Abstract
Summary
Bone loss and vascular calcification coincide in patients with end-stage renal disease, similar as to what is observed in the general population. In the present bone biopsy study, we provide further evidence that (micro-)inflammation may represent a common soil for both diseases.
Introduction
Vascular calcification is a common complication of end-stage renal disease (ESRD) and is predictive of subsequent cardiovascular disease and mortality. Mounting evidence linking bone disorders with vascular calcification has contributed to the development of the concept of the bone-vascular axis. Inflammation is involved in the pathogenesis of both disorders. The aim of the present study was to evaluate the relationship between aortic calcification, inflammation, and bone histomorphometry in patients with ESRD.
Methods
Parameters of inflammation and mineral metabolism were assessed in 81 ESRD patients (55 ± 13 year, 68 % male) referred for renal transplantation. Static bone histomorphometry parameters were determined on transiliac bone biopsies performed during the transplant procedure. Aortic calcification was quantified on lateral lumbar X-rays using the Kauppila method.
Results
Aortic calcification, low bone turnover, and low bone area were observed in 53, 37, and 21 % of patients respectively. Inflammatory markers were found to be independently associated with aortic calcification (hsIL-6) and low bone area (TNF-α). Low bone area associated with aortic calcification, independent of age, diabetes, and inflammation.
Conclusions
Low bone area and inflammation associates with aortic calcification, independent of each other and traditional risk factors. Our data emphasize the role of (micro-)inflammation in the bone-vascular axis in CKD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic kidney disease (CKD) predisposes to osteoporosis [1] and vascular calcification [2], conditions that are both related to poor outcomes, including fractures [3] and cardiovascular disease [4]. The close relationship between bone metabolism and vasculature, also referred to as the bone-vascular axis [5, 6], raises the possibility of a common underlying pathophysiological mechanism driving bone loss, vascular disease, and/or vascular calcification. Of note, the association between osteoporosis and vascular calcification is not specific to CKD [4, 7–9] and remained significant after adjustment for age, which suggests an age-independent relationship [4, 7–13]. Arterial tissue is calcified in an organized, regulated process by mechanisms similar to those involved in the mineralization of bone [14]. Several lines of evidence suggest that inflammation promotes both calcification [15, 16] and osteoporosis [17] and as such may play a central role in the bone-vascular axis.
Clinical studies evaluating the relationship between bone status and vascular health in CKD patients so far yielded inconsistent results, with some researchers reporting a relationship between vascular calcification and low bone volume [11, 18] and others reporting a relationship between vascular calcification and low bone turnover [10, 19, 20]. Power issues, case-mix, and differences between arterial territories analyzed (conduit arteries versus resistance arteries) may explain this (apparent) inconsistency.
The present study aimed to investigate to which extent inflammation and bone status either independent or in concert with each other is associated with aortic calcification in patients with end-stage renal disease (ESRD).
Methods
Patient population
The present study refers to the baseline data of an ongoing longitudinal observational trial evaluating the impact of renal transplantation on bone histomorphometry (NCT01886950). All patients were listed for renal transplantation, 18 years of age or older, able to provide consent, and had not received bisphosphonates or denosumab during the preceding 6 months. The study was performed according to the Declaration of Helsinki and approved by the Ethics Committee of the University Hospital Leuven. Informed consent was obtained from all patients. Relevant demographic, smoking habit, and clinical data were extracted from electronic patient files at the time of transplantation. Hyperlipidaemia was defined as total cholesterol >200 mg/dl and/or LDL-cholesterol >100 mg/dl or statin intake. Cardiovascular history was defined as history of myocardial infarction, percutaneous coronary artery intervention, cardiac surgery, peripheral artery disease, or cerebrovascular disease. Hypertension was defined as a systolic blood pressure above 140 mmHg or diastolic blood pressure above 90 mmHg and/or with treatment for hypertension. Tobacco use was defined as “none,” “past,” or “current.”
