Abstract
This study aimed at showing the yeast diversity in feces of Algerian infants, aged between 1 and 24 months, hospitalized at Bejaia hospital (northeast side of the country). Thus, 20 colonies with yeast characteristics were isolated and identified using biochemical (ID32C Api system) and molecular (sequencing of ITS1-5.8S-ITS2 region) methods. Almost all colonies isolated (19 strains) were identified as Candida spp., with predominance of Candida albicans species, and one strain was identified as Saccharomyces cerevisiae. Screening of strains with inhibitory activities unveiled the potential of Candida parapsilosis P48L1 and Candida albicans P51L1 to inhibit the growth of Escherichia coli ATCC 25922 and Staphylococcus aureus ATCC 25923. Further studies performed with these two Candida strains revealed their susceptibility to clinically used antifungal compounds and were then characterized for their cytotoxicity and hemolytic properties. On the other hand, Saccharomyces cerevisiae P9L1 isolated as well in this study was shown to be devoid of antagonism but resulted safe and overall usable as probiotic.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The human gastrointestinal tract is a complex ecological niche containing a multitude of microbes including bacteria, yeast and fungi. These microbes are foreseen to be inherited from the mother and the surrounding environments and colonize the gastrointestinal tract of infants immediately after the birth (O’Hara and Shanahan 2006). Bacteria are the most dominant microbes (more than 99 % of total population) (Ojetti et al. 2009), but eukaryotic cells such as yeasts and filamentous fungi are also part of this microbiota (Rajilić-Stojanović et al. 2009). The presence of yeasts in the gastrointestinal tract of infants was observed at early age, although these unicellular eukaryotic cells represent <1 % of the gut microbiota (Chandler et al. 1980). However, their role and functions in the equilibrium of the microbiota are not insignificant (Parfrey et al. 2011). Candida species are typically harmless eukaryotic commensal yeasts that are members of the Ascomycota phylum and can thus be recovered from the mammalian and environment sources. They are detected in all gastrointestinal sections of about 70 % of healthy adults and are normally found in feces. Most of yeasts isolated are members of the Candida genus (Schulze and Sonnenborn 2009) and are commonly located in the normal commensal microbiota on the mucosal surfaces of the gastrointestinal and genitourinary tracts (Kumamoto 2011). Candida species were also encountered in the majority of neonates by the end of the first month of life (Schulze and Sonnenborn 2009). Remarkably, Candida genus could provoke local or systemic opportunistic infections in hospitalized patients, particularly in patients with compromised immune system (Moris et al. 2008). Most often Candida albicans is the guilty agent, but prevalence of non-albicans Candida species in some patients was reported (Mac Callum 2010). Harmless and nonpathogenic species such as Saccharomyces cerevisiae were also reported (Psomas et al. 2001). S. cerevisiae is marketed as probiotic formulation to treat various human gastrointestinal disorders (Lukaszewicz 2012). The beneficial effects of yeasts include their competitiveness for nutrients and adhesion, production of antagonistic compounds, immunomodulation, cholesterol assimilation, toxin elimination and adhesion and then neutralization of pathogenic bacteria (Moslehi-Jenabian et al. 2010; Hatoum et al. 2012; Ceugniez et al. 2015). Here, we use a culture-dependent approach to establish the yeast diversity of Algerian infants hospitalized at Bejaia hospital, for reasons other than gastrointestinal disorders. This analysis permitted the isolation of 20 yeasts with a bulk of C. albicans species, and lesser with non-albicans Candida species and one isolate of S. cerevisiae P9L1. This report unveils the inhibitory properties of yeast pathogens C. parapsilosis P48L1 and C. albicans P51L1. These antagonistic yeasts as well as S. cerevisiae P9L1 were deeply studied for their negative and positive effects. To the best of our knowledge, this is the first report shedding light and dealing with yeast diversity from an Algerian infants reservoir.
