Abstract
Summary
Vertebral fracture assessment (VFA) with densitometric devices uses less radiation than spinal radiography. We assessed risk of new vertebral fracture (VF) in women with baseline fracture identified on VFA using algorithm-based qualitative diagnosis. Women with VF had significantly greater risk of VF after 6 years compared to those without baseline fracture.
Introduction
Prevalent VFs predict future fracture and are identifiable on vertebral fracture assessment (VFA) using bone densitometry devices. We have previously performed cross-sectional, but not longitudinal, VFA using the algorithm-based qualitative method (ABQ). We aimed to examine the prevalence and incidence of VF and test the association between prevalent and incident VF identified by ABQ VFA.
Methods
We used ABQ to assess vertebral images obtained at baseline and 6 years (Hologic devices) in 674 women at ages 39 to 80 years participating in the Osteoporosis and Ultrasound Study. Criteria for prevalent and incident VF were endplate fracture, with/without cortical fracture. We compared proportions (chi-squared test) and characteristics (two-sample t tests and analysis of variance) of women with and without VF and calculated odds ratios for incident VF in women with prevalent VF (logistic regression).
Results
Prevalent VF was identified in one premenopausal woman and 41 postmenopausal women. Incident VF was identified in 18 postmenopausal women. Odds ratios (95% CI) for incident VF in postmenopausal women with prevalent VF were 7.8 (2.8, 22.1) (unadjusted) and 4.3 (1.4, 13.7) (adjusted for age and bone mineral density, BMD). Women with prevalent or incident VF were older (P < 0.01), with lower hip BMD (P < 0.001) compared to women without VF.
Conclusions
Population-based postmenopausal women had relatively low prevalence and incidence of VF analysed with the ABQ method applied to VFA. Women with prevalent fracture had a significantly greater risk of incident VF than women without prevalent fracture.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Baseline (prevalent) vertebral fracture is a powerful independent predictor of future fracture risk [1], but many fractures do not come to clinical attention. One of the reasons for this is that spinal radiographs are not routinely obtained due to the risks of exposure to ionising radiation. However, diagnostic vertebral images can now be obtained by means of x-ray absorptiometry. This technique, known as vertebral fracture assessment (VFA), uses less radiation than is required to obtain a conventional radiograph of the spine [2]. The approach recommended by the International Society for Clinical Densitometry for definition of fractures in VFA is the identification of vertebral height that is at least 20% shorter than expected [3, 4]. This approach is based on the Genant semiquantitative classification [5] which is integrated into the vertebral analysis software on both Hologic and GE Lunar devices. Fractures may be identified visually and confirmed quantitatively using the manufacturer's analysis software.
In Sheffield, we use a diagnostic approach that requires evidence of endplate fracture, with no minimum requirement for apparent reduction in vertebral height, namely the algorithm-based qualitative method (ABQ) [6]. We have published data on the application of the ABQ method to VFA for visual diagnosis of prevalent vertebral fractures [7, 8], but have not previously used the method in longitudinal VFA. Image quality is an important consideration in the ABQ definition of fracture, because of the emphasis on visual assessment of the endplate. We wished to evaluate the accuracy of the ABQ definition of prevalent vertebral fracture on VFA by testing the association with incident vertebral fractures. The main aim of this study was to test the association between prevalent and incident vertebral fractures identified by ABQ on VFA. We also wished to examine the frequency of prevalent and incident vertebral fracture identified using this approach.
