Abstract
Summary
Widespread poor vitamin D status, a health risk for bone disease, increases the need for new food sources of vitamin D. Light-exposed edible mushrooms synthesize vitamin D2. Bioavailability, safety, and efficacy of high levels of vitamin D2 from mushrooms to support bone health was established in chronically fed growing rats.
Introduction
Poor vitamin D status from reduced sun exposure is made worse by limited access to vitamin D-containing foods. Exposing white button mushrooms to ultraviolet B (UVB) light markedly increases their vitamin D2 content, creating a new food source of vitamin D. We used a growing rat model to determine safety, bioavailability, and efficacy in support of bone growth by vitamin D2 from UVB-exposed mushrooms.
Methods
We fed 150 weanling female rats one of five diets for 10 weeks, all formulated on AIN-93 G. Control diets contained no mushrooms either with or without vitamin D3. Other diets contained 2.5% and 5.0% of UVB-exposed or -unexposed mushrooms. Safety of the high levels of vitamin D2 from mushrooms was assessed by animal growth and by Von Kossa staining for soft tissue calcification. Bioavailability was determined from changes in circulating levels of 25-hydroxyvitamin D [25(OH)D] and parathyroid hormone (PTH). Efficacy in support of bone growth was determined from measures of femur bending properties, size, mineralization, and microarchitecture.
Results
Diets containing 2.5% and 5.0% light-exposed mushrooms significantly raised 25(OH)D and suppressed PTH levels compared to control-fed rats or rats fed 5.0% mushroom unexposed to light. Microarchitecture and trabecular mineralization were only modestly higher in the light-treated mushroom-fed rats compared to the controls. Von Kossa staining revealed no soft tissue calcification despite very high plasma 25(OH)D.
Conclusions
Vitamin D2 from UVB-exposed mushrooms is bioavailable, safe, and functional in supporting bone growth and mineralization in a growing rat model without evidence of toxicity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Until the last decade, adequacy of vitamin D intake was not a pressing public health concern, because of the widely accepted assumption that cutaneous vitamin D synthesis from sun exposure, vitamin D3 or cholecalciferol, was thought to meet most of our needs with respect to bone health [1]. The majority of circulating 25-hydroxyvitamin D [25(0H)D], the main indicator of vitamin D nutritional status, originates from cutaneous synthesis of vitamin D3 upon exposure to adequate sunlight; however, seasonal changes, living at high latitudes or low polluted altitudes, dark skin pigmentation, and aging are among the many factors that can impede this process, requiring periodic reliance on dietary sources to supply the precursor to 25(OH)D [2]. The national surveys in North America continue to show a high prevalence of poor vitamin D status as measured by serum 25(OH)D and low dietary intake of vitamin D-rich foods [3–5]. While adverse skeletal effects of poor vitamin D status are well established [6], this trend raises additional public health concern due to the growing evidence confirming a significant association between poor vitamin D status and increased risk of nonskeletal, chronic, autoimmune, and infectious diseases and mortality.
Low vitamin D intake is largely due to the limited number of foods that are naturally rich in vitamin D or are fortified with vitamin D [7]. Vitamin D was listed as one of four critical nutrients that Americans need to consume more of in the Federal Dietary Guidelines for Americans, 2010 [8, 9]. The 2010 Dietary Guidelines Advisory Committee concluded that the typical American diet contains inadequate amounts of these nutrients including vitamin D and that efforts to meet these nutrient needs should be made through food rather than dietary supplements [9].
Two forms of vitamin D occur in foods—cholecalciferol or D3 found in some animal products and fortified foods and ergocalciferol or D2 from yeast and fungi, such as white button mushrooms, when they are exposed to ultraviolet B (UVB) light [10–12] are used in food fortification with some restrictions. For example, fortification of soy milk and other plant- or grain-based milks is restricted to vitamin D2 because it is not of animal origin [13]. In developing new foods using either vitamin D2 or D3, both forms of vitamin D must be absorbed and bioavailable for use in different tissues including bone. Bioavailability requires vitamin D2 or D3 to be transported after absorption to the liver primarily via chylomicrons where it is hydroxylated and released to the circulation as either 25(OH)D2 or 25(OH)D3 which circulates bound to vitamin D binding protein (DBP) [14, 15]. For a novel dietary source of vitamin D to be considered bioavailable, the parent compound must be both absorbed and efficiently hydroxylated to the intermediate form [25(OH)D] that circulates and delivers the precursor to tissues to be further metabolized to the active hormonal form of vitamin D (1,25-dihydroxyvitamin D). Circulating levels of the intermediate metabolite [25(OH)D2 or 25(OH)D3] are used as both a nutritional status indicator and as a measure of vitamin D bioavailability from different food sources [16].