Biochemical measurements
Random, non-fasting blood samples were collected immediately before transplantation. After centrifugation, serum was aliquoted and stored at −80 °C until further analysis. Creatinine, hematocrit, calcium, phosphorus, total alkaline phosphatase (AP), C-reactive protein (CRP), and cholesterol were all measured using standard laboratory techniques. Serum 1,25(OH)2D (calcitriol) and 25(OH)D (calcidiol) levels were measured using a radioimmunoassay. Serum full-length PTH levels were determined by an immunoradiometric assay (IRMA), as described elsewhere [21]. TNF-α (R&D Systems) and hsIL-6 (eBioscience) were measured by ELISA.
Bone histomorphometry
Bone biopsies were taken under general anesthesia at the end of the renal transplant procedure using a needle with an internal diameter of 4.5 mm (Osteobell, Biopsybell), at a site 2 cm posterior and 2 cm inferior to the anterior iliac spine. Since the timing of deceased donor kidney transplantation is unpredictable, bone biopsies were performed without double tetracycline labeling. The specimens were transferred into 70 % ethanol and prepared for quantitative histomorphometry as previously described [22]. Five-micrometer thick sections of non-decalcified bone were stained by the modified Goldner technique for light-microscopic examination. All measurements of length, width, and area were done using a digitizer interfaced with a microcomputer, and the results represent two-dimensional variables. Bone histomorphometric data were reported using standardized nomenclature and definitions [23]. Osteoblast-covered perimeter (ObPm) and osteoclast-covered perimeter (OcPm) were all expressed as a percentage of the total bone perimeter (BPm). The absence of tetracycline labeling precluded the assessment of dynamic histomorphometric parameters (bone formation rate, mineralization lag time, etc.). We used the bone area to total tissue area (BAr/Tar), osteoid area to bone area (OAr/BAr), and the ratio of osteoblast-covered perimeter to total bone perimeter (ObPm/BPm) as surrogate markers for bone volume, mineralization, and turnover, respectively (Table 1). The latter parameter, as opposed to osteoclast-covered perimeter to total bone perimeter (OcPm/BPm), showed good correlation with bone formation rate as determined by dynamic bone histomorphometry in a separate cohort of dialysis patients (n = 27, r = 0.64, P = 0.0004, unpublished data).
Vascular calcification
Aortic calcification was graded using the Kauppila method in which both the location and the severity of mineral deposits at each lumbar vertebral segment (L1–L4) were evaluated [24]. The composite score (i.e., the summation of scores of individual aortic segments both for the anterior and posterior wall) had a maximum of 24. One reader (SH) analyzed all lateral lumbar radiographs, blinded for clinical data.
Statistical analysis
Continuous variables are expressed as mean (standard deviation, SD) for normally distributed variables or median (inter quartile range (IQR)), otherwise. Differences between groups were analyzed using parametric or non-parametric one-way ANOVA, with post hoc correction for multiple comparisons, as appropriate. Correlations were examined using Spearman rank. Univariate and multivariate linear and logistic regressions with backward selection were used to model determinants of bone parameters and vascular calcification. The SAS version 9.3 (SAS Institute, Cary, NC) software program was used for the statistical analysis. Two-sided p < 0.05 was considered statistically significant.
Results
Demographics
Between September 2010 and September 2012, 261 patients underwent renal transplantation and were found eligible to be enrolled in the study. One hundred ten patients consented to procedure and bone biopsies of sufficient quality to allow determination of static bone histomorphometric parameters were obtained in 81 renal transplant recipients (Fig. 1). These patients did not significantly differ from non-participating patients transplanted in the same time period (Supplementary Table 1). Relevant demographics, clinical and biochemical parameters, and mineral metabolism therapy of the study population are summarized in Table 2. Seventy-five percent were men, 25 % were diabetic. Three women were on oral contraceptive therapy. Mean age was 55 ± 14 years. Primary renal disease was diabetes in 16.4 %, glomerulonephritis/vasculitis in 20.9 %, interstitial nephritis in 15.5 %, cystic/hereditary/congenital in 17.3 %, vascular in 6.4 %, miscellaneous in 5.5 %, and unknown or missing in 18.2 % of patients. Fifty-six patients (69 %) were treated with intermittent hemodialysis (1 nocturnal hemodialysis) and 21 (26 %) patients were on peritoneal dialysis. Four (5 %) patients were transplanted pre-emptive.
