Abstract
Summary
Decreased serum sclerostin was evident in patients with primary hyperparathyroidism and was inversely related to parathyroid hormone (PTH). Sclerostin normalized earlier than biochemical bone turnover markers (BTMs) following parathyroidectomy.
Introduction
There is limited information on the changes of serum sclerostin in conditions with chronic PTH excess in humans. The main objectives of the present study were to: (1) examine cross-sectionally the changes of serum sclerostin levels in patients with primary hyperparathyroidism (PHPT), (2) study the time course changes in serum sclerostin in PHPT patients following parathyroidectomy (PTX) followed up longitudinally for 12 months, and (3) compare the changes in serum sclerostin to that of BTMs.
Methods
We studied 60 PHPT patients and compared them with 74 PTX patients together with 268 age- and sex-matched healthy controls. Also, we followed 27 PTX patients longitudinally at 2, 4, 6, 10, 30, 60, 180, and 360 days postoperatively. Serum sclerostin, BTMs, and minerals were measured. Also, bone mineral density was determined by dual energy X-ray absorptiometry.
Results
Patients with PHPT exhibited significantly lower mean serum sclerostin [mean, in picomoles per liter; 95% confidence interval (CI)] (28.98; 27.94–30.03) than that obtained for PTX patients (37.01; 35.75–38.27) and healthy controls (46.22; 45.13–47.31) (P < 0.0001, for each case), respectively. Serum PTH inversely correlated with serum sclerostin (r = −0.651, P < 0.0001). Serum sclerostin was normalized in PTX patients by the tenth day postoperatively and remained within the expected reference range thereafter.
Conclusions
Significantly decreased serum sclerostin was evidenced in PHPT patients as compared with PTX and euparathyroid controls. The inverse PTH and sclerostin relationship suggests that sclerostin is downregulated by PTH in humans. Serum sclerostin normalized earlier than BTMs following parathyroidectomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
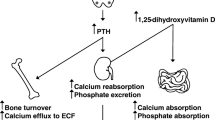
Sclerostin is a glycoprotein, coded for by the SOST gene, produced almost exclusively by osteocytes [and to a lesser extent by other cell types (kidney, vascular)] [1], and is considered to be a potent inhibitor of osteoblastogenesis. After secretion by osteocytes, sclerostin travels via the canaliculi to the bone surface where it binds to co-receptors low density lipoprotein receptor-related protein (LRP) five and LRP six and prevents colocalization with frizzled protein and Wnt signaling pathway, thus reducing osteoblastogenesis and bone formation [2–4]. In humans, the significance of sclerostin is highlighted by two genetic disorders associated with significant progressive increases in bone mass namely: sclerosteosis and van Buchem's disease [5–7]. Recently, Mirza et al. demonstrated in a small group of 20 postmenopausal women significant negative correlations between serum sclerostin, free-estrogen index, and PTH levels [8]. Furthermore, SOST-null mice have a high bone-mass phenotype, [9] and overexpression of normal human SOST alleles in mice causes osteopenia [10]. These observations suggested that inhibition of sclerostin may have therapeutic potentials for treating low bone mass disorders [11]. Indeed, recent studies demonstrated that using anti-sclerostin neutralizing antibodies in rats [12] and primates [13] increased bone density and bone strength. More recently, Padhi et al. showed that treatment of postmenopausal women with anti-sclerostin resulted in dose-dependent increased bone formation markers [14]. Very recently, van Lierop et al. demonstrated significantly lower sclerostin levels in 34 patients with primary hyperparathyroidism (PHPT) as compared with 54 euparathyroid patients following the PHPT treatment and suggested that sclerostin is downregulated by PTH in humans [15]. In an extension of these studies, the main objectives of the present study are to: (1) examine cross-sectionally the changes in serum sclerostin levels in patients with PHPT as compared with euparathyroid patients, (2) study the time course changes in serum sclerostin levels following parathyroidectomy in patients with PHPT followed up longitudinally for a period of 12 months, and (3) compare the changes in serum sclerostin with that of BTMs, namely: serum osteocalcin (s-OC), serum bone-specific alkaline phosphatase (s-bone-ALP), serum procollagen type 1 N-terminal propeptide (s-PINP), serum cross-linked C-terminal telopeptide of type 1 collagen (s-CTX), urinary N-terminal telopeptide collagen (u-NTX), and serum tartrate-resistant acid phosphatase isoform-5b (s-TRACP-5b), respectively.