Our study was designed to test the bioavailability of vitamin D2 from light-exposed edible mushrooms, which are the only natural food source of vitamin D2 commonly consumed in the USA and Canada [13, 17]. The ability of commonly consumed white button mushrooms (Agaricus bisporis) to make ample levels of vitamin D2 is well established as it is for other varieties of edible fungi [10–12, 18–21]. We hypothesized that vitamin D2 from fresh mushrooms exposed to UVB light postharvest would be absorbed, bioavailable, safe, and effective in support of bone growth. We further hypothesized that even at intake levels exceeding the dietary recommendations for the rat, the mushroom source of vitamin D2 would support optimal bone growth without safety concerns such as soft tissue calcification. Here, we report our findings from a 10-week feeding study that was also designed to examine the effects of vitamin D2 from light-exposed white button mushrooms on immune response in growing female rats terminally challenged with endotoxin [22]. In this report, we address vitamin D2 bioavailability, efficacy in support of bone growth and safety at very high doses from this novel food source of vitamin D2 in order to assure a wide margin of safety for human consumption.
Materials and methods
Experimental design
The study utilized 300 weanling female Sprague–Dawley rats (3 weeks old) that were allowed an acclimation period of 1 week prior to being randomized into the study. The large number of rats studied required us to stagger the 10-week feeding periods over a year. We conducted a total of ten separate, 10-week feeding trials with each trial consisting of 30 rats (a squad). A total of ten squads of 30 rats were studied with each squad containing six animals in each dietary experimental group. Three of the six rats in each of the five dietary groups served as saline controls which were used to evaluate functionality of vitamin D2 in bone, while the remaining three were used to evaluate effects on immune response. Careful attention was paid to limit confounding variables utilizing rat pups from no more than three litters with each squad of thirty rats studied (obtained from Harlan, Indianapolis, IN). All rats were housed individually in polycarbonate, microisolator cages with deionized water and test diet available ad libitum. All rats were housed in dedicated air-conditioned rooms with 12 h light and dark cycles and room temperature maintained at 18–26°C and 40–70% relative humidity. The animal protocol was approved by the IACUC committee of the Center for Food Safety and Applied Nutrition of the US Food and Drug Administration (protocol number 502), and the study was conducted according to the Animal Welfare Act guidelines.
Once randomized, the rats were fed one of five diets, all formulated based on AIN-93 G (Research Diets, New Brunswick, NJ) to contain different levels of vitamin D2 and either light-exposed mushroom powder or mushroom powder from unexposed mushrooms (Table 1). The feeding regime period was 10 weeks. At the end of each feeding regime, half of the rats were challenged with lipopolysaccharide (LPS) [23] to determine immune response (results are reported elsewhere); the remaining half received a control saline injection. In order to avoid potential confounding factors from the LPS challenge, the right femurs from rats in the saline control group were analyzed in this study.
At necropsy, blood was drawn into K3EDTA vacutainer tubes, centrifuged for plasma separation and stored in dedicated aliquots at -80°C until analyzed. In this paper, we report the effects of mushrooms and vitamin D2-enriched mushrooms on the levels of circulating 25(OH)D and parathyroid hormone (PTH) as measures of vitamin D status and bioavailability. Microcomputed tomography (micro-CT) analysis of the distal femur was used to assess the mushrooms’ ability to support bone growth, and histological evidence of soft tissue calcification was assessed to assure safety of very high levels of vitamin D2 from white button mushrooms fed daily for 10 weeks.
Diets
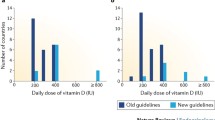
All five experimental diets were made by Research Diets and were formulated based on the AIN-93 G formula with modification to adjust for desired vitamin D content and to adjust for the addition of UVB treated or untreated mushroom powder (Table 1). In order to more closely resemble the typical high fat American diet, all diets differed from the standard AIN-93 G formula by their 15% fat content in contrast to the standard 5% fat content. The fat content was composed of 15% (150 g/kg diet) American fat blend consisting of 37.5 g cocoa butter, 4.5 g linseed oil, 52.5 g palm oil, 28.5 safflower oil, and 27.0 g sunflower oil. As shown in Table 1, control diet (column 1) and vitamin D-deficient control diet (column 2) contained no mushroom powder and contained either the recommended level of vitamin D3 [24] or no vitamin D3, while the remaining test diets were all made with vitamin D-free premix and contained 5.0% unexposed mushroom powder, or 2.5% or 5.0% UVB light-treated mushroom powder added at the expense of cornstarch. Estimated vitamin D content of the five diets was calculated from direct analyses of the mushroom powder. Powdered, freeze-dried, light-exposed, and -unexposed white button mushrooms were generously provided by the Australian Mushroom Growers Association through Mushrooms Canada and the Guelph Food Technology Center (GFTC) and samples from each contained 15 and <0.5 μg vitamin D2/g dried mushroom, respectively, as analyzed by Dr. Pirjo Mattila, MTT Agrifood, Finland [25, 26]. The rats were estimated to consume 20, 0, 2.4, 300, and 600 IU of vitamin D/day, respectively, from each of the experimental diets.
