Abstract
Intravesical mitomycin C (MMC) is commonly used to treat bladder cancer but is associated with local adverse effects. Here, we investigate the effects of MMC on release of urothelial mediators and production of inflammatory cytokines. Recovery and the effects of repeat treatment were also investigated. Urothelial cells were treated with MMC for 2 h at 37 °C. Immediately, 24 h and 7 days following MMC treatment, effects were assessed in terms of changes in ATP, acetylcholine and PGE2 release, and the presence of inflammatory cytokines and nitric oxide in incubation medium. Endpoints were also assessed 7 days after repeat MMC treatment. Immediately following MMC treatment at the clinical concentration (2 mg/mL), stretch-induced ATP release was significantly decreased, basal acetylcholine release was enhanced, while basal PGE2 was depressed and response to stretch increased. Twenty-four hours after treatment, basal acetylcholine was significantly increased ([MMC] ≥0.0002 mg/mL) and basal PGE2 enhanced (0.02 mg/mL). A 326-fold increase in interleukin-8 secretion and significant increase in nitric oxide release were also detected at 24 h. One week after single and repeat MMC treatment, urothelial ATP, acetylcholine and PGE2 had recovered while the increase in nitric oxide and interleukin-8 was still evident. These results indicate that urothelial mediator release is affected by MMC treatment with full recovery by 1 week. However, a concurrent increase in secretion of the inflammatory cytokine interleukin-8 and nitric oxide was also detected 24 h following treatment, which were still evident after the recovery period. These changes may play a role in the local adverse effects associated with intravesical MMC treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intravesical therapy which administers cytotoxic agents into the bladder lumen is an important approach for treatment of superficial bladder cancer. However, a high recurrence rate (48 to 70 %) and incidence of progression (7 to 40 %) of the disease is still reported (Logan et al. 2012). Intravesical administration delivers high concentrations of cytotoxic agents to the target cancer cells, with the added advantage of limited systemic exposure. Mitomycin C (MMC), doxorubicin and epirubicin are common agents used for the treatment of superficial bladder cancer via this targeted means of delivery. Despite limited systemic side effects, there is evidence of significant local adverse effects such as chemical cystitis (dysuria, increased urinary frequency and urgency) following this treatment (Dalton et al. 1991; Elmamoun et al. 2014; Koya et al. 2006; Thrasher and Crawford 1992). It has been shown that intravesical MMC treatment causes chemical cystitis in 41 % of patients, with dysuria, increased urgency and frequency, suprapubic pain and discomfort reported (Kamat and Lamm 2000; Pouya et al. 1996). In addition, decreased bladder volume and contracted bladder are associated with this treatment (Duque and Loughlin 2000).
The urothelium which lines the luminal surface of the bladder is in close proximity with the cytotoxic agents during intravesical treatment. The urothelium was originally thought to act as a simple distensible barrier protecting the underlying nerves, muscular and vascular tissues from the potentially harmful contents of the urine. However, recent studies have shown that the urothelium can release a number of chemical mediators and transmitters including ATP (Burnstock 2011), acetylcholine (Birder 2010; Hanna-Mitchell et al. 2007), prostaglandin E2 (Aizawa et al. 2010; Apodaca et al. 2007; Birder 2005; Tanaka et al. 2011) and nitric oxide (Birder et al. 1998) in response to chemical and mechanical stimuli during bladder filling to communicate with underlying tissues, and regulate sensory mechanisms and bladder contraction (Birder et al. 2010; Cockayne et al. 2000; Maggi et al. 1988). Despite the urothelium acting as an effective barrier to the movement of substances from the bladder lumen to the deeper tissue layers, there is evidence that some intravesical chemotherapeutic agents diffuse into the detrusor muscle including MMC and doxorubicin, albeit only at a fraction of the luminal concentration (Wientjes et al. 1991, 1993).
We recently reported that doxorubicin, at clinically relevant concentrations and durations of treatments, alters release of ATP, Ach and PGE2 from urothelial cells (Kang et al. 2013). Twenty-four hours following treatment, urothelial mediator release was still affected and induction of pro-inflammatory cytokines (interleukin (IL)-8 and IL-1β) was observed.
Generally, intravesical treatments are received at weekly intervals. To our knowledge, recovery of urothelial function over longer periods such as this has not been assessed to date. The aim of this study was to investigate the effects of MMC on basal and stretch-induced release of urothelial mediators (acetylcholine, ATP, prostaglandin E2) from human urothelial cells and determine whether changes in urothelial function may provide an explanation for the urological adverse effects experienced by patients treated with intravesical MMC. The release of inflammatory cytokines and nitric oxide from urothelial cells after MMC treatment was also assessed to determine if inflammation may play a role in the adverse effects associated with treatment. In addition, recovery of urothelial function was assessed 1 week post-treatment and repeat treatments conducted.
Materials and methods
Cell culture
Human urothelial cells (RT4) were obtained from the European Collection of Cell Cultures. Cells were grown and maintained at 37 °C with 5 % CO2 in McCoy’s 5 A culture medium (Invitrogen, Victoria, Australia) containing L-glutamine, phenol red, 10 % faetal bovine serum (Invitrogen, Victoria, Australia) and 500 U/mL penicillin-streptomycin (Invitrogen, Victoria, Australia). Cell viability was assessed by typan blue exclusion.