Subjects and methods
Study design
During the period of January 2007 and December 2009, a total of 80 consecutive patients (44 men and 36 women) with untreated persistent PHPT and 85 patients (44 men and 41 women) cured following successful parathyroidectomy [euparathyroid controls (PTX)] (from patients attending outpatient clinics at King Abdulaziz University Hospital, New Jeddah Clinic Hospital, and Al-Khandara Clinic Hospital) together with 330 healthy age- and sex-matched controls who all agreed to participate in the present study were studied. Subjects were asked to visit a special clinic at the Center of Excellence for Osteoporosis Research (CEOR), King Abdulaziz University, Jeddah, to be enrolled in the study. Age, body weight, height, and body mass index (BMI; kilograms/square meter) were recorded. All subjects were medically examined and interviewed using standardized questionnaire to collect information on lifestyle, smoking habits, level of physical activity in leisure time, and the use of vitamins and medications as described previously [16]. Subjects with chronic diseases including osteoarthritis or established osteoporosis, with evident endocrine disorders (except PHPT patients), or on any of drug treatment (including postmenopausal hormonal replacement therapy) with possible effect on bone metabolism (e.g., selective estrogen receptor modulators, calcitonin, phytoestrogens, anti-convulsants, thyroid hormones, bisphosphonates, and/or glucocorticoids) were excluded from the final analysis. Subjects who reported a recent clinical fracture (within 2 years), were pregnant or lactating, taking oral contraceptives (for women), or had missing data for final analysis were also excluded. Accordingly, 60 patients (33 men and 27 women) with untreated PHPT and 74 patients (38 men and 36 women) with PTX together with 268 healthy age- and sex-matched controls were studied and included in the final analysis.
In addition, all included subjects exhibited normal complete blood count and renal (serum creatinine in women <105 μmol/l and in men <120 μmol/l) and hepatic function tests (serum aspartate aminotransferase <30 U/l, alkaline phosphatase between 80 and 280 U/l, and gamma-glutamyl transferase <60 U/l). In the present study, PHPT was defined as serum intact PTH levels greater than the upper limit of normative reference values used in CEOR (i.e., >8.0 pmol/l) in the presence of increased serum calcium levels >2.60 mmol/l. Patients with PTX were included when cure was confirmed by postoperative normalization of serum intact PTH and calcium levels, which continued for a period not less than 12 months following parathyroidectomy. Healthy age- and sex-matched controls (144 men and 124 women) were selected from the pool of healthy subjects attending the clinics of CEOR for bone health assessment and enrolled in the study as described previously [17], and all had normal serum intact PTH (<8.0 pmol/l) and calcium (<2.50 mmol/l) levels. Subjects enrolled in the present study underwent BMD determinations and provided blood and urine samples for the measurements of serum sclerostin, various hormones, and biochemical BTMs together with other relevant analytes.
A subgroup of 31 patients with PHPT (13 women and 14 men; age, 50.30 ± 6.35 years) was followed up longitudinally for a period of 12 months following successful parathyroidectomy. They were among the 74 patients that were included in the present cross-sectional study (i.e., postoperative PTX) and were asked to participate in the follow-up study on the effects of parathyroidectomy on the time course changes of serum as compared with various BTMs. However, four patients refused to complete the follow-up examinations. All remaining 27 patients had normal serum calcium levels postoperatively. The results of this subgroup of patients were compared with that of age- and sex-matched healthy controls described in the present study. Then all patients were examined as described above, underwent BMD determinations (basal and 6 and 12 months postoperatively), and provided blood and urine samples at 0, 2, 4, 6, 10, 30, 60, 180, and 360 days postoperatively for the measurements of serum sclerostin, various hormones, minerals, and BTMs together with relevant analytes as described below. In the two studies, informed consent was obtained from each participant prior to inclusion into both studies. The protocols of both studies were in agreement with the CEOR's ethical standards and the Helsinki Declaration of 1975 as revised in 1989. Both studies were also approved by CEOR's Human Ethics Research Committee.