Materials and methods
Isolation of yeasts
Yeasts were isolated from feces of 62 infants without gastrointestinal disorders (diarrhea), aged between 1 and 24 months, and hospitalized in the pediatric service of Khalil Amrane hospital at Bejaia city (Algeria). An aliquot (1 g) of feces was resuspended in 9 ml of saline solution (0.9 % NaCl) and then plated in yeast extract-peptone-dextrose agar (YPD), pH 5.5, supplemented with 100 µg/ml of filter-sterilized oxytetracycline (Biokar, France). Plates were incubated at 37 °C for 48 h. Five colonies with yeast characteristics were purified by repeated streaking on YPD agar plates. These colonies were then maintained in YPD broth at +4 °C until use.
Biochemical identification of yeasts with ID 32C Api systems
All yeast colonies were identified based on their biochemical profiles using ID32C strips (BioMérieux, Marcy l’Etoile, France). Before inoculation of the ID32C system, strains were streaked on YPD agar plates and incubated for 24 h at 25 °C. After inoculation, ID32C systems were incubated at 25 °C for 48 h. After this period of incubation, the carbohydrate assimilation profile obtained for each tested isolate was compared to the database apiweb version 3.0 (BioMérieux) to obtain the final yeast diagnosis (Ceugniez et al. 2015).
Statistical analysis of ID32 C and ITS1-5.8S-ITS2 rDNA sequencing was performed with the software SPSS® Statistic v20 of IBM® (Armonk, NY, USA). Correlation and comparison were made with the crossed grid methods using Kappa of Cohen value.
Molecular identification of yeasts by sequencing their ITS1-5.8S-ITS regions
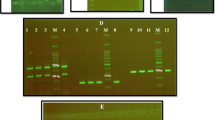
Total DNA was extracted from each isolate with the Bust n’Grab method (Harju et al. 2004). Afterward, it was quantified and amplified using the ITS1 forward primer 5′-TCC GTA GGT GAA CCT GCG G-3′ and the ITS4 reverse primer 5′-TCC TCC GCT TAT TGA TAT GC-3′ (Belloch et al. 1998; Schoch et al. 2012) and the following PCR program: initial denaturation 5 min at 94 °C, denaturation 30 s at 94 °C, annealing 30 s at 57 °C, elongation 1 min at 72 °C and final elongation 5 min at 72 °C. Thirty-five cycles were used for each amplification.
PCR products were purified using the Nucleospin® Gel and PCR Clean-Up kit of Machery-Nagel (Düren, Germany). PCR products were sequenced at Eurofins Genomics (Ebersberg, Germany). All these sequences were compared to those available on the NCBI database using a megablast research, and confirmed using the Ribosomal Database project on sequence match with default parameters except size placed at “<1200” parameter (Cole et al. 2014).
Screening of yeasts with inhibitory activities
The spot-on-lawn method was used to evaluate the antagonistic activity of yeast isolates against E. coli ATCC 25922, S. aureus ATCC 25923 and Listeria innocua CLIP 74915. An overnight culture of each yeast isolate was prepared in YPD broth at 37 °C and individually inoculated onto YPD agar plates by spot-inoculating 5 µl, leading to a zone of inhibition of 6 mm. The plates were incubated at 37 °C for 48 h. The growth in each plate was then overlaid with 10 ml of molten nutrient agar [0.7 % (w/v) agar, Fluka, Ireland] previously inoculated with the pathogen cultures (106 CFU/ml). The plates were incubated aerobically at 37 °C for 18 h and then examined for growth inhibition zones (Gotcheva et al. 2002).
Hemolytic activity
The hemolytic activity of yeasts was carried out as recently described by Kumar and Sharma (2013) but with slight modifications. Thus, 10 µl of yeast culture was spotted onto YPD agar plates containing 5 % (v/v) sheep blood (Eurobio, Les Ulis, France). Plates were incubated at 37 °C for 48 h in aerobic conditions. After this period, a transparent/semitransparent zone around the spots was considered as positive hemolytic activity.
Acid and bile tolerance
The survival under conditions simulating those encountered in the gastrointestinal tract was investigated for antagonistic yeasts and S. cerevisiae. To test the strains for acid tolerance, yeasts from fresh (24 h) culture in YPD broth were centrifuged (5000g, 10 min) and the pellets obtained were washed twice with phosphate-buffered saline (PBS) and then resuspended, at 107 CFU/ml, in 5 ml of PBS adjusted to pH 1.5, 2 or 3. Samples were taken after 0, 1 and 3 h of incubation at 37 °C and plated onto YPD agar to determine the number of viable cells. Survival rate was determined by comparing the number of viable cells after incubation to the initial suspended cells number. To test the bile tolerance, 5 ml PBS containing 0.3, 0.5, 1 and 2 % (w/v) oxgall bile (Sigma-Aldrich, Steinheim, Germany) was inoculated with the yeast culture (106 CFU/ml) and then incubated at 37 °C for 4 h. After incubation, survival rate was determined as described for acid tolerance assays.