Methods
Study participants
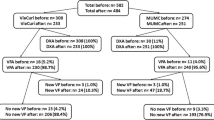
We analysed vertebral images obtained from women participating in the population-based Osteoporosis and Ultrasound Study (OPUS). This was a prospective study based in five European centres, namely Aberdeen (Department of Rheumatology, NHS Grampian, in association with the University of Aberdeen, Aberdeen, UK), Kiel (Medizinische Physik, Klinik fur Diagnostische Radiologie, Univesitätsklinikum Schleswig-Holstein, Campus Kiel, Kiel, Germany), Paris (Centre d'Evaluation des Maladies Osseuses, Service de Rhumatologie, Assistance-Publique, Hopital Cochin, Universite Rene Descartes, Paris, France) and Sheffield (Metabolic Bone Centre, Northern General Hospital, UK) [9]. Baseline visits (1999 to 2001) were attended by 463 premenopausal women, ages 20–39 years, and 2,399 postmenopausal women, ages 55–80 years. Exclusion criteria for entry into the study were disorders that precluded valid quantitative ultrasound measurements or general inability to undergo the study examinations. UK women were recruited from local general practices, German women were randomly selected from government registers and French women were randomly selected from the registers of a complementary health insurance system. All study participants who had attended baseline visits were invited for follow-up visits at 6 years, and 62% of them responded positively (Fig. 1). The analysis reported here is based on a subset of women who attended both baseline and follow-up for VFA using Hologic devices, and for whom viable VFA scans were available for both visits. Thus, the subset analysis was restricted to women examined in Kiel, Paris and Sheffield. We excluded women who were scanned using Lunar GE devices (Aberdeen and Berlin) because we were unable to read these images in Sheffield. The Hologic devices in Kiel, Paris and Sheffield were upgraded between baseline and follow-up visits, which resulted in loss or corruption of some baseline scans. The final number of women included in the current analysis was 674 (73 premenopausal, 601 postmenopausal).
Vertebral imaging and bone density assessments
Vertebral images were obtained using a Hologic QDR 4500A or Discovery A densitometer (Hologic Inc, Bedford, MA). The spine was imaged in the posterior–anterior and lateral projections to include vertebrae T4 and L4. Bone density scans of the lumbar spine and hip were acquired by dual-energy x-ray absorptiometry using the same devices. Areal bone mineral density (BMD) measurements were standardised and cross-calibrated across centres; these procedures were performed at the coordinating centre in Kiel. Vertebrae were excluded from the calculation of mean BMD if there was evidence of fracture on the bone density scan; women with more than two fractures between L1 and L4 were excluded from the analysis of spine BMD. Vertebrae with evidence of degenerative change were not excluded from BMD estimates.
Assessment of vertebral images
The vertebral images were viewed using the Hologic Discovery analysis software version 12.0. Vertebrae T4 through L4 were assessed visually by a single reader (LF) using the ABQ approach [6] and blinded to the age and identity of each participant. Prevalent vertebral fractures were identified first from baseline images without reference to those acquired at follow-up. Incident vertebral fractures were identified by comparing 6-year follow-up and baseline images.
Prevalent vertebral fracture was identified on baseline images when the appearances were in keeping with endplate fracture, with or without fracture of the cortex [6]. The baseline vertebral images were categorised as either fracture-positive, when there was evidence of one or more vertebral fractures with or without the appearance of ‘reduced’ (short) vertebral height in unfractured vertebrae, or fracture-negative (no evidence of fracture). The severity of fracture was estimated subjectively. Fractures were recorded as concave (fracture at one endplate), biconcave (fracture at both endplates), wedge (concave fracture plus fracture of the anterior cortex) or crush (concave fracture plus fracture of the anterior, lateral and posterior cortices). Fractures were graded mild if vertebral height appeared reduced by up to 25% or moderate/severe if vertebral height appeared reduced by more than 25%. This approach is similar to the Genant semiquantitative (SQ) approach to grading fracture severity in which the thresholds for reduction in vertebral height are 20–25% (grade 1, mild), 25–40% (grade 2, moderate) and >40% (grade 3, severe) [5]. The difference between the ABQ and SQ methods is that when there is evidence of fracture at the endplate, there is no minimum threshold for apparent reduction in vertebral height using the ABQ method. Hence, fracture may be identified by ABQ when vertebral height appears reduced by less than 20%. Fracture and vertebral height can be difficult to assess accurately on an image affected by oblique projection due to inaccurate patient positioning or to the parallax effect (due to the divergence of the x-ray beam). These effects give the endplates an elliptical appearance that may mask, or give a false appearance of endplate fracture. When using the ABQ method, this problem is addressed by checking the symmetry of the endplates. However, the parallax effect is less problematic in VFA due to the different beam geometry used in x-ray absorptiometry, compared to conventional radiography (fan versus cone beam).