Specimen collection
Venous blood samples were collected in the morning under standardized conditions between 9:00 and 11:00 a.m. after an overnight fast together with second-void morning urine samples. Serum and urine samples were stored at −85°C within 30 min after centrifugation at 2,500×g for 10 min. The samples were stored until analyzed for the determinations of serum sclerostin and BTMs. Serum sclerostin, BTMs, and other analytes were performed at the same time point according to the manufacturer's instructions.
Measurements of hormones and other analytes
Serum intact PTH and serum 25-hydroxyvitamin D [25(OH)D] together with other analytes were measured by commercially available immunoassays as described previously [18].
Measurements of sclerostin and biochemical BTMs
Serum sclerostin levels were measured on coded specimen using enzyme-linked immunosorbent assay supplied by Biomedica (Biomedica Gruppe, Biomedica Medizinprodukte GmbH & Co KG, Wien, Austria). This assay uses a polyclonal goat antihuman sclerostin antibody as a capture antibody and a biotin-labeled mouse monoclonal anti-sclerostin antibody for detection. The assay had a range of 0 to 240 pmol/l with a detection limit at 3.60 pmol/l. None of the measured values for sclerostin in the subjects of the present study were below the limits of detection for the assay. Serum samples with high sclerostin were used as quality control to confirm the specificity for endogenous sclerostin, and these endogenous controls were determined reproducibly over time as a measure of the assay reproducibility. The intra- and inter-assay CVs were 4.5% and 5.6%, respectively. Results of further validation of the assay of sclerostin are presented in Table 1. Thus, linearity was assessed by serially diluting serum samples with sample diluents (dilutions 1:2, 1:4, and 1:8) and comparing observed values with expected values (observed recoveries ranged from 100% to 108%) (Table 1). Also, recovery of spiked exogenous sclerostin was tested by adding different concentrations of exogenous human recombinant sclerostin (supplied by R&D Systems, Minneapolis, MN, USA) (three different concentrations) into eight different human serum samples presenting with various levels of endogenous sclerostin. Spiked recovery ranged from 93% to 108% for a typical sample presented in Table 1. Human sclerostin used was found to be stable (as demonstrated by SDS-PAGE) according to the manufacturer's instructions. Serum intact OC and other biochemical BTMs were measured by methods described previously [18].
Bone mineral densitometry measurements
BMD (grams/square centimeter) was determined for the anteroposterior lumbar spine (L1–L4) and mean of proximal right and left femur (total and sub-regions) by dual energy X-ray absorptiometry using (LUNAR Prodigy Model, Lunar Corp., Madison, WI), according to standard protocol. Quality control procedures were carried out in accordance with the manufacturer's recommendations as described previously [19]. BMD values were classified according to WHO criteria: a T-score between −1 and −2.5 is indicative of osteopenia, while a T-score lower than −2.5 reflects osteoporosis, and a T-score higher than −1 is considered normal [20].
Statistical analysis
Results are presented as means (±SD), and categorical variables are expressed as frequencies as appropriate. Data were analyzed using SPSS-Statistical Package (version 15.0 for Windows Smart Viewer) supplied by SPSS Inc. 2000, Mapinfo Corp. Tokyo, NY, USA. Results that were not normally distributed were log-transformed before analysis. A P value <0.05 is considered statistically significant. All subjects were stratified by parathyroid hormone status to assess variations in serum sclerostin and BTMs together with other variables using one-way ANOVA testing, and descriptive statistics for variables were reported. Associations between continuous variables were examined by Pearson's correlation co-efficient and partial correlation analysis after adjustment for age and/or BMI. For the longitudinal part of the study, the Mann–Whitney U test was used for comparisons between groups. The Friedman repeated analysis of variance on ranks was used for examining changes over time, and results from the various follow-up points were evaluated against baseline employing Dunn's method of multiple comparisons.
Results
The main anthropometric and clinical characteristics of the studied men and women (cross-sectional study) are presented in Table 2. There were no marked differences with respect to age, sex, and BMI; however, patients with PHPT exhibited significantly lower values for BMD for the lumbar spine (L1–L4) and neck femur, as compared with that for PTX and age- and sex-matched controls. As expected by the inclusion criteria, the mean serum intact PTH (P < 0.0001) and ionized calcium levels (P < 0.0001) were significantly higher and that of serum phosphate (P < 0.0001) significantly lower in the PHPT group as compared with the PTX and healthy controls (Table 1). Patients with PHPT exhibited significantly lower serum 25(OH)D values as compared with the PTX group and healthy controls. Patients with PHPT exhibited significantly higher levels of bone formation (by 46.7% for s-OC and 44.9% for s-PINP) and resorption (by 1.7-fold for s-CTX and 72.3% for u-NTX) markers, respectively, as compared with those obtained for PTX subjects (P < 0.0001 for each case).