Biomarkers of vitamin D status
The Dia Sorin (Stillwater, MN) radioimmunoassay (RIA) was used to measure rat plasma levels of total 25(OH)D [25(OH)D2 + 25(OH)D3].This widely used RIA measures both the vitamin D2 and D3 metabolites to produce total 25(OH)D concentrations which are considered the best biomarkers of vitamin D status [6, 16]. Inter assay variation based on low (9.3–19.7 ng/ml) and high (50.7–68.9 ng/ml) controls were 15% and 13%, respectively. Rat plasma PTH levels were determined using ALPCO Diagnostic’s rat PTH IRMA (Salem, NH). Assay performance based on high controls (336–560 pg/ml) was 10.6% and 15.2% for inter- and intraassay variation, respectively. Plasma creatinine levels were measured as a surrogate biomarker for renal function using a quantitative colorimetric kit (Bioassays Systems, Hayward, CA).
Microcomputed tomography of femur
Three-dimensional (3-D) bone microstructure was measured in 150 right femurs (saline-challenged control rats only) using microcomputed tomography (micro-CT 100, Scanco Medical, Basserdorf, Switzerland). The entire femur was imaged at an isotropic voxel size of 24 μm (nominal resolution). Trabecular bone microarchitecture and mineralization were analyzed in the metaphyseal region of the distal femur, close to the growth plate where newly formed trabecular bone would best reflect any nutritional insults. Sagittal and transverse sections of the reconstructed images were used to identify trabecular bone just proximal to the fused growth plate (Fig. 1). A total of 70 contiguous slices of trabecular bone from the anterior, lateral quadrant proximal to the growth plate was manually contoured with automated morphing algorithms that linearly interpolated between manual contours every ten slices. Segmentation to distinguish trabecular bone from background was visually chosen (threshold = 235, sigma = 0, support = 0). From these segmented images, automated distance transformation algorithms were used to calculate the following morphological parameters: bone volume fraction (BV/TV), trabecular thickness (Tb.Th), trabecular spacing (Tb.Sp), trabecular number (Tb.N), and connectivity density (Conn.D.) based on methods of Hildebrand and Ruegsegger [27–29]. Principal material orientations (H1, H2, and H3) and degree of anisotropy (DA) were calculated using 3-D mean intercept length techniques. Trabecular bone mineralization (in mg/cc HA) was computed from attenuation values of grayscale micro-CT images based on hydroxyapatite (HA) calibration standards. In addition, an approximately 2-mm section of cortical bone at the midshaft (50% from the distal end) was analyzed for cortical thickness and polar moment of inertia (pMOI).
Femur bending strength
Load at break was measured in three-point bending at the mid-shaft of right rat femurs from the saline control group (n = 150) using a table top Instron 4465 universal testing machine. Femurs were oriented in the anterior–posterior direction with the span between end supports consistently set at 14 mm. All tests were completed at 10 mm/min until fracture.
Histology of kidney, liver, and spleen
A pilot study sampling the entire last squad of 30 rats (with 6 rats from each dietary group) was conducted in order to determine if the high vitamin D2 consumption from the light-exposed mushrooms or the possible development of secondary hyperparathyroidism from the chronic consumption of vitamin D-deficient diets resulted in soft tissue calcification. Tissue samples of liver, spleen, and kidney from each of the 30 rats were taken at necropsy and fixed in formalin. Sections of kidney, liver, and spleen were stained with hematoxylin and eosin and with the Von Kossa method for mineralization [30] and were evaluated by light microscopy. Tissue sectioning and staining was conducted by LifeSpan BioSciences (Seattle, WA) who directed the blinded pathology evaluation. The histology results shown in Table 3 are presented as the number of rats out of a total of six per dietary group that were positive for the specific organ pathology. For each of the dietary groups, there were no Von Kossa positive rat spleens, livers, or kidneys.
Statistical analyses
The results are shown as the mean and SD of each dietary group. The data were tested for normality and an appropriate one-way analysis of variance (ANOVA) followed by pairwise comparisons were used to determine the significance of any differences among the dietary groups, with significance set at (p < 0.05 for most parameters and at p < 0.008 when multiple comparisons were made among micro-CT measures of the femur trabecular bone.). Levene’s test for homogeneity was used initially followed by Welch’s ANOVA and least squares means was used for post-ANOVA comparisons. For the two status indicators, 25(OH)D and PTH, and all bone parameters measures significantly different from the control diet-fed rats or from the vitamin D-deficient control-fed rats are indicated by * p < 0.05; ^ p < 0.008; ** p < 0.001 and ‡ p < 0.05, ‡‡ p < 0.001; @ p < 0.008, respectively.
