Abstract
Summary
This matched case-control study compared the computed tomography (CT)-based regional bone density of patients with fragility fractures of the sacrum to a control without fracture. Patients with a sacral fracture demonstrated a significantly lower regional bone density of the sacrum, the sacral bone density not being correlated with the BMD by DXA of the spine.
Introduction
The aim of this study is to compare the computed tomography-based regional bone density measured by Hounsfield units (HUs) in patients with and without fragility fractures of the sacrum.
Methods
Patients aged ≥ 50 years with a fragility fracture of the sacrum were compared to patients of similar age and gender who had a fall from standing height without fracture (n = 46). A matched case-control analysis was conducted by retrospective chart review and assessment of areal bone mineral density by lumbar DXA and by volumetric regional HU measurements in uncalibrated CT scans of the sacrum.
Results
Patients with a sacral fracture (age 74 ± 11 years) showed a lower bone density in the body of S1 (HU 85 ± 22) when compared to the matched control group without fracture (age 73 ± 10 years, HU 125 ± 37, p < 0.001). The CT-based bone density of S1 did not correlate with the DXA values of the lumbar spine (r = 0.223, p = 0.136), and lumbar spine T-scores did not differ between the groups (− 2.0 ± 1.3 vs. − 1.9 ± 1.2, p = 0.786). All measurements are based on uncalibrated scans, and absolute HU values are restricted to scans made on Siemens SOMATOM Force or SOMATOM Edge scanners.
Conclusions
Patients with fragility fractures of the sacrum demonstrated a lower regional volumetric bone density of the sacrum when compared to a cohort without a fracture. Local sacral volumetric bone density as measured by CT seems to be independent from the areal BMD as measured by DXA of the lumbar spine.
Level of evidence: level III.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is frequent among the elderly population and is associated with an increased risk for fragility fractures [1, 2]. Fragility fractures can result in immobility-associated complications and death [1, 3, 4]. While vertebral fractures are the most common osteoporotic fractures, fragility fractures of the pelvis have increasingly come into focus as they may more directly affect a person’s ability to walk [5]. Morbidity and mortality rates after fragility fractures of the pelvis are comparable to those after hip fractures [6].
In order to avoid such fractures, it is important to identify individuals at risk. A key risk factor for sustaining a fragility fracture is impaired bone quality. The most accepted method for detecting osteopenia or osteoporosis by evaluating the areal bone mineral density (BMD) is dual-energy X-ray absorptiometry (DXA) of the hip or vertebra. The DXA T-score is correlated with fracture risk and can indicate progression or remission of osteoporosis [7, 8]. However, DXA of the hip or spine may not necessarily depict the bone quality of the pelvis.
In contrast to DXA, computer tomographs (CTs) are readily available for immediate diagnosis of pelvic fractures. Bone quality in the fracture region, in terms of volumetric bone density, can be estimated from Hounsfield unit (HU) measurements in routine diagnostic CT scans [7, 9,10,11]. Furthermore, a correlation of CT gray values in HU and biomechanical properties has been shown [1, 7, 9, 11, 12]. Using HU in combination with structural parameters as trabecular thickness, trabecular number, and ratio between bone total volume and trabecular volume may predict biomechanical properties even better [11]. The advantage of HU is that it can be measured with most of the standard picture archiving systems (PACS) available.
Silva et al. proposed that HU measurements can be used as a predictor for fracture patterns and failure loads [13]. Whereas the DXA is less widely available, CT scans have become a routine diagnostic tool in patients with fragility fractures of the pelvis or sacrum. Using CT-based HU measurements of the sacrum for the assessment of bone quality in these patients would have the advantage of no added costs, no additional radiation exposure, and immediate information about the local bone density of the fractured entity.
The hypothesis of this study was that the sacral bone density expressed in HU is lower in patients with fragility fractures of the pelvis than in normal controls.
The aim of the current study was to compare the bone density in HU with computed tomography in the fractured sacral alae of an elderly population compared to matched case controls.
Methods
Patients
The protocol of the present study was approved by the local ethics committee (Kantonale Ethik-Kommission Zürich, KEK-ZH-No. 2016-01758).