Mitomycin C treatment of urothelial cells
Twenty-four-well plates were seeded at a density of 0.3 × 106 (for immediate effects), 0.15 × 106 (for 24 h post-treatment effects) or 0.1 × 106 (for 1 week post-treatment effects) cells per well and incubated overnight to allow cells to adhere. Cells were treated with MMC (Cayman Chemical, Michigan, USA) at concentrations up to 2 mg/mL diluted in McCoy’s 5A culture medium, which is the clinical dose used for intravesical therapy. The plate was then incubated for 2 h at 37 °C. Cells were then used immediately, 24 h or 1 week later to generate samples for analysis of urothelial mediator release.
Urothelial cells were treated with lower concentrations of MMC for 24 h and 1 week post-treatment experiments as a previous study showed that the concentration of MMC that reaches the urothelial cells is approximately 3 % of intravesical concentration (Wientjes et al. 1993). They also report that the amount of MMC penetrating normal bladder tissue is lower than the levels penetrating the superficial tumours of the bladder. In addition, often the dose used clinically is half of that used here (Colombo et al. 2012). Therefore, these lower concentrations are more likely to reflect the concentration reached in urothelial cells in vivo. In addition, higher concentrations of MMC left cell viability too low to allow for measurement of urothelial mediator release as would be expected with such a high concentration. Since cultured urothelial cells are actively proliferating unlike urothelial cells in situ, they are likely to be more vulnerable to the cell death mechanisms of chemotherapeutic agents such as MMC that tend to be more specific for proliferating cells. Hence, it is more appropriate to assess the drug at concentrations that have little effect on cell viability.
Repeat MMC treatment of urothelial cells
One week after MMC treatment (0.002 mg/mL), a second treatment with the same concentration was performed for 2 h at 37 °C. Following MMC treatment, cells were washed with PBS and incubated with fresh drug-free culture medium for 1 week. Cells were used 1 week after the second MMC treatment to generate samples for analysis of urothelial mediator release.
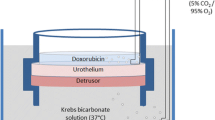
Mediator release from urothelial cells
Following the incubation, medium was aspirated and cells were washed with PBS prior to adding Krebs bicarbonate solution (118.4 mmol/L NaCl, 24.9 mmol NaHCO3, 4.7 mmol KCl, 1.9 mmol CaCl2, 1.15 mmol MgSO4, 1.15 mmol KH2PO4 and 11.7 mmol glucose; 280 mOsm/L) to each well. After 15 min, the solutions in each well were collected for measurement of basal mediator release from MMC- and vehicle-treated control cells. For stretch-induced release of urothelial mediators, hypotonic Krebs bicarbonate solution (50 % of normal NaCl content; 180 mOsm/L) was added to each well. After 15 min, solutions in each well were collected for analysis of stimulated release of urothelial mediators. The use of hypotonic Krebs solution causes the cells to swell, mimicking the stretch that occurs during bladder filling (Kang et al. 2013; McDermott et al. 2012).
Luciferin/luciferase assay
ATP was measured using an ATP determination kit (Molecular Probes) and the assay was carried out according to the manufacturer’s instructions. A standard curve using known concentrations of ATP was constructed and used to calculate ATP concentration in samples. Luminescence was measured using a Modulus microplate reader (Promega). ATP concentrations measured were normalized to controls using corresponding resazurin reduction data.
Acetylcholine assay
Acetylcholine was measured using Amplex® Red Acetylcholine Assay kit (Molecular Probes). The assay was performed according to the manufacturer’s protocol. Acetylcholine concentration in samples was calculated using standard curves constructed from known acetylcholine standards. Fluorescence was measured on a Modulus Microplate reader (Ex. 540/Em. 590 nm). Acetylcholine concentrations measured were normalized to controls using corresponding resazurin reduction data.
Prostaglandin E2 assay
The level of prostaglandin E2 released from RT4 cells was measured using Prostaglandin E2 EIA (Cayman Chemicals). Samples and standards were analyzed using a Modulus microplate reader (420 nm). The assay was performed according to manufacturer’s protocol. Prostaglandin E2 concentrations measured were normalized to controls using corresponding resazurin reduction data.
Resazurin viability assay
Reduction of the redox dye resazurin to resorufin was used to measure the viability of cells. Cells were seeded in 96-well microtitre plates 24 h prior to the addition of MMC (0–2 mg/mL) for 2 h at 37 °C. Treatment medium was removed and replaced with fresh culture medium and cultures maintained at 37 °C for 24 h or 7 days. Following 24 h or 7 days, incubation medium above the cells was removed and replaced with fresh medium containing 44 μM resazurin. After 2 h incubation, reduction of resazurin to resorufin was determined by fluorescence (exCitation 530 nm; emission 590 nm) using a Modulus microplate reader. Appropriate cell-free controls were also included. Under all conditions tested, the extent of resazurin reduction was directly proportional to viable cell counts (data not shown). No change in cell number was observed immediately after 2 h MMC treatment. Viability was also assessed 7 days after repeat MMC treatment.
Inflammatory cytokine analysis
Cell-free incubation medium was collected from T25 culture flasks 24 h and 1 week after the first MMC pretreatment and also 1 week after the second MMC pretreatment. The presence of inflammatory cytokines (interleukin-8, interleukin-1β, interleukin-6, interleukin-10, interleukin-12p70 and tumour necrosis factor) was analysed using a BD™ Cytometric Bead Array Human Inflammatory Cytokines Kit according to the manufacturer’s instructions. Standard and sample fluorescence were analysed on a BD™ FACS Calibur flow cytometer. Concentrations of inflammatory cytokines measured were normalized to controls using corresponding resazurin reduction data.