Results
Growth
Fig. 2 shows the mean body weights over the 10-week feeding period for the five different diet groups. The presence of mushroom, adequate, excess, or deficient levels of vitamin D had no apparent effect on body weight in growing female rats. Mean body weights were not different among animals fed different diets at any point during the 10-week feeding study. These findings of no effect on growth suggest no general toxicity from long-term mushroom consumption with or without vitamin D.
Bioavailability of Vitamin D from mushrooms
Vitamin D2 from UVB-exposed mushrooms is highly bioavailable as shown in Table 2. Rats fed the 5.0% UVB mushroom diet had a mean plasma 25(OH)D level that was in the excess vitamin D range (159 ± 29 ng/ml) for humans. This diet contained 30 times the National Research Council (NRC) recommendation for vitamin D in the growing rat [24]. Rats fed the NRC level for vitamin D3 with no mushroom (control diet) showed a final group mean 25(OH)D level of 32 ± 11 ng/ml, which is within the normal human reference range for the DiaSorin assay (30–100 ng/ml). Circulating 25(OH)D levels above 150 ng/ml in humans are considered excessive, and values below 30 ng/ml are inadequate [31]. Plasma 25(OH)D concentrations below 10 ng/ml, as shown for the vitamin D-deficient control-fed rats and the 5.0% unexposed mushroom-fed rats, are in the vitamin D-deficient range. Vitamin D2 from mushrooms therefore was both bioavailable and effective in suppressing the PTH level (Table 2). This was demonstrated by the significantly higher PTH levels in rats fed the vitamin D-deficient control compared to the vitamin D replete groups (p < 0.001). Group mean PTH level in rats consuming the vitamin D-deficient 5.0% unexposed mushroom diet was also significantly lower (p < 0.002) than the vitamin D-deficient control-fed group suggesting that mushrooms may contain factors that facilitate calcium absorption thus reducing PTH secretion.
Femur density and microarchitecture
We evaluated the metaphyseal region close to the growth plate of the distal femur because it is the most recently formed trabecular bone and presumably the most sensitive to dietary factors affecting mineralization. No trabecular micro-CT parameters shown in Table 2 were significantly different from the control-fed group for both the UVB-exposed mushroom-fed groups. There is, however, a notable trend toward higher values for BV/TV, Conn.D, Tb.N, Tb.Th, and mean density in the 5% UVB mushroom group compared to the control-fed rats, suggesting the higher vitamin D2 content of light-exposed mushrooms maximized bone mineralization. In contrast, generally lower trabecular measures relative to the control group were observed in rats fed the vitamin D-deficient control diet, but none of these measures reached the adjusted statistical significance level (p < 0.008). Despite the low vitamin D content of the diet, rats fed the 5.0% unexposed mushroom diet showed statistically significant (p < 0.01) higher connectivity density and mean trabecular mineralization, but lower trabecular thickness compared to the control group. The presence of mushrooms in the diet, with and without vitamin D, apparently stimulates bone accretion as suggested by the significantly longer femurs (p < 0.001) in all the mushroom-fed rats. Higher vitamin D intake from light treated mushroom diets had greater impact on cortical bone as shown by the higher mean midshaft cortical thickness and pMOI (p < 0.01) relative to the control-fed rats. Nevertheless, no differences in cortical bone strength were observed from the load at break measures. In earlier micro-CT measurements (data not shown) scanned at a greater distance from the growth plate, distal femur trabecular microarchitecture was not affected by the high circulating 25(OH)D levels. Curiously, in these measures in more mature bone, distal femur density was also significantly greater in the rats fed 5.0% mushroom with no vitamin D compared to the rats fed the 2.5% and 5.0% vitamin D-enriched mushrooms.
Histology
The use of EDTA-containing blood collection tubes prevented determination by conventional analyses of hypercalcemia, the initial indicator of vitamin D toxicity which in time leads to soft tissue calcification [30, 31]. Plasma creatinine levels were measured in order to provide information concerning renal function which may be impaired in the case of hypercalcemia in response to long-term consumption of high levels of vitamin D. No significant differences were observed in mean plasma levels of creatinine indicating no apparent impairment of renal function after 10 weeks of feeding the high vitamin D mushroom diets. Group mean ± SD plasma creatinine levels (mg/dl) were as follows: 0.628 ± 0.089, 0.667 ± 0.093, 0.668 ± 0.116, 0.682 ± 0.101, 0.667 ± 0.097 for the control, control no vit. D, 5% untreated mushroom, 2.5% and 5% UVB-treated mushroom diets, respectively.
As shown in Table 3, 10 weeks of feeding very high levels of ergocalciferol was not associated with soft tissue calcification as detected by Von Kossa staining. Even with serum 25(OH)D levels in the potentially toxic end of the normal human range in rats fed 2.5% or 5.0% UVB-exposed mushroom diets, no evidence of kidney, liver, or spleen calcium deposition was observed. Similarly, calcification of these organs was not observed in rats with elevated PTH levels consuming vitamin D-deficient diets, which is commonly associated with extra-skeletal calcification.
