Abstract
Summary
The incidence of hip fracture in Sweden is substantially lower in immigrants than in the population born in Sweden. Thus, the use of a FRAX® model in immigrants overestimates the risk of fracture, and the use of country of origin-specific models may be more appropriate.
Introduction
Age-specific fracture and mortality rates vary between countries so that FRAX tools are country-specific. In the case of immigrants, it is not known whether the model for the original or the new country is most appropriate. The aim of this study was to compare the incidence of hip fractures in foreign-born and Swedish-born individuals residing in Sweden.
Methods
We studied the incidence of hip fracture in all men and women aged 50 years or more in Sweden between 1987 and 2002. The population comprised 2.8 million Swedish-born and 270,000 foreign-born individuals.
Results
Incident hip fractures occurred in 239,842 Swedish-born and 12,563 foreign-born individuals. The hip fracture incidence rose with age for both groups and was higher for women than men amongst both Swedish-born and foreign-born individuals. The hip fracture incidence for the Swedish-born cohort was approximately twice that of immigrants. For example, at the age of 70 years, the annual hip fracture incidence (per 100,000) was 450 (95 % CI 446–454) for a Swedish-born woman and 239 (95 % CI 223–257) for a foreign-born woman at the time of immigration. The hip fracture incidence rose slowly with time from immigration (0.6 % per annum, 95 % CI 0.5–0.8 %) but remained significantly lower than for Swedish-born individuals even after 40 years of residence.
Conclusions
The incidence of hip fracture in Sweden is substantially lower in immigrants than in the population native to Sweden. Although there was a small rise in age- and sex-specific incidence after immigration, the incidence remained markedly lower than that observed in Swedish-born individuals. Thus, the use of a FRAX model for Sweden will overestimate the risk of fracture for foreign-born individuals living in Sweden.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Advances in transport and communication infrastructure have allowed a dramatic increase in the movement of individuals between countries, whether to seek employment, undertake study or escape persecution [1]. Such migration has major consequences for health care in destination countries, both in terms of unfamiliar diseases, such as rare infections, and more common chronic non-communicable diseases (NCDs), such as osteoporosis, diabetes and cardiovascular disease [2–4]. In such circumstances, both genetic and environmental factors may be relevant but has been relatively poorly characterized for most NCDs [5]. Immigration brings with it a potentially marked change in the prevailing environment, in terms of diet and lifestyle, together with other ecological factors such as water fluoridation and air pollution. These new environmental factors interact with the innate genetic make-up of the individual to modify disease risk [5]. Given the heterogeneity in environment and genotype, it is by no means certain what the effect of migration from one country to another will be on a specific disease.
The consequence of osteoporosis fragility fractures clearly represents a major burden to modern society, costing the European Union approximately €37 billion annually or 3 % of the total health care spend [6]. Highly effective treatments are now available to treat osteoporosis, and the clinical assessment of patients judged to be at risk of fracture is a critical step in the management of the disease [7]. FRAX® provides such a clinical tool for the calculation of fracture probability to identify individuals at high risk [8, 9]. Models are calibrated to country-specific epidemiology as both fracture and death risk (which are combined to yield fracture probability as opposed to fracture incidence) vary between countries [10, 11]. Thus, a FRAX model for one country may not be appropriate for another country [12]. In order to use FRAX optimally, it is therefore important to ascertain whether fracture incidence rates in an immigrant population are closer to those of the original, or the new country of residence.
We aimed, therefore, to compare the incidence of hip fractures in foreign-born and Swedish-born individuals living in Sweden using population wide data.
Methods
We studied admissions to Swedish hospitals for hip fracture between January 1987 and December 2002 for persons above the age of 50 years. The source comprised the national Swedish register (the patient register to the National Board of Health and Welfare) which documents each hospital admission on a continuous basis. A unique personal identifier permitted the tracking of individuals for multiple admissions. The database included all patients discharged from hospital according to the disease category and surgical procedure. Registration is a legal requirement, is backed by financial inducement and has an accuracy that exceeds 90 % for surgical admissions [13]. Hip fractures were identified on the basis of the relevant International Classification of Diseases (ICD) code (ICD 9: 820x or ICD 10: S720–S724 or S727–S729 before and after 1996, respectively) and a surgical procedure for proximal femur fracture by the operation code ICD9 841, 82x or NFB, NFJ in the operation code fields [14]. The cases were documented by age, sex and region of birth. We examined the incidence of hip fracture in men and women aged 50 years (born 1939–1987) or more between 1987 and 2002. Where appropriate, follow-up ended at the date of emigration.