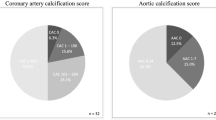
Aortic calcification
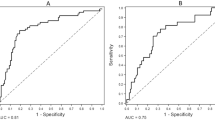
Aortic calcification was present in 53 % of the patients. Median [range] aortic calcification score was 2.5 [0–23]. Table 2 compares clinical parameters and biochemistry between patients with and without aortic calcification. Patients with aortic calcification were characterized by older age, higher prevalence of hypertension, diabetes mellitus, and history of cardiovascular disease. Biochemical mineral metabolism parameters did not differ between patients with and without aortic calcification. HsIL-6 levels were significantly higher, whereas TNF-α tended to be higher in patients with aortic calcification. In univariate logistic regression, older age, diabetic state, cardiovascular history, lower 1,25(OH)2D levels, and higher hsIL-6 levels were associated with the presence of aortic calcification (Supplementary Table 2). In multivariate analysis, older age (OR 1.2 per year increase, P < 0.0001), diabetes (OR 8.1, P = 0.04), hypertension (OR 6.7; P = 0.04), and higher hsIL-6 (OR 4.6 per pg/ml, P = 0.03) were independently associated with the presence of aortic calcification.
Bone histomorphometry
The ObPm/BPm ratio, a surrogate marker of bone turnover, was low, normal, and high in 37.0, 27.0, and 36.0 % of the patients, respectively. Bone volume, as assessed by the ratio of the bone area to total tissue area (BAr/TAr), was low, normal, and high in 21.0, 39.5, and 39.5 % of the patient population, respectively. The OAr/BAr, a surrogate marker of bone mineralization, was low in only one patient. The ObPm/BPm and to a lesser extent OcPm/BPm positively associated with serum PTH and total AP levels (Table 3). Gender, diabetic state and dialysis modality did not correlate with histomorphometric parameters of bone turnover/mineralization/volume (Tables 3 and 4). Patients with low BAr/TAr were characterized by older age, higher TNF-α levels, and a tendency toward higher hsIL-6 levels (Tables 3 and 4). In multivariate analysis, both age (β = −0.007; P = 0.01) and TNF-α (β = −0.14; P = 0.03) were identified as independent determinants of BAr/TAr, explaining 16 % of its variation (P = 0.002).
Relationship between aortic calcification and bone histomorphometry
BAr/TAr was significantly lower (P < 0.001), while the ObPm/BPm ratio (P = 0.13) and the OcPm/BPm ratio (P = 0.07) at best tended to be lower in patients with aortic calcification (Fig. 2). In logistic regression, BAr/TAr was identified as a significant determinant of aortic calcification, independent of age, diabetic state, and inflammatory markers (OR per % increase 0.01; P = 0.03). Of interest, the mineralized area (Md.Ar) showed congruent results compared to BAR/TAr, with significant higher mineralized area in patients without aortic calcification as compared to patients free of aortic calcification (0.24 ± 0.06 versus 0.19 ± 0.06; p < 0.0001).
Discussion
The present study demonstrates that a low BAr/TAr, a marker of bone volume, is an independent determinant of aortic calcification in patients with ESRD and confirms the important role of inflammation in the bone-vascular axis.
CKD is an independent cardiovascular (CV) risk factor and the risk of death increases exponentially with the progressive decline of renal function. Traditional and non-traditional CV risk factors, including disorders of mineral and bone metabolism, are suggested to account for the extreme CV morbidity and mortality rates in CKD patients. In 2006, the term CKD-mineral and bone disorder (CKD-MBD) was coined to describe a syndrome that is manifested by abnormalities in mineral and bone metabolism and/or extra-skeletal calcifications [25]. Intense cross talk exists between the bone and the vasculature, which is commonly referred to as the bone-vascular axis, and the pathological hallmarks of parallel diseased bone and arterial vessels are vascular calcification and renal osteodystrophy, respectively.