Discussion
When developing new food sources of vitamin D, such as light-exposed mushrooms, the safety and efficacy at levels of vitamin D that exceed the 2010 upper level (UL) of safe intake must be established in preclinical models such as the growing rat [31]. Species differences in size and requirements make it difficult to exceed the UL in a growing rat model. We tested vitamin D2 from mushrooms at a level approximately 30-fold higher than the recommended dietary intake of vitamin D for a growing rat, but at the recommended daily allowance (RDA) for normal adult men and women younger than 70 years [24, 31]. This represents a 30-fold safety factor over the normal rat intake of vitamin D. We reasoned that exposing mushrooms to ultraviolet radiation did not constitute the introduction of a novel ingredient into a food and that initial safety testing should need only to continue for a sufficient duration to determine the development of adverse effects that can occur in vitamin D toxicity or approximately 10 weeks in a growing rat.
Evidence suggests that vitamin D2 is less effective than vitamin D3 in sustaining plasma 25(OH)D levels in humans [32], which may raise question about extrapolation of efficacy findings from rats to humans. The rat model, however, may be more sensitive to the potential toxicity of vitamin D2 in very high doses because the rat preferentially hydroxylates ergocalciferol (D2) over cholecalciferol (D3) to the intermediate metabolite, 25(OH)D [33]. We found no evidence of toxicity such as growth retardation, impairment of renal function indicated by elevated plasma creatinine levels or calcification of soft tissues (kidney, spleen, and liver) after 10 weeks of consuming either 300 or 600 IU vitamin D2 each day. Our findings of the safety of very high doses of vitamin D2 are consistent with those in old world monkeys [34] and humans [35, 36] consuming very high levels of vitamin D2 daily over months.
We have greater confidence in the extrapolation of safety data from rodents to humans because our testing design includes a safety factor, in this case a 30-fold higher intake level. In contrast, there is no safety factor that can compensate for metabolic differences between rats and humans when extrapolating efficacy data to humans, and therefore, we urge caution in generalizing the use of this food source as a means of improving vitamin D status in the general population. Others have shown good bioavailability of vitamin D2 from light-exposed white button mushrooms in rats [11, 20], and in the present study, we have demonstrated that mushrooms serving as the sole source of vitamin D can sustain adequate and high levels of circulating 25(OH)D in rats. Earlier studies in humans [37–39] have shown vitamin D2 from mushroom consumption to be bioavailable, but these human studies either fed very high bolus doses [39], lacked rigorous control of the vitamin content generated by light exposure [37, 38], or were conducted in adults with confirmed vitamin D deficiency [38, 39] during the winter months when endogenous synthesis of vitamin D3 was limited. Urbain and German colleagues [39] demonstrated good bioavailability in winter without toxicity in young adults consuming soup made from light-exposed white button mushrooms, delivering 28,000 IU vitamin D2 per weekly serving. Similarly, Ozzard et al [38] demonstrated that light-exposed mushrooms effectively raised 25(OH)D levels and suppressed PTH in a young Asian vegan living in London. Under conditions of low 25(OH)D status and limited endogenous synthesis, vitamin D2 from mushrooms appears to be effective in raising total 25(OH)D levels. However, an important limitation to the extrapolation of these findings to the general population stems from evidence that vitamin D2 may increase plasma 25(OH)D2, while resulting in a decrease in 25(OH)D3 levels and failure to further elevate total 25(OH)D [40]. Long-term clinical studies in old and young subjects with both adequate and poor baseline vitamin D status are needed to monitor safety and efficacy over summer and winter with varying doses of vitamin D2 from mushrooms, particularly doses that exceed the UL of 4000 IU D2/day.
We also showed functional efficacy of the mushroom derived vitamin D2 in sustaining bone mineralization in growing rats. An important limitation of our study design was the high calcium content of all the diets (1% Ca) that possibly hindered our ability to observe a marked difference between the rats fed vitamin D-deficient diets with and without mushrooms. When vitamin D and calcium are low or insufficient in the diet (0.4% Ca), clear differences in microarchitecture were observed between the vitamin D-deficient and replete rats using the same micro-CT methods used in this study [41]. These authors also found that cortical bone was maintained in preference to trabecular bone in vitamin D-deficient growing rats fed low calcium diets [41]. Given the higher calcium content of the diets fed in the present study, the slight elevation in PTH relative to control-fed rats, which was observed in the vitamin D-deficient 5.0% unexposed mushroom-fed rats, may have stimulated greater bone accretion and growth. The adequate calcium content of our diets may explain the minor, less significant impairment of trabecular mineralization observed in vitamin D-deficient mushroom- and control-fed rats. Alternatively, mushrooms may have some as yet unknown component that stimulates growth, a possibility considering the stimulatory effect on the innate immune system observed in the rats fed vitamin D2-rich light-exposed mushrooms after challenge with LPS [22].