All 198 consecutive patients aged over 49 years managed for pelvic low-energy trauma at a university trauma center between January 2007 and October 20, 2016, and examined with both computed tomography (CT) of the pelvis and DXA of the spine were retrieved using institutional clinical information system (KISIM, Cistec AG, Zurich, Switzerland).
Only patients with an isolated fragility fracture of the pelvis with unilateral involvement of the sacrum who had CT and DXA scans within 18 months of the trauma were included (n = 34). A fragility fracture of the sacrum was defined as a cortical discontinuation secondary to an inadequate trauma (e.g., falling from standing height). Patients with only a unilateral fracture were included to allow for unbiased measurements at the contralateral, unfractured side of the sacrum.
Excluded were nine patients because of earlier documented sacral fracture (n = 2), out-of-hospital CT examination (n = 2), bone tumors or metastatic disease of the spine and pelvis (n = 0), spinal deformity or degenerative changes (n = 4), and inadequate scan technique (n = 3).
Twenty-three fracture patients were included into the final analysis and were matched by age and gender to a cohort of patients who had had a fall from standing height but no fracture of the pelvis and had a CT scan of the sacrum and a DXA of the spine within 18 months after the trauma. Matching was conducted by a data query from the institutional clinical information system and was possible for all 23 patients. By a retrospective electronic chart review, demographic data including weight and height as well as data regarding the patients’ smoking history, drinking behavior, rheumatic diseases, previously documented osteoporotic fragility fractures, and bisphosphonate and cortisone medications were collected (Table 1).
Imaging
DXA scan data, obtained for the first to the fourth lumbar vertebrae, included T-scores and areal BMD (measured in g/cm2) [7]. CT scans were performed on multiple-detector computed tomography (MDCT) units using standard protocol settings (see Table 2); raw data were reconstructed in axial images at 1.5-mm slice thickness and 1.5-mm increment using bone convolution kernel and field of view 340 × 340 with a matrix 512 × 512 (SOMATOM Force or SOMATOM Edge, Siemens Healthineers, Munich, Germany). The scanners were calibrated regularly by the use of a phantom.
Hounsfield unit measurements
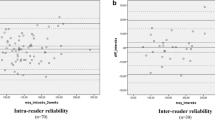
Volumetric bone density expressed in HU was done in the corpus of S1, S2, and L5 and in the alae of S1 in CT scans of the pelvis. The multi-planar reformats (MPR) tool of the picture archiving system (Impax, AGFA HealthCare, Mortsel, Belgium) was used to measure the HU values for the different sites. To standardize measurements, while taking normal anatomic variation into consideration, the midbody location of S1, S2, and L5, as well as the midpoint of the S1 alae, was defined by two cross-reference lines in each of the axial, sagittal, and coronal planes [12]. In the sagittal plane, the reference lines were drawn parallel to the tangent of the inferior and of the superior vertebral plates as well as the most dorsal and ventral points of the sacral and lumbar bodies (Fig. 1). In the axial plane, the reference lines were drawn through the midpoints of the spinal process and parallel to the tangent of the most anterior point of the sacral and lumbar bodies. In the coronal plane, the reference lines were drawn through the midpoints of the sacrum as well as, for measuring the alae, through the midpoints of the sacral foramina and parallel to the tangent of the most anterior points of the sacral body as well as the most anterior points of the alae.
For each point of interest, the largest possible circular region of interest (ROI) was placed, excluding the adjacent cortical bone to reduce the potential of distorting the average medullary volume (Fig. 1) [7]. Similar to the study of Schreiber et al., initial tests displayed no significant difference between mean values of multiple small, round ROIs versus a single maximally sized circular ROI [7]. In the fracture group, only the ala contralateral to the fracture was measured, in which values for both alaes were averaged in the control group. All measurements were performed in triplicate and averaged. For each sacral or lumbar body, the axial and sagittal ROIs were averaged.
Statistical analysis
A matched case-control analysis was conducted (N = 23 per group; N total = 46).
The primary outcome was the CT-based bone density of the body of S1 measured in HU. Prior to data acquisition, a sample size calculation was performed with a desired two-tailed type I error of 0.05 and a power of 0.90. Based on literature data, a relevant difference was considered to be 30 HU with an expected standard deviation of 40 HU [7]. This revealed a minimum sample size of 19 per group, which in the current study is exceeded by the 23 matched pairs with 46 patients included in total [14].