Antifungal susceptibility tests
Antagonistic yeasts as well as S. cerevisiae were tested for in vitro susceptibility to amphotericin, 5-fluorocytosin, fluconazole, voriconazole and caspofungin of clinical use using the CLSI BMD method (Clinical and standard, Institute). Minimum inhibitory concentration (MIC) assays were read after 24 h of incubation when tested against Candida spp., whereas the MIC endpoints for triazoles were read after 48 h when they were tested against non-Candida yeasts. In all instances, MICs were determined visually as the lowest concentration of drug that caused significant diminution of growth levels.
Adhesion and cytotoxicity assays performed on antagonistic yeasts
Cell line culture
The cell line used for the adhesion and cytotoxicity assays was the human colorectal adenocarcinoma Caco-2 (Sigma-Aldrich, Steinheim, Germany). Cells were routinely grown in 75 cm2 flasks in a controlled atmosphere of 5 % CO2 and 95 % air at 37 °C in Dulbecco’s Modified Essential Medium (DMEM, Biowest, France) containing 4.5 g/l glucose, 2 mM l-glutamine, 100 U/ml penicillin, 100 U/ml streptomycin, 1 % (v/v) nonessential amino acids and 10 % (v/v) fetal bovine serum (FBS). All the reagents were from PAN-Biotech GmbH (Aidenbach, Germany).
Adhesion assay
To assess the adhesion potential, when sub-confluence was reached, Caco-2 cells were prepared in 24-well tissue culture plates by seeding 4 × 104 cells per well and incubating for 24 h. Overnight yeast cultures (107 CFU/ml) were harvested by centrifugation (5000g, 10 min), resuspended in DMEM without FBS and antibiotics and then applied on confluent Caco-2 cell monolayers (106 CFU/well). After 2 h of incubation at 37 °C (5 % CO2 and 95 % air), monolayers were washed twice with 300 µl of phosphate-buffered saline (PBS, 100 mM, pH 7.4) to remove nonadherent yeasts, and Caco-2 cells were lyzed by incubation at room temperature for 15 min in the presence of 0.1 % Triton X100, to keep yeast only. Lysates were diluted and plated onto YPD agar to determine the number of adherent yeasts.
CCK-8 cytotoxicity assay
Cytotoxicity of selected yeast strains toward Caco-2 cells was assessed in vitro using the Cell Counting Kit-8 (CCK-8) assay (Dojindo Molecular Technologies, Japan). CCK-8 allows convenient assays using water-soluble tetrazolium salt: WST-8[2-(2-methoxy-4-nitrophenyl)-3-(4-nitrophenyl)-5-(2,4-disulfophenyl)-2H-tetrazolium, monosodium salt)], which produces, upon bioreduction by cellular dehydrogenases, an orange-colored formazan. The amount of formazan produced is directly proportional to the number of living cells. Caco-2 cells were seeded at a density of 8 × 103 cells/well in 96-well cell culture plates and preincubated for 24 h before being incubated with yeasts (105 CFU/well) prepared in DMEM as described for the adhesion assay. After incubation, the medium was removed and cells were incubated with 150 µl of DMEM containing 50 µl of CCK-8 reagent for 4 h 37 °C. The relative viability (%) was then calculated based on absorbance at 450 nm using a microplate reader (Xenius SAFAS, Monaco). Results were expressed as percentage of proliferation. Viability of nontreated control cells was defined as 100 %. Absorbance of wells without Caco-2 cells and with yeasts was subtracted from absorbance of wells containing Caco-2 cells and yeasts.
