Abstract
Cannabidiol, the major non-psychoactive component of marijuana, has various pharmacological actions of clinical interest. It is reportedly effective as an anti-inflammatory and anti-arthritic in murine collagen-induced arthritis. The present study examined the anti-inflammatory and anti-hyperalgesic effects of cannabidiol, administered orally (5–40 mg/kg) once a day for 3 days after the onset of acute inflammation induced by intraplantar injection of 0.1 ml carrageenan (1% w/v in saline) in the rat. At the end of the treatment prostaglandin E2 (PGE2) was assayed in the plasma, and cyclooxygenase (COX) activity, production of nitric oxide (NO; nitrite/nitrate content), and of other oxygen-derived free radicals (malondialdehyde) in inflamed paw tissues. All these markers were significantly increased following carrageenan.
Thermal hyperalgesia, induced by carrageenan and assessed by the plantar test, lasted 7 h. Cannabidiol had a time- and dose-dependent anti-hyperalgesic effect after a single injection. Edema following carrageenan peaked at 3 h and lasted 72 h; a single dose of cannabidiol reduced edema in a dose-dependent fashion and subsequent daily doses caused further time- and dose-related reductions.
There were decreases in PGE2 plasma levels, tissue COX activity, production of oxygen-derived free radicals, and NO after three doses of cannabidiol. The effect on NO seemed to depend on a lower expression of the endothelial isoform of NO synthase. In conclusion, oral cannabidiol has a beneficial action on two symptoms of established inflammation: edema and hyperalgesia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Marijuana has been known for centuries as a psychoactive medicinal plant. Among its therapeutic applications in the past, alleviation of inflammation, asthma and some forms of pain have been widely described (Mechoulam 1986). Of the different cannabinoids, the most important psychoactive compound is considered to be Δ9-tetrahydrocannabinol (THC). The other important compounds are cannabidiol, cannabigerol, cannabinol, cannabichromene and olivetol, their biosynthetic precursor. THC has potent psychotropic effects, which have complicated the full assessment of its therapeutic potential; cannabidiol, however, does not produce psychoactive effects (Razdan 1986), because it has very low affinity for cannabinoid receptor subtypes CB1 and CB2 (Showalter et al. 1996; Bisogno et al. 2001).
Some reports have described the anti-inflammatory effects of cannabidiol in standard animal tests and isolated cell assays (Sofia et al. 1973; Formukong et al. 1988) and its ability to interfere with some inflammatory mediators (Malfait et al. 2000; Coffey et al. 1996; Formukong et al. 1988; Watzl et al. 1991; Srivastava et al. 1998). Malfait et al. (2000) showed that cannabidiol has beneficial activity in established collagen-induced arthritis in mice.
These findings prompted us to test cannabidiol in a rat model of acute inflammation induced by an intraplantar (i.pl.) injection of carrageenan, frequently used to study inflammation and acute inflammatory pain. To study whether cannabidiol was effective on established inflammation, the compound was administered after the appearance of the classical inflammatory signs. Carrageenan causes edema and exacerbated sensitivity to thermal stimulus, which is known as hyperalgesia. Both these events result from the combined effect of proinflammatory cytokines, cyclooxygenase (COX) products and sympathomimetic amines (Nakamura and Ferreira 1987). The carrageenan-induced inflammatory response has also been linked to neutrophil infiltration and the production of neutrophil-derived free radicals, such as hydrogen peroxide, superoxide and OH° radicals, as well as to the release of other neutrophil-derived mediators (Agha and Gad 1995). The L-arginine-nitric oxide (NO) pathway has also been proposed as an important player in the carrageenan-induced inflammatory response (Tracey et al. 1995; Salvemini et al. 1996a).