Further statistical analysis was done by the use of SPSS for Windows 23.0 (SPSS, Chicago, Illinois, USA). Data are presented as frequencies (n) and means with the standard deviation (SD). Case matching of patients was performed based on age (± 5 years), gender, and trauma (fall from standing height).
To assess differences between the two matched groups, a paired-sample t test was used for the normally distributed continuous data and McNemar’s test for categorical data. [15] Correlations between continuous data sets were tested using the Pearson’s correlation coefficient. The level of statistical significance was set at p ≤ 0.05.
Results
Forty-six female patients with a mean age of 73.1 years (SD 10.4 years) were analyzed in this matched case-control study.
In the current study, the body of S1 showed the highest CT-based bone density (HU 105, SD 36) when compared to the body of S2 (HU 43, SD 46; ANOVA, p < 0.001), the sacral alae at the level of S1 (HU 0, SD 36; ANOVA, p < 0.001), and the body of L5 (HU 82, SD 36; ANOVA, p = 0.029; Fig. 2). The sacral alae had the lowest bone density of all measured regions (ANOVA, p < 0.001).
Patients with a sacral fracture (mean age 74 years, SD 11 years) showed a significantly lower average bone density in the corpus of S1 (HU 85, SD 22, Fig. 3) when compared to the matched control group without fracture (mean age 73 years, SD 10 years, all female; HU 125, SD 37, paired-sample t test, p < 0.001). In line with this, the alae of the fracture group had a significantly lower bone density when compared to the control (HU − 22, SD 29 vs. HU 23, SD 28; paired-sample t test, p < 0.001; Fig. 3).
The lumbar spine T-scores did not differ between the groups (− 2.0, SD 1.3 vs. − 1.9, SD 1.2, paired-sample t test, p = 0.786).
The whole-population T-score measured at the lumbar spine (total mean − 2.0, SD 1.2) did correlate with the CT-based bone density of neither S1 (HU 104, SD 36, Pearson’s r = 0.223, p = 0.136) nor L5 (HU 81, SD 36, Pearson’s r = 0.196, p = 0.198).
In this very homogeneous group of matched elderly female patients, both the lumbar T-score (Pearson’s r = − 0.185, p = 0.217) and the CT-based bone density measured in HU in S1 (Pearson’s r = − 0.182, p = 0.227) did not correlate with age (total mean 73 years, SD 10 years; Fig. 4).
Discussion
This study aimed to compare the bone density in HU with computed tomography in the fractured sacral alae of an elderly population compared to matched case controls.
It was our hypothesis that the sacral bone density expressed in HU is lower in patients with fragility fractures of the pelvis than in normal controls.
In this study, individuals with a sacral fracture had a significantly lower average bone density in the body of S1 when compared to the matched control group without fracture. The fracture cohort showed a significantly lower bone density in the first sacral segment and the alae of S1. In the regional analysis, the sacral alae had the lowest bone density of all measured regions; this was especially prominent in the alae of the fracture group.
In line with previously published studies, the body of S1 showed the highest and the sacral alae showed the lowest CT-based bone density compared to the other measured sites in this study [12, 16]. This is consistent with data by Peretz et al. who identified a so-called alar void in the sacral ala at S1, representing a zone with a lower bone thickness compared to the S1 vertebral body [1, 16, 17]. It has previously been proposed that fragility fractures of the sacrum are typically located in this paraforaminal region. [16, 18]
The HU-determined bone density of the sacrum did not correlate with the lumbar DXA values. This is in line with literature, where only weak correlations between the two values have been found [19,20,21]. Local sacral volumetric bone density seems to be independent of the areal BMD as measured by DXA of the lumbar spine. Our findings indicate that HU measurements of the sacrum may have a higher sensitivity than DXA T-scores as a determinant of the pelvic fragility fracture risk.
