Abstract
Summary
We conducted a systematic review of randomized controlled trials (RCTs) of bisphosphonates for the prevention of osteopenia in kidney-transplant recipients. Bisphosphonates improved bone mineral density at the lumbar spine and femoral neck after 12 months. However, additional well-designed RCTs are required to determine the optimal treatment strategy.
Osteopenic–osteoporotic syndrome is a bone complication of renal transplantation. Bisphosphonates, calcitonin, and vitamin D analogs may be used to prevent or treat osteoporosis or bone loss after renal transplantation. However, there is currently no widely recognized strategy for the prevention of corticosteroid-induced osteoporosis. This study aims to assess the available evidence to guide the targeted use of bisphosphonates for reducing osteoporosis and bone loss in renal-transplant recipients. We searched the Cochrane Central Register of Controlled Trials, PubMed, and EMBASE for randomized controlled trials of bisphosphonates for osteoporosis or bone loss after renal transplantation. A total of 352 abstracts were identified, of which 55 were considered for evaluation and 9 were included in the final analysis. The primary outcome measure was change in the bone mineral density (BMD) of the lumbar spine and femoral neck after 12 months. Data extraction was performed independently by two investigators. BMD at the lumbar spine was improved after treatment with bisphosphonates [9 trials; 418 patients; weighted mean difference (WMD), 0.61; 95 % confidence interval (CI), 0.16–1.06]. Eight trials (406 patients) that reported changes in BMD at the femoral neck also showed improved outcomes after treatment with bisphosphonates (WMD, 0.06; 95 % CI, 0.03–0.09). Bisphosphonates improve BMD at the lumbar spine and femoral neck after 12 months in renal-transplant recipients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Successful renal transplantation corrects many metabolic abnormalities associated with the development of renal osteodystrophy. However, osteopenia and osteoporosis remain prevalent, even in patients with well-functioning grafts. Increasing attention has focused on preventing late complications of transplantation and on patient quality of life by addressing factors affecting long-term morbidity, such as cardiovascular risk, post-transplantation diabetes mellitus, cancer, and bone disease [1–3].
Osteopenic–osteoporotic syndrome is a bone complication of renal transplantation. Although renal transplantation corrects abnormalities of calcium and phosphorus metabolism in patients with uremia, it may result in disturbances to bone metabolism, such as osteopenia, caused by treatment with glucocorticoids and cyclosporine. However, there is currently no widely recognized strategy for the prevention of corticosteroid-induced osteoporosis.
Bone mineral density (BMD) in the lumbar spine decreases by 5 % during the first year after engraftment [4], and longitudinal studies of stable renal-transplant recipients revealed an annual bone loss of 1.7 % in the lumbar spine [5]. Mineral and bone disorders are common following kidney transplantation and are characterized by loss of bone volume and mineralization abnormalities that may lead to low bone turnover [6].
BMD can be reduced by 6.8 and 8.8 % at 6 and 18 months, respectively, after successful renal transplantation [7]. Pre-existing osteopenia may deteriorate in kidney-graft recipients as a result of immunosuppressive therapy with calcineurin inhibitors [8] or corticosteroids [9]. Furthermore, immunosuppressive agents used in solid-organ transplantation can exert various effects on bone metabolism [10]. Changes in fracture rate and BMD are associated with secondary osteoporosis, though not as strongly as with primary osteoporosis.
Bisphosphonates such as pamidronate and ibandronate can prevent bone loss during the first year post-transplantation [11, 12]. Pamidronate is easy to administer and well-tolerated with no any serious adverse effects, and a recent meta-analysis suggested that it had a beneficial effect on bone loss, with no correlation with renal toxicity during the first year after renal transplantation [13].
In this review, we aimed to identify a rationale for the use of bisphosphonates for the prevention or treatment of osteoporosis or bone loss after renal transplantation.
Methods
Inclusion criteria
We conducted a review of randomized controlled trials (RCTs) that used bisphosphonates to treat osteopenia or osteoporosis in renal-transplant recipients. Trials that met the following criteria were included: (1) full-text original articles, (2) administration of bisphosphonates by any route (oral and parenteral), (3) intervention for the treatment of osteopenia or osteoporosis before or after transplantation, and (4) follow-up of patients for >12 months.