The prevalence of vascular calcification increases with worsening renal function and ranges from 40 % in patients with CKD stage 3, to 80–90 % in patients with end-stage renal disease [2]. Reported prevalence rates show important variation, which may be explained, at least partly by case-mix, differences in arterial territories analyzed and in the sensitivity of imaging techniques used. Traditional risk factors, including old age, diabetes, arterial hypertension, and history of cardiovascular disease, account to a large extent for the high prevalence of aortic calcifications in CKD patients [26]. Of note, patients enrolled in the present study were all renal transplant candidates and as such represented a younger patient group with less comorbidity than the overall dialysis population. These population characteristics presumably explain the relatively low prevalence of aortic calcification observed in the present cohort (53 %). A similar prevalence was recently reported in a comparable cohort [27].
Bone disorders occur early in the course of CKD and become very prevalent in advanced CKD [28]. The gold standard to evaluate bone disorders in CKD is quantitative histomorphometric bone biopsy analysis. An international committee sponsored by Kidney Disease: Improving Global Outcomes concurred that the most important parameters to describe renal osteodystrophy are turnover, mineralization, and volume (TMV classification) [25]. Using ObPm/BPm as surrogate parameter of bone turnover, low bone turnover was observed in 37 % of patients with ESRD enrolled in the present study. This prevalence of low bone turnover is lower as compared to a recent large survey covering bone biopsies in dialysis patients between 2003 and 2008 [29]. Case-mix may account at least partly for this discrepancy. While age and prevalence of diabetes were comparable, dialysis vintage was significantly shorter in our cohort. It should be emphasized that eligibility for renal transplantation was the only selection criterion in the present study, and that, different from previous surveys, patients were not selected on clinical symptoms, biochemical criteria or suspicion of aluminum toxicity. A low trabecular bone volume, as defined by a trabecular BAr/TAr below 16.8 %, was seen in 21 % of patients. Only few bone biopsy studies so far dealt with the prevalence rate of “osteoporosis” in CKD and values reported varied between 16 and 54 %. This wide variation is due to case-mix and lack of a uniform histomorphometric definition of osteoporosis within the setting of CKD [11, 17, 29].
Interestingly, low trabecular bone volume, but not low bone turnover associated with aortic calcification. Previous studies evaluating the association between vascular calcification and bone histomorphometry in CKD patients have yielded inconsistent findings. Some investigators found an association between systemic arterial calcification (aorta and the main peripheral arteries) [10, 20] or coronary artery calcification [19] and indices of low bone turnover, but not (trabecular) bone area/volume. Others, conversely, found an association between coronary artery calcifications and low (trabecular) bone area/volume, but like us, failed to find a correlation with histomorphometric indices of bone turnover [11, 13]. Again, case-mix, heterogeneity of the arterial tree and power issues may account for the inconsistency.
Our data confirm and extend data from cross-sectional and longitudinal studies in both the general population [4, 7, 30] and CKD [31–33] patients showing a direct relationship between vascular calcification and low bone mass as determined by DEXA (reflecting the composite of bone area and mineralization). Some have suggested that low bone mass is an even stronger predictor of cardiovascular disease than other well-known risk factors, such as serum cholesterol and smoking in postmenopausal women [30].
The mechanisms underlying the bone-vascular axis remain poorly understood [6]. Mounting evidence points to inflammation as a potential common culprit [34, 35]. It is well recognized that CKD is a micro-inflammatory state [36, 37]. In the present study, TNF-α and hsIL-6 were substantially increased, being above the upper normal range in 43 and 51 % of patients, respectively. These prevalence rates of micro-inflammation are however substantially lower than previously reported in ESRD populations, which, once again may be due to case-mix [38].
In the present study, hsIL-6 was identified as a significant determinant of aortic calcification, independent of age, diabetes, and hypertension, confirming the previously described relationship between vascular calcification and markers of inflammation in CKD patients [15, 16] as well as in the general population [39] and in diabetics [40]. Underlying pathophysiological mechanisms are complex and multiple. Inflammatory cytokines can promote vascular smooth muscle cell calcification [41], in part through the activation of Msx2-Wnt/β-catenin signalling [42]. Moreover, inflammatory cytokines may promote the process of endothelial to mesenchymal transition, leading to osteogenic gene expression and cytokine production by endothelial cells [34]. Finally, inflammation may repress the important calcification inhibitor fetuin-A [43].