Baseline images without evidence of vertebral fracture were further sub-categorised as normal (vertebral heights appeared normal), or non-fracture short vertebral height (SVH) when one or more vertebral heights appeared ‘reduced’ (in comparison to the variation we would normally expect to see within and between vertebrae) without evidence of endplate fracture. The reason for this was to determine whether SVH was significantly associated with incident vertebral fracture, to evaluate the impact of excluding SVH from the definition of prevalent vertebral fracture. Vertebral heights were not measured, and a minimum threshold for ‘shortness’ of height compared to expected appearances was not applied.
Incident vertebral fracture was identified when the appearances of a vertebra classified fracture-negative at baseline fulfilled the ABQ criteria for definition of a prevalent vertebral fracture [6]. For the purposes of this analysis, 6-year follow-up scans were categorised as fracture-positive (one or more new vertebral fractures in previously unfractured vertebrae) or fracture-negative (no new fractures). The follow-up images were not sub-categorised by SVH because we would not expect to see significant changes from baseline within this timescale.
Data analysis
We calculated the number and percent of women with vertebral fracture at baseline and 6 years, respectively. In women who were fracture-negative at baseline, we calculated the number and percent of women with SVH. In women with incident vertebral fractures at 6 years, we compared the proportions of women who had been identified fracture-positive or fracture-negative at baseline and the proportions of women who had been identified normal/SVH at baseline (chi-squared test). Mean baseline values for age, height, weight and BMD were compared in women with and without vertebral fractures using the two-sample t test. Odds ratios (ORs) for incident vertebral fracture were calculated for women who were identified fracture-positive at baseline and for women with non-fracture SVH at baseline using logistic regression. We also performed logistic regression with adjustment for baseline variables that were significantly associated with presence of vertebral fracture. Statistical analysis was performed using MedCalc® version 11.3.3.0 (MedCalc Software bvba) and SPSS version 12. We used a threshold of P < 0.05 to indicate statistical significance.
Results
Frequency of vertebral fracture at baseline and 6-year follow-up
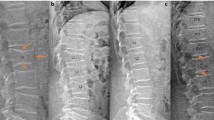
In this subset of the OPUS population, only one premenopausal woman had vertebral fracture identified at baseline, and there were no incident vertebral fractures in this age group. Forty-one postmenopausal women were identified with prevalent vertebral fractures at baseline (Table 1); this represents 7% of the full postmenopausal OPUS population. Eighteen postmenopausal women were identified with incident vertebral fracture at 6 years (3% of the postmenopausal subset). The distribution of fractures by vertebral level is shown in Fig. 2. Ten percent of vertebrae could not be reliably assessed due to poor image quality: these were predominantly between vertebrae T4 and T6.
Prevalent and incident vertebral fractures identified in 601 postmenopausal women studied at baseline and 6 years. Vertebral images were obtained using a Hologic fan-beam densitometer. Vertebral fractures were identified by the ABQ method [6]. Results are presented as the frequency of fracture at each vertebral level
Among postmenopausal women with incident vertebral fracture, a significantly greater proportion had been identified with prevalent vertebral fracture at baseline compared to those identified fracture-negative (P < 0.0001) (Table 1). Among postmenopausal women with no prevalent vertebral fracture at baseline, there was no difference in the proportions of women with (3%) or without SVH (2%) who went on to sustain incident vertebral fracture (P = 0.640) (Table 1).
Characteristics of postmenopausal women with and without vertebral fracture
Postmenopausal women with prevalent vertebral fracture at baseline were significantly older (P < 0.0001) and had significantly lower total hip BMD (P < 0.0001) compared to women who were fracture-negative (Table 2). Women with incident vertebral fractures at 6 years were also older (P = 0.002) with lower total hip BMD (P = 0.001) compared to women without incident fractures. There was a trend towards lower lumbar spine BMD in women with incident vertebral fractures (P = 0.086) (Table 3). The results were similar when means were compared in women with incident vertebral fracture and women without vertebral fracture at either baseline or follow-up (Table 3).