Country of birth was designated as one of eight regions: Sweden, Africa, Asia, Europe without Sweden, North America, Oceania, Union of Soviet Socialist Republics (USSR) and South America (Table 1). No information was available on the exact country of birth. There was, however, information on immigration from other Nordic countries. The region of birth was unknown in 1069 foreign-born individuals and was excluded from further analysis. For the regional estimates, we excluded Oceania because of the low sample size and number of hip fractures that were recorded. With regard to illegal immigrants, Sweden has a national health service that is free at the point of contact. It is most unlikely, therefore, that fractures would be missed in legal immigrants. Fractures may have been missed in illegal immigrants, but neither the individual nor the fracture would be registered.
An extension of the Poisson regression model [15] was used to study the association between age, sex, the time since immigration on the one hand and the risk of hip fracture. The observation period of each participant was divided in intervals of 1 year. One fracture per person was counted. The relationship between age and hip fracture incidence was evaluated using a linear piecewise model with knots at 70 and 90 years, in order to allow the increase of hip fracture with age to differ with intervals of age. The determination of the beta coefficients were performed separately for Swedish-born and foreign-born individuals. The association between age, sex, time and the risk of fracture was described as the hazard ratio per 1 unit change. Two-sided values of p were used for all analyses, and p < 0.05 was considered to be significant.
Results
There were 2,756,874 Swedish-born individuals and 269,129 (9 %) foreign-born individuals in the register comprising men and women aged 50 years or above in Sweden in January 1987 (see Table 1). The mean age of immigrants was lower than in native Swedes (p < 0.001), though this varied by place of birth.
Swedish-born individuals
The incidence of hip fracture by age and sex in Swedish-born individuals is shown in Table 2. The risk of hip fracture was higher in women than in men with an HR of 1.68 (95 % CI 1.66–1.69). Hip fracture incidence rose progressively with age. Before the age of 70 years, the rise for 1 year of age was by 12 % (95 % CI 12–13 %). The corresponding increase between the ages of 70 and 90 years was by 14 % (95 % CI 13–14 %) and after the age 90 years was by 0.6 % (95 % CI 0.3–1.0 %). There was a small but significant decrease in risk of hip fracture with time by 0.6 % for each calendar year (95 % CI 0.5–0.7 %; p < 0.001), a phenomenon evident in women (0.8 %; 95 % CI 0.7–0.9 %; p < 0.001) but not in men (0.0 %; 95 % CI −0.2–0.1; p > 0.30).
Foreign-born individuals living in Sweden
The risk of hip fracture was higher for women than for men HR 1.52 (95 % CI 1.45–1.62) for immigrants. Hip fracture incidence rose significantly with age throughout the whole age range (Table 2). Before the age of 70 years, the rise was by 13 % per year (95 % CI 12–14 %). The corresponding risk increase between the ages of 70 and 90 years was 15 % per year (95 % CI 14–15 %), but after the age 90 years, there was a significant decrease by 3 % per year (95 % CI −7–0 %). At all ages and for both sexes, the incidence of hip fracture was lower in immigrants than in native Swedes.
There was a small but significant increase in age-adjusted risk of hip fracture with time from immigration (p < 0.001) by 0.61 % (95 % CI 0.46–0.77 %) for each year of follow-up for men and women together. At the age of 50 years, the incidence per 100,000 was 15 for men and 22 for women (Table 3) 5 years after immigration. Twenty years after immigration, the corresponding incidences were 16 and 25. At the age of 90 years, the incidence per 100,000 was 2428 for men and 3713 for women after 5 years after immigration. Twenty years after immigration, the corresponding incidences were 2661 and 4070.