Nitrate/nitrite analysis
Cell-free incubation medium was collected from T25 culture flasks 24 h and 1 week after the first 2 h MMC pretreatment and also 1 week after the second MMC pretreatment. Release of urothelial nitric oxide into the incubation medium was assessed by measuring its metabolites nitrate and nitrite using a Nitrate/Nitrite Fluorometric Assay Kit (Cayman Chemicals). The assay was conducted according to manufacturer’s instructions. Nitrate/nitrite concentration in samples was calculated using standard curves constructed from known standards. Fluorescence was measured on a Modulus Microplate reader. Nitrate/nitrite concentrations measured were normalized to controls using corresponding resazurin reduction data.
Statistical analysis
Results are expressed as mean ± standard deviation (S.D.). Data were analysed using a paired Student’s t test or one-way ANOVA with Dunnett multiple comparisons test, using Graphpad InStat3 software (San Diego, CA). Significance levels were defined as P < 0.05 (*), P < 0.01 (**) and P < 0.001 (***).
Results
Immediate effects of MMC on urothelial mediator release
Immediately following treatment, no significant change was observed in basal release of ATP from human urothelial cells at all concentrations of MMC tested (Fig. 1a). Stimulated release of ATP was observed in vehicle-treated control urothelial cells and cells treated with MMC (0.0002–0.2 mg/mL), with significant increase above basal levels of ATP release in response to hypotonic stimulation; except at 2 mg/mL where stimulated release of ATP was completely abolished (95 % decrease) (Fig. 1b).
Immediate effects of 2 h mitomycin C (MMC) treatment on basal extracellular a ATP, c acetylcholine and e prostaglandin E2 concentrations, and b ATP, d acetylcholine and f prostaglandin E2 response to hypo-osmotic stimulation. Data expressed as means ± S.D. of at least four determinations. (*P < 0.05 comparing MMC treated vs. vehicle control)
Immediately following MMC treatment, while basal release of acetylcholine from urothelial cells exposed to 2 mg/mL was significantly increased (2-fold) compared to vehicle-treated control cells, stimulated release of acetylcholine was not significantly affected by MMC in comparison to control (Fig. 1c, d).
Basal release of prostaglandin E2 from cells treated with 2 mg/mL of MMC was significantly decreased (7-fold) immediately following 2 h drug exposure compared to control (Fig. 1e). A significant decrease in release of prostaglandin E2 in response to hypotonic stimulation was observed in cells treated with MMC (0.0002–0.2 mg/mL) (Fig. 1f). In contrast, there was a significant increase in stimulated release of prostaglandin E2 from cells treated with 2 mg/mL of MMC.
Effects of MMC on urothelial cell viability and mediator release 24 h post-treatment
Twenty-four hours following MMC pretreatment, a concentration-dependent decrease in urothelial cell viability was observed, with significant changes detected in cells treated with MMC ≥0.0002 mg/mL (Fig. 2a).
Since urothelial mediator release is affected immediately after MMC treatment, the ability of the urothelium to recover was assessed. Release of urothelial mediators was measured 24 h after MMC pretreatment with lower MMC concentrations, as these are more likely to reflect the concentration reached in urothelial cells in vivo, which has been estimated to be 3 % of intravesical concentration (Wientjes et al. 1993). Both basal and stimulated release of ATP from MMC pretreated urothelial cells remained unchanged compared to vehicle-treated controls 24 h following treatment (Fig. 3a, b). In contrast, 24 h after MMC treatment, concentration-dependent increase in basal acetylcholine release was observed with significant increases at both 0.0002 and 0.02 mg/mL (Fig. 3c) but stimulated acetylcholine remained unchanged compared to controls (Fig. 3d). In addition, basal release of PGE2 was significantly increased in urothelial cells pretreated with 0.02 mg/mL MMC compared to control cells (Fig. 3e) and PGE2 response to stretch was not observed in both controls and MMC pretreated cells 24 h following treatment with basal release being significantly higher than stimulated release at 0.02 mg/mL MMC (Fig. 3f).
Twenty-four hour post-treatment effects of mitomycin C (MMC) on basal extracellular a ATP, c acetylcholine, e prostaglandin E2 concentrations, and b ATP, d acetylcholine and f prostaglandin E2 response to hypo-osmotic stimulation. Data are expressed as means ± S.D. of at least four determinations. (**P < 0.01 or ***P < 0.001 comparing MMC-treated vs. vehicle control)
Effects of single and repeat MMC treatment on urothelial cell viability and mediator release at 1 week
One week following MMC pretreatment, urothelial cell viability was not affected in cells treated with MMC ≤0.02 mg/mL; however, complete cell death was observed in cells treated with 0.2 and 2 mg/mL MMC (Fig. 2b). No significant changes in ATP, Ach or PGE2 release were observed 1-week post-treatment with MMC (0.002 mg/mL) (data not shown).
To assess the long-term (1 week) and repeat treatment effects of MMC, urothelial mediator release from cells treated with 0.002 mg/mL MMC was assessed. This treatment concentration was selected to ensure adequate viable cell numbers for endpoint experiments. Urothelial cell viability was reduced to 86.64 ± 5.7 % 1 week after repeat MMC treatment with 0.002 mg/mL. Again, no significant change in ATP, Ach or PGE2 release was observed 1 week after repeat MMC treatment (0.002 mg/mL) (data not shown).