Patients with PHPT had significantly lower mean serum sclerostin (28.98 pmol/l; 95% CI 27.94–30.03) than that obtained for PTX subjects (37.01 pmol/l; 95% CI 35.75–38.27) and healthy controls (46.22 pmol/l; 95% CI 45.13–47.31) (P < 0.0001 for each case), respectively (Fig. 1); however, there was also a significant difference in the mean serum sclerostin values among subjects with PTX and healthy controls (P < 0.002). Serum intact PTH showed significantly negative correlations with serum sclerostin in subjects with PHPT and EuPTH (r = −0.651, P < 0.0001) (Fig. 2).
In the longitudinal follow-up study, preoperatively, all 27 patients with PHPT were hypercalcemic but with normal renal function. At baseline sampling, bone formation markers were higher by 56.8%, 74.7%, and 99.2% for s-OC, s-bone ALP, and s-PINP, respectively, as compared with age- and sex-matched healthy controls. Also, bone resorption markers were higher by 42.4%, 56.6%, and 43.7% for s-CTX, u-NTX, and s-TRACP-5b among patients with PHPT as compared, respectively, to age- and sex-matched controls. Serum sclerostin levels were decreased in patients with PHPT (by 62.9%) (P < 0.0001). Of the patients studied, 78.3% and 17.4% had serum 25(OH)D levels at <25 and <12.5 nmol/l, respectively. Immediately following parathyroidectomy, both serum and urinary calcium levels were normalized. Changes in serum sclerostin and measured BTMs are presented in Fig. 3. Serum sclerostin increased immediately following surgery [on days 2, 4, and 6 were (picomoles per liter) 22.76 ± 3.43, 27.18 ± 3.94, and 30.32 ± 4.54, respectively], returned to normal levels by the tenth day postoperatively (34.99 ± 6.53 pmol/l), and remained within expected reference values for the age group of healthy subjects throughout the follow-up period. All BTMs declined significantly during the follow-up period (Fig. 3). Serum CTX (decreased by 13.6–44.8%) and uNTX (decreased by 10.2–33.8%) exhibited the highest decrease in values following surgery as compared with other BTMs, respectively. All showed significant decline by the first month postoperatively, attained expected reference values within the first 6 months, and remained so throughout the follow-up period of 12 months.
Serum sclerostin a and biochemical BTM b–g levels in 27 patients following parathyroidectomy and followed for 12 months. Serum sclerostin and all BTMs change significantly over time (Friedman's repeated analysis of variance on ranks, P < 0.001). Asterisks, values significantly different from baseline (day 0) values (Dunn's method *P < 0.01, **P < 0.001). Dashed lines represent 95% confidence intervals of reference values used in CEOR for sclerostin and BTMs measured
The BMD values at all sites measured showed significant increases by 12 months postoperatively: the increase in BMD was 3.2% in the lumbar spine (L1–L4) (P < 0.001), 3.1% in total hip (P < 0.001), 3.9% in the trochanter (P < 0.001), and 3.4% in the neck femur (P < 0.001), respectively (data not shown).
