, version 8.2.
Results
Fifteen of the initial 20 subjects were included in the pharmacokinetic and pharmacodynamic data analysis. Five subjects dropped out as specified above. Nine subjects received 20 mg/day citalopram, and six subjects received 10 mg/day escitalopram for 10 days. There were no significant demographic differences between the two treatment groups at baseline (Table 1).
SERT occupancy at 6 and 54 h post last dose
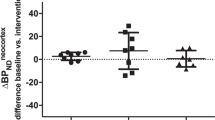
At 6 h after last dose, the mean (±SD) SERT occupancy in the midbrain was 81.5% (±5.4) for 10 mg/day escitalopram and 64.0% (±12.7) for 20 mg/day citalopram (p = 0.008), despite similar plasma concentrations of S-citalopram. At 54 h after the last dose, the mean SERT occupancy was 63.3% (±12.1) for escitalopram and 49.0% (±11.7) for citalopram (p = 0.04). The mean occupancy values were significantly higher for escitalopram compared to citalopram (p = 0.005; Fig. 1).
SERT occupancy relative to plasma levels of escitalopram
Figure 2 shows the individual midbrain SERT occupancy values 6 and 54 h after last intake of study medication vs S-citalopram plasma concentrations immediately before the SPECT scans with the fitted E max model overlaid.
Individual SERT occupancy values (%) vs S-citalopram serum concentrations after administration of escitalopram (10 mg/day, n = 6) or citalopram (20 mg/day, n = 9) for 10 days. Data are shown for day 10 (6 h after last medication) and day 12 (54 h after last medication) together. Single data points as well as the corresponding fitted E max curves are shown for both 10 mg/day escitalopram (ESC) and 20 mg/day citalopram (CIT). These data indicate a significantly higher blockade of SERT by escitalopram compared to citalopram (p = 0.03)
The estimated mean (±SE) E max values for 10 mg/day escitalopram and 20 mg/day citalopram were 89.6% (±5.7) and 71.8% (±4.8), respectively. The EC50 values were estimated to be 5.3 nmol/l (±1.6) and 5.7 nmol/l (±1.8) for escitalopram and citalopram, respectively. A significantly higher (p = 0.03) E max value was estimated after administration of escitalopram compared to citalopram, whereas no significant difference was observed between escitalopram and citalopram for the EC50 (p = 0.84).
SERT occupancy and plasma level over time
Pairwise comparison revealed a statistically significant decrease in SERT occupancy in midbrain between the first SPECT scan (6 h after last dose) and the second scan after the last dose (54 h after last dose) for 10 mg/day escitalopram (p < 0.01) and 20 mg/day citalopram (p < 0.05). Figure 3 shows the mean SERT occupancies for 10 mg escitalopram and 20 mg citalopram together with the mean plasma concentration-time profiles for S-citalopram. A decrease of approximately 50% in occupancy (based on the two time points from 6 to 54 h postdose) was estimated to be approximately 130 h after dose for both escitalopram and citalopram.
Pharmacokinetics
The pharmacokinetic results are summarized in Table 2. Plots of time vs S-citalopram concentration in plasma for 10 mg escitalopram and 20 mg citalopram are shown in Fig. 3. The mean (±SD) t max of S-citalopram was 7.8 h (±6.1) and 5.5 h (±0.0) for 20 mg citalopram and 10 mg escitalopram, respectively. For S-citalopram, the mean C max (±SD) was 51.7 nmol/l (±15.8) and 51.4 nmol/l (±12.9), mean t 1/2 (±SD) was 24.6 h (±8.0) and 24.2 h (±5.2), for 20 mg/day citalopram and 10 mg/day escitalopram, respectively. In the 20 mg/day citalopram group, the following parameters for R-citalopram were found: t max = 7.8 h (±6.1), C max = 85.4 nmol/l (±31.8) and t 1/2 = 39.1 h (±11.7). No significant difference for the pharmacokinetic parameters t max, C max and t 1/2 of S-citalopram between the citalopram and escitalopram groups were found.