The limitations of this study are inherent with its retrospective study design. Thus, the relationship between the occurrence of a sacral fracture and low HU values of the sacrum may not be proven to be causal due to potential confounders not accounted for by the study design. However, it was sought to compensate for this by adhering to a strict matched case-control design following an a priori sample size calculation. All patients included into analysis happened to be female. This may be a potential bias or simply represent the reality when dealing with elderly patients with fragility fractures of the pelvis. Of notice, the sample of this study was not powered to investigate differences in DXA scans and thus, one cannot safely exclude that differences in DXA values exist in patients with versus without pelvic fractures.
The key primary outcome variable of this study was HU values. All measurements were repeated three times, but even sequential measurements of radiographic parameters are always highly dependent on the quality of the CT scans. The scans were taken by the use of last-generation CT scanners of a single company. This has the advantage of a higher between-scanner reliability of the data, but the results may be less comparable across CT scans acquired by the use of CT scanners from other manufacturers or of older generation [22].
As we were looking for a parameter that clinicians could measure using their standard PACS, the CT-based HU measurements were performed without using comparative phantoms. Uncalibrated CT scans cannot be seen as a replacement of DXA or quantitative CT [23]. The CT scanners used for this study were calibrated by the use of phantoms on a regular basis and were performed with automatic exposure control, which aims to adjust the tube current on the basis of the amount of attenuation detected, accounting for the patient’s body habitus [7]. However, these automatic exposure protocols are highly dependent on the manufacturer of the CT scanner and there exist differences in HU/BMD conversion of up to 20% [22]. Therefore, the results of this study cannot be directly compared to other studies but need to be set in context of these variabilities (Appendix 1).
In summary, HU values may not be an ideal tool for assessing absolute bone mineral density. However, the results of this matched case-control analysis in combination with the findings of other studies [7, 19, 24] suggest that HU measurements could be used for an earlier identification of patients at risk for fragility fractures of the pelvis—even in the presence of a normal DXA T-score. A lack of general osteopenia in the lumbar spine, as measured in this study by DXA and local HU values of L5, does not necessarily preclude the presence of a noticeable local osteoporosis of the sacrum. In this manner, the HU value may be used as a guide for performing supplementary investigations, such as DXA scans or blood tests, for metabolic bone disease [7].
HU values may even prove to be a prognostic factor of implant stability [25,26,27,28] and serve in the decision-making for or against cement augmentation of sacral screw fixation [29].
It has to be clear, though, that uncalibrated CT scans such as those used in this study cannot replace a standardized assessment of bone mineral density (e.g., by DEXA or QCT). Future studies may further investigate the predictive power of CT-based bone density measurements and—in a further step—may implement algorithms based on HU threshold values. Yet, while HU normative values are available for other regions of the skeleton [30, 31], further investigations will be needed to generate reference values for the spine and the sacrum.
Conclusion
In a matched analysis (age/gender/injury severity), patients with fragility fractures of the pelvis demonstrated lower general and regional bone densities of the sacrum when compared with a cohort without a fracture. This difference was especially pertinent in the comparison of the alae of the S1 level. Local sacral volumetric bone density seems to be independent from the areal BMD as measured by DXA of the lumbar spine. CT-based evaluation of the local bone density may serve as a predictive marker for the elderly patient’s risk of sustaining a fragility fracture of the pelvis.