We have previously shown that this rat model of acute inflammation was characterized by inflamed paw hyperalgesia, lasting 7 h (Conti et al. 2002), paw edema, lasting 72 h (Costa et al. 2002), and increases in COX activity, NO and oxygen-derived free radicals, that can cause lipid peroxidation and cellular damage (Beckman et al. 1990; Radi et al. 1991; Rubbo et al. 1994), which were still detectable in the inflamed tissues four days after carrageenan (Costa et al. 2002). In the light of this experimental evidence, we also evaluated the influence of repeated treatment with cannabidiol on the mediators and systems responsible for the development and maintenance of carrageenan-induced edema.
Materials and methods
Animals
Male Wistar rats (100–120 g, Harlan, Italy) were used. They were housed in a room with controlled temperature (22±1°C), humidity (60±10%) and light (12 h per day) for at least a week before being used. Food and water were available ad libitum. Animal care was in accordance with Italian State regulations governing the care and treatment of laboratory animals (Permission no. 94/2000A).
Drugs
λ-Carrageenan was purchased from Sigma-Aldrich, Milano, Italy and cannabidiol, dissolved in methanol, was kindly supplied by GW Pharma, Salisbury, UK. After drying off the methanol under speed-vacuum, the cannabidiol residue was emulsified in cremophor, ethanol, and saline (1:1:18).
Experimental design
Acute inflammation was induced by i.pl. injection of 0.1 ml carrageenan (1% w/v in saline) into the right paw. Cannabidiol, or an appropriate volume of vehicle, was administered orally (5, 7.5, 10, 20, and 40 mg/kg; 0.5 ml/hg) after the induction of acute inflammation: 2 h after carrageenan on the 1st day and at the same time as the first injection on the 2nd and 3rd days. Control animals received an i.pl. injection of saline (0.1 ml) and oral doses of drug vehicle.
Carrageenan-induced edema
The paw volume was measured with a plethysmometer (Ugo Basile, Varese, Italy). On the 1st day, the volume was measured immediately before the injection of carrageenan or saline and then after 3, 5, 6, and 7 h. On the next 2 days, paw volumes were recorded just before drug or vehicle injection, and on the last day (the 4th after carrageenan) just before euthanasia. Data are expressed as edema (difference in volume between the right and left paws).
Carrageenan-induced hyperalgesia
Thermal hyperalgesia was evaluated on the same animals used to determine edema, employing the radiant heat method (Hargreaves et al. 1988). After baseline withdrawal latencies (s) had been recorded, hyperalgesia was estimated for each animal 3, 5, 6, and 7 h after carrageenan.
Biochemical studies
Four days after carrageenan injection, animals were killed by cervical dislocation, paws were cut at the level of the calcaneus bone, weighed, crushed at 0–4°C and used for determination of the COX activity and the levels of nitrite/nitrate (NO2 −/NO3 −), endothelial NO synthase (eNOS) protein, and malondialdehyde (MDA). Blood was collected in tubes containing 6.7 mM indomethacin and a buffered solution (pH 7.4) of 0.04 mM disodium EDTA in 0.8% NaCl, as anticoagulant, and immediately centrifuged at 1,250 g for 10 min. The upper plasma layer was removed, rapidly frozen in liquid nitrogen and stored at −20°C until the PGE2 assay.
PGE2 plasma level
This was determined by an EIA procedure employing the commercial kit from Amersham Pharmacia Biotech (Milano, Italy).
COX activity
This was determined polarographically in the microsomal fraction of paw tissue homogenate, as previously described (Costa et al. 2002) and expressed as nanoatoms O/min/g wet tissue, according to Gierse et al. (1999).
NO production
NO was assessed on the basis of NO2 −/NO3 −, which are the oxidation end-products of NO. The paw tissue was homogenized and centrifuged as previously described (Costa et al. 2002) and NO2 −/NO3 − concentrations were measured using the method of Misko et al. (1993).
Lipid peroxide
Lipid peroxides were assayed spectrophotometrically as MDA content, according to the procedure reported by Ohkawa et al. (1979), in hind paw homogenate prepared with a T25, 18 N Ultra-Turrax in a ratio of 1 g wet tissue to 9 ml potassium phosphate (50 mM)-EDTA (0.1 mM) buffer pH 7.4.