Trials involving transplantations other than renal transplantation, including kidney–pancreas transplants, were excluded. Trials that did not involve dual-energy X-ray absorptiometry (DXA) were also excluded. Trials including mixed populations were only included when data for patients receiving a kidney transplant were provided in the publication or were received from the authors on request.
Search strategy
Electronic searches were performed in PubMed (1966 to May 2014), EMBASE (1980 to May 2014), and the Cochrane Central Register of Controlled Trials using optimally sensitive search strategies for the identification of RCTs. We searched for the following medical subject headings and text words: kidney transplantation, osteopenia, osteoporosis, and RCT. The titles and abstracts of the identified studies were analyzed by two of the authors (JW and JHX) in consultation with a third author (XJC), according to the inclusion criteria. The reference lists of the identified articles were also searched. Trials reported in any language were considered.
Data extraction and quality assessment
Each trial was assessed by two independent authors (JW and JHX) who extracted data on study-sample characteristics, agent type and route of administration, trial method, and outcomes. The primary outcome measure was changes in BMD of the lumbar spine and femoral neck after 12 months. The risk of bias in the included RCTs was assessed using the risk of bias assessment tool from the Cochrane Collaboration [14]. Selection bias, performance bias, detection bias, attribution bias, and other biases in the included RCTs were assessed. Differences in and difficulties with data extraction were resolved by discussion among the authors. In the event of missing or incomplete data, the trial investigators were contacted for clarification. Three reviewers (JW, MY, JHX) independently assessed the qualities of the included studies and differences were resolved by discussion.
For trials reporting pre- and post-intervention values, mean changes were obtained by subtracting the pre-intervention from the post-intervention values and standard deviations were estimated using the following formula:
in which the correlation between the pre- and post-intervention values (r pre,post) was assumed to be 0.5.
Statistical analysis
Bisphosphonates, calcitonin, and vitamin D analogs were compared with controls according to the recommendations of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses [15]. Heterogeneity of treatment effects among the studies was tested using Q (heterogeneity χ 2) and I 2 statistics [16]. Values of P < 0.10 and I 2 > 50 % were considered to indicate significant heterogeneity. Random-effect models were used when heterogeneity was present; otherwise, fixed-effect models were used. Summary estimators of treatment effects were calculated using relative risk or weighted mean difference (WMD) and 95 % confidence intervals (CI), as appropriate. Data were represented graphically using Forest plots. The main analysis was conducted using the random-effects model, as described by Der-Simonian and Laird [17]. Direct comparisons were performed using RevMan statistical software, version 5.1 (Nordic Cochrane Center) [18].
Results
Description of studies
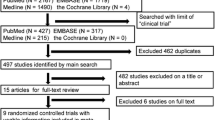
The search strategy retrieved 352 potentially relevant records (Fig. 1), comprising 163 trials from PubMed, 121 from EMBASE, 65 from the Cochrane Central Register of Controlled Trials, and three from manual searches. Overall, 111 records were excluded by screening the titles and abstracts. The remaining 55 full-text articles were retrieved for additional scrutiny, among which 46 were ineligible because of nonuse of DXA, lack of primary outcome, unrelated to treatment for osteoporosis, or lack of full text. Nine RCTs met the eligibility criteria [11, 12, 19–25], all of which used bisphosphonates in relation to osteoporosis, included DXA examinations, and involved changes in BMD after 12 months as an outcome. The characteristics of the included RCTs are summarized in Table 1.
Methodological quality of RCTs
Figure 2 shows a graphical summary of the risk of bias assessments of the included studies based on the risk of bias domains. Based on the Cochrane criteria, three of the nine studies had low risks of selection bias, detection bias, and performance bias [11, 23, 24]. High risks of bias were identified as failure to describe or use appropriate allocation concealment (5/9) and lack of effective blinding procedures (observer, 6/9; patient, 5/9). Four studies [12, 20, 21, 25] included groups with equal distributions of clinical conditions. None of the studies had equal age and sex distributions. Four trials [11, 19, 21, 25] did not mention patient dropouts.