Aggregation assays
The auto-aggregation assays were performed using the method described by Kos et al. (2003). Yeast was grown for 24 h at 37 °C in YPD broth. The cells were harvested by centrifugation (5000g, 10 min at 4 °C), washed twice with PBS (pH 7.2) and resuspended in the PBS. Cells suspensions were mixed by vortexing for 30 s, and auto-aggregation was determined after 2 and 4 h of incubation at 37 °C. An aliquot (1 ml) of these suspensions was carefully removed from the upper zone, and the absorbance at 600 nm was read on a spectrophotometer (Shimadzu, Germany). The auto-aggregation percentage was expressed as:
where A t represented the absorbance at time t = 2 or 4 h and A 0 the absorbance at t = 0 h.
For co-aggregation with pathogens, E. coli ATCC 25922 and S. aureus ATCC 25923 were grown in nutrient broth at 37 °C for 18 h. Yeast and pathogens cell suspensions from overnight cultures were prepared as described above in PBS. Equal volumes (2 ml) of yeast and pathogen suspensions were mixed by vortexing 30 s in glass test tubes. Control tubes contained 4 ml of suspension of each bacterial and yeast strains. Absorbance was measured immediately and after 2 h incubation at 37 °C. The percentage of co-aggregation was calculated using equation:
where A represented absorbance, x and y represented each of the two strains in the control tubes, and (x + y) their mixture.
Construction of phylogenetic tree
A phylogenetic tree was established on PhyML v3.1 based on Maximum-Likelihood algorithm, after ClustalΩ multialign of all sequenced strains, and with following parameters: bootstrap on branch support of 1000 replicates, nucleotide equilibrium frequencies on optimized, invariable sites in optimized, across site variations in optimized, tree-searching operation in best of NNI & SPR and starting tree at BioNJ and optimized tree topology. To set up this phylogenetic tree, we used the recent seaview software (Gouy et al. 2010).
Results
Yeasts isolated from Algerian infants display inhibitory properties
Yeasts were isolated from feces of infants aging between 1 and 24 months (Table 1). Afterward, their identification was performed by ID 32C Api system, and sequencing of the ITS1-5.8S-ITS2 region is shown in Table 1. Out of 20 strains identified by these two independent methods, only the identification of P5L1 and P27L1 resulted to be different. The identification of P1L1 is consistent because Pichia kuriavzevii, which is a synonym for Issatchenkia orientalis, is the teleomorph of C. krusei (Table 1). Thus, these two independent methods showed a good correlation and concordance, as supported statistically with Kramer and Kappa values of 0.914 and 0.615, respectively. Out 20 colonies, 19 colonies belonged to Candida species, whilst one colony was identified as S. cerevisiae P9L1. In this repertoire, C. albicans was the dominant species. The ITS1-5.8S-ITS2 sequences of C. albicans isolated here were highly similar (>99 %) to that of C. albicans ATCC 10231 (Table 1). The phylogenetic tree indicated that all the C. albicans isolates belonged to the same group (Fig. 1; Table 2), considering the strain P35L1 as the most “ancestral”. Remarkably, the reference strain C. albicans ATCC 10231, not present in the hospital, was in the same group of hospital strains, advocating that a multigenic phylogenetic tree would be more suitable.
Furthermore, pathogen yeasts C. parapsilosis P48L1 and C. albicans P51L1 displayed inhibitory activities against E. coli ATCC 25922 and S. aureus ATCC 25923 (Table 3; Fig. 2).
Highlights on probiotic properties of antagonistic yeasts
Adhesion and cytotoxicity to Caco-2 cells
The capabilities of adhesion of C. parapsilosis p48L1, C. albicans p51L1 and S. cerevisiae P9L1 to human Caco-2 cells are studied. As shown in Fig. 3a, the highest level of adhesion was obtained with S. cerevisiae P9L1 with 6.34 %, followed then by C. parapsilosis P48L1 with 2.03 % and C. albicans P51L1 with 0.76 %. Besides, a cytotoxic effect was observed as expected for C. parapsilosis P48L1 and C. albicans P51L1 with 5.33 and 20.56 % survival, respectively (Fig. 3b). However, no cytotoxic effect was registered for S. cerevisiae P9L1 (Fig. 3b), as no significant difference was noted between the control test (noninfected Caco-2 cells) and S. cerevisiae P9L1 with a p value >0.5.