Determination of eNOS by Western blot analysis
Tissue was homogenized in 1:4 (w/v) Tris-HCl (50 mM)-EDTA (0.1 mM) buffer, pH 7.4, containing a protease inhibitor cocktail (one tablet for 10 ml; Roche Diagnostics, Milano, Italy). The homogenate was centrifuged at 9,000 g for 10 min at 4°C and the supernatant was ultracentrifuged at 100,000 g for 1 h at 4°C. The microsomal fraction was stored at −80°C until eNOS assay. eNOS was assayed according to Costa et al. (2002).
Statistical analysis
The results were expressed as the mean±SEM. The data were analyzed using one-way analysis of variance (ANOVA) followed by Tukey’s post-hoc test for multiple comparisons. Differences were considered significant at P<0.05. The correlation coefficient (r) was calculated using GraphPAD Software (San Diego, CA, USA).
Results
Effect of cannabidiol on paw hyperalgesia
Intraplantar injection of carrageenan in rats led to a time-dependent thermal hyperalgesia with maximal effect at 3 h (Fig. 1). At this time, hyperalgesia was significantly reduced by the low doses of cannabidiol (5 and 7.5 mg/kg) and abolished by the higher ones (10, 20, and 40 mg/kg). Six hours after carrageenan injection, the lower doses of cannabidiol also abolished hyperalgesia. At no dose did cannabidiol affect the withdrawal latency of the contralateral paws, which remained constant at basal levels for the entire experiment (data not shown).
Effect of different single doses of cannabidiol, administered orally to the rat 2 h after carrageenan, on ipsilateral hindpaw withdrawal latency 3, 5, 6, and 7 h after carrageenan. Each point represents the mean ± SEM of 4–6 rats. °P<0.01 vs. inflamed/vehicle, °°P<0.001 vs. inflamed/vehicle;**P<0.001 vs. inflamed/vehicle for all doses of cannabidiol
Effect of cannabidiol on paw edema
The carrageenan-induced edema remained high throughout the days, as previously shown by us in this rat model of acute inflammation (Costa et al. 2002). All doses of cannabidiol, except the lowest one (5 mg/kg), elicited a slight decrease of edema, already evident a few hours after the first administration (data not shown). Subsequent daily doses of cannabidiol further reduced the edema; particularly at 4 days when the reduction amounted to 50% with 5 mg/kg, about 65% with 7.5, 10 and 20 mg/kg, doses which seemed equipotent, and to 100% with 40 mg/kg (P<0.0001; Fig. 2). After the last dose the reduction in edema was log dose-related (r=0.8514, P<0.05).
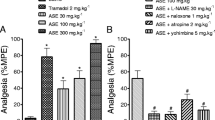
Effect of cannabidiol on the COX system
Four days after carrageenan plasma PGE2 was significantly higher than in non-inflamed animals—about 85%; cannabidiol prevented this increase in a dose-related fashion (r=0.9362, P<0.01). The highest dose (40 mg/kg) brought the PGE2 content down to that of non-inflamed rats (Fig. 3A). At the end of treatment, COX activity measured ex vivo in the paw tissues injected with carrageenan was significantly higher (36%) than in the paw injected with saline. Five mg/kg of cannabidiol did not affect this increase, whereas 7.5 and 10 mg/kg non-significantly reduced COX activity (14% and 21% respectively); 20 and 40 mg/kg cannabidiol brought COX activity down to the level of non-inflamed tissues (P<0.0001; Fig. 3B).