Bisphosphonates versus placebo or no treatment
Changes in lumbar spine BMD were reported in all nine trials, and improved after treatment with bisphosphonates (418 patients; WMD, 0.61; 95 % CI, 0.16–1.06), especially pamidronate. Eight trials (406 patients) also reported improved BMD at the femoral neck after treatment with bisphosphonates (WMD, 0.06; 95 % CI, 0.03–0.09), especially alendronate (Figs. 3 and 4). Levels of parathyroid hormone (PTH) were decreased in both the bisphosphonate-treated and placebo/untreated groups [11, 12, 21, 22, 24], with no significant difference between the two groups (WMD, 0.17; 95 % CI, −0.19–0.53). Four studies reported fracture rates [12, 22–24], but the positive effect of ibandronate on BMD was not accompanied by a reduction in fracture rate within the 12-month period [12, 24].
Discussion
This meta-analysis demonstrated that treatment with bisphosphonates had a beneficial effect on changes in BMD at both the lumbar spine and femoral neck. Current European Best Practice Guidelines recommend bisphosphonate treatment in potentially high-risk groups, including patients with pre-existing fractures and severe osteoporosis, patients with diabetes, recipients of kidney and pancreas transplants, and postmenopausal women [26]. Similarly, the Kidney Disease Outcomes Quality Initiative recommends limiting glucocorticoid therapy and measuring BMD at regular intervals to assess the presence or development of osteoporosis [27], and treatment with a parenteral bisphosphonate in the event of a BMD T-score <−2 standard deviations. The findings of the present study support the recommendation that bisphosphonates should be considered to improve BMD after renal transplantation. However, the trials demonstrated broad heterogeneity in terms of bisphosphonate use, with four studies using parenteral pamidronate, three using oral alendronate (5 and 10 mg), and two using intravenous injection of ibandronate.
Although treatment with bisphosphonates for 12 months is recommended when osteopenia is diagnosed, some studies [4, 19] also observed the effects after 6 months. However, although these results indicated non-inferior and effective changes in BMD of the lumbar spine and femoral neck with bisphosphonate treatment, their use for 6 months was less effective, and the 6-month results were therefore not analyzed in the current meta-analysis. The majority of RCTs recorded the outcomes after 12 months of treatment. However, long-term treatment is required after renal transplantation, and the timings of the BMD scans after transplantation varied from 6 months to several years after surgery.
A previous meta-analysis [28] reviewed interventions for the prevention of bone disease in renal-transplant recipients with a focus on osteoporotic fractures and other bone diseases, and concluded that bisphosphonates and vitamin D had beneficial effects on BMD at the lumbar spine and femoral neck [29]. Although the articles included in this previous meta-analysis were published over 10 years [28], to the best of our knowledge, there has been no significant increase in the quality or quantity of relevant RCTs for the interventional effects of bisphosphonates on osteoporosis after renal transplantation, and no large-scale studies are currently registered with clinicaltrials.gov.
This review had several limitations. Fracture rate or fracture risk is the main consequence of osteoporosis, and efforts have been made to estimate these rather than relying solely on measurements of BMD. However, we were unable to draw any conclusions regarding these, because only four of the included studies evaluated the fracture rate [12, 22–24].
DXA provides no specific information on bone turnover, and BMD results should thus be interpreted together with clinical findings and bone-turnover biomarkers. The important biomarker PTH can exacerbate low bone turnover in renal-transplant recipients. Although PTH levels were decreased after renal transplantation in five studies [11, 12, 21, 22, 24], there was no significant difference between patients with and without bisphosphonate treatment, implying that bisphosphonates may not aggravate pre-existing hyperparathyroidism. Bone biopsies are required to demonstrate the course of events, but this is an invasive procedure and the subsequent analysis is time-consuming [30, 31]. However, bone-biopsy findings could help clinicians to decide on an appropriate therapeutic strategy and should thus be performed in patients with chronic kidney disease.
The patient populations varied among the included studies. Some trials excluded women to eliminate the confounding effects of menopausal status on outcomes, while other trials included both sexes. Only one trial clearly described the proportion of postmenopausal women, and the impact of this variable is thus unclear. The age distributions within the populations were also large, ranging from 20 to 70 years, which represented an important confounding factor. Furthermore, the small sample sizes in most studies (apart from one) reduced the strength of the conclusions that could be drawn from the data.
It was difficult to assess the included RCTs because of the omission of detailed information on the methods used in the trials. Most reports failed to include information on the method of allocation concealment, whether or not the outcome assessors were blinded, and whether an intention-to-treat analysis was used.