With an estimated 40% of the worldwide population at risk for vitamin D deficiency [6], there is a critical need to provide new dietary sources of vitamin D that are palatable, not of animal origin, and affordable in order to meet the diverse taste, dietary, and religious needs of the global population [15, 17]. The need for higher intakes of vitamin D is evidenced by changes in the 2011 dietary reference intake guidelines (RDA) which increased recommended vitamin D intakes from 200 and 400 IU/day to 600 and 800 IU/day for normal healthy men and women greater than 1 year of age and over 70 years, respectively [31]. In addition, the Endocrine Society Clinical Practice Committee of experts in vitamin D more recently issued recommendations for patients at risk for vitamin D deficiency [6], which were generally three times higher than the 2011 RDA for men and women older than 19 years. The committee also suggested a significantly higher UL of safe intake for these adults at risk, raising the UL from 4000 to 10,000 IU/day [6]. The expert committee recommended using either vitamin D2 or vitamin D3, despite reports that vitamin D2 is less effective than vitamin D3 when used as a dietary supplement in humans [32]. The US Food and Drug Administration does not distinguish between the efficacy of vitamin D2 and D3 used to fortify foods or as a dietary supplement [7]. The 2010 Dietary Guidelines for Americans also reiterate the need for higher vitamin D intakes and emphasize that the vitamin D should come predominantly from food sources [9]. Whiting et al. [5] and others [4, 7, 15, 17] have shown that despite mandatory fortification of fluid milk in Canada and the USA, the average intake of vitamin D from food alone is very low compared to the 2011 dietary recommended intake (RDA) of 600 IU/day. These national average intakes from food alone are 250 IU/day for the national Canadian community [5] and, on average, less than 250 IU/day for the US population according to the 2005–2006 US National Health and Education Survey [4]. In reality, the guidelines for healthy living established for the USA and Canada are significantly higher than the level of vitamin D actually consumed from food alone.
Vitamin D2 is the only form of vitamin D that meets the dietary and religious needs of a diverse population, largely because it is not of animal origin. However, to meet the needs of all socioeconomic segments of our population a new food source for vitamin D must also be affordable. The 2010 federal government’s update of the food pyramid called on Americans to eat more foods containing potassium, vitamin D, calcium, and dietary fiber [9, 42, 43]. Foods containing these nutrients are not easily affordable to many North Americans, especially with respect to vitamin D and potassium (fatty fish like salmon, milk, fortified orange juice) [43]. With the cost of milk and fortified orange juice subject to constant market change and continued higher cost due to bad weather or higher fuel expenses, Monsivais et al. [43] suggests that healthy eating according to the government guidelines may become an exclusive privilege of the rich. Mushrooms are good sources of potassium and can be exposed postharvest to a controlled light source to precisely generate 100% or more of the RDA (600 IU) of vitamin D2 in a single serving of 100 g fresh mushrooms that will remain stable under normal storage conditions [19], all for less than US$1. Availability of high vitamin D mushrooms to poor segments of our population at risk for vitamin D insufficiency will remain a problem without further study and dissemination of the health benefits of vitamin D-containing mushrooms. Particular attention should be given to the possible application of megadoses of vitamin D2 from mushrooms to combat diseases in children in addition to rickets, especially in populations without access to fortified milk. Several studies show potential health benefits from high dose vitamin D2 supplements to enhance bone growth in Indian girls [44] and to treat cystic fibrosis [45].
In conclusion, we have demonstrated the potential for light-exposed white button mushrooms to become a safe, bioavailable, effective, and affordable dietary source of vitamin D2 for use in diverse populations worldwide with poor vitamin D status and with limited access to sun or other dietary sources.