a Adhesion capabilities of C. albicans P51L1, C. parapsilosis P48L1 and S. cerevisiae P9L1 to Caco-2 cells after 2 h of incubation at 37 °C. The data are the means of at least three independent experiments. b Cytotoxic effect of C. albicans P51L1, C. parapsilosis P48L1 and S. cerevisiae P9L1 on Caco-2 cells (24 h). The data are the means of at least three independent experiments. Means without a common letter are different (p < 0.01) using one-way ANOVA with Tukey test for pairwise comparisons
Resistance to acidic conditions, bile concentration and antifungal compounds
As shown on Fig. 4a, the survival of S. cerevisiae P9L1 was pH dependent. At pH 3, this yeast resisted perfectly even after 3 h of incubation. When the pH was adjusted to 2 and 1.5, a drop in survival rate was registered reaching thereof 92.1 and 28.4 % after 3 h of incubation, respectively. Conversely, no decrease in survival of C. parapsilosis P48L1 and C. albicans P51L1 was registered. Similarly, these three yeasts were examined for their bile tolerance. As shown on Fig. 4b, C. parapsilosis P48L1 and C. albicans P51L1 were fully resistant to 2 % (not for 4 %, data not shown) of bile concentration and after 4 h of incubation, contrarily to S. cerevisiae P9L1, which was unable to support such harsh conditions as only 46.7 % of survival was registered.
a Survival rate of the strains S. cerevisiae P9L1, C. parapsilosis P48L1 and C. albicans P51L1 under acidic pH conditions after 1 and 3 h of incubation. b Survival rate of S. cerevisiae P9L1, C. parapsilosis P48L1 and C. albicans P51L1 at different bile concentrations after 2 and 4 h of incubation. The standard deviations are indicated by error bars. The data are the means of values from three independent experiments. Means without a common letter are different (p < 0.05) using one-way ANOVA with Tukey test for pairwise comparisons
Moreover, the antifungal susceptibility profiles of C. parapsilosis P48L1, C. albicans P51L1 and S. cerevisiae P9L1 were performed in an effort to provide MIC data (Table 4) for optimal therapy. The assays performed showed that C. parapsilosis P48L1, C. albicans P51L1 and S. cerevisiae P9L1 were susceptible to clinical antifungal compounds such as amphotericin B, 5-fluorocytosin, fluonazole, voriconazole and caspofungin. The interpretation of susceptibility and resistance to antifungal compounds were performed in agreement with the EUCAST and CLSI recommendations (Cuenca-Estrella et al. 2012).
Hemolytic activities and aggregation properties
Candida albicans P51L1 and S. cerevisiae P9L1 could be considered as nonhemolytic strains contrary to C. parapsilosis P48L1 which resulted to be hemolytic (Fig. 5). The auto-aggregation rate of S. cerevisiae was 22.5 ± 2.6 and 45.9 ± 3.4 % after 2 and 4 h of incubation, respectively. This strain co-aggregated with two tested pathogenic bacteria. Notably, the co-aggregation was stronger and faster with E. coli ATCC 25922 (38.2 ± 3.9 %) than with S. aureus ATCC 25923 (23.5 ± 2.9 %) after 2 h of incubation. Conversely, the antagonistic strains C. parapsilosis P48L1 and C. albicans P51L1 did not co-aggregate with the tested pathogenic bacteria. These strains showed an auto-aggregation rate of 41.5 ± 1.9 and 31.6 ± 2.9 after 4 h, respectively (Table 5). Thus, C. albicans P51L1 was the less auto-aggregative strain.
Accession numbers
The ITS1-5.8S-ITS2 rDNA sequences of the strains isolated here are available on NCBI under accession number KP878240 to KP878254.