Effect of repeated treatment with cannabidiol on A PGE2 levels in plasma and on B COX activity in microsomes from paw tissues 4 days after carrageenan injection. Each bar represents the mean ± SEM of 4–6 rats. *P<0.05, **P<0.01, ***P<0.001 vs. non-inflamed; °P<0.05, °°P<0.01, °°°P<0.001 vs. inflamed/vehicle
Effect of cannabidiol on the NO system
Four days after carrageenan, inflammation was associated with an elevated production of NO, evaluated as end-products of its metabolism, in the paw tissues: nitrite/nitrate was about four times the levels in non-inflamed tissue. Repeated treatment with cannabidiol reduced this increase in a dose-related fashion (r=0.9810, P<0.01; Fig. 4). The production of nitrite/nitrate in inflamed tissues was associated with an increase in the level of protein corresponding immunologically to the 140 kDa endothelial isoform of eNOS (Fig. 5). Inducible NOS did not contribute to the production of NO end-products, since it was not detectable at this phase of inflammation, as previously shown (Costa et al. 2002). Repeated treatment with cannabidiol reduced the enhancement of eNOS at the lower doses (5, 7.5, and 10 mg/kg) and abolished it at 20 and 40 mg/kg (Fig. 5).
Representative immunoblotting showing eNOS protein in the microsomal fraction of paw tissues 4 days after carrageenan injection: effect of repeated treatment with cannabidiol. 1 Non-inflamed; 2 and 8 inflamed/cannabidiol 5 mg/kg; 3 inflamed/cannabidiol 40 mg/kg; 4 inflamed/cannabidiol 7.5 mg/kg; 5 inflamed/cannabidiol 10 mg/kg; 6 inflamed/cannabidiol 20 mg/kg; 7 inflamed/vehicle
Effect of cannabidiol on lipoperoxidation
Four days after carrageenan, inflammation was accompanied by a 2.5-fold rise in the MDA level in paw tissues. Repeated treatment with cannabidiol reduced this increase in a dose-related fashion (r=0.9674, P<0.01). The highest dose (40 mg/kg) abolished the lipoperoxidation (Fig. 6).
Discussion
The antinociceptive activity of cannabidiol has been studied in the past with the classical analgesic tests, such as the hot plate, Randall-Selitto and writhing tests. These have given conflicting results. Sanders et al. (1979) compared the analgesic actions of cannabidiol and THC in the acetic acid abdominal constriction test and found that a dose of 200 mg/kg of cannabidiol was not active. Sofia et al. (1975) also reported that oral cannabidiol (>300 mg/kg) had no significant analgesic effect in the acetic acid-induced writhing (chemical stimulus) and hot plate (thermal stimulus) tests in mice and in the Randall-Selitto paw pressure test (mechanical stimulus) in rats. Cannabidiol was, however, more potent than other natural cannabinoids in the phenylbenzoquinone (PBQ)-induced mouse writhing test (model of peripheral pain) when given orally 20 min before the i.p. injection of PBQ. It was about 360 times more potent than aspirin and 590 times more potent than THC (Formukong et al. 1988; Evans 1991). In accordance with Sanders et al. (1979) and Sofia et al. (1975) in our hands too cannabidiol showed no analgesic activity in normal conditions and the withdrawal latency of the contralateral paw did not change from the baseline. However, we have shown here, for the first time, that in inflammatory conditions, cannabidiol had potent anti-hyperalgesic activity. Only 1 h after single, very low doses, cannabidiol abolished the hyperalgesia, which develops in the rat paw after carrageenan injection.
We have previously reported that in the rat paw acute inflammation involved significant edema and increases in classical inflammatory mediators, even four days after carrageenan injection; repeated administration of indomethacin (5 mg/kg, p.o.), used as a representative NSAID, after the onset of inflammation, reversed these reactions (Costa et al. 2002). Here we found that this natural constituent of cannabis had dose-dependent anti-inflammatory activity, when administered after the onset of inflammation, indicating that it has a significant therapeutic effect, which may be of benefit in inflammatory diseases. Malfait et al. (2000) have reported the therapeutic efficacy of oral cannabidiol in murine collagen-induced arthritis.