Discussion
In the present study, serum sclerostin levels were measured using a commercially available immunoassay that has been validated and used by other studies [21–23]. Recently, McNulty et al. compared the immunoassay used in the present study with another commercially available one (obtained from TECO-Medical, AG, Sissach, Switzerland) and concluded that the same sclerostin immunoassay should be used for comparing groups of patients or patients being followed longitudinally [24]. The present study is the first longitudinal study after parathyroidectomy showing the longitudinal changes in serum sclerostin as compared with that obtained for BTMs. In addition, our findings from the cross-sectional part of the present study confirm that serum sclerostin is lower in patients with chronic PTH excess due to PHPT as compared with that of PTX and age- and sex-matched healthy controls, as observed very recently by van Lierop et al. [15] in patients with PHPT. Also, in the present study, healthy controls had higher serum sclerostin levels than that of euparathyroid PTX subjects, where the opposite was seen in the study of van Lierop et al. [15] (i.e., being intermediate between values of patients with HPHT and that of euparathyroid PTX subjects). Such differences could be related to variations in the demographic characteristics of the populations studied including age, the levels of serum PTH, and the stage of the disease as well as the percentage of men and women contributing to the two populations. Thus, the cross-sectional results, showing lower sclerostin levels in PTX patients as compared with corresponding healthy controls, are consistent with the longitudinal results showing that serum sclerostin values normalize following parathyroidectomy. Moreover, we observed a significant inverse correlation between serum sclerostin and intact PTH levels. Patients with PHPT exhibited significantly higher degree of bone turnover as indicated by higher values for both bone formation and resorption markers confirming previous studies [17, 19]. Also, the results of the present study confirm that patients who were followed up for a period of 12 months, following parathyroidectomy, within 1 month attained normalization of serum sclerostin levels similar to the values of age- and sex-matched healthy controls. However, measured BTMs normalized within the first 6 months postparathyroidectomy. It is important to state that we have chosen to study patients with PHPT in order to simulate in vivo, as closely as possible, the effect of chronic excess of PTH on sclerostin, as previously demonstrated in experimental animals [11]. Moreover, we selected to use patients after parathyroidectomy and cured of PHPT as controls (PTX) to exclude the expected potential confounding factors, other than the excess of PTH associated with PHPT. The results of the present study corroborate and extend the observations by other studies on the changes in biochemical BTMs in PHPT, with increases in both resorption and to a lesser extent formation markers [17, 19, 25, 26]. Thus, the findings of the present study reveal that the increase in serum sclerostin and the decrease in biochemical BTMs do not continue beyond the first month and the first 6 months following parathyroidectomy, respectively, and that normalization of serum sclerostin seems to occur earlier than that for the biochemical BTMs measured. Our results show that serum sclerostin is associated with bone response to chronic PTH excess in patients with PHPT, possibly partly through removing the antagonizing effect on the Wnt/β-catenin signaling. This observation may be of relevance in the long-term therapy in patients with PHPT. In such patients, the bone resorption rate is much higher than that for the formation rate, indicating that the compensatory increase in bone formation rate is impaired. However, given the exclusive expression of sclerostin in osteoblasts/osteocytes in bone, the lowered serum sclerostin levels in the face of chronic elevation of PTH might be a possible compensatory mechanism to correct for the lowered rate of bone formation to counteract the higher rate of bone resorption associated with PHPT. Such suggestion may explain the observed changes in serum sclerostin among patients with PHPT, although other mechanisms could be involved. The PHPT patients in the present study were, however, a small group of subjects, possibly resulting in reduced statistical power. However, since they were compared with age- and sex-matched treated patients who had PHPT prior to therapeutic intervention, together with the observed changes in sclerostin levels in PTX patients followed up longitudinally for 12 months, lend further support to confirm the action of normalizing sclerostin levels by the endogenous changes in serum intact PTH levels.
Recent studies showed that the positive effect of chronic PTH excess on osteoblastogenesis could result from actions of the hormone on osteocytes via changes in the expression of SOST. Consistent with the evidence that SOST is upregulated by Runx2 (osteoblast specific transcription factor required for anti-apoptotic effect of PTH) [27] and that PTH induces proteasomal degradation of Runx2 protein [28], chronic excess of PTH significantly decreases the expression of SOST-mRNA and sclerostin in osteocytes both in vivo and in vitro [11]. In addition, PTH had a positive stimulatory effect on the production of other growth factors [29] by stromal/osteoblastic cells and increased osteoclastic bone resorption which resulted in the release of TGFβ from bone matrix [30], thus increasing osteoclast number without affecting osteoblast apoptosis [11]. Moreover, recent studies in humans showed that intermittent PTH therapy of postmenopausal women resulted in marked decreases in serum sclerostin levels and enhanced bone formation [31]. Taken all together with findings of the present study, these lend further support to the hypothesis that, in humans and experimental animals, at least part of the anabolic effect of PTH on bone may be mediated via an inhibition of sclerostin production and/or stimulation of its clearance or increased osteoblasts production and/or decreased osteoblastic apoptosis due to a decrease in Runx2 levels below the threshold needed for survival signaling. Accordingly, it is possible that the sclerostin-mediated effects of PTH on osteoblastogenesis are amplified by the above-mentioned actions.