Discussion
This study showed, for the first time, the yeast diversity of Algerian infants hospitalized at Bejaia hospital. Out of 20 strains isolated and purified from feces of different donors, 19 strains belonged to Candida species, and one was identified as S. cerevisiae P9L1. The identification performed with biochemical (ID32C Api system) and molecular (sequencing of ITS1-5.8S-ITS2 region) methods showed a very good reliability. The most abundant species recovered was C. albicans, a species that has been found in diverse niches including the normal gastrointestinal tract, oral cavity and urogenital tract microbiota (De Vos et al. 2012). Recently, Papon et al. (2013) pointed out C. albicans as the most frequent agent of candidiasis. Similar studies carried out worldwide reported the dominance of C. albicans species in infant feces. Indeed, Rozkiewicz et al. (2005) studied the prevalence of this pathogen in feces of hospitalized children with and without diarrhea in Bialystok (Poland). The authors identified C. parapsilosis and C. krusei, and noteworthy C. albicans. Indeed, 131 strains belonged to C. albicans (Rozkiewicz et al. 2005). The incidence of fecal C. albicans in children with and without diarrhea was comparable (Rozkiewicz et al. 2005). In another study carried out on Nigerian infants, C. albicans resulted as the dominant species even other species including C. tropicalis, C. pseudotropicalis, C. glabrata and C. parapsilosis were also identified (Enweani et al. 1994). The study realized by Forbes et al. (2001) on fecal yeasts in feces of hospitalized children in Western Australia has revealed the presence of C. albicans, C. parapsilosis, C. guillermondii, C. lipolytica, C. humicola, Torulopsis glabrata, Trichsporon beigelii and Rhodotorula glutinis, but C. albicans was the most commonly identified species.
Moreover, non-albicans Candida (NAC) species have been also isolated from feces of Algerian infants but with a lower isolation rate. The NAC species isolated were C. krusei (synonym: Issatchenkia orientalis), C. glabrata, C. rugosa, C. parapsilosis, C. tropicalis, C. rugosa and C. famata (synonym: Debaryomyces hansenii). According to Papon et al. (2013), the NAC species now account for a substantial part of clinical isolates collected worldwide in hospitals.
The last decade has demonstrated the success of DNA-sequence-based methods (SBM methods) as suitable method to study epidemiology of C. albicans. To strengthen the SBM approaches, we show here that ITS1-5.8S-ITS2 sequences analysis is a robust and affordable method that might be used to identify C. albicans species and NAC species. The dendrogram resulting from ITS1-5.8S-ITS2 sequences analysis led us to think that our C. albicans isolates are genetically related to C. albicans ATCC 10231 (data not shown).
Screening of inhibitory activities has shed light on the potential of C. parapsilosis P48L1 and C. albicans P51L1 to inhibit E. coli ATCC 25922 and S. aureus ATCC 25923. In the best of our knowledge, this is the first report underlining inhibitory properties of notorious pathogen yeast species from infant origin. C. parapsilosis P48L1 and C. albicans P51L1 were active against E. coli ATCC 25922 and S. aureus ATCC 25923 although they were unable to co-aggregate and weakly aggregating, arguing that a cell–cell contact might not be only the inhibitory pathway requested. Related to inhibitory activities of yeasts, Hatoum et al. (2012) reported that most often yeast antagonism was attributed to killer toxins. However, yeast antagonism remains to be investigated contrarily to its bacterial counterpart, which is well characterized (Drider and Rebuffat 2011). The auto-aggregation is considered as key element for adhesion and biofilm formation. Indeed, the auto-aggregation potential reported for S. cerevisiae P9L1 renders this strain as potential candidate for probiotic design. Moreover, the co-aggregation confers the ability to form a barrier against pathogens, and it is thereof considered as an important property for probiotic strains according to Mobili et al. (2010). S. cerevisiae P9L1 isolated in this study fulfills these properties.
The adverse effects registered for C. parapsilosis P48L1 and C. albicans P51L1 yeasts render evidently these strains as nonsuitable for probiotic design in spite of their antagonism against E. coli ATCC 25922 and S. aureus ATCC 25923, their in vitro tolerance to bile salts and susceptibility to traditional antifungal compounds such as amphotericin B, 5-fluorocytosin, fluonazole, voriconazole and caspofungin, which are routinely and clinically used and recommended to treat fungi infections therapy.
Further, C. parapsilosis P48L1 and C. albicans P51L1, conversely to harmless S. cerevisiae P9L1, displayed low adhesion score and cytotoxic effects to human epithelial colorectal adenocarcinoma Caco-2 cells. The adhesion process to host cells has been described as a prerequisite factor in the Candida infection process (Schulze and Sonnenborn 2009; Vazquez and Sobel 2011) on the other hand considered the adhesion step as a key event, which permits interactions between probiotics and the host cells (Lu and Walker 2001).