Carrageenan-induced inflammation is due to various mediators such as histamine, 5-hydroxytryptamine, bradykinin, prostaglandins and other COX products (Di Rosa and Willoughby 1971), which operate in parallel to produce this inflammatory response. In addition, at the site of inflammation different cells, including leukocytes, endothelial cells and sensory nerve cells, produce NO, a potent reactive free radical. The simultaneous production of NO and neutrophil-derived oxygen radicals leads to the formation of ONOO− (peroxynitrite), which is considered responsible for the cytotoxicity and lipid peroxidation. This phenomena is one of the basic mechanisms leading to the degradation of membrane lipids and disruption of cell membranes (Yoshikawa and Kondo 1981). Previous investigations showed how closely the anti-inflammatory effect of several compounds is related to their ability to protect against lipid peroxidation (Symons et al. 1988; Claxson et al. 1990; Griffiths et al. 1992).
We found that cannabidiol reduced the stimulation of the COX system induced by carrageenan inflammation; the increases in plasma PGE2 levels and COX activity, measured ex vivo in the inflamed paw tissues, were inhibited in a dose-related manner by cannabidiol. Even at the highest dose (40 mg/kg), however, cannabidiol did not lower COX activity below that found in non-inflamed tissues.
Cannabidiol, like many other cannabinoids, is a powerful antioxidant. Compared with other commonly used antioxidants, cannabidiol protected neurons to a greater degree than the dietary antioxidants α-tocopherol and ascorbate (Hampson et al. 1998). These properties help account for our findings, showing that cannabidiol causes a dose-related reduction in the increases in MDA and NO2 −/NO3 −, end-products of the conversion of NO, in inflamed paw tissues. The cannabidiol-induced decrease in NO2 −/NO3 − was associated with a reduction in the expression of eNOS, the enzymatic isoform responsible for NO production in this late phase of carrageenan-induced inflammation (Costa et al. 2002). However, the ability of cannabidiol and of other cannabinoids to inhibit NO production by mouse peritoneal macrophages activated by lipopolysaccharides and IFN-γ was previously shown by Coffey et al. (1996). Our result is noteworthy in the light of previous reports that the administration of NOS inhibitors to rats reduced carrageenan-induced paw edema (Handy and Moore 1998; Salvemini et al. 1996b). It was difficult to correlate the decrease in edema induced by cannabidiol with its effects on the various biochemical parameters. Only the 40 mg/kg dose, which completely abolished inflammation, simultaneously normalized all biochemical inflammatory parameters, while lower doses were not as effective on the edema or on these parameters. The lower doses (5 and 7.5 mg/kg), which were significantly anti-inflammatory, did not reduce the COX system overactivity or lipoperoxide production, and significantly inhibited only the increase in NO paw tissue and the expression of eNOS. These findings could reflect a difference in sensitivity of COX and NO systems to cannabidiol. In addition it should be pointed out that stimulation of these systems showed a different time course during the carrageenan-induced inflammation; in fact, 4 days after carrageenan, the level of NO in inflamed paw tissues was much lower than 3 h post injection (data not shown), according to Salvemini et al. (1996b) and to our previous results (Costa et al. 2002), while the COX system and lipoperoxidation in inflamed animals were still increased 4 days after carrageenan as well as in the acute phase (data not shown). So only the higher doses of cannabidiol administered three times were dose-dependently able to prevent the increases in COX activity and products (PGE2) and the lipid peroxidation still largely present in damaged tissues.
In summary, our findings show, first, that cannabidiol had potent beneficial anti-hyperalgesic effects on carrageenan-evoked thermal hyperalgesia, and anti-inflammatory efficacy on carrageenan-induced paw edema. It also significantly inhibited the overproduction of NO, eNOS, MDA and PGE2 and the stimulation of COX activity in paw tissues; however these findings do not establish whether these systems could represent the molecular target of cannabidiol.