Effects of MMC on inflammatory cytokine and nitric oxide release
The presence of inflammatory cytokines (interleukin-8, interleukin-1β, interleukin-6, interleukin-10, interleukin-12p70 and tumour necrosis factor) in urothelial cell incubation medium was tested 24 h and 1 week after the first MMC treatment and also 1 week after the second MMC treatment as a measure of urothelial inflammation. Interleukin-8 was secreted by untreated urothelial cells at 24 h, while urothelial cells treated with MMC (0.02 mg/mL) showed a 326-fold increase in release (25.52 ± 2.53 pg/mL control vs. 8321 ± 654 pg/mL treated, P < 0.01) (Fig. 4a). Interleukin-1β, interleukin-6, interleukin-10, interleukin-12p70 and tumour necrosis factor were not detected in control or treated samples at any timepoint tested. Increased interleukin-8 secretion was also detected 1 week after the first (13-fold increase from) and repeat (7-fold increase compared to) MMC treatment (Fig. 4b, c).
Metabolites of nitric oxide (nitrate and nitrite) were measured in incubation medium to determine the effects of MMC on urothelial nitric oxide release. Nitric oxide was released by untreated urothelial cells at 24 h, with a significant increase observed from cells treated with MMC (0.02 mg/mL) (Fig. 5a). A significant increase in urothelial release of nitric oxide was also evident 1 week after the first MMC treatment (Fig. 5b), but 1 week after the second MMC treatment no significant differences could be detected compared to control (data not shown).
Discussion
Intravesical MMC is commonly used for the treatment of superficial bladder cancer. While systemic exposure is limited by this targeted means of delivery, local adverse effects are often reported. As the urothelium is in close contact with high concentrations of cytotoxic agents during intravesical chemotherapy, it is probable that the local adverse effects associated with cancer treatment including MMC may be due to changes in the release of urothelial mediators. We previously reported that doxorubicin treatment results in alterations in the release of urothelial mediators (ATP, acetylcholine and prostaglandin E2) immediately and 24 h following treatment (Kang et al. 2013). In addition, there are strong links between development of bladder symptoms and inflammation in other conditions (Nomiya et al. 2012; Yoshimura et al. 2002) and the cytotoxic agent doxorubicin has been shown to increase urothelial secretion of interleukin-8 and interleukin-1β (Kang et al. 2013). Thus, the present study investigated the effects of the commonly used intravesical chemotherapeutic agent MMC on urothelial function, markers of inflammation and the ability to recover following single and repeat treatments. The results of our study suggest that the pain and bladder dysfunction experienced by patients following intravesical MMC may be due to induction of inflammatory cytokines and enhanced nitric oxide (NO) release, which persist through the recovery period and also following repeat treatment.
The in vitro urothelial culture model used in this study has been used previously to assess urothelial mediator release by our group and others (McDermott et al. 2012; Kang et al. 2013; Mansfield and Hughes 2014a, b). In vivo models are complicated by the presence of structural heterogeneity and do not allow for toxic mechanisms to be clearly defined. Using cultured urothelial cells allowed us to investigate the effects of MMC at cellular level and aids in identification of urothelial specific effects. The complexity of bladder tissue is such that multiple cell types in the bladder wall release the mediators of interest in this study (Cheng et al. 2011). Given that our aim was to assess the effects of MMC on urothelial function, interpretation of changes in mediator release from intact tissue is complicated by multiple sources of release. A major limitation of animal studies is difficulty with interpretation based on species differences. Therefore, a significant advantage of the urothelial model used here is that it is of human origin and has been shown to release ATP, Ach and PGE2 under basal and stretch conditions as in the intact bladder. We must however be mindful of the limitations of cell culture models when interpreting results and making conclusions that relate to the clinical setting due to possible changes to functional characteristics in cultured cells and the complexity of the whole organism. Future pharmacological and physiological studies are therefore necessary to confirm if our conclusions regarding the role inflammation are valid.
It is well established that as the bladder stretches during filling, ATP is released from the urothelium to act on purinoreceptors (P2X2/3) present on urothelial and suburothelial (lamina propria) sensory Aδ and small diameter C fibers, stimulating the afferent arm of the micturition reflex and giving rise to the perception of pain, respectively (Burnstock 2011; Cockayne et al. 2000; Kumar et al. 2007, 2010; Souslova et al. 2000). Intravesical MMC treatment causes urological adverse effects such as painful urination and urgency. Enhanced release of ATP has been reported in a number of disorders of the bladder such as idiopathic and neurogenic bladder overactivity (OAB) (Kumar et al. 2010). ATP is also greatly enhanced from the urothelium of patients with painful bladder syndrome (PBS) (Kumar et al. 2007). Therefore, in this study, enhanced release of ATP from the urothelial cells was expected by MMC treatment. Surprisingly, MMC had an inhibitory effect on stimulated release of ATP at the clinical concentration (2 mg/mL) immediately after treatment. Similarly, doxorubicin has inhibitory effects of urothelial ATP release (Kang et al. 2013). The urological side effects experienced by patients following intravesical MMC treatment cannot be explained by inhibition in stimulated ATP release reported here. The discrepancy may be addressed by various factors. One is that the pain induced by MMC treatment may be due to increased sensitivity of afferent C fibers rather than the increase in ATP release that is observed in other bladder disorders mentioned previously. Decreased ATP release reported here may not directly take part in causing urinary symptoms but may impact on the release of other urothelial mediators, potentially leading to abnormal communication between the urothelium and underlying layers such as myofibroblasts, nerves and detrusor muscle. Another possibility is that there may be enhanced release of ATP from other cells in the bladder wall resulting in symptoms of pain. Both interstitial cells and smooth muscle cells from the bladder have been shown to release ATP during stretch (Cheng et al. 2011).