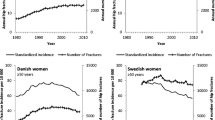
The incidence with time from immigration in foreign-born women using a linear model is shown in Fig. 1 at the age of 70 years. The incidence of hip fracture per 100,000 for a 70-year-old foreign-born woman at the time of immigration was 239 (95 % CI 223–257) and rose modestly with calendar year so that 45 years after immigration, the incidence was 315 (95 % CI 298–333) (Fig. 1). Even after 45 years, the incidence of hip fracture was markedly lower than in Swedish-born women of the same age. For example, the incidence of hip fracture in 1995, the year mid-way across the time period studied, for 70-year-old women born in Sweden was 450 (95 % CI 446–454) (see Fig. 1). Thus, despite the increase in hip fracture risk with time since immigration, the risk remained far lower than that for Swedish-born women of the same age. The same pattern was observed at all ages and in men (data not shown).
Subgroups of foreign-born
The majority of foreign-born were from Europe (87 %) and Asia (5 %) (see Table 1). Hip fracture rates 5 years after immigration were consistently lower in foreign-born women than the rates for Sweden (Table 4). In the case of men, however, rates in Asian and African immigrants were not markedly lower than the rates seen in Swedish-born men though the confidence intervals for both were wide (Table 4). For individuals born in Europe, there was a statistically significant increase in incidence with time from immigration by 0.48 % per year (95 % CI 0.30–0.65; p < 0.001) (Table 4). Within Europe, immigrants excluding other Nordic countries had markedly lower fracture rates than the Nordic countries. For individuals born in Europe outside Nordic countries, there was a statistically significant increase in incidence with time from immigration by 0.38 % per year (95 % CI 0.13–0.63; p = 0.0026). For the other regions, the change per year from immigration ranged from −0.2 to 2.0 % (Table 4).
Discussion
The principal finding of the present analysis of the whole population of Sweden is that hip fracture incidence in Sweden is substantially lower in immigrants than in the Swedish-born population. We observed a small rise in incidence after immigration but which remained markedly lower than that observed in Swedish-born individuals. These disparities suggest that, in foreign-born individuals in Sweden, approaches to risk stratification, such as the use of FRAX, should be based on data calibrated to the country of origin, rather than to the Swedish-born population.
It is well established that there are marked differences in hip fracture rates worldwide [11, 16–19], and the incidence of hip fractures in Sweden is amongst the highest globally for women, second only to Denmark [11]. It is to be expected, therefore, that the immigrant population would have lower fracture rates than native-born Swedes at the time of immigration. Within Europe, fracture rates were higher in immigrants from other Nordic countries than the rest of Europe. Similar findings have been reported for Stockholm County [20] and in a large case-control study from Sweden [4]. In the latter study, foreign-born individuals had a reduced risk of hip fracture, with odds ratios of 0.47–0.77 for men and 0.42–0.88 for women, findings similar to those of the present study. In the UK, Caucasian men and women are at increased risk of hip and other fractures than ethnic groups from the Caribbean, Africa or Asia [21]. The lower fracture rates in the immigrant population contrast with the documented poorer health status [22] and higher mortality [23, 24] of these individuals.
It is of interest that male immigrants from Asia and Africa had incidence rates that were only slightly lower than men born in Sweden. The strength of this observation is limited by the relatively small sample size with wide confidence intervals, but a relatively high risk has previously been noted in male but not in female Asian immigrants to Stockholm [20]. The relatively high rates are particularly surprising in African immigrants where the scant information base suggests that the hip fracture rates are much lower than those in Europe [11]. Low income and language fluency [25] and poor vitamin D status [26] are predictors of higher hip fracture risk, but these factors do not provide an explanation of the relatively high fracture rates early after immigration. The most likely explanation is selection bias favouring the immigration of African men at high risk to the labour market, although it was not possible, using the current dataset, to identify individual risk factors which might account for these observations.
In the present study, we also found that the reduced incidence in immigrants persisted for up to 45 years after immigration. A small rise in incidence did occur after immigration but remained markedly lower than that observed in Swedish-born individuals. Similar findings have been previously reported in Sweden but with a shorter follow-up [4]. These findings are consistent with observations in Hawaii. On the Hawaiian island of Oahu, hip fracture rates in individuals of Japanese origin did not change between 1979–1981 and 1991–1995, but, in this instance, hip fracture rates were similar to indigenous Caucasians [27] though lower than rates elsewhere in the USA [28]. Elsewhere in the USA, hip fracture rates are lower in Black and Asian Americans than in the Caucasian population even though many will not be first generation immigrants [19].