Of interest, even in this cohort with relatively mild micro-inflammation, TNF-α and hsIL-6 levels negatively correlated with bone area [17]. This observation is consistent with evidence showing that the local production of inflammatory cytokines, such as TNF-α and IL-1β, leads to increased bone resorption and decreased bone formation [44, 45]. These effects are mediated, in part, via cytokine-induced increases in RANKL, a key stimulator of bone resorption, by osteoblasts and T cells [46]. TNF-α is also an inhibitor of bone formation [47], tilting the balance toward bone resorption with subsequent bone loss [34]. IL-6 is produced by osteoblast cells and possesses bone-resorbing activity, probably by increasing the formation of mature osteoclasts from hematopoietic progenitors [48]. Our data corroborate with a recent study linking elevated circulating TNF-α levels with decreased bone mineral density and incident fractures in CKD-5D [49]. Our results and those of others, conversely, conflict with data reported by Barreto et al., showing a positive correlation between TNF-α levels and bone area [17]. These authors speculate that elevated TNF-α expression may represent a homeostatic feedback mechanism to counteract excessive bone mass gain. This hypothesis, however, although to some extent sound, conflicts with a bench of experimental and clinical evidence [44, 45].
Inflammation thus represents a common soil for bone loss and vascular calcification and might indeed explain the coincidence of these diseases in the present ESRD cohort [35, 50]. Interestingly, the association between low bone area and aortic calcification remained significant after adjustment for age, diabetes, and inflammatory markers. This suggests that additional factors may be involved and calls for additional research [6].
The strength of our study is the relatively large sample size. By combining bone histomorphometry and vascular imaging in 81 patients, this study is among the largest of its kind. It should however be acknowledged that this sample size still confers a substantial risk for a type II statistical error. Furthermore, the only selection criterion for study entry was eligibility for renal transplantation. This precludes any selection on suspected bone pathology, often being present in previous bone biopsy-based histomorphometric studies. Our study also has limitations. First, bone turnover was based on static bone parameters solely. As patients were enrolled at the time of deceased kidney transplantation, which is unpredictable, double tetracycline labeling was not possible. The observation of a good correlation between static and dynamic bone turnover parameters in a preceding study is reassuring. Nonetheless, we acknowledge that lack of power may explain why we, as opposed to others, failed to find a relationship between surrogate marker of bone turnover and vascular calcification. Second, we cannot exclude misclassification bias, related to the use of a single laboratory value rather than time-averaged concentrations. Moreover, blood sampling time was not standardized due to the unpredictability of the deceased donor transplant procedure. That we nonetheless found significant associations, underlines its robustness.
In summary, our data support the hypothesis that (micro-)inflammation is the common soil of low bone volume and aortic calcification in CKD. Besides CKD, other common diseases, including diabetes mellitus, and aging are increasingly acknowledged to be associated with a low-grade chronic inflammatory status. We envisage that our findings will fuel additional studies investigating the bone and vascular effects of dietary [51] and pharmacological [52] interventions targeting (micro-)inflammation in these populations.
References