The discovery of muscarinic and nicotinic receptors on the urothelium has attracted further interest in the role of acetylcholine in bladder function as a chemical mediator of neural-urothelial interactions (Birder 2010). Muscarinic receptors are primarily known for their role in voiding but there is evidence showing that the urothelium expresses the full complement of muscarinic receptors (M1–M5) as well as the enzymes necessary for the synthesis, release and metabolism of acetylcholine (Birder 2010; Hanna-Mitchell et al. 2007; Kullmann et al. 2008). Studies have shown that acetylcholine is released from the urothelium in response to stretch (mechanical stimulation) as well as chemical stimulation (Birder 2010). The role of acetylcholine in the urothelium is still being identified but it has been suggested that once released, urothelial-derived acetylcholine may act in a paracrine manner to stimulate the detrusor muscle and nerves, or in an autocrine manner to stimulate urothelial-associated muscarinic receptors (Birder 2010; Hanna-Mitchell et al. 2007). Also, a study by Kanai et al. (2007) which applied muscarinic receptor agonist to strips of rat bladder tissue induced membrane-potential transients and Ca2+ transients that begin near the urothelial-suburothelial interface and then spread to the detrusor smooth muscle, raising the possibility that the urothelium could regulate the generation of spontaneous, non-voiding contraction in the bladder. Hence, increased release of basal acetylcholine from the urothelial cells immediately and 24 h following MMC treatment may activate cholinergic transmission in the bladder, possibly leading to the bladder overactivity observed in patients treated with intravesical MMC.
The action of the urothelial-derived PGE2 in the bladder are not well understood yet but it has been reported to stimulate spontaneous bladder contractions (de Jongh et al. 2007), stimulate release of ATP from urothelial cells (Tanaka et al. 2011) and sensitize bladder capsaicin-sensitive afferent neurons (Maggi et al. 1988) which may play important roles in modulation of nerve and detrusor functions (Apodaca et al. 2007; Birder 2005). A study using mice has demonstrated that overexpression of PGE2 in the bladder stimulates the micturition reflex through activation of C-fibres (Aoki et al. 2009; Maggi et al. 1988). In addition, inhibition of cyclooxygenase improved storage function in rats with detrusor overactivity, indicating potential stimulatory effects of PGE2 on bladder micturition reflex (Yokoyama 2010). In this study, MMC had an inhibitory effect on basal release of PGE2 immediately following treatment with the clinical dose. This may be due to changes in ATP release that were observed immediately after treatment as these two mediators are reported to be co-related (Tanaka et al. 2011). In contrast, 24 h following treatment with a 100-fold lower MMC concentration, an excitatory effect of MMC on basal release of PGE2 was observed. Doxorubicin has also been shown to increase basal but also stimulated release of PGE2 from urothelial cells (Kang et al. 2013). An increase in PGE2 release by MMC may lead to a sensitization of the micturition reflex, possibly causing increased urinary frequency as well as perception of pain which are side effects commonly experienced by patients treated with MMC. Therefore, while less ATP release was observed here following MMC treatment, sensitization of nerves due to the enhanced PGE2 release reported would mean that less ATP is required to stimulate sensory activity.
Release of inflammatory mediators is associated with intravesical Bacillus Calmette-Guerin (BCG) treatment (de Boer et al. 1997) and has also been linked to chemotherapeutic agents such as doxorubicin (Abou El Hassan et al. 2003). Previous studies have also shown that MMC induces release of IL-8 in human fibroblasts (Chou et al. 2007). We have also recently reported that the chemotherapeutic agent doxorubicin induces release of IL-8 and IL-1β from treated urothelial cells (Kang et al. 2013). Here, we assessed the effects on MMC on release of a number of human inflammatory cytokines from urothelial cells but only IL-8 was detected, with a 326-fold increase 24 h after treatment. IL-8 was still elevated 1 week after treatment and again following repeat MMC treatment, while release of normal urothelial mediators had recovered. Inflammation has been shown to increase bladder afferent excitability and is believed to contribute to bladder overactivity and pain (Hayashi et al. 2009; Wyndaele and De Wachter 2003). Cytokines are thought to alter cell-cell communication by affecting gap-junctions in bladder smooth muscle and suburothelial myofibroblasts, in addition to altering voltage-gated K+ channel expression in bladder afferents (Hayashi et al. 2009; Heinrich et al. 2011). Our data suggests that sustained release of inflammatory cytokines rather than changes in urothelial mediator release may be important in the development of the bladder overactivity and pain experienced by patients following intravesical treatment.