The persistence of lower hip fracture risks in the immigrant population has implications for fracture risk assessment that make use of FRAX in that the FRAX model for Sweden will overestimate the risk of fracture for a foreign-born individual living in Sweden. The use of FRAX models from the country of origin is likely to provide a more accurate assessment of fracture probability. It is relevant that FRAX in Sweden is based on national information on the whole population, irrespective of birth origin. Thus, hip fracture risks of native Swedes may be underestimated by 4–5 % in the present study.
The strength of the present study is in its longitudinal design based on the entire Swedish population. In addition, the accuracy of the available registers is high. The foreign-born immigrants were younger and more often men, but age and sex adjustment did not alter the conclusions. The majority of immigration to Sweden is for the labour market, and there is likely to a healthy selection bias. Limitations of the present study were that potential confounders such as economic status, specific country of origin and other risk factors for fracture were not available in the cohort. It is notable that the overall data on immigrants are driven largely by European immigrants with perhaps less power to make conclusions about the other groups. It is also possible that some immigrants return to their country of origin without informing the relevant authorities which would underestimate the hip fracture risk in the immigrant population. The relevance for successive generations is not known. The present findings are relevant for Sweden and are not necessarily applicable to other settings, particularly in countries that have low or intermediate fracture risks.
We conclude that hip fracture incidence in Sweden is substantially lower for immigrants than in the Swedish-born population. Although there was a small rise in incidence after immigration, the incidence remained markedly lower than that observed in Swedish-born individuals. Thus, the use of a FRAX model for Sweden will overestimate the risk of fracture for a foreign-born individual living in Sweden, and use of country of origin-specific models will generally be appropriate.
References
United Nations, Department of Economic and Social Affairs, Population Division (2013) Trends in international migrant stock: the 2013 revision—migrants by age and sex. (United Nations database, POP/DB/MIG/Stock/Rev.2013/Age)
Hemminki K (2014) Immigrant health, our health. Eur J Pub Health 24(Suppl 1):92–95
Bo A, Zinckernagel L, Krasnik A, Petersen JH, Norredam M (2014) Coronary heart disease incidence among non-Western immigrants compared to Danish-born people: effect of country of birth, migrant status, and income. Eur J Prev Cardiol
Albin B, Hjelm K, Elmstahl S (2010) Lower prevalence of hip fractures in foreign-born individuals than in Swedish-born individuals during the period 1987–1999. BMC Musculoskelet Disord 11:203. doi:10.1186/1471-2474-11-203
Holroyd CR, Harvey NC, Edwards MH, Cooper C (2013) Environment. In: Watts R, Conaghan PG, Denton C, Foster H, Isaacs J, Muller-Ladner U (eds) Oxford textbook of rheumatology, 4th edn. Oxford University Press, Oxford
Hernlund E, Svedbom A, Ivergård M, Compston J, Cooper C, Stenmark J, McCloskey EV, Jönsson B, Kanis JA (2013) Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos 8:136. doi:10.1007/s11657-013-0136-1
Kanis JA, McCloskey EV, Johansson H, Cooper C, Rizzoli R, Reginster JY, Scientific Advisory Board of the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO) and the Committee of Scientific Advisors of the International Osteoporosis Foundation (IOF) (2013) European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 24:23–57
Kanis JA, Johnell O, Oden A, Johansson H, McCloskey E (2008) FRAX and the assessment of fracture probability in men and women from the UK. Osteoporos Int 19:385–397
Kanis JA, on behalf of the World Health Organization Scientific Group (2008) Assessment of osteoporosis at the primary health-care level. Technical Report. WHO Collaborating Centre, University of Sheffield, UK
Kanis JA, Johnell O, De Laet C, Jonsson B, Oden A, Ogelsby AK (2002) International variations in hip fracture probabilities: implications for risk assessment. J Bone Miner Res 17:1237–1244