Cunningham J, Sprague SM, Cannata-Andia J, Coco M, Cohen-Solal M, Fitzpatrick L, Goltzmann D, Lafage-Proust MH, Leonard M, Ott S, Rodriguez M, Stehman-Breen C, Stern P, Weisinger J (2004) Osteoporosis in chronic kidney disease. Am J Kidney Dis 43:566–571
Budoff MJ, Rader DJ, Reilly MP, Mohler ER III, Lash J, Yang W, Rosen L, Glenn M, Teal V, Feldman HI (2011) Relationship of estimated GFR and coronary artery calcification in the CRIC (Chronic Renal Insufficiency Cohort) Study. Am J Kidney Dis 58:519–526
Ball AM, Gillen DL, Sherrard D, Weiss NS, Emerson SS, Seliger SL, Kestenbaum BR, Stehman-Breen C (2002) Risk of hip fracture among dialysis and renal transplant recipients. JAMA 288:3014–3018
Tanko LB, Christiansen C, Cox DA, Geiger MJ, McNabb MA, Cummings SR (2005) Relationship between osteoporosis and cardiovascular disease in postmenopausal women. J Bone Miner Res 20:1912–1920
Thompson B, Towler DA (2012) Arterial calcification and bone physiology: role of the bone-vascular axis. Nat Rev Endocrinol 8:529–543
London GM (2009) Bone-vascular axis in chronic kidney disease: a reality? Clin J Am Soc Nephrol 4:254–257
Schulz E, Arfai K, Liu X, Sayre J, Gilsanz V (2004) Aortic calcification and the risk of osteoporosis and fractures. J Clin Endocrinol Metab 89:4246–4253
Naves M, Rodriguez-Garcia M, Diaz-Lopez JB, Gomez-Alonso C, Cannata-Andia JB (2008) Progression of vascular calcifications is associated with greater bone loss and increased bone fractures. Osteoporos Int 19:1161–1166
Hyder JA, Allison MA, Wong N, Papa A, Lang TF, Sirlin C, Gapstur SM, Ouyang P, Carr JJ, Criqui MH (2009) Association of coronary artery and aortic calcium with lumbar bone density: the MESA Abdominal Aortic Calcium Study. Am J Epidemiol 169:186–194
London GM, Marty C, Marchais SJ, Guerin AP, Metivier F, de Vernejoul MC (2004) Arterial calcifications and bone histomorphometry in end-stage renal disease. J Am Soc Nephrol 15:1943–1951
Adragao T, Herberth J, Monier-Faugere MC, Branscum AJ, Ferreira A, Frazao JM, Dias CJ, Malluche HH (2009) Low bone volume—a risk factor for coronary calcifications in hemodialysis patients. Clin J Am Soc Nephrol 4:450–455
Rodriguez-Garcia M, Gomez-Alonso C, Naves-Diaz M, Diaz-Lopez JB, Diaz-Corte C, Cannata-Andia JB (2009) Vascular calcifications, vertebral fractures and mortality in haemodialysis patients. Nephrol Dial Transplant 24:239–246
Barreto DV, Barreto FC, Carvalho AB, Cuppari L, Cendoroglo M, Draibe SA, Moyses RM, Neves KR, Jorgetti V, Blair A, Guiberteau R, Fernandes Canziani ME (2005) Coronary calcification in hemodialysis patients: the contribution of traditional and uremia-related risk factors. Kidney Int 67:1576–1582
Neven E, De Schutter TM, De Broe ME, D'Haese PC (2011) Cell biological and physicochemical aspects of arterial calcification. Kidney Int 79:1166–1177
Oh J, Wunsch R, Turzer M, Bahner M, Raggi P, Querfeld U, Mehls O, Schaefer F (2002) Advanced coronary and carotid arteriopathy in young adults with childhood-onset chronic renal failure. Circulation 106:100–105
Guerin AP, London GM, Marchais SJ, Metivier F (2000) Arterial stiffening and vascular calcifications in end-stage renal disease. Nephrol Dial Transplant 15:1014–1021
Barreto FC, Barreto DV, Moyses RM, Neves CL, Jorgetti V, Draibe SA, Canziani ME, Carvalho AB (2006) Osteoporosis in hemodialysis patients revisited by bone histomorphometry: a new insight into an old problem. Kidney Int 69:1852–1857
Barreto DV, Barreto FC, Carvalho AB, Cuppari L, Draibe SA, Dalboni MA, Moyses RM, Neves KR, Jorgetti V, Miname M, Santos RD, Canziani ME (2008) Association of changes in bone remodeling and coronary calcification in hemodialysis patients: a prospective study. Am J Kidney Dis 52:1139–1150
Tomiyama C, Carvalho AB, Higa A, Jorgetti V, Draibe SA, Canziani ME (2010) Coronary calcification is associated with lower bone formation rate in CKD patients not yet in dialysis treatment. J Bone Miner Res 25:499–504