Nitric oxide plays a major role in the bladder outlet region during micturition, inducing relaxation and preventing large increases in pressure during bladder contraction (Bustamante et al. 2010). Along with acetylcholine, NO is released as a co-transmitter from parasympathetic nerves and exerts an inhibitory effect on contraction (Dokita et al. 1991). Recently, the urothelium has been shown to be an alternative source of NO in the bladder; endothelial NO synthase (eNOS) has been identified in umbrella cells of the rat urothelium and stretch or muscarinic receptor stimulation has been shown to release NO from these cells in culture (Birder et al. 1998; Giglio et al. 2005). The function of urothelial NO is uncertain, but indirect evidence suggests a role in modulating sensory nerve activity (Birder et al. 1998) and nitric oxide donors have recently been shown to inhibit afferent nerve activity (Aizawa et al. 2011). NO donors have been shown to inhibit urothelial contraction and inhibit pacemaker activity (Moro et al. 2012). There is also some evidence to suggest that NO can exert excitatory effects: in isolated mouse bladder, it has been shown that NO can increase phasic contractile activity (Gillespie and Drake 2004), and in precontracted human detrusor strips, both relaxation and contraction responses to NO donors have been observed (Moon 2002). Elevated levels of NO have been reported with inflammatory disease of the bladder including bacterial cystitis, interstitial cystitis and after BCG treatment for bladder cancer, and are thought to play a role in inflammation progression (Ehren et al. 1999; Logadottir et al. 2004; Lundberg et al. 1996). iNOS expression was shown to be localized in the urothelium of bladder cancer patients following BCG treatment (Koskela et al. 2012), while increased NOS expression and enhanced NO release from the bladder mucosa are also associated with cyclophosphamide-induced cystitis (Andersson et al. 2008). A recent study reported that inhibition of NOS prevents muscarinic and purinergic dysfunction and development of cyclophosphamide-induced cystitis in the rat (Aronsson et al. 2014). Elevated bladder wall nitric oxide production has been reported in patients with interstitial cystitis, with a concurrent increase in IL-6, IL-10 and IL-17A mRNA (Logadottir et al. 2014). Here, we show an increase in NO release from urothelial cells 24 h following MMC treatment which persists 7 days following single and repeat treatment. This may contribute to the pain and alterations in bladder function experienced in patients following intravesical MMC treatment.
The efficacy of intravesical agents is generally well described; however, their safety profiles receive less attention. While systemic side effects are rare, local adverse effects are frequently reported. Here, we show that MMC treatment alters urothelial release of ATP, PGE2 and Ach initially, but that release of these mediators returns to normal following a period of recovery. The results of our study therefore suggest that the pain and bladder dysfunction experienced by patients following intravesical MMC may be due to induction of inflammatory cytokines and enhanced NO release, which persist through the recovery period and also following repeat treatment.
References
Abou El Hassan MA, Verheul HM, Jorna AS, Schalkwijk C, van Bezu J, van der Vijgh WJ, Bast A (2003) The new cardioprotector monohydroxyethylrutoside protects against doxorubicin-induced inflammatory effects in vitro. Br J Cancer 89:357–362. doi:10.1038/sj.bjc.6601022
Aizawa N, Igawa Y, Nishizawa O, Wyndaele JJ (2010) Effects of CL316,243, a beta 3-adrenoceptor agonist, and intravesical prostaglandin E2 on the primary bladder afferent activity of the rat. Neurourol Urodyn 29:771–776. doi:10.1002/nau.20826
Aizawa N, Igawa Y, Nishizawa O, Wyndaele JJ (2011) Effects of nitric oxide on the primary bladder afferent activities of the rat with and without intravesical acrolein treatment. Eur Urol 59:264–271. doi:10.1016/j.eururo.2010.10.035
Andersson MC, Tobin G, Giglio D (2008) Cholinergic nitric oxide release from the urinary bladder mucosa in cyclophosphamide-induced cystitis of the anaesthetized rat. Br J Pharmacol 153:1438–1444. doi:10.1038/bjp.2008.6
Aoki K, Hirayama A, Tanaka N, Yoneda T, Yoshida K, Fujimoto K, Hirao Y (2009) A higher level of prostaglandin E2 in the urinary bladder in young boys and boys with lower urinary tract obstruction. Biomed Res 30:343–347
Apodaca G, Balestreire E, Birder LA (2007) The uroepithelial-associated sensory web. Kidney Int 72:1057–1064. doi:10.1038/sj.ki.5002439
Aronsson P, Vesela R, Johnsson M, Tayem Y, Wsol V, Winder M, Tobin G (2014) Inhibition of nitric oxide synthase prevents muscarinic and purinergic functional changes and development of cyclophosphamide-induced cystitis in the rat. BioMed Res Int 2014:359179. doi:10.1155/2014/359179
Birder LA (2005) More than just a barrier: urothelium as a drug target for urinary bladder pain. Am J Physiol Ren Physiol 289:F489–F495. doi:10.1152/ajprenal.00467.2004
Birder LA (2010) Urothelial signaling. Auton Neurosci 153:33–40. doi:10.1016/j.autneu.2009.07.005