References
Agha A, Gad MZ (1995) Lipid peroxidation and lysosomal integrity in different inflammatory models in rats: the effects of indomethacin and naftazone. Pharmacol Res 32:279–285
Beckman JS, Beckman TW, Chen TW, Marshall PA, Freeman BA (1990) Apparent hydroxyl radical production by peroxynitrite: implication of endothelial injury from nitric oxide and superoxide. Proc Natl Acad Sci USA 87:1620–1624
Bisogno T, Hanus L, De Petrocellis L, Tchilibon S, Ponde DE, Brandi I, Moriello AS, Davis JB, Mechoulam R, Di Marzo V (2001) Molecular target for cannabidiol and its synthetic analogues: effect on vanilloid VR1 receptors and on the cellular uptake and enzymatic hydrolysis of anandamide. Br J Pharmacol 134:845–852
Claxson A, Morris C, Blake D, Siren M, Halliwell B, Gustafsson T, Lofkvist B, Bergelin I (1990) The anti-inflammatory effects of D-myoinositol-1,2,6-triphosphate (PP56) on animal models of inflammation. Agents Actions 29:68–70
Coffey RG, Yamamoto Y, Snella E, Pross S (1996) Tetrahydrocannabinol inhibition of macrophage nitric oxide production. Biochem Pharmacol 52:743–751
Conti S, Costa B, Colleoni M, Parolaro D, Giagnoni G (2002) Antiinflammatory action of endocannabinoid palmitoylethanolamide and the synthetic cannabinoid nabilone in a model of acute inflammation in the rat. Br J Pharmacol 135:181–187
Costa B, Conti S, Giagnoni G, Colleoni M (2002) Therapeutic effect of the endogenous fatty acid amide, palmitoylethanolamide, in rat acute inflammation: inhibition of nitric oxide and cyclo-oxygenase systems. Br J Pharmacol 137:413–420
Di Rosa M, Willoughby DA (1971) Screens for anti-inflammatory drugs. J Pharm Pharmacol 23:297–300
Evans FJ (1991) Cannabinoids: the separation of central from peripheral effects on a structural basis. Planta Med 57 [Suppl]:60–67
Formukong EA, Evans AT, Evans FJ (1988) Analgesic and anti-inflammatory activity of constituents of Cannabis sativa L. Inflammation 12:361–371
Gierse JK, Koboldt CM, Walker MC, Siebert K, Isakson PC (1999) Kinetic basis for selective inhibition of cyclo-oxygenase. Biochem J 339:607–614
Griffiths HR, Dowling EJ, Sahinoglu T, Blake DR, Parnham M, Lunec J (1992) The selective protection afforded by ebselen against lipid peroxidation in a ROS-dependent model of inflammation. Agents Actions 36:107–111
Hampson AJ, Grimaldi M, Axelrod J, Wink D (1998) Cannabidiol and Δ9-tetrahydrocannabinol are neuroprotective antioxidants. Proc Natl Acad Sci USA 95:8268–8273
Handy RL, Moore PK (1998) A comparison of the effects of L-NAME, 7-NI and L-NIL on carrageenan-induced hindpaw oedema and NOS activity. Br J Pharmacol 123:1083–1088
Hargreaves K, Dubner R, Brown F, Flores C, Joris J (1988) A new and sensitive method for measuring thermal nociception in cutaneous hyperalgesia. Pain 32:77–98
Malfait AM, Gallily R, Sumariwalla PF, Malik AS, Andreakos E, Mechoulam R, Feldmann M (2000) The nonpsychoactive cannabis constituent cannabidiol is an oral anti-arthritic therapeutic in murine collagen-induced arthritis. Proc Natl Acad Sci USA 97:9561–9566
Mechoulam R (1986) The pharmacohistory of Cannabis sativa. In: Mechoulam R (ed) Cannabinoids as therapeutic agents. CRC, Boca Raton, pp 1–19
Misko TP, Schilling RJ, Salvemini D, Moore WM, Currie MG (1993) A fluorimetric assay for the measurement of nitrite in biological samples. Anal Biochem 214:11–16