Association between prevalent and incident vertebral fractures
In postmenopausal women, incident vertebral fracture at 6 years was significantly associated with prevalent vertebral fracture identified at baseline. The unadjusted OR for incident vertebral fracture was 7.8 (95% CI 2.8, 22.1). The OR remained significant after adjustment for age and total hip BMD (Table 4). The unadjusted OR for women with only mild prevalent vertebral fracture was 5.3 (95% CI 1.4, 19.8); after adjustment for age and total hip BMD, the OR was 3.7, but the confidence intervals spanned zero (0.9, 14.7) (Table 4). Among postmenopausal women without prevalent vertebral fracture at baseline, there was no association between SVH and incident vertebral fracture (P = 0.748) (Table 4).
Discussion
We performed the first analysis of longitudinal VFA using the ABQ method, in a subset of the OPUS population-based cohort. The prevalence of postmenopausal women with prevalent vertebral fracture at baseline was 7%; in premenopausal women, it was <1%. Incident vertebral fractures were identified at 6-year follow-up in 3% of postmenopausal women. Prevalent vertebral fracture in postmenopausal women was associated with an eightfold greater risk of incident vertebral fracture (P < 0.001). The greater risk remained significant after adjusting for age and BMD (OR 4.3).
The prevalence of vertebral fracture in this postmenopausal subset of OPUS is the same as in a previous study of postmenopausal women in which the ABQ method was used to identify vertebral fractures from spinal radiographs [10]. That study was also population based and included women of a similar age range (50 to 85 years at baseline) to our postmenopausal subset. In our earlier cross-sectional VFA study (OPUS baseline), the prevalence of women with vertebral fracture identified by ABQ was 9% [7]; that analysis was based on UK women only, whereas the current analysis also included women from Paris and Kiel.
The ABQ method generally identifies fewer prevalent fractures than other approaches [8, 11] which might explain the lower prevalence in this compared to other recent VFA studies [12–16]. We could have failed to detect some fractures due to poor differentiation of the vertebral endplates on VFA, but the relatively low prevalence identified by ABQ may also reflect differences in the criteria used to define fracture. Non-fracture SVH was identified in 39% of the postmenopausal women without prevalent vertebral fracture in this subset, and we could have misclassified some women with true fractures within this group. However, SVH was not significantly associated with low bone density in this subset, nor was it significantly associated with incident vertebral fracture identified on VFA (Table 4). Nevertheless, our results need to be interpreted cautiously due to the small number of vertebral fractures and limited power.
To date, the ABQ method has not been recommended for use in VFA [3, 17] because until recently, there were no data for evidence of a link with incident fractures. In the current analysis, we observed a strong association between prevalent fractures identified by ABQ and the incidence of new vertebral fractures, even after adjustment for age and BMD. This builds on recent evidence of a significant association between ABQ prevalent vertebral fracture and incident fracture identified on radiographs, in which women with prevalent vertebral fracture had a relative risk of 5.8 for incident vertebral fracture (univariate analysis) [10].
Previous studies have established that VFA may be a useful tool to identify patients with vertebral fractures that may not otherwise have been detected on the basis of bone density alone [18–20]; our current analysis strengthens the case for using VFA alongside other fracture risk assessment tools. To our knowledge, the predictive power of VFA for future osteoporotic fracture has only been reported in one previous publication; this was a study of older patients screened for entry into a clinical trial of clodronate [21]. In that analysis, vertebral fractures were identified by the McCloskey morphometric algorithm, with visual differential diagnosis of non-osteoporotic deformities. Odds ratios for incident vertebral fractures were not reported, but women with prevalent vertebral fracture identified on VFA had an OR of 2.0 for hip fracture and 2.29 for any osteoporotic fracture, and these remained statistically significant after adjusting for age, BMD and treatment.
Our study had some limitations. Seventy-three percent of postmenopausal women who attended OPUS at baseline returned for follow-up visits at 6 years; our postmenopausal subset represented only 34% of OPUS returners. On average, our subset was broadly similar to the full population in terms of baseline characteristics, but the women in our subset did have higher total hip BMD (P < 0.001) and higher broadband ultrasound attenuation at the heel (P < 0.01) (post hoc analysis). However, site-specific differences in BMD were observed across the whole of the OPUS study [22]. Nevertheless, the incidence of vertebral fracture in our subset may have been lower than might have been observed in the full baseline population; thus, our results may not be directly applicable to the wider population. The relatively low prevalence and incidence of vertebral fractures in our study population may also have limited the power of our statistical analyses. Fracture assessments made from spinal radiographs are generally considered the gold standard, but we did not have access to ABQ radiographic readings for direct comparison with ABQ VFA in this subset. Our analysis was based on images acquired by Hologic devices only: different results might be obtained using other manufacturers' machines because of slight differences in the way that vertebral images are acquired and processed.