References
Wagner D, Kamer L, Sawaguchi T, Richards RG, Noser H, Rommens PM (2016) Sacral bone mass distribution assessed by averaged three-dimensional CT models: implications for pathogenesis and treatment of fragility fractures of the sacrum. J Bone Joint Surg Am 98(7):584–590. https://doi.org/10.2106/JBJS.15.00726
Gauthier A, Kanis JA, Jiang Y, Martin M, Compston JE, Borgstrom F, Cooper C, McCloskey EV (2011) Epidemiological burden of postmenopausal osteoporosis in the UK from 2010 to 2021: estimations from a disease model. Arch Osteoporos 6(1-2):179–188. https://doi.org/10.1007/s11657-011-0063-y
Babayev M, Lachmann E, Nagler W (2000) The controversy surrounding sacral insufficiency fractures: to ambulate or not to ambulate? Am J Phys Med Rehabil 79(4):404–409. https://doi.org/10.1097/00002060-200007000-00014
Mears SC, Berry DJ (2011) Outcomes of displaced and nondisplaced pelvic and sacral fractures in elderly adults. J Am Geriatr Soc 59(7):1309–1312. https://doi.org/10.1111/j.1532-5415.2011.03455.x
Johnell O, Kanis JA (2006) An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 17(12):1726–1733. https://doi.org/10.1007/s00198-006-0172-4
Taillandier J, Langue F, Alemanni M, Taillandier-Heriche E (2003) Mortality and functional outcomes of pelvic insufficiency fractures in older patients. Joint Bone Spine 70(4):287–289. https://doi.org/10.1016/S1297-319X(03)00015-0
Schreiber JJ, Anderson PA, Rosas HG, Buchholz AL, AG A (2011) Hounsfield units for assessing bone mineral density and strength: a tool for osteoporosis management. J Bone Joint Surg Am 93(11):1057–1063. https://doi.org/10.2106/JBJS.J.00160
Marshall D, Johnell O, Wedel H (1996) Meta-analysis of how well measures of bone mineral density predict occurrence of osteoporotic fractures. BMJ 312(7041):1254–1259. https://doi.org/10.1136/bmj.312.7041.1254
Baum T, Carballido-Gamio J, Huber MB, Müller D, Monetti R, Räth C, Eckstein F, Lochmüller EM, Majumdar S, Rummeny EJ, Link TM, Bauer JS (2010) Automated 3D trabecular bone structure analysis of the proximal femur—prediction of biomechanical strength by CT and DXA. Osteoporos Int 21(9):1553–1564. https://doi.org/10.1007/s00198-009-1090-z
Marinova M, Edon B, Wolter K, Katsimbari B, Schild HH, Strunk HM (2015) Use of routine thoracic and abdominal computed tomography scans for assessing bone mineral density and detecting osteoporosis. Curr Med Res Opin 31(10):1871–1881. https://doi.org/10.1185/03007995.2015.1074892
Teo JC, Si-Hoe KM, Keh JE, Teoh SH (2006) Relationship between CT intensity, micro-architecture and mechanical properties of porcine vertebral cancellous bone. Clin Biomech (Bristol, Avon) 21(3):235–244. https://doi.org/10.1016/j.clinbiomech.2005.11.001
Salazar D, Lannon S, Pasternak O, Schiff A, Lomasney L, Mitchell E, Stover M (2015) Investigation of bone quality of the first and second sacral segments amongst trauma patients: concerns about iliosacral screw fixation. J Orthop Traumatol 16:301–308
Silva MJ, Keaveny TM, Hayes WC (1998) Computed tomography-based finite element analysis predicts failure loads and fracture patterns for vertebral sections. J Orthop Res 16(3):300–308. https://doi.org/10.1002/jor.1100160305
Rosner B (1995) Fundamentals of biostatistics, 4th edn. Duxbury Press
Breslow NE, Day NE (1980) Statistical methods in cancer research. Volume I—the analysis of case-control studies. IARC Sci Publ (32):5–338
Wagner D, Kamer L, Rommens PM, Sawaguchi T, Richards RG, Noser H (2014) 3D statistical modeling techniques to investigate the anatomy of the sacrum, its bone mass distribution, and the trans-sacral corridors. J Orthop Res 32(11):1543–1548. https://doi.org/10.1002/jor.22667
Peretz AM, Hipp JA, Heggeness MH (1998) The internal bony architecture of the sacrum. Spine (Phila Pa 1976) 23(9):971–974. https://doi.org/10.1097/00007632-199805010-00001
Linstrom NJ, Heiserman JE, Kortman KE, Crawford NR, Baek S, Anderson RL, Pitt AM, Karis JP, Ross JS, Lekovic GP, Dean BL (2009) Anatomical and biomechanical analyses of the unique and consistent locations of sacral insufficiency fractures. Spine (Phila Pa 1976) 34(4):309–315. https://doi.org/10.1097/BRS.0b013e318191ea01