The ratio of R-citalopram to S-citalopram in the 20 mg/day citalopram group is shown in Table 2. The ratio was lowest immediately before the SPECT scan 6 h postdose, with a mean (±SD) value of 1.6 (±0.3). Immediately before the SPECT scan 54 h postdose, the R/S ratio increased to a mean value of 2.9 (±1.2).
Adverse events
Adverse events were reported by four out of six in the escitalopram group and five out of nine subjects in the citalopram group. All adverse events were rated as “mild” according to the UKU scale (Lingjaerde et al. 1987).
Discussion
In the present study, SERT occupancy was investigated in the midbrain of healthy subjects after multiple dose administration (10 days) of equivalent doses of escitalopram and citalopram, with respect to the amount of S-citalopram (i.e., 10 mg/day escitalopram or 20 mg/day citalopram). The results indicate that 10 mg of escitalopram has a higher SERT occupancy than 20 mg of citalopram after multiple dose administration. Furthermore, the SERT occupancy relative to plasma levels of escitalopram is lower when subjects are treated with the racemate (citalopram). For both medications, there is no difference in the SERT occupancy decline rate after the last dose given.
The higher SERT occupancy for escitalopram vs citalopram is in contrast to occupancy values obtained in a recent single-dose comparison of equimolar doses of escitalopram and citalopram using the same methodology (Klein et al. 2006). In that study, SERT occupancy values were similar (60–75% for escitalopram and 65–70% for citalopram) following single doses of escitalopram (5, 10, 20 mg) and citalopram (10 and 20 mg). Our finding of a higher occupancy for escitalopram in this study can be explained by multiple dosing. There may either be an adaptive process over time, or an attenuating effect of R-citalopram on the degree of occupancy of SERT, which is more apparent when the relative concentration of R-enantiomer is high compared to the S-enantiomer, as it is the case after multiple, but not single doses (Klein et al. 2006).
A higher occupancy after the administration of escitalopram may result in a more complete inhibition of SERT and thus lead to a potentiation of the serotonergic output, as described in preclinical microdialysis experiments (Mork et al. 2003). This mechanism may offer the promising possibility for escitalopram vs citalopram to have therapeutic advantages, as has recently been substantiated by the findings of head-to-head short-term (Moore et al. 2005) and long-term (Colonna et al. 2005) studies in depressed patients.
Meyer et al. (2001, 2004) have previously investigated the occupancy of SERT after different doses of citalopram (20–60 mg) and several other SSRIs using the PET ligand [11C]DASB and found mean occupancy values of approximately 80% after 4 weeks of treatment at therapeutic doses. An 80% occupancy is in accordance with the results from this study for escitalopram, whereas a lower mean occupancy value was found at steady state for citalopram. However, direct comparisons of the data with our study must be made with caution. First, Meyer et al. (2004) administered higher doses of citalopram (20 mg up to 60 mg) for a longer duration (10 vs 28 days) than we did. Second, it has to be acknowledged that [11C-DASB] represents the gold standard PET ligand for SERT-imaging providing quantitative results compared to the semiquantitative measurements with the [123I]ADAM SPECT methodology. Third, there was no stereoselective analysis of the different fractions of S- and R-enantiomers included in that PET study but only the sum of both enantiomers quoted.
In our study, a difference between brain and plasma kinetics of citalopram and escitalopram was observed. Whereas the plasma elimination half-life was 25–40 h for S- and R-citalopram, the SERT occupancy decline rate (based on the two time points) was approximately 130 h for both escitalopram and citalopram. A similar discrepancy between decline in plasma concentrations and brain occupancy for antipsychotics was previously shown by Tauscher et al. (2002a), whereas Takano et al. (2006) could demonstrate a reasonable relationship between plasma and brain kinetics for the SSRI fluvoxamine. Based on Takano’s results, the time course for fluvoxamine can be estimated from plasma pharmacokinetics and median effective dose (ED50) value, while this does not seem to be the case for either escitalopram or citalopram.