References
Institute of Medicine, Food and Nutrition Board (1997) Dietary reference intakes: calcium, phosphorus, magnesium, vitamin D, and fluoride. National Academy Press, Washington, DC
Whiting S, Greene T, Calvo M (2007) Vitamin D intakes in North America and Asia-Pacific Countries are not sufficient to prevent vitamin D insufficiency. J Steroid Biochem Mol Bio 103:626–630
Looker A, Pfeiffer C, Lacher D, Schleicher R, Picciano M, Yetley E (2008) Serum 25-hydroxyvitamin D status of the US population: 1988–1994 compared to 2000–2004. Am J Clin Nutr 88:1519–1527
Bailey R, Dodd K, Goldman J, Gache J, Dwyyer J, Moshfegh A, Sempos C, Picciano M (2010) Estimation of total usual calcium and vitamin D intakes in the United States. J Nutr 140:817–822
Whiting S, Langlois K, Vantanparast H, Greene-Finestone L (2011) The vitamin D status of Canadians relative to the 2011 Dietary reference intakes: an examination in children and adults with and without supplement use. Am J Clin Nutr 94:128–135
Holick M, Binkley N, Bischoff-Ferrari H, Gordon C, Hanley D, Heaney R, Murad H, Weaver C (2011) Evaluation, treatment, and prevention of vitamin D deficiency: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 96:1911–1930
Calvo M, Whiting S, Barton C (2004) Vitamin D fortification in the US and Canada: current status and research needs. Am J Clin Nutr 80:1710S–17106S
Department of Agriculture, Department of Health and Human Services, Dietary guidelines for Americans 2010 [Internet]. Government Printing Office, Washington, DC; 2011 Jan 11. Available from: http://www.cnpp.usda.gov/DGAs2010-PolicyDocument.htm. Last accessed August 5, 2011
Dietary guidelines advisory committee. The report of the dietary guidelines advisory committee on the dietary guidelines for Americans, 2010. Department of Health and Human Services, Washingtion, DC, 2010. Available from: http://www.cnpp.USDA.gov/dgas2010-dgacreport.htm. Last accessed August 11, 2011
Mau J, Chen P, Yanf J (1998) Ultraviolet irradiation increased vitamin D2 content of edible mushrooms. J Agric Food Chem 46:5269–5272
Jasinghe V, Perera C (2005) Distribution of ergosterol in different tissues of mushrooms and its effect on the conversion of ergosterol to vitamin D2 by UV irradiation. Food Chem 92:541–546
Simon R, Phillips K, Horst R, Munro I (2011) Vitamin D mushrooms: comparison of the composition of button mushrooms (Agaricus bisporus) treated post harvest with UVB light or sunlight. J Agric Food Chem 59:8724–8732. Publication date: 8 July 2011
Whiting S, Calvo M (2011) Chapter 54: Lifestyle and nutritional determinants of vitamin status. In: Feldman D, Pike WJ, Adams JS (eds) Vitamin D, 3rd edn, pp 979–1007. Wiley-Blackwell
Haddad J, Matsuoka L, Hollis B, Hu Y, Wortsman J (1993) Human plasma transport of vitamin D after its endogenous synthesis. J Clin Invest 91:2552–2555
Calvo M, Whiting S, Barton C (2005) Vitamin D intake: a global perspective of current status. J Nutr 135:310–316
Hollis B (2005) Circulating 25-hydroxyvitamin D levels indicative of vitamin D sufficiency: implications for establishing a new effective dietary intake recommendation for vitamin D. J Nutr 135:317–322
Calvo M, Whiting S (2010) Chapter 18: Determinants of vitamin D intakes. In: Holick MF (ed) Vitamin D: physiology, molecular biology and clinical applications, 2nd edn, pp 361–382. Humana Press
Mattila P, Piironen V, Uusi-Rauva E, Koivistoinen P (1994) Vitamin D contents in edible mushrooms. J Agric Food Chem 42:2449–2453
Roberts J, Teichert A, McHugh T (2008) Vitamin D2 formation from post-harvest UV-B treatment of mushrooms (Agaricus bisporus) and retention during storage. J Agric Food Chem 56:4541–4544
Koyyalamudi S, Jeong S, Song C, Cho K, Pang G (2009) Vitamin D2 formation and bioavailability from Agaricus bisporus button mushroom treated with ultraviolet irradiation. J Agric Food Chem 57:3351–3355
Phillips K, Ruggio D, Horst R, Minor B, Simon R, Feeney M, Byrdwell W, Haytowitz D (2011) Vitamin D and sterol composition of ten types of mushrooms from retail suppliers in the United States. J Agric Food Chem 59:7841–7853
Babu U, Balan K, Amankwa-Sakyi M, Garthoff L, Calvo M (2011) Assessment of immuno-modulatory effects of vitamin D2-enriched mushroom consumption on LPS response using splenocyte microarray of genes regulating inflammatory cytokines, chemokines and their receptors. Mol Nutr Food Res, submitted for publication
Garthoff L, Sobotka T (2001) From farm to table to brain: foodborne pathogen infection and the potential role of the neuro-immune-endocrine system in neuro sequelae. Nutr Neurosci 4:333–374
Fleet J, Gliniak C, Xue Y, Smith K, McCreedy R, Adedokun S (2008) Serum metabolite profiles and target tissue gene expression define the effect of cholecalciferol intake on calcium metabolism in rats and mice. J Nutr 138:1114–1120