The current included trials also enrolled recipients from 0 to 24 months after transplantation. Future trials should consider randomizing enrollment before surgery and commencing interventions after graft function has been established [28].
Conclusions
This systematic review confirmed that treatment with bisphosphonates before and after renal transplantation had a favorable effect on BMD, with bisphosphonates, such as pamidronate and alendronate, being preferable to other treatments. Furthermore, the analyzed RCTs had small sample sizes, were of relatively poor quality, and had short follow-up periods, indicating the need for additional, well-designed RCTs to establish evidence-based recommendations regarding dosages, monitoring of interventions, adverse effects, and standardization of follow-up for BMD, to determine the optimal treatment for renal-transplant patients.
References
Glicklich D, Vohra P (2014) Cardiovascular risk assessment before and after kidney transplantation. Cardiol Rev 22:153–162
Lane JT, Dagogo-Jack S (2011) Approach to the patient with new-onset diabetes after transplant (NODAT). J Clin Endocrinol Metab 96:3289–3297
Wong G, Chapman JR, Craig JC (2014) Death from cancer: a sobering truth for patients with kidney transplants. Kidney Int 85:1262–1264
Torregrosa JV, Moreno A, Gutierrez A, Vidal S, Oppenheimer (2003) Alendronate for treatment of renal transplant patients with osteoporosis. Transplant Proc 35:1393–1395
Pichette V, Bonnardeaux A, Prudhomme L, Gagne M, Cardinal J, Ouimet D (1996) Long-term bone loss on kidney transplant recipients: a cross-sectional and longitudinal study. Am J Kidney Dis 28:105–114
Kalantar-Zadeh K, Molnar MZ, Kovesdy CP, Mucsi I, Bunnapradist S (2012) Management of mineral and bone disorder after kidney transplantation. Curr Opin Nephrol Hypertens 21:389–403
Julian BA, Laskow DA, Dubovsky J, Dubovsky EV, Curtis JJ, Quarles LD (1991) Rapid loss of vertebral mineral density after renal transplantation. N Engl J Med 325:544–550
Movsowitz C, Schlosberg M, Epstein S, Ismail F, Fallon M, Thomas S (1990) Combined treatment with cyclosporin A and cortisone acetate minimizes the adverse bone effects of either agent alone. J Orthop Res 8:635–641
Nishimura J, Ikuyama S (2000) Glucocorticoid-induced osteoporosis: pathogenesis and management. J Bone Miner Metab 18:350–352
Torres A, Lorenzo V, Salido E (2002) Calcium metabolism and skeletal problems after transplantation. J Am Soc Nephrol 13:551–558
Fan SL, Almond MK, Ball E, Evans K, Cunningham J (2000) Pamidronate therapy as prevention of bone loss following renal transplantation. Kidney Int 57:684–690
Grotz W, Nagel C, Poeschel D, Cybulla M, Petersen KG, Uhl M, Strey C, Kirste G, Olschewski M, Reichelt A, Rump LC, Poeschel D (2001) Effect of ibandronate on bone loss and renal function after kidney transplantation. J Am Soc Nephrol 12:1530–1537
Wang Z, Han Z, Tao J, Lu P, Liu X, Wang J, Wu B, Huang Z, Yin C, Tan R, Gu M (2014) Clinical efficacy and safety of pamidronate therapy on bone mass density in early post-renal transplant period: a meta-analysis of randomized controlled trials. PLoS One 9:e108106
Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA (2011) Cochrane Bias Methods Group; Cochrane Statistical Methods Group. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339:b2700
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560
Der Simonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177–188
The Nordic Cochrane Centre (2011) The Cochrane Collaboration. Review manager (RevMan) [computer program]. Version 5.1; Copenhagen
Nam JH, Moon JI, Chung SS, Kim SI, Park KI, Song YD, Kim KR, Lee HC, Huh K, Lim SK (2000) Pamidronate and calcitriol trial for the prevention of early bone loss after renal transplantation. Transplant Proc 32:1876
Koc M, Tuglular S, Arikan H, Ozener C, Akoglu E (2002) Alendronate increases bone mineral density in long-term renal transplant recipients. Transplant Proc 34:2111–2113