Birder LA, Apodaca G, De Groat WC, Kanai AJ (1998) Adrenergic- and capsaicin-evoked nitric oxide release from urothelium and afferent nerves in urinary bladder. Am J Physiol 275:F226–F229
Birder LA, Kanai AJ, Cruz F, Moore K, Fry CH (2010) Is the urothelium intelligent? Neurourol Urodyn 29:598–602. doi:10.1002/nau.20914
Burnstock G (2011) Therapeutic potential of purinergic signalling for diseases of the urinary tract. BJU Int 107:192–204. doi:10.1111/j.1464-410X.2010.09926.x
Bustamante S, Orensanz LM, Recio P, Carballido J, Garcia-Sacristan A, Prieto D, Hernandez M (2010) Functional evidence of nitrergic neurotransmission in the human urinary bladder neck. Neurosci Lett 477:91–94. doi:10.1016/j.neulet.2010.04.040
Cheng Y, Mansfield KJ, Sandow SL, Sadananda P, Burcher E, Moore KH (2011) Porcine bladder urothelial, myofibroblast, and detrusor muscle cells: characterization and ATP release. Front Pharmacol 2:27. doi:10.3389/fphar.2011.00027
Chou SF, Chang SW, Chuang JL (2007) Mitomycin C upregulates IL-8 and MCP-1 chemokine expression via mitogen-activated protein kinases in corneal fibroblasts. Invest Ophth Vis Sci 48:2009–2016. doi:10.1167/Iovs.06-0835
Cockayne DA et al (2000) Urinary bladder hyporeflexia and reduced pain-related behaviour in P2X3-deficient mice. Nature 407:1011–1015. doi:10.1038/35039519
Colombo R, Rocchini L, Suardi N, Benigni F, Colciago G, Bettiga A, Pellucchi F, Maccagnano C, Briganti A, Salonia A, Rigatti P, Montorsi F (2012) Neoadjuvant short-term intensive intravesical mitomycin C regimen compared with weekly schedule for low-grade recurrent non-muscle-invasive bladder cancer: preliminary results of a randomised phase 2 study. Eur Urol 62:797–802. doi:10.1016/j.eururo.2012.05.032
Dalton JT, Wientjes MG, Badalament RA, Drago JR, Au JL (1991) Pharmacokinetics of intravesical mitomycin C in superficial bladder cancer patients. Cancer Res 51:5144–5152
de Boer EC, Somogyi L, de Ruiter GJ, de Reijke TM, Kurth KH, Schamhart DH (1997) Role of interleukin-8 in onset of the immune response in intravesical BCG therapy for superficial bladder cancer. Urol Res 25:31–34
de Jongh R, van Koeveringe GA, van Kerrebroeck PE, Markerink-van Ittersum M, de Vente J, Gillespie JI (2007) The effects of exogenous prostaglandins and the identification of constitutive cyclooxygenase I and II immunoreactivity in the normal guinea pig bladder. BJU Int 100:419–429. doi:10.1111/j.1464-410X.2007.07011.x
Dokita S, Morgan WR, Wheeler MA, Yoshida M, Latifpour J, Weiss RM (1991) NG-nitro-L-arginine inhibits non-adrenergic, non-cholinergic relaxation in rabbit urethral smooth muscle. Life Sci 48:2429–2436
Duque JL, Loughlin KR (2000) An overview of the treatment of superficial bladder cancer. Intravesical chemotherapy. Urol Clin N Am 27:125–135
Ehren I, Hosseini A, Herulf M, Lundberg JO, Wiklund NP (1999) Measurement of luminal nitric oxide in bladder inflammation using a silicon balloon catheter: a novel minimally invasive method. Urology 54:264–267
Elmamoun MH, Christmas TJ, Woodhouse CR (2014) Destruction of the bladder by single dose mitomycin C for low-stage transitional cell carcinoma (TCC)—avoidance, recognition, management and consent. BJU Int 113:E34–E38. doi:10.1111/bju.12340
Giglio D, Ryberg AT, To K, Delbro DS, Tobin G (2005) Altered muscarinic receptor subtype expression and functional responses in cyclophosphamide induced cystitis in rats. Auton Neurosci 122:9–20. doi:10.1016/j.autneu.2005.07.005
Gillespie JI, Drake MJ (2004) The actions of sodium nitroprusside and the phosphodiesterase inhibitor dipyridamole on phasic activity in the isolated guinea-pig bladder. BJU Int 93:851–858. doi:10.1111/j.1464-410X.2003.04727.x
Hanna-Mitchell AT, Beckel JM, Barbadora S, Kanai AJ, de Groat WC, Birder LA (2007) Non-neuronal acetylcholine and urinary bladder urothelium. Life Sci 80:2298–2302. doi:10.1016/j.lfs.2007.02.010
Hayashi Y et al (2009) Bladder hyperactivity and increased excitability of bladder afferent neurons associated with reduced expression of Kv1.4 alpha-subunit in rats with cystitis. Am J Physiol Regul Int Comp Physiol 296:R1661–R1670. doi:10.1152/ajpregu.91054.2008
Heinrich M, Oberbach A, Schlichting N, Stolzenburg JU, Neuhaus J (2011) Cytokine effects on gap junction communication and connexin expression in human bladder smooth muscle cells and suburothelial myofibroblasts. PLoS One 6:e20792. doi:10.1371/journal.pone.0020792
Kamat AM, Lamm DL (2000) Intravesical therapy for bladder cancer. Urology 55:161–168
Kanai A et al (2007) Origin of spontaneous activity in neonatal and adult rat bladders and its enhancement by stretch and muscarinic agonists. Am J Physiol Ren Physiol 292:F1065–F1072. doi:10.1152/ajprenal.00229.2006
Kang SH, Chess-Williams R, Anoopkumar-Dukie S, McDermott C (2013) Induction of inflammatory cytokines and alteration of urothelial ATP, acetylcholine and prostaglandin E2 release by doxorubicin. Eur J Pharmacol 700:102–109. doi:10.1016/j.ejphar.2012.11.053
Koskela LR, Poljakovic M, Ehren I, Wiklund NP, de Verdier PJ (2012) Localization and expression of inducible nitric oxide synthase in patients after BCG treatment for bladder cancer. Nitric Oxide Biol Chem Off J Nitric Oxide Soc 27:185–191. doi:10.1016/j.niox.2012.07.001