The pharmacokinetics of escitalopram and citalopram from our study, in terms of t max, C max, AUCss and t 1/2, are comparable to the ones available in the literature (Baumann and Larsen 1995; Larsen et al. 2001; Sogaard et al. 2005). Given the different accumulation of S-citalopram and R-citalopram due to the more rapid elimination of S-citalopram (Voirol et al. 1999), the R/S-citalopram ratios were higher at steady state than after administration of single doses (Klein et al. 2006).
In summary, a higher SERT occupancy in midbrain was found after multiple dose administration of 10 mg/day escitalopram compared to 20 mg/day citalopram despite similar plasma concentrations of the S-enantiomer. These results can also be explained by an attenuating effect of R-citalopram on the occupancy of S-citalopram at the serotonin transporter.
References
Backstrom I, Bergstrom M, Marcusson J (1989) High affinity [3H]paroxetine binding to serotonin uptake sites in human brain tissue. Brain Res 486:261–268
Bauer M, Whybrow PC, Angst J, Versiani M, Möller HJ, WFSBP Task Force on Treatment Guidelines for Unipolar Depressive Disorders (Allain H, Anderson I, Ayuso-Gutierrez JL, Baldwin D, Bech P, Benkert O, Berk M, Bitter I, Bourgeois ML, Burrows G, Cassano G, Cetkovich-Bakmas M, Cookson JC, da Costa D, Gheorghe MD, Heinze G, Higuchi T, Hirschfeld RM, Höschl C, Hoelsboer-Trachsler E, Kasper S, Katona C, Keller MB, Kulhara P, Kupfer DJ, Lecrubier Y, Leonard B, Licht RW, Lingjaerde O, Lublin H, Mendlewicz J, Mitchell P, Paykel ES, Puzynski S, Rush AJ, Rybakowski JK, Schweitzer I, Unützer J, Vestergaard P, Vieta E, Yamada K) (2002) World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for biological treatment of unipolar depressive disorders, part 1: acute and continuation treatment of major depressive disorder. World J Biol Psychiatry 3:5–43
Baumann P, Larsen F (1995) The pharmacokinetics of citalopram. Rev Contemp Pharmacother 6:287–295
Colonna L, Andersen HF, Reines EH (2005) A randomized, double-blind, 24-week study of escitalopram (10 mg/day) versus citalopram (20 mg/day) in primary care patients with major depressive disorder. Curr Med Res Opin 21(10):1659–1668, (Oct)
Gutierrez MM, Rosenberg J, Abramowitz W (2003) An evaluation of the potential for pharmacokinetic interaction between escitalopram and the cytochrome P450 3A4 inhibitor ritonavir. Clin Ther 25:1200–1210
Herold N, Uebelhack K, Franke L, Amthauer H, Luedemann L, Bruhn H, Felix R, Uebelhack R, Plotkin M (2006) Imaging of serotonin transporters and its blockade by citalopram in patients with major depression using a novel SPECT ligand [(123)I]-ADAM. J Neural Transm 113:659–670
Kasper S (2004) Unique mechanism of action for escitalopram: does it hold the promise? Int J Psychiatry Clin Pract 8:15–18
Kish SJ, Furukawa Y, Chang LJ, Tong J, Ginovart N, Wilson A, Houle S, Meyer JH (2005) Regional distribution of serotonin transporter protein in postmortem human brain: is the cerebellum a SERT-free brain region? Nucl Med Biol 32(2):123–128, 2005 (Feb)
Klein N, Sacher J, Geiss-Granadia T, Attarbaschi T, Mossaheb N, Lanzenberger R, Pötzi C, Holik A, Spindelegger C, Asenbaum S, Dudczak R, Tauscher J, Kasper S (2006) In vivo imaging of serotonin transporter occupancy by means of SPECT and [123I]ADAM in healthy subjects treated with different doses of escitalopram or citalopram. Psychopharmacology 3:263–272
Larsen F, Priskorn M, Overo KF (2001) Lack of citalopram effect on oral digoxin pharmacokinetics. J Clin Pharmacol 41:340–346