The strengths of the present study include its reasonably large sample size of patients with PHPT including the control groups, PTX, and age- and sex-matched healthy controls with strict detailed inclusion criteria including BMD measurements. In addition, we examined the changes in serum sclerostin and BTM levels among PHPT patients followed up for a period of 12 months. Moreover, both serum sclerostin and intact PTH levels were determined with minimized pre-analytical variations due to possible circadian rhythm and/or food intake: standardized the sampling time with samples obtained following overnight fasting. Thus, the main limitations of the present study were its cross-sectional design, and hence not sufficient to demonstrate causality, and its being based on a single measurement of serum sclerostin and intact PTH levels. Although, the serial measurements of serum sclerostin, intact PTH, and BTMs among the 27 patients following parathyroidectomy lend stronger support to the interaction between serum sclerostin and that of intact PTH, further studies are needed to explore the relationship between both sclerostin and PTH. Finally, we recognize that there is currently no information on the stability of sclerostin or its degradation in circulation and/or upon storage at −85°C; further studies are needed in this regard.
In conclusion, our results show that serum sclerostin is decreased in patients with PHPT as compared with that with PTX or age- and sex-matched healthy controls and that it normalizes earlier than BTMs following parathyroidectomy in parallel with the normalization of PTH, suggesting that sclerostin is downregulated by endogenous PTH in humans. Thus, the actions of PTH on bone appear to be complex and involved a variety of signaling pathways in bone marrow stroma cells, osteoblasts, and osteocytes [32, 33]. Further studies are needed to explore the molecular mechanisms that describe the actions of PTH on bone remodeling and bone balance including those related to its interaction with sclerostin. It is suggested that measuring serum sclerostin and BTMs simultaneously may prove helpful in evaluating and/or monitoring the changes in the rate of bone turnover and osteocytic function caused by primary hyperparathyroidism or in other bone-diseased states in humans (including osteoporosis, renal osteodystrophy, and arthritis) as well as disease states in patients with myeloma, hemodialysis, and/or cardiovascular disease. Further studies are warranted in this respect.
References
Silvestrini G, Ballanti P, Leopizzi M, Sebastiani M, Berni S, DiVitro M, Bonucci E (2007) Effects of intermittent parathyroid hormone (PTH) administration on SOST mRNA and protein in rat bone. J Molecu Histol 38:261
Kneissel M (2009) The promise of sclerostin inhibition for the treatment of osteoporosis. IBM S BoneKEy 6:259–264
Li X, Zhang Y, Kang H, Liu W, Liu P, Zhang J, Harris SE, Wu D (2005) Sclerostin binds to LRP5/6 and antagonizes canonical Wnt signaling. J Biol Chem 280:19883–19887
Ellies DL, Viviano B, McCarthy J, Rey JP, Itasaki N, Saunders S, Krumlauf R (2006) Bone density ligand, sclerostin, directly interacts with LRP5 but not LRP5/6 and antagonizes canonical Wnt signaling. J Biol Chem 21:1738–1749
Brunkow ME, Gardner JC, Van Ness J, Paeper BW, Kovacevich BR, Proll S, Zhao L, Sabo PJ, Fu Y, Alisch RS, Gillett L, Colbert T, Tacconi P, Galas D, Hamersma H, Beighton P, Mulligan J (2001) Bone dysplasia sclerosteosis results from loss of the SOST gene product, a novel cystine knot-containing protein. Am J Hum Genet 68:577–589
Staehling-Hampton K, Proll S, Paeper BW, Zhao L, Charmely P, Brown A, Gardner JC, Galas D, Schatzman RC, Beighton P, Papapoulos S, Hamersma H, Brunkow ME (2002) A 52-kb deletion in the SOST-MEOX1 intergenic region on 17q12–q21 is associated with van Buchem disease in the Dutch population. Am J Med Genet 110:144–152