Koya MP, Simon MA, Soloway MS (2006) Complications of intravesical therapy for urothelial cancer of the bladder. J Urol 175:2004–2010. doi:10.1016/S0022-5347(06)00264-3
Kullmann FA, Artim D, Beckel J, Barrick S, de Groat WC, Birder LA (2008) Heterogeneity of muscarinic receptor-mediated Ca2+ responses in cultured urothelial cells from rat. Am J Physiol Ren Physiol 294:F971–F981. doi:10.1152/ajprenal.00313.2007
Kumar V, Chapple CR, Rosario D, Tophill PR, Chess-Williams R (2010) In vitro release of adenosine triphosphate from the urothelium of human bladders with detrusor overactivity, both neurogenic and idiopathic. Eur Urol 57:1087–1092. doi:10.1016/j.eururo.2009.11.042
Kumar V, Chapple CR, Surprenant AM, Chess-Williams R (2007) Enhanced adenosine triphosphate release from the urothelium of patients with painful bladder syndrome: a possible pathophysiological explanation. J Urol 178:1533–1536. doi:10.1016/j.juro.2007.05.116
Logadottir Y, Delbro D, Fall M, Gjertsson I, Jirholt P, Lindholm C, Peeker R (2014) Cytokine expression in patients with bladder pain syndrome/interstitial cystitis ESSIC type 3C. J Urol 192:1564–1568. doi:10.1016/j.juro.2014.04.099
Logadottir YR, Ehren I, Fall M, Wiklund NP, Peeker R, Hanno PM (2004) Intravesical nitric oxide production discriminates between classic and nonulcer interstitial cystitis. J Urol 171:1148–1150. doi:10.1097/01.ju.0000110501.96416.40, discussion 1150-1141
Logan C, Brown M, Hayne D (2012) Intravesical therapies for bladder cancer—indications and limitations. BJU Int 110(Suppl 4):12–21. doi:10.1111/j.1464-410X.2012.11619.x
Lundberg JO et al (1996) Elevated nitric oxide in the urinary bladder in infectious and noninfectious cystitis. Urology 48:700–702. doi:10.1016/S0090-4295(96)00423-2
Maggi CA et al (1988) Prostanoids modulate reflex micturition by acting through capsaicin-sensitive afferents. Eur J Pharmacol 145:105–112
Mansfield KJ, Hughes JR (2014a) Effect of inflammatory mediators on ATP release of human urothelial RT4 cells. BioMed Res Int 2014:182862. doi:10.1155/2014/182862
Mansfield KJ, Hughes JR (2014b) P2Y receptor modulation of ATP release in the urothelium. BioMed Res Int 2014:830374. doi:10.1155/2014/830374
McDermott C, Chess-Williams R, Grant GD, Perkins AV, McFarland AJ, Davey AK, Anoopkumar-Dukie S (2012) Effects of Pseudomonas aeruginosa virulence factor pyocyanin on human urothelial cell function and viability. J Urol 187:1087–1093. doi:10.1016/j.juro.2011.10.129
Moon A (2002) Influence of nitric oxide signalling pathways on pre-contracted human detrusor smooth muscle in vitro. BJU Int 89:942–949
Moro C, Leeds C, Chess-Williams R (2012) Contractile activity of the bladder urothelium/lamina propria and its regulation by nitric oxide. Eur J Pharmacol 674:445–449. doi:10.1016/j.ejphar.2011.11.020
Nomiya M et al (2012) Increased bladder activity is associated with elevated oxidative stress markers and proinflammatory cytokines in a rat model of atherosclerosis-induced chronic bladder ischemia. Neurourol Urodyn 31:185–189. doi:10.1002/nau.21191
Pouya M, Opsomer RJ, Wese FX, Saleh M, Donnay M, Van Cangh PJ (1996) Complications of intravesical mitomycin chemotherapy, apropos of 2 clinical case reports. Acta Urol Belg 64:47–53
Souslova V et al (2000) Warm-coding deficits and aberrant inflammatory pain in mice lacking P2X3 receptors. Nature 407:1015–1017. doi:10.1038/35039526
Tanaka I, Nagase K, Tanase K, Aoki Y, Akino H, Yokoyama O (2011) Modulation of stretch evoked adenosine triphosphate release from bladder epithelium by prostaglandin E(2). J Urol 185:341–346. doi:10.1016/j.juro.2010.09.042
Thrasher JB, Crawford ED (1992) Complications of intravesical chemotherapy. Urol Clin N Am 19:529–539
Wientjes MG, Badalament RA, Wang RC, Hassan F, Au JL (1993) Penetration of mitomycin C in human bladder. Cancer Res 53:3314–3320
Wientjes MG, Dalton JT, Badalament RA, Drago JR, Au JL (1991) Bladder wall penetration of intravesical mitomycin C in dogs. Cancer Res 51:4347–4354
Wyndaele JJ, De Wachter S (2003) The basics behind bladder pain: a review of data on lower urinary tract sensations. Int J Urol Off J Jpn Urol Assoc 10(Suppl):S49–S55
Yokoyama O (2010) Pharmacological and genetic analysis of mechanisms underlying detrusor overactivity in rats. Neurourol Urodyn 29:107–111. doi:10.1002/nau.20746
Yoshimura N, Seki S, Chancellor MB, de Groat WC, Ueda T (2002) Targeting afferent hyperexcitability for therapy of the painful bladder syndrome. Urology 59:61–67
Acknowledgments
This study was funded by a project grant from Cancer Council Queensland and the National Health and Medical Research Council of Australia (527502).
Conflict of interest
The authors have no conflict of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kang, S.H., Chess-Williams, R., Anoopkumar-Dukie, S. et al. Recovery of urothelial mediator release but prolonged elevations in interleukin-8 and nitric oxide secretion following mitomycin C treatment. Naunyn-Schmiedeberg's Arch Pharmacol 388, 781–791 (2015). https://doi.org/10.1007/s00210-015-1092-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00210-015-1092-7