Alacreu E, Moratal D, Arana E (2017) Opportunistic screening for osteoporosis by routine CT in Southern Europe. Osteoporos Int 28(3):983–990. https://doi.org/10.1007/s00198-016-3804-3
Burke CJ, Didolkar MM, Barnhart HX, Vinson EN (2016) The use of routine non density calibrated clinical computed tomography data as a potentially useful screening tool for identifying patients with osteoporosis. Clin Cases Miner Bone Metab 13(2):135–140. 10.11138/ccmbm/2016.13.2.135
Lee SJ, Binkley N, Lubner MG, Bruce RJ, Ziemlewicz TJ, Pickhardt PJ (2016) Opportunistic screening for osteoporosis using the sagittal reconstruction from routine abdominal CT for combined assessment of vertebral fractures and density. Osteoporos Int 27(3):1131–1136. https://doi.org/10.1007/s00198-015-3318-4
Engelke K (2017) Quantitative computed tomography—current status and new developments. J Clin Densitom 20(3):309–321. https://doi.org/10.1016/j.jocd.2017.06.017
Engelke K, Libanati C, Fuerst T, Zysset P, Genant HK (2013) Advanced CT based in vivo methods for the assessment of bone density, structure, and strength. Curr Osteoporos Rep 11(3):246–255. https://doi.org/10.1007/s11914-013-0147-2
Emohare O, Wiggin M, Hemmati P, Switzer J (2015) Assessing bone mineral density following acute hip fractures: the role of computed tomography attenuation. Geriatr Orthop Surg Rehabil 6(1):16–21. https://doi.org/10.1177/2151458514560215
Turkyilmaz I, Aksoy U, McGlumphy EA (2008) Two alternative surgical techniques for enhancing primary implant stability in the posterior maxilla: a clinical study including bone density, insertion torque, and resonance frequency analysis data. Clin Implant Dent Relat Res 10(4):231–237. https://doi.org/10.1111/j.1708-8208.2008.00084.x
Turkyilmaz I, Sennerby L, McGlumphy EA, Tozum TF (2009) Biomechanical aspects of primary implant stability: a human cadaver study. Clin Implant Dent Relat Res 11(2):113–119. https://doi.org/10.1111/j.1708-8208.2008.00097.x
Turkyilmaz I, Tumer C, Ozbek EN, Tozum TF (2007) Relations between the bone density values from computerized tomography, and implant stability parameters: a clinical study of 230 regular platform implants. J Clin Periodontol 34(8):716–722. https://doi.org/10.1111/j.1600-051X.2007.01112.x
Lund T, Oxland TR, Jost B, Cripton P, Grassmann S, Etter C, Nolte LP (1998) Interbody cage stabilisation in the lumbar spine: biomechanical evaluation of cage design, posterior instrumentation and bone density. J Bone Joint Surg Br 80(2):351–359. https://doi.org/10.1302/0301-620X.80B2.7693
Osterhoff G, Dodd AE, Unno F, Wong A, Amiri S, Lefaivre KA, Guy P (2016) Cement augmentation in sacroiliac screw fixation offers modest biomechanical advantages in a cadaver model. Clin Orthop Relat Res 474(11):2522–2530. https://doi.org/10.1007/s11999-016-4934-9
Shapurian T, Damoulis PD, Reiser GM, Griffin TJ, Rand WM (2006) Quantitative evaluation of bone density using the Hounsfield index. Int J Oral Maxillofac Implants 21(2):290–297
Turkyilmaz I, Ozan O, Yilmaz B, Ersoy AE (2008) Determination of bone quality of 372 implant recipient sites using Hounsfield unit from computerized tomography: a clinical study. Clin Implant Dent Relat Res 10(4):238–244. https://doi.org/10.1111/j.1708-8208.2008.00085.x
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The protocol of the present study was approved by the local ethics committee (Kantonale Ethik-Kommission Zürich, KEK-ZH-Nr. 2016–01758).
Conflicts of interest
None.
Electronic supplementary material
ESM 1
(DOCX 191 kb)
Rights and permissions
About this article
Cite this article
Schönenberg, D., Guggenberger, R., Frey, D. et al. CT-based evaluation of volumetric bone density in fragility fractures of the pelvis—a matched case-control analysis. Osteoporos Int 29, 459–465 (2018). https://doi.org/10.1007/s00198-017-4307-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-017-4307-6