Mattila P, Lampi A-M, Ronkainen R, Tovio J, Piironen V (2002) Sterol and vitamin D2 contents in some wild and cultivated mushrooms. Food Chem 76:293–298
Jasinghe V, Perera C (2006) Ultraviolet irradiation: the generator of vitamin D2 in edible mushrooms. Food Chem 95:638–643
Müller R, Koller B, Hildebrand T, Laib A, Gianolini S, Rüegsegger P (1996) Resolution dependency of microstructural properties of cancellous bone based on three-dimensional mu-tomography. Technol Health Care 4:113–119
Hildebrand T, Rüegsegger P (1997) Quantification of bone microarchitecture with the structure model index. Comput Methods Biomech Biomed Eng 1:15–23
Hildebrand T, Laib A, Müller R, Dequecker J, Rüegsegger P (1999) Direct three-dimensional morphometric analysis of human cancellous bone microstructural data from spine, femur, iliac crest and calcaneus. J Bone Miner Res 14:1167–1174
Bills C, Eisenberg H, Pallante S (1974) Complexes of organic acids with calcium phosphate: the Von Kossa stain as a clue to the composition of bone mineral. Johns Hopkins Med J 128:194–207
Institute of Medicine, Food and Nutrition Board (2011) Dietary reference intakes for calcium and vitamin D; National Academy of Science (NAS). The National Academy Press, Washington, DC
Armas L, Hollis B, Heaney R (2004) Vitamin D2 is much less effective than vitamin D3 in humans. J Clin Endocrinol Metab 89:5387–5391
Horst R, Napoli J, Littledike T (1982) Discrimination in the metabolism of orally dosed ergocalciferol and cholecalciferol by the pig, rat and chick. Biochem J 204:185–189
Hunt R, Garcia F, Walsh R (1972) A comparison of the toxicity of ergocalciferol and cholecalciferol in rhesus monkeys. J Nutr 102:975–986
Stephenson D, Peiris A (2009) The lack of vitamin toxicity and megadose of daily ergocalciferol (D2) therapy: a case report and literature review. Southern Med J 102:765–768
Binkley N, Gemar D, Engelke J, Gangnon R, Ramamurthy R, Krueger D, Drezner M (2011) Evaluation of ergocalciferol and cholecalciferol dosing, 1,6000 IU daily or 50,000 IU monthly in older adults. J Clin Endocrinol Metab 96:981–988
Ouitila T, Mattila P, Piironen V, Lambert-Allardt C (1999) Bioavailability of vitamin D from wild edible mushrooms (Cantharellus tubaeformis) as measured with a human bioassay. Am J Clin Nutr 69:95–98
Ozzard A, Hear G, Morrison G, Hoskin M (2009) Vitamin D deficiency treated by consuming UVB-irradiated mushrooms. Br J Gen Pract 58:644–645
Urbain P, Singler F, Ihorst G, Biesalski, Bertz H (2011) Bioavailability of vitamin D2 from UV-B-irradiated button mushrooms in healthy adults deficient in serum 25-hydroxyvitamin D: a randomized controlled trial. Euro J Clin Nutr 65:965–971
Tjellesen L, Hummer L, Christiansen C, Rodbro P (1986) Serum concentration of vitamin D metabolites during treatment with vitamin D2 and D3 in normal premenopausal women. Bone Miner 1:407–413
Lee A, Anderson P, Sawyer R, Moore A, Forwood M, Steck R, Morris H, O’Loughlin P (2010) Discordant effects of vitamin D deficiency in trabecular and cortical bone architecture and strength in growing rodents. J Steroid Biochem Mol Biol 121:284–287
Biancuzzo R, Young A, Bilbuld D, Cai M, Winter M, Klein E, Ameri A, Salameh W, Chen T, Holick M (2010) Fortification of orange juice with vitamin D2 or vitamin D3 is as effective as an oral supplement in maintaining vitamin D status in adults. Am J Clin Nutr 91:1621–1626
Monsivais P, Aggarwal A, Drewnowski A (2011) Following federal guidelines to increase nutrient consumption may lead to higher food costs for consumers. Heal Aff 30:1–7
Khadilkar A, Sayyad M, Sanwalka N, Bhandari D, Naik S, Khadilkar V, Mughal M (2010) Vitamin D supplementation and bone mass accrual in underprivileged adolescent Indian girls. Asia Pac J Clin Nutr 19:465–472
Boas S, Hageman J, Ho L, Liveris M (2009) Very high-dose ergocalciferol is effective for correcting vitamin D deficiency in children and young adults with cystic fibrosis. J Cyst Fibros 8:270–272
Sources of support
The Mushroom Council, and the US FDA Centers for Food Safety and Applied Nutrition and Devices and Radiological Health.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
The findings and conclusions presented in this manuscript are those of the authors and do not necessarily represent the views or opinions of the US FDA.
Rights and permissions
About this article
Cite this article
Calvo, M.S., Babu, U.S., Garthoff, L.H. et al. Vitamin D2 from light-exposed edible mushrooms is safe, bioavailable and effectively supports bone growth in rats. Osteoporos Int 24, 197–207 (2013). https://doi.org/10.1007/s00198-012-1934-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-012-1934-9