To sum up, this prospective study allowed the isolation of 20 yeasts including C. albicans and NAC species from Algerian infants. C. parapsilosis P48L1 and C. albicans P51L1 exhibited antibacterial activity against pathogenic bacteria but resulted to be toxic. S. cerevisiae P9L1 appeared to be devoid of hemolytic activity, resistant to acidic conditions, tolerant to increasing bile concentration, and able to adhere to epithelial cells, aggregate and co-aggregates with pathogens. To the best of our knowledge, this is the first report discussing yeast diversity in a north-African reservoir and characterizing these yeasts for their positive and negative effects.
References
Belloch C, Barrio E, Garcia MD, Querol A (1998) Phylogenetic reconstruction of the yeast genus Kluyveromyces: restriction map analysis of the 5.8S rRNA gene and the two ribosomal internal transcribed spacer. Syst Appl Micriobiol 21:266–273
Ceugniez A, Drider D, Jacques P, Coucheney F (2015) Yeast diversity in a traditional French cheese “Tomme d’orchies” reveals infrequent and frequent species with associated benefits. Food Microbiol 52:177–184
Chandler FW, Kaplan W, Ajello L (1980) Color atlas and text of the histopathology of mycotic diseases. Year Book Medical Publisher, Chicago, p 333
Cole JR, Wang Q, Fish JA, Chai B, McGarrell DM, Sun Y, Brown CT, Porras-Alfaro A, Kuske CR, Tiedje JM (2014) Ribosomal Database Project: data and tools for high throughput rRNA analysis. Nucleic Acids Res 42:D633–D642
Cuenca-Estrella M, Verweij PE, Arendrup MC, Arikan-Akdagli S, Bille J, Donnelly JP, Jensen HE, Lass-Flörl C, Richardson MD, Akova M, Bassetti M, Calandra T, Castagnola E, Cornely OA, Garbino J, Groll AH, Herbrecht R, Hope WW, Kullberg BJ, Lortholary O, Meersseman W, Petrikkos G, Roilides E, Viscoli C, Ullmann AJ, ESCMID Fungal Infection Study Group 2012 (2012) ESCMID* guideline for the diagnosis and management of Candida diseases 2012: diagnostic procedures. Clin Microbiol Infect 7:9–18
De Vos WM, Engstrand L, Drago L, Reid G, Schauber J, Hay R, Mendling W, Schaller M, SpillerR Gahan CG, Rowland I (2012) Human microbiota in health and disease. SelfCare 3(S1):1–68
Drider D, Rebuffat S (2011) Prokaryotic antimicrobial peptides: from genes to applications. Springer, New York, p 451
Enweani IB, Obi CL, Jokpeyibo M (1994) Prevalence of Candida species in Nigerian children with diarrhoea. J Diarrhoeal Dis Res 12:133–135
Forbes D, Ee L, Camer-Pesci P, Ward PB (2001) Faecal Candida and diarrhea. Arch Dis Child 84:328–331
Gotcheva V, Hristozova E, Hristozova T, Guo M, Roshkova Z, Angelov A (2002) Assessment of potential probiotic properties of lactic acid bacteria and yeast strains. Food Biotechnol 16:211–225
Gouy M, Guindon S, Gascuel O (2010) SeaView version 4: a multiplatform graphical user interface for sequence alignment and phylogenetic tree building. Mol Biol Evol 27:221–224
Harju S, Fedosyuk H, Peterson KR (2004) Rapid isolation of yeast genomic DNA: bust n’ Grab. BMC Biotechnol 4:8
Hatoum R, Labrie S, Fliss I (2012) Antimicrobial and probiotic properties of yeasts: from fundamental to novel applications. Front Microbiol 3:421
Kos B, Susković J, Vuković S, Simpraga M, Frece J, Matosić S (2003) Adhesion and aggregation ability of probiotic strain Lactobacillus acidophilus M92. J Appl Microbiol 94:981–987
Kumamoto CA (2011) Inflammation and gastrointestinal Candida colonization. Curr Opin Microbiol 14:386–391
Kumar A, Sharma PC (2013) In vitro studies on selective virulence traits of fluconazole resistant Candida species isolated from clinical cases. Int J Biol Pharm Res 4:685–696