Balemans W, Patel N, Ebeling M, van Hul E, Wuyts W, Lacza C, Dioszegi M, Dikkers FG, Hildering P, Willems PJ, Verheij JB, Lindpaintner K, Vickery B, Foernzler D, van Hul W (2002) Identification of a 52 kb deletion downstream of the SOST gene in patients with van Buchem disease. J Med Genet 39:91–97
Mirza FS, Padhi ID, Raisz LG, Lorenzo JA (2010) Serum sclerostin levels negatively correlate with parathyroid hormone levels and free estrogen index in postmenopausal women. J Clin Endocrinol Metab 95:1991–1997
Li X, Ominsky MS, Niu Q-T, Sun N, Daugherty B, D'Agostin D, Kurahara C, Gao Y, Cao J, Gong J, Asuncion F, Barrero M, Warmington K, Dwyer D, Stolina M, Morony S, Sarosi I, Kostenuik PJ, Lacey DL, Simonet WS, Ke HZ, Paszty C (2008) Targeted deletion of the sclerostin gene in mice results in increased bone formation and bone strength. J Bone Miner Res 23(6):860–869
Winkler DG, Sutherland MK, Geoghegan JC, Yu C, Hayes T, Skonier JE, Shpektor D, Jonas M, Kovacevich BR, Staehling-Hampton K, Appleby M, Brunkow ME, Latham JA (2003) Osteocyte control of bone formation via sclerostin, a novel of BMP antagonist. EMBO J 22:6267–6276
Bellido T, Ali AA, Gubrij I, Plotkin LI, Iu Q, O'brien CA, Manolagas SC, Jilka RL (2005) Chronic elevation of parathyroid hormone in mice reduces expression of sclerostin by osteocytes: a novel mechanism for hormonal control of osteoblastogenesis. Endocrinology 146:4577–4583
Li X, Omnisky MS, Warmington KS, Morony S, Gong J, Cao J, Gao Y, Shlhoub V, Tipton B, Haldankar R, Chen Q, Winters A, Boone T, Geng Z, Niu QT, Ke HZ, Kostenuik PJ, Simonet WS, Lacey DL, Paszty C (2009) Sclerostin antibody treatment increases bone formation, bone mass and bone strength in a rat model of postmenopausal osteoporosis. J Bone Miner Res 24(4):578–588
Ominsky MS, Vlasseros F, Jolette J, Smith SY, Stouch B, Doellgast G, Gong J, Gao Y, Cao J, Graham K, Tipton B, Cai J, Deshpande R, Zhou L, Hale MD, Lightwood DJ, Henry AJ, Popplewell AG, Moore AR, Robinson MK, Lacey DL, Simonet WS, Paszty C (2010) Two doses of sclerostin antibody in cynomolgus monkeys increases bone formation, bone mineral density, and bone strength. J Bone Miner Res 25(5):948–959
Padhi D, Jang G, Stouch B, Fang L, Posvar E (2011) Single-dose, placebo-controlled, randomized study of AMG785, a sclerostin monoclonal antibody. J Bone Miner Res 26(1):19–26
van Lierop AH, Witteveen JE, Hamdy NAT, Papapoulos SE (2010) Patients with primary hyperparathyroidism have lower circulating levels than euparathyroid controls. Eur J Endocrinol 163:833–837
Ardawi M-SM, Qari MH, Rouzi AA, Maimani AA, Radaddi RM (2010) Vitamin D status in relation to obesity, bone mineral density, bone turnover markers and vitamin D receptor genotypes in healthy Saudi pre- and postmenopausal women. Osteoporos Int 22:462–475
Christiansen P, Steiniche T, Brixen K, Hessov I, Melsen F, Heickendroff L, Mosekilde LE (1999) Primary hyperparathyroidism: short-term changes in bone remodeling and bone mineral density following parathyroidectomy. Bone 25(2):237–244
Ardawi M-SM, Maimani AA, Bahksh TA, Rouzi AA, Qari MH, Radaddi RM (2010) Reference intervals of biochemical bone turnover markers for Saudi Arabian women: a crosssectional study. Bone 47:804–814
Christianser P, Steiniche T, Brixen K, Hessov I, Melsen F, Heickendroff L, Mosekilde LE (1999) Primary hyperparathyroidism: effect of parathyroidectomy on regional bone mineral density in Danish patients: a three-year follow-up study. Bone 25(5):589–595
World Health Organization (1994) Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. Technical Report Series. WHO, Geneva, No. 843