Kanis JA, Odén A, McCloskey EV, Johansson H, Wahl D, Cyrus Cooper C, on behalf of the IOF Working Group on Epidemiology and Quality of Life (2012) A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos Int 23:2239–2256
Leslie WD, Brennan SL, Lix LM, Johansson H, Oden A, McCloskey E, Kanis JA (2013) Direct comparison of eight national FRAX(R) tools for fracture prediction and treatment qualification in Canadian women. Arch Osteoporos 8:145. doi:10.1007/s11657-013-0145-0
Ludvigsson JF, Andersson E, Ekbom A, Feychting M, Kim JL, Reuterwall C, Heurgren M, Olausson PO (2011) External review and validation of the Swedish national inpatient register. BMC Public Health 11:450. doi:10.1186/1471-2458-11-450
Rosengren BE, Ahlborg HG, Mellstrom D, Nilsson JA, Bjork J, Karlsson MK (2012) Secular trends in Swedish hip fractures 1987–2002: birth cohort and period effects. Epidemiology 23:623–630
Breslow NE, Day NE (1987) Statistical methods in cancer research. IARC Scientific Publications No 32 Volume II p 131–135
Schwartz AV, Kelsey JL, Maggi S, Tuttleman M, Ho SC, Jonsson PV, Poor G, Sisson de Castro JA, Xu L, Matkin CC, Nelson LM, Heyse SP (1999) International variation in the incidence of hip fractures: cross-national project on osteoporosis for the World Health Organization program for research on aging. Osteoporos Int 9:242–253
Bacon WE, Maggi S, Looker A, Harris T, Nair CR, Giaconi J, Honkanen R, Ho SC, Peffers KA, Torring O, Gass R, Gonzalez N (1996) International comparison of hip fracture rates in 1988–89. Osteoporos Int 6:69–75
Sibai AM, Nasser W, Ammar W, Khalife MJ, Harb H, Fuleihan Gel H (2011) Hip fracture incidence in Lebanon: a national registry-based study with reference to standardized rates worldwide. Osteoporos Int 22:2499–2506
Cauley JA, El-Hajj Fuleihan G, Arabi A, Fujiwara S, Ragi-Eis S, Calderon A, Chionh SB, Chen Z, Curtis JR, Danielson ME, Hanley DA, Kroger H, Kung AW, Lesnyak O, Nieves J, Pluskiewicz W, El Rassi R, Silverman S, Schott AM, Rizzoli R, Luckey M (2011) Official positions for FRAX(R) clinical regarding international differences from Joint Official Positions Development Conference of the International Society for Clinical Densitometry and International Osteoporosis Foundation on FRAX(R). J Clin Densitom 14:240–262
Furugren L, Laflamme L (2007) Hip fractures among the elderly in a Swedish urban setting: different perspectives on the significance of country of birth. Scand J Public Health 35:11–16
Hippisley-Cox J, Coupland C (2012) Derivation and validation of updated QFracture algorithm to predict risk of osteoporotic fracture in primary care in the United Kingdom: prospective open cohort study. BMJ 344, e3427
Pudaric S, Sundquist J, Johansson SE (2003) Country of birth, instrumental activities of daily living, self-rated health and mortality: a Swedish population-based survey of people aged 55–74. Soc Sci Med 56:2493–2503
Albin B, Hjelm K, Ekberg J, Elmstahl S (2005) Mortality among 723,948 foreign- and native-born Swedes 1970–1999. Eur J Pub Health 15:511–517
Albin B, Hjelm K, Ekberg J, Elmstahl S (2006) Higher mortality and different pattern of causes of death among foreign-born compared to native Swedes 1970–1999. J Immigr Minor Health 8:101–113
Zingmond DS, Soohoo NF, Silverman SL (2006) The role of socioeconomic status on hip fracture. Osteoporos Int 17:1562–1568
Holvik K, Meyer HE, Haug E, Brunvand L (2005) Prevalence and predictors of vitamin D deficiency in five immigrant groups living in Oslo, Norway: the Oslo Immigrant Health Study. Eur J Clin Nutr 59:57–63
Ross PD, Huang C (2000) Hip fracture incidence among Caucasians in Hawaii is similar to Japanese. A population-based study. Aging (Milano) 12:356–359
Ross PD, Norimatsu H, Davis JW, Yano K, Wasnich RD, Fujiwara S, Hosoda Y, Melton LJ 3rd (1991) A comparison of hip fracture incidence among native Japanese, Japanese Americans, and American Caucasians. Am J Epidemiol 133:801–809
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Johansson, H., Odén, A., Lorentzon, M. et al. Is the Swedish FRAX model appropriate for Swedish immigrants?. Osteoporos Int 26, 2617–2622 (2015). https://doi.org/10.1007/s00198-015-3180-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-015-3180-4