Conclusions: population-based postmenopausal women had relatively low prevalence and incidence of vertebral fracture identified by VFA using the ABQ method. Women with prevalent vertebral fracture had a significantly greater risk of incident vertebral fracture compared to women without prevalent fracture.
References
Klotzbuecher CM, Ross PD, Landsman PB, Abbott TA, Berger M (2000) Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res 15:721–739
Blake GM, Rea JA, Fogelman I (1997) Vertebral morphometry studies using dual-energy x-ray absorptiometry. Semin Nucl Med 27:276–290
Schousboe JT, Vokes T, Broy SB, Ferrar L, McKiernan F, Roux C, Binkley N (2008) Vertebral fracture assessment: the 2007 ISCD official positions. J Clin Densitom 11(1):92–108
Vokes T, Bachman D, Baim S, Binkley N, Broy S, Ferrar L, Lewiecki EM, Richmond B, Schousboe J (2006) Vertebral fracture assessment: the 2005 ISCD official positions. J Clin Densitom 9:37–46
Genant HK, Wu CY, van Kuijk C, Nevitt MC (1993) Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 8:1137–1148
Jiang G, Eastell R, Barrington NA, Ferrar L (2004) Comparison of methods for the visual identification of prevalent vertebral fracture in osteoporosis. Osteoporos Int 15:887–896
Ferrar L, Jiang G, Clowes JA, Peel NF, Eastell R (2008) Comparison of densitometric and radiographic vertebral fracture assessment using the algorithm-based qualitative (ABQ) method in postmenopausal women at low and high risk of fracture. J Bone Miner Res 23:103–111
Ferrar L, Jiang G, Schousboe JT, DeBold CR, Eastell R (2008) Algorithm-based qualitative and semiquantitative identification of prevalent vertebral fracture: agreement between different readers, imaging modalities, and diagnostic approaches. J Bone Miner Res 23:417–424
Glüer CC, Eastell R, Reid DM, Felsenberg D, Roux C, Barkmann R, Timm W, Blenk T, Armbrecht G, Stewart A, Clowes J, Thomasius FE, Kolta S (2004) Association of five quantitative ultrasound devices and bone densitometry with osteoporotic vertebral fractures in a population-based sample: the OPUS study. J Bone Miner Res 19:782–793
Finigan J, Greenfield DM, Blumsohn A, Hannon RA, Peel NF, Jiang G, Eastell R (2008) Risk factors for vertebral and nonvertebral fracture over 10 years: a population-based study in women. J Bone Miner Res 23:75–85
Ferrar L, Jiang G, Cawthon PM, San Valentin R, Fullman R, Lambert L, Cummings SR, Black DM, Orwoll E, Barrett-Connor E, Ensrud K, Fink HA, Eastell R (2007) Identification of vertebral fracture and non-osteoporotic short vertebral height in men: the MrOS study. J Bone Miner Res 22:1434–1441
Xu WW, Perera S, Medich D, Fiorito G, Wagner J, Berger LK, Greenspan SL (2011) Height loss, vertebral fractures, and the misclassification of osteoporosis. Bone 48:307–311
El Maghraoui A, Morjane F, Nouijai A, Achemlal L, Bezza A, Ghozlani I (2009) Vertebral fracture assessment in Moroccan women: prevalence and risk factors. Maturitas 62:171–175
Jager PL, Jonkman S, Koolhaas W, Stiekema A, Wolffenbuttel BHR, Slart RHJA (2010) Combined vertebral fracture assessment and bone mineral density measurement: a new standard in the diagnosis of osteoporosis in academic populations. Osteoporos Int 22(4):1059–1068
Vokes TJ, Gillen DL (2010) Using clinical risk factors and bone mineral density to determine who among patients undergoing bone densitometry should have vertebral fracture assessment. Osteoporos Int 21:2083–2091