London GM, Marchais SJ, Guerin AP, Boutouyrie P, Metivier F, de Vernejoul MC (2008) Association of Bone Activity, Calcium Load, Aortic Stiffness, and Calcifications in ESRD. J Am Soc Nephrol 19:1827–1835
Bouillon R, Coopmans W, Degroote DE, Radoux D, Eliard PH (1990) Immunoradiometric assay of parathyrin with polyclonal and monoclonal region-specific antibodies. Clin Chem 36:271–276
Spasovski GB, Bervoets ARJ, Behets GJS, Ivanovski N, Sikole A, Dams G, Couttenye MM, De Broe ME, D'Haese PC (2003) Spectrum of renal bone disease in end-stage renal failure patients not yet on dialysis. Nephrol Dial Transplant 18:1159–1166
Dempster DW, Compston JE, Drezner MK, Glorieux FH, KANIS JA, Malluche H, Meunier PJ, Ott SM, Recker RR, Parfitt AM (2013) Standardized nomenclature, symbols, and units for bone histomorphometry: a 2012 update of the report of the ASBMR Histomorphometry Nomenclature Committee. J Bone Miner Res 28:2–17
Kauppila LI, Polak JF, Cupples LA, Hannan MT, Kiel DP, Wilson PW (1997) New indices to classify location, severity and progression of calcific lesions in the abdominal aorta: a 25-year follow-up study. Atherosclerosis 132:245–250
Moe S, Drueke T, Cunningham J, Goodman W, Martin K, Olgaard K, Ott S, Sprague S, Lameire N, Eknoyan G (2006) Definition, evaluation, and classification of renal osteodystrophy: a position statement from Kidney Disease: improving Global Outcomes (KDIGO). Kidney Int 69:1945–1953
Cannata-Andia JB, Rodriguez-Garcia M, Carrillo-Lopez N, Naves-Diaz M, Diaz-Lopez B (2006) Vascular calcifications: pathogenesis, management, and impact on clinical outcomes. J Am Soc Nephrol 17:S267–S273
Meneghini M, Regalia A, Alfieri C, Barretta F, Croci D, Gandolfo MT, Vettoretti S, Rastaldi MP, Messa P (2013) Calcium and osteoprotegerin levels predict the progression of the abdominal aortic calcifications after kidney transplantation. Transplantation 96:42–48
Coen G, Mazzaferro S, Ballanti P, Sardella D, Chicca S, Manni M, Bonucci E, Taggi F (1996) Renal bone disease in 76 patients with varying degrees of predialysis chronic renal failure: a cross-sectional study. Nephrol Dial Transplant 11:813–819
Malluche HH, Mawad HW, Monier-Faugere MC (2011) Renal osteodystrophy in the first decade of the new millennium: analysis of 630 bone biopsies in black and white patients. J Bone Miner Res 26:1368–1376
von der RP, Hansen MA, Hassager C (1999) The association between low bone mass at the menopause and cardiovascular mortality. Am J Med 106:273–278
Braun J, Oldendorf M, Moshage W, Heidler R, Zeitler E, Luft FC (1996) Electron beam computed tomography in the evaluation of cardiac calcification in chronic dialysis patients. Am J Kidney Dis 27:394–401
Toussaint ND, Lau KK, Strauss BJ, Polkinghorne KR, Kerr PG (2008) Associations between vascular calcification, arterial stiffness and bone mineral density in chronic kidney disease. Nephrol Dial Transplant 23:586–593
Asmus HG, Braun J, Krause R, Brunkhorst R, Holzer H, Schulz W, Neumayer HH, Raggi P, Bommer J (2005) Two year comparison of sevelamer and calcium carbonate effects on cardiovascular calcification and bone density. Nephrol Dial Transplant 20:1653–1661
Khosla S (2011) The bone and beyond: a shift in calcium. Nat Med 17:430–431
New SE, Aikawa E (2011) Molecular imaging insights into early inflammatory stages of arterial and aortic valve calcification. Circ Res 108:1381–1391
Herbelin A, Nguyen AT, Zingraff J, Urena P, Descamps-Latscha B (1990) Influence of uremia and hemodialysis on circulating interleukin-1 and tumor necrosis factor alpha. Kidney Int 37:116–125
Kaysen GA (2001) The microinflammatory state in uremia: causes and potential consequences. J Am Soc Nephrol 12:1549–1557