Nakamura M, Ferreira SH (1987) A peripheral sympathetic component in inflammatory hyperalgesia. Eur J Pharmacol 135:145–153
Ohkawa H, Ohishi N, Yagi K (1979) Assay for lipid peroxides in animal tissues by thiobarbituric acid reaction. Anal Biochem 95:351–358
Radi R, Beckman JS, Bush KM, Freeman BA (1991) Peroxynitrite-induced membrane lipid peroxidation: the cytotoxic potential of superoxide and nitric oxide. Arch Biochem Biophys 288:481–487
Razdan RK (1986) Structure activity relationships in cannabinoids. Pharmacol Rev 38:75–149
Rubbo H, Radi R, Trujillo M, Telleri R, Kalyanaraman B, Barnes S, Kirk M, Freeman BA (1994) Nitric oxide regulation of superoxide and peroxynitrite-dependent lipid peroxidation. J Biol Chem 269:26066–26075
Salvemini D, Wang ZQ, Bourdon DM, Stern MK, Currie MG, Manning PT (1996a) Evidence of peroxynitrite involvement in the carrageenan-induced rat paw edema. Eur J Pharmacol 303:217–220
Salvemini D, Wang ZQ, Wyatt PS, Bourdon DM, Marino MH, Manning PT, Currie MG (1996b) Nitric oxide: a key mediator in the early and late phase of carrageenan-induced rat paw inflammation. Br J Pharmacol 118:829–838
Sanders J, Jackson DM, Starmer GA (1979) Interactions among the cannabinoids in the antagonism of the abdominal constriction response in the mouse. Psychopharmacology 61:281–285
Showalter VM, Compton DR, Martin BR, Abood ME (1996) Evaluation of binding in a transfected cell line expressing a peripheral cannabinoid receptor (CB2): identification of cannabinoid receptor subtype selective ligands. J Pharmacol Exp Ther 264:463–468
Sofia RD, Knobloch LC, Vassar HB (1973) The anti-edema activity of various naturally occurring cannabinoids. Res Commun Chem Pathol Pharmacol 6:909–918
Sofia RD, Vassar HB, Knobloch LC (1975) Comparative analgesic activity of various naturally occurring cannabinoids in mice and rats. Psychopharmacologia 40:285–295
Srivastava MD, Srivastava BI, Brouhard B (1998) Delta-9-tetrahydrocannabinol and cannabidiol alter cytokine production by human immune cells. Immunopharmacology 40:179–185
Symons AM, Dowling EJ, Parke DV (1988) Lipid peroxidation, free radicals and experimental inflammation. Basic Life Sci 49:987–990
Tracey WR, Nakane M, Kuk J, Budzig G, Klinghofer V, Harris R, Cartel G (1995) The nitric oxide synthase inhibitor, L-NG-monomethylarginine, reduces carrageenan-induced pleurisy in the rat. J Pharmacol Exp Ther 273:1295–1299
Watzl B, Scuderi P, Watson RR (1991) Marijuana components stimulate human peripheral blood mononuclear cell secretion of interferon gamma and suppress interleukin-1 alpha in vitro. Int J Immunopharmacol 13:1091–1097
Yoshikawa T, Kondo M (1981) In: Goto Y, Yagi K (eds) Lipid peroxide and disease. Igaku-shoin, Tokyo, p 210
Acknowledgements
This work was supported by grants from the Italian Ministry for Education, University and Research (M.I.U.R.). The authors thank GW Pharma for kindly supplying cannabidiol.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Costa, B., Colleoni, M., Conti, S. et al. Oral anti-inflammatory activity of cannabidiol, a non-psychoactive constituent of cannabis, in acute carrageenan-induced inflammation in the rat paw. Naunyn-Schmiedeberg's Arch Pharmacol 369, 294–299 (2004). https://doi.org/10.1007/s00210-004-0871-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00210-004-0871-3