Gaudio A, Pennisi P, Bratengeir C, Torrisi V, Linder B, Mangiafico RA, Pulvirenti I, Hawa G, Tringali G, Fiorce CE (2010) Increased sclerostin serum levels associated with bone formation and resorption markers in patients with immobilization-induced bone loss. J Clin Endocrinol Metab 95:2248–2253
Modder UIL, Clowes JA, Hoey K, Peterson JM, McCready L, Oursler MJ, Riggs BL, Khosla S (2011) Regulation of circulating sclerostin levels by sex steroids in women and men. J Bone Miner Res 26(1):27–34
Modder UI, Hoey KA, Amin S, McCready LK, Chenbach SJ A, Riggs BL, Melton LJ III, Khosla S (2011) Relation of age, gender and bone mass to circulating sclerostin levels in women and men. J Bone Miner Res 26(2):373–379
McNulty M, Singh RJ, Li X, Bergstralh EJ, Kumar R (2011) Determination of serum and plasma sclerostin concentrations by enzyme-linked immunoassays. J Clin Endocrinol Metab 96:E1159–E1162
Guo CY, Thomas WE, AlDehaimi AW, Assiri AM, Eastell R (1996) Longitudinal changes in bone mineral density and bone turnover in postmenopausal women with primary hyperparathyroidism. J Clin Endocrinol Metab 81:3487–3491
Osterode W, Winker R, Bieglmayer C, Vierhapper H (2004) Effects of parathyroidectomy on lead mobilization from bone in patients with primary hyperparathyroidism. Bone 35:942–947
Bellido T, Ali AA, Plotkin LI, Fu Q, Gubrij I, Roberson PK, Weinstein RS, O'Brien CA, Manolagas SC, Jilka RL (2003) Proteasomal degradation of Runx2 shortens parathyroid hormone-induced anti-apoptotic signaling in osteoblasts. A putative explanation for why intermittent administration is needed for bone anabolism. J Biol Chem 278:50259–50272
Keller H, Kneissel M (2005) SOST is a target gene for PTH in bone. Bone 37:148–158
Aubin JE, Heersche JNM (2001) Cellular actions of parathyroid hormone on osteoblast and osteoclast differentiation. In: Bilezikian JP, Marcus R, Levine MA (eds) The parathyroids. Basic and clinical concepts. Academic, San Diego, pp 199–211
Pfeilschifter J, Munday GR (1987) Modulation of type β transforming growth factor activity in bone cultures by osteoporotic hormones. Proc Natl Acad Sci USA 84:2024–2028
Drake MT, Srinivasan B, Modder UI, Peterson JM, McCready LK, Riggs BL, Dwyer D, Stolina M, Kostenuik P, Khosla S (2010) Effects of parathyroid hormone treatment on circulating sclerostin levels in postmenopausal women. Bone Miner Res 95(11):5056–5062
Datta NS, Abou-Samra AB (2009) PTH and PTHrP signaling in osteoblasts. Cell Signal 21:1245–1254
Jilka RL (2007) Molecular and cellular mechanisms of the anabolic effect of intermittent PTH. Bone 40:1434–1446
Acknowledgments
We are grateful to the Ministry of Higher Education for financial support to the Center of Excellence for Osteoporosis Research (CEOR) at King Abdulaziz University (grant #s CEOR/001-08 and CEOR/004-08), Jeddah, Saudi Arabia. We thank Dr. M. Bellal and Dr. A.A. Yousif at the Department of Surgery of the New Jeddah Clinic Hospital for their help in the longitudinal study of the present work. We thank all the subjects who participated in the present study, and we thank all the staff and colleagues at CEOR, King Abdulaziz University Hospital, New Jeddah Clinic Hospital, Al-Khandara Clinic Hospital, and the Primary Care Health Centers for their invaluable assistance during the execution of the present study. Special thanks are due to Ms. Veronica Orbacedo for her excellent secretarial help.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ardawi, MS.M., Al-Sibiany, A.M., Bakhsh, T.M. et al. Decreased serum sclerostin levels in patients with primary hyperparathyroidism: a cross-sectional and a longitudinal study. Osteoporos Int 23, 1789–1797 (2012). https://doi.org/10.1007/s00198-011-1806-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-011-1806-8