Stenvinkel P, Wanner C, Metzger T, Heimburger O, Mallamaci F, Tripepi G, Malatino L, Zoccali C (2002) Inflammation and outcome in end-stage renal failure: does female gender constitute a survival advantage? Kidney Int 62:1791–1798
Jenny NS, Brown ER, Detrano R, Folsom AR, Saad MF, Shea S, Szklo M, Herrington DM, Jacobs DR Jr (2010) Associations of inflammatory markers with coronary artery calcification: results from the Multi-Ethnic Study of Atherosclerosis. Atherosclerosis 209:226–229
Alman AC, Kinney GL, Tracy RP, Maahs DM, Hokanson JE, Rewers MJ, Snell-Bergeon JK (2013) Prospective association between inflammatory markers and progression of coronary artery calcification in adults with and without type 1 diabetes. Diabetes Care 36:1967–1973
Tintut Y, Patel J, Territo M, Saini T, Parhami F, Demer LL (2002) Monocyte/macrophage regulation of vascular calcification in vitro. Circulation 105:650–655
Al-Aly Z, Shao JS, Lai CF, Huang E, Cai J, Behrmann A, Cheng SL, Towler DA (2007) Aortic Msx2-Wnt calcification cascade is regulated by TNF-alpha-dependent signals in diabetic Ldlr-/- mice. Arterioscler, Thromb, Vasc Biol 27:2589–2596
Ketteler M, Bongartz P, Westenfeld R, Wildberger JE, Mahnken AH, Böhm R, Metzger T, Wanner C, Jahnen-Dechent W, Floege J (2003) Association of low fetuin-A (AHSG) concentrations in serum with cardiovascular mortality in patients on dialysis: a cross-sectional study. Lancet 361:827–833
Pfeilschifter J, Chenu C, Bird A, Mundy GR, Roodman GD (1989) Interleukin-1 and tumor necrosis factor stimulate the formation of human osteoclastlike cells in vitro. J Bone Miner Res 4:113–118
Ferreira A, Saraiva M, Behets G, Macedo A, Galvao M, D'Haese P, Drueke TB (2009) Evaluation of bone remodeling in hemodialysis patients: serum biochemistry, circulating cytokines and bone histomorphometry. J Nephrol 22:783–793
Hofbauer LC, Lacey DL, Dunstan CR, Spelsberg TC, Riggs BL, Khosla S (1999) Interleukin-1beta and tumor necrosis factor-alpha, but not interleukin-6, stimulate osteoprotegerin ligand gene expression in human osteoblastic cells. Bone 25:255–259
Kobayashi K, Takahashi N, Jimi E, Udagawa N, Takami M, Kotake S, Nakagawa N, Kinosaki M, Yamaguchi K, Shima N, Yasuda H, Morinaga T, Higashio K, Martin TJ, Suda T (2000) Tumor necrosis factor alpha stimulates osteoclast differentiation by a mechanism independent of the ODF/RANKL-RANK interaction. J Exp Med 191:275–286
Feyen JH, Elford P, Di Padova FE, Trechsel U (1989) Interleukin-6 is produced by bone and modulated by parathyroid hormone. J Bone Miner Res 4:633–638
Panuccio V, Enia G, Tripepi R, Aliotta R, Mallamaci F, Tripepi G, Zoccali C (2012) Pro-inflammatory cytokines and bone fractures in CKD patients An exploratory single centre study. BMC Nephrol 13:134
Hjortnaes J, Butcher J, Figueiredo JL, Riccio M, Kohler RH, Kozloff KM, Weissleder R, Aikawa E (2010) Arterial and aortic valve calcification inversely correlates with osteoporotic bone remodelling: a role for inflammation. Eur Heart J 31:1975–1984
Krishnamurthy VM, Wei G, Baird BC, Murtaugh M, Chonchol MB, Raphael KL, Greene T, Beddhu S (2012) High dietary fiber intake is associated with decreased inflammation and all-cause mortality in patients with chronic kidney disease. Kidney Int 81:300–306
Saisho Y (2015) Metformin and inflammation: its potential beyond glucose-lowering effect. Endocr Metab Immune Disord Drug Targets
Acknowledgments
Part of this work was presented at the 46th American Society of Nephrology Congress, Atlanta, USA, 5-10/11/2013.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 14 kb)
Rights and permissions
About this article
Cite this article
Viaene, L., Behets, G.J., Heye, S. et al. Inflammation and the bone-vascular axis in end-stage renal disease. Osteoporos Int 27, 489–497 (2016). https://doi.org/10.1007/s00198-015-3233-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-015-3233-8