Lu L, Walker WA (2001) Pathologic and physiologic interactions of bacteria with the gastrointestinal epithelium. Am J Clin Nutr 73:1124–1130
Lukaszewicz M (2012) Saccharomyces cerevisiae var. boulardii: probiotic yeast. In: Rigobelo EC (ed) Probiotics. In Tech, Rijeka, Croatia, pp 385–398
Mac Callum DM (2010) Candida infections and modelling disease. In: Ashbee HR, Bignell E (eds) Pathogenic yeasts, the yeast handbook. Springer, Heidelberg, pp 41–67
Mobili P, Gerbino E, Tymczyszyn EE, Gómez-Zavaglia A (2010) S-layers in lactobacilli: structural characteristics and putative role in surface and probiotic properties of whole bacteria. In: Méndez-Vilas A (ed) Current research, technology and education topics in applied microbiology and microbial biotechnology. Formatex Research Center, Badajoz, pp 1224–1234
Moris DV, Melhem MSC, Martins MA, Mendes RP (2008) Oral Candida spp. colonization in human immunodeficiency virus-infected individuals. J Venom Anim Toxins 14:224–257
Moslehi-Jenabian S, Lindegaard PL, Jespersen L (2010) Beneficial effects of probiotic and food borne yeasts on human health. Nutrients 2:449–473
O’Hara A, Shanahan F (2006) The gut flora as a forgotten organ. EMBO Rep 7:688–693
Ojetti V, Gigante G, Ainora ME, Fiore F, Barbaro F, Gasbarrini A (2009) Microflora imbalance and gastrointestinal diseases. Dig Liver Dis Suppl. 3:35–39
Papon N, Courdavault V, Clastre M, Bennett RJ (2013) Emerging and emerged pathogenic Candida species: beyond the Candida albicans paradigm. PLoS Pathog 9:e1003550
Parfrey LW, Walters WA, Knight R (2011) Microbial eukaryotes in the human microbiome: ecology, evolution, and future directions. Front Microbiol 2:153
Psomas E, Andrighetto C, Litopoulou-Tzanetaki E, Lombardi A, Tzanetakis N (2001) Some probiotic properties of yeast isolates from infant faeces and Feta cheese. Int J Food Microbiol 69:125–133
Rajilić-Stojanović M, Smidt H, de Vos WM (2009) Diversity of the human gastrointestinal tract microbiota revisited. Environ Microbiol 9:2125–2136
Rozkiewicz D, Daniluk T, Sciepuk M, Kurzqtkowska B, Ołdak E, Zaremba ML (2005) Prevalence of Candida albicans in stool of hospitalized children in 2003 with or without diarrhea from the Bialystok region. Przegl Epidemiol 59:43–51
Schoch CL, Seifert KA, Huhndorf S, Robert V, Spouge JL, Levesque CA, Chen W, Fungal Barcoding Consortium (2012) Nuclear ribosomal internal transcribed spacer (ITS) region as a universal DNA barcode marker for fungi. Proc Natl Acad Sci USA 109:6241–6246
Schulze J, Sonnenborn U (2009) Yeasts in the gut: from commensals to infectious agents. Dtsch Arztebl Int 106:837–842
Vazquez JA, Sobel JD (2011) Candidiasis. In: Kauffman CA, Pappas PG, Sobel JD, Dismukes WE (eds) Essentials of clinical mycology. Springer, New York, pp 167–206
Acknowledgments
The authors are indebted to Dr. Xavier Lepoutre (Victor Provo hospital at Roubaix, France) for assessment of antifungal susceptibility and to Dr. Delphine Caly (Lille 1 University, France) for critical reading and English improvement of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interests regarding the publication of this paper.
Additional information
Communicated by Olaf Kniemeyer.
Rights and permissions
About this article
Cite this article
Seddik, H.A., Ceugniez, A., Bendali, F. et al. Yeasts isolated from Algerian infants’s feces revealed a burden of Candida albicans species, non-albicans Candida species and Saccharomyces cerevisiae . Arch Microbiol 198, 71–81 (2016). https://doi.org/10.1007/s00203-015-1152-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00203-015-1152-x