Fuerst T, Wu C, Genant HK, von Ingersleben G, Chen Y, Johnston C, Econs MJ, Binkley N, Vokes TJ, Crans G, Mitlak BH (2009) Evaluation of vertebral fracture assessment by dual X-ray absorptiometry in a multicenter setting. Osteoporos Int 20:1199–1205
Grados F, Fechtenbaum J, Flipon E, Kolta S, Roux C, Fardellone P (2009) Radiographic methods for evaluating osteoporotic vertebral fractures. Joint Bone Spine 76:241–247
Howat I, Carty D, Harrison J, Fraser M, McLellan AR (2007) Vertebral fracture assessment in patients presenting with incident nonvertebral fractures. Clin Endocrinol 67:923–930
Chapurlat RD, Duboeuf F, Marion-Audibert HO, Kalpakçioglu B, Mitlak BH, Delmas PD (2006) Effectiveness of instant vertebral assessment to detect prevalent vertebral fracture. Osteoporos Int 17:1189–1195
Middleton ET, Steel SA (2008) Routine versus targeted vertebral fracture assessment for the detection of vertebral fractures. Osteoporos Int 9:1167–1173
McCloskey EV, Vasireddy S, Threlkeld J, Eastaugh J, Parry A, Bonnet N, Beneton M, Kanis JA, Charlesworth D (2008) Vertebral fracture assessment (VFA) with a densitometer predicts future fractures in elderly women unselected for osteoporosis. J Bone Miner Res 23:1551–1568
Paggiosi MA, Glüer C-C, Roux C, Reid DM, Felsenberg D, Barkmann R, Eastell R (2011) International variation in proximal femur bone mineral density. Osteoporos Int 22(2):721–729
Acknowledgements
The OPUS study was sponsored by Eli Lilly, Sanofi-aventis, Procter and Gamble Pharmaceuticals, Hoffman-La Roche, Pfizer and Novartis, and we acknowledge the support of the National Institute for Health Research, UK, via its Biomedical Research Units funding scheme. Dr. Ferrar received support via a Medical Research Council UK research fellowship (2004–2008). We thank the following members of the OPUS teams at the five participating centres for their contributions: Alison Stewart, Rosie Reid and Lana Gibson (Aberdeen); the members of the Zentrum fur Muskel und Knochenforschung (Berlin), Gabriele Armbrecht, Friederike Tomasius, Frank Touby, Martina Kratzsch and Tilo Blenk; Reinhard Barkmann, Wolframm Timm, Antonia Gerwin, Maren Glüer, Roswitha John, Roswitha Marunde-Ott, Marika Mohr, Regina Schlenger, Pia Zschoche, Carsten Liess and Carsten Rose (Kiel); Therese Kolta and Nathalie Delfau (Paris) and Jackie Clowes, Margaret Paggiosi, Nicky Peel, Judy Finigan and Debbie Swindell (Sheffield).
Conflicts of interest
Richard Eastell is a consultant for Unilever and receives research funding. He has received consulting fees from Amgen, Astrazeneca, GlaxoSmithKline, Medtronics, Nastech, Nestle, Fonterra Brands, Novartis, Ono Pharma, Osteologix, Pfizer, Lilly, Sanofi-aventis, Procter and Gamble, Tethys, Unilever, Unipath, Inverness Medical and grants from AstraZeneca, Amgen, Procter and Gamble, Unipath, Pfizer, Lilly, Novartis, Osteologix, Medical Research Council, Arthritis Research UK, Crescent Diagnostics, Nittoboseki, Nestle and Sanofi-aventis. He has also received honoraria from Takeda, Lilly, Amgen, the National Osteoporosis Foundation, Procter and Gamble and GlaxoSmithKline Nutrition.
Disclaimer
The views expressed in this publication are those of the authors and not necessarily those of the NHS, the NIHR or the UK Department of Health.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ferrar, L., Roux, C., Felsenberg, D. et al. Association between incident and baseline vertebral fractures in European women: vertebral fracture assessment in the Osteoporosis and Ultrasound Study (OPUS). Osteoporos Int 23, 59–65 (2012). https://doi.org/10.1007/s00198-011-1701-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-011-1701-3