El-Agroudy AE, El-Husseini AA, El-Sayed M, Mohsen T, Ghoneim MA (2005) A prospective randomized study for prevention of postrenal transplantation bone loss. Kidney Int 67:2039–2045
Walsh SB, Altmann P, Pattison J, Wilkie M, Yaqoob MM, Dudley C, Cockwell P, Sweny P, Banks LM, Hall-Craggs M, Noonan K, Andrews C, Cunningham J (2009) Effect of pamidronate on bone loss after kidney transplantation: a randomized trial. Am J Kidney Dis 53:856–865
Torregrosa JV, Fuster D, Monegal A, Gentil MA, Bravo J, Guirado L, Muxí A, Cubero J (2011) Efficacy of low doses of pamidronate in osteopenic patients administered in the early post-renal transplant. Osteoporos Int 22:281–287
Smerud KT, Dolgos S, Olsen IC, Åsberg A, Sagedal S, Reisæter AV, Midtvedt K, Pfeffer P, Ueland T, Godang K, Bollerslev J, Hartmann A (2012) A 1-year randomized, double-blind, placebo-controlled study of intravenous ibandronate on bone loss following renal transplantation. Am J Transplant 12:3316–3325
Okamoto M, Yamanaka S, Yoshimoto W, Shigematsu T (2014) Alendronate as an effective treatment for bone loss and vascular calcification in kidney transplant recipients. J Transplant 2014:269613
EBPG Expert Group on Renal Transplantation (2002) European best practice guidelines for renal transplantation. Section IV: long-term management of the transplant recipient. Nephrol Dial Transplant 17(Suppl 4):1–67
National Kidney Foundation (2003) K/DOQI clinical practice guideline for bone metabolism and disease in chronic kidney disease. Am J Kidney Dis 42:S1–S201
Palmer SC, Strippoli GF, McGregor DO (2005) Interventions for preventing bone disease in kidney transplant recipients: a systematic review of randomized controlled trials. Am J Kidney Dis 45:638–649
Veenstra DL, Best JH, Hornberger J, Sullivan SD, Hricik DE (1999) Incidence and long-term cost of steroid-related side effects after renal transplantation. Am J Kidney Dis 33:829–839
Yamaguchi T, Kanno E, Tsubota J, Shiomi T, Nakai M, Hattori S (1996) Retrospective study on the usefulness of radius and with fractures from those without fractures. Bone 19:549–555
Lobão R, Carvalho AB, Cuppari L, Ventura R, Lazaretti-Castro M, Jorgetti V, Vieira JG, Cendoroglo M, Draibe SA (2004) High prevalence of low bone mineral density in pre-dialysis chronic kidney disease patients: bone histomorphometric analysis. Clin Nephrol 62(6):432–439
Acknowledgments
This study was supported by grants from the Natural Science Foundation of China (81403416, 81403419), Natural Science Foundation of Shanghai (12ZR1450400), Training Project of Young College Teachers in Shanghai (ZZSZY12064), Innovative Research Team of Ministry of Education (1RT1270), National Basic Research Program of China (2010CB530404), Shanghai Municipal Commission of Health and Family Planning (2012L032A), and “Top Priority” Clinical Medical Center ((2012)52).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Appendix 1. Search strategy of PubMed
Appendix 1. Search strategy of PubMed
Search (((((((((controlled clinical trial[Publication Type]) OR ((trial[Title]) OR randomly[Title/Abstract])) OR clinical trials as topic[MeSH Major Topic]) OR placebo[Title/Abstract]) OR randomized[Title/Abstract]) OR randomized controlled trial[Publication Type])) NOT ((animals[MeSH Terms]) NOT (“humans”[MeSH Terms] AND “animals”[MeSH Terms])))) AND ((((((osteoporosis) OR bone mineral density) OR bone loss) OR osteopenia)) AND ((((kidney transplant) OR renal transplantation) OR kidney transplantation) OR renal transplant)).
Rights and permissions
About this article
Cite this article
Wang, J., Yao, M., Xu, Jh. et al. Bisphosphonates for prevention of osteopenia in kidney-transplant recipients: a systematic review of randomized controlled trials. Osteoporos Int 27, 1683–1690 (2016). https://doi.org/10.1007/s00198-015-3465-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-015-3465-7