Lingjaerde O, Ahlfors UG, Bech P, Dencker SJ, Elgen K (1987) The UKU side effect rating scale. A new comprehensive rating scale for psychotropic drugs and a cross-sectional study of side effects in neuroleptic-treated patients. Acta Psychiatr Scand Suppl 334:1–100
Meyer JH, Wilson AA, Ginovart N, Goulding V, Hussey D, Hood K, Houle S (2001) Occupancy of serotonin transporters by paroxetine and citalopram during treatment of depression: a [(11)C]DASB PET imaging study. Am J Psychiatry 158:1843–1849
Meyer JH, Wilson AA, Sagrati S, Hussey D, Carella A, Potter WZ, Ginovart N, Spencer EP, Cheok A, Houle S (2004) Serotonin transporter occupancy of five selective serotonin reuptake inhibitors at different doses: an [11C]DASB positron emission tomography study. Am J Psychiatry 161:826–835
Moore N, Verdoux H, Fantino B (2005) Prospective, multicentre, randomized, double-blind study of the efficacy of escitalopram versus citalopram in outpatient treatment of major depressive disorder. Int Clin Psychopharmacol 20:131–137
Mork A, Kreilgaard M, Sanchez C (2003) The R-enantiomer of citalopram counteracts escitalopram-induced increase in extracellular 5-HT in the frontal cortex of freely moving rats. Neuropharmacology 45:167–173
Murdoch D, Keam SJ (2005) Escitalopram: a review of its use in the management of major depressive disorder. Drugs 65:2379–2404
Noble S, Benfield P (1997) Citalopram: a review of its pharmacology, clinical efficacy and tolerability in the treatment of depression. CNS Drugs 8:410–432
Oya S, Choi SR, Hou C, Mu M, Kung MP, Acton PD, Siciliano M, Kung HF (2000) 2-((2-((dimethylamino)methyl)phenyl)thio)-5-iodophenylamine (ADAM): an improved serotonin transporter ligand. Nucl Med Biol 27:249–254
Sacher J, Asenbaum S, Klein N, Geiss-Granadia T, Mossaheb N, Pötzi C, Attarbaschi T, Lanzenberger R, Dudczak R, Kasper S, Tauscher J (2006) [123I]ADAM: a novel SPECT ligand for quantification of serotonin transporters in humans. Int J Neuropsychopharmacology Feb. 17, 1--8 [Epub ahead of print]
Sanchez C, Boyeso KP, Ebert B, Reines EH, Braestrup C (2004) Escitalopram versus citalopram: the surprising rde of the R-enantiomer. Psychopharmacology 174(2):163--176
Sogaard B, Mengel H, Rao N, Larsen F (2005) The pharmacokinetics of escitalopram after oral and intravenous administration of single and multiple doses to healthy subjects. J Clin Pharmacol 45:1400–1406
Takano A, Suhara T, Ichimiya T, Yasuno F, Suzuki K (2006) Time course of in vivo 5-HTT transporter occupancy by fluvoxamine. J Clin Psychopharmacol 26:188–191
Tauscher J, Jones C, Remington G, Zipursky RB, Kapur S (2002a) Significant dissociation of brain and plasma kinetics with antipsychotics. Mol Psychiatry 7:317–321
Voirol P, Rubin C, Bryois C, Kosel M, Buclin T, Baumann P (1999) Pharmacokinetic consequences of a citalopram treatment discontinuation. Ther Drug Monit 21:263–266
Acknowledgement
This study was supported by an unrestricted grant from H. Lundbeck A/S and the “Bürgermeisterfonds der Stadt Wien” PNr: 2180/03.
Statement of interest
SK has received research grants, consultancy fees and lecture fees from a number of pharmaceutical companies in the area of CNS development including Lundbeck, the manufacturer of citalopram and escitalopram, and JT works now as an employee for Eli Lilly.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Klein, N., Sacher, J., Geiss-Granadia, T. et al. Higher serotonin transporter occupancy after multiple dose administration of escitalopram compared to citalopram: an [123I]ADAM SPECT study. Psychopharmacology 191, 333–339 (2007). https://doi.org/10.1007/s00213-006-0